Abstract
Background and purpose — The burden of road traffic injuries globally is rising rapidly, and has a huge effect on health systems and development in low- and middle-income countries. Malawi is a small low-income country in southeastern Africa with a population of 16.7 million and a gross national income per capita of only 250 USD. The impact of the rising burden of trauma is very apparent to healthcare workers on the ground, but there are very few data showing this development.
Patients and methods — The annual number of femoral fracture patients admitted to Kamuzu Central Hospital (KCH) in the Capital of Malawi, Lilongwe, from 2009 to 2014 was retrieved from the KCH trauma database. Linear regression curve estimation was used to project the growth in the burden of femoral fractures and the number of operations performed for femoral fractures over the same time period.
Results — 992 patients with femoral fractures (26% of all admissions for fractures) presented at KCH from 2009 through 2014. In this period, there was a 132% increase in the annual number of femoral fractures admitted to KCH. In the same time period, the total number of operations more than doubled, but there was no increase in the number of operations performed for femoral fractures. Overall, there was a 7% mortality rate for patients with femoral fractures.
Interpretation — The burden of femoral fractures in Malawi is rising rapidly, and the surgical resources available cannot keep up with this development. Limited funds for orthopedic trauma care in Malawi should be invested in central training hospitals, to develop a sustainable number of orthopedic surgeons and improve current infrastructure and equipment. The centralization of orthopedic surgical care delivery at the central training hospitals will lead to better access to surgical care and early return of patients to local district hospitals for rehabilitation, thus increasing surgical throughput and efficiency in a more cost-effective manner, with the goal of expanding the future orthopedic surgical workforce to meet the national need.
The burden of road traffic injuries (RTIs) globally is rising rapidly, and it has a huge impact on health systems and development in low- and middle-income countries (LMICs). RTIs are already the leading cause of death in young people aged 15–29 years globally (WHO 2015), and this mortality is most pronounced in LMICs (Patton et al. 2009). In addition to this devastating loss of young lives, RTIs also have a severe economic impact on governments in LMICs, with the World Health Organisation estimating that RTIs cost countries 3% of their GDP globally (WHO 2015). In South Africa, RTIs are estimated to cost society a massive 8% of GDP (WHO 2015).
Despite having the lowest number of motor vehicles per capita, the African WHO region has the highest incidence or road traffic crashes in the world (WHO 2015). Malawi is estimated to have the second highest incidence of road traffic deaths of all countries, at 35 deaths per 100,000 population per year, which is only marginally less than in Thailand (36 per 100,000). For comparison, the USA has 11, the UK has 2.9, and Norway has 3.8 deaths per 100,000 per year. In addition to the mortality burden, it is estimated that more than 20 times as many are injured and need treatment (Peden 2004). Estimates of the number of people with permanent disability after RTIs vary from 0.5% of those who are injured in Croatia to 60% of those injured in Guatemala, and are likely to depend on injury mechanisms, the severity of injuries, and the quality of the existing public healthcare system in each country. Estimates for most LMICs, however, appear to suggest that 10–15% of RTI victims end up with a permanent disability of some kind (WHO 2015).
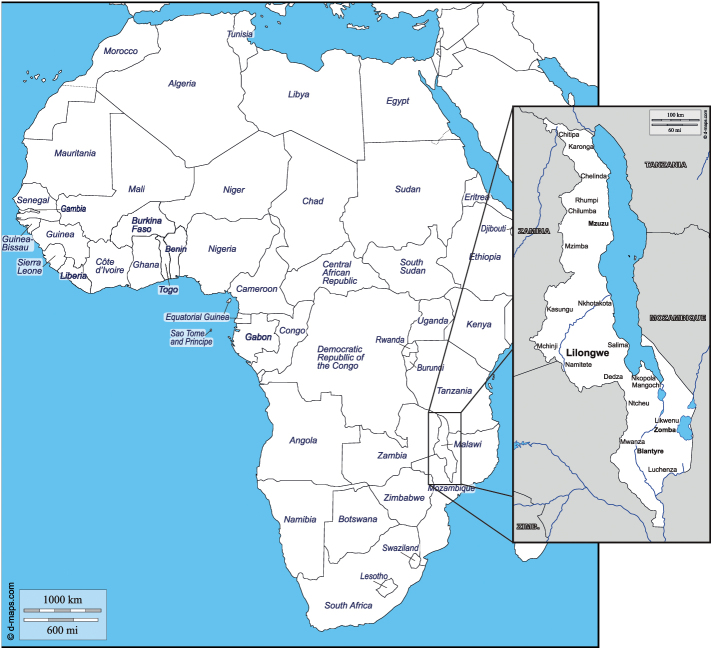
Malawi is a small country in southeastern Africa (Figure 1), with a population of 16.7 million (World Bank 2014). It is a low-income country with a gross national income (GNI) per capita of only 250 USD (World Bank 2014), and an annual total health expenditure per capita of only 26 USD, the tenth lowest in the world. For comparison, this is 374 times less than in Norway. 85% of the population depends on subsistence farming and more than half of the population live below the poverty line.
Figure 1.
Malawi is a densely populated, landlocked country in southern Africa. About twothirds of the length of the country lies along the western shore of Lake Malawi, the third largest lake in Africa after Lake Victoria and Lake Tanganyika. Courtesy of d-maps.com (http://www.dmaps.com).
Kamuzu Central Hospital (KCH), in the capital, Lilongwe, is the referral hospital for the Central Region of Malawi. It has a catchment population of approximately 6 million people. The hospital has approximately 900 beds, 250 of which belong to the Department of Surgery—including 72 pediatric beds that are each usually occupied by at least 2 children. Approximately 80 adult beds and 32 pediatric beds are occupied by patients with orthopedic trauma or infections. During the study period, there was originally only 1 orthopedic surgeon, which later increased to 2 orthopedic surgeons and 2 orthopedic surgery trainees, or registrars (Young et al. 2016). There were also 7 orthopedic clinical officers, who have undergone 18 months of training in treating orthopedic trauma and other conditions (Mkandawire et al. 2008). They took care of most of the day-to-day work in the outpatient department and contributed to both ward work and surgery. The Department of Surgery has 4 operating theaters, only 1 of which is available for orthopedic surgery. We have noticed a dramatic increase in the rate of admissions for severe injury over the last few years, but very few data have been published describing this trend over time in Malawi.
KCH has a trauma surveillance registry, supported by the University of North Carolina, that has captured all patients presenting to the KCH casualty department since 2008 (Samuel et al. 2009). During this period, we have been using the SIGN intramedullary (IM) nail to treat femoral fractures at KCH. All operations performed using this IM nail are registered in the SIGN online surgical database (Young et al. 2011).
From 2008 to the present, the capacity to deliver orthopedic services at KCH has increased through institutional collaboration with Haukeland University Hospital in Norway and the start of a training program for orthopedic surgeons at KCH (Young et al. 2016). However, the increasing burden of traumatic injury with the associated increase in injury severity in a hospital system with limited theater availability has necessitated a change in clinical practice. Priority has increasingly had to be given to patients with life- and limb-threatening conditions such as acute musculoskeletal infections in children and severe open fractures in young adults. As a result, other trauma patients who would otherwise benefit greatly from surgery, such as patients with femoral fractures or displaced lower arm fractures, are treated nonoperatively—resulting in poor clinical and functional outcomes (Young et al. 2012).
In this study, we evaluated the trends in burden of trauma and we assessed the effect on delivery of service at KCH in Malawi, using adult femoral fracture incidence and therapeutic intervention as a proxy for healthcare system needs.
Methods
This study was an audit of prospectively collected hospital trauma registry data at KCH. The number of patients (aged ≥16 years) with femoral fractures who were admitted to KCH per year from 2009 through 2014 was retrieved from the KCH trauma database. All patients who present at the KCH casualty department after injury are registered in this database (National Health Sciences Research Committee approval no. 813). The number of femoral fractures operated per year was retrieved from the SIGN online surgical database, and the total number of orthopedic surgical procedures performed was collected from the KCH theater register book.
Statistics
Descriptive statistics were done using Stata SE version 13.1. Bivariate analysis was performed using Pearson’s chi-square test for categorical variables and Student’s 2-sample t-test for continuous variables. When comparing medians of continuous variables, we used the median test. Regression-line estimations for the number of femoral fractures admitted to KCH per year, the annual number of operations done for femoral fractures, and the total number of orthopedic operations at KCH were calculated using IBM SPSS Statistics version 22. The level of statistical significance was set at 5%.
Results
3,779 adults (age ≥16 years) were admitted to Kamuzu Central Hospital due to fractures from 2009 through 2014. Of these patients, 992 (26%) presented with femoral fractures. 39 patients (4%) died in the casualty department and 83 were registered as discharged from casualty, leaving 866 patients admitted to the ward (28% women). Year-by-year data are presented in Table. Men admitted with femoral fractures had a median age of 36 (16–96) years, as compared to a median age of 60 (16–93) years in women (p < 0.001). 55% of men were RTI victims, as compared to 25% of women (p < 0.001). The length of hospital stay was similar for men (30 (SD 30) days) and women (31 (SD 23) days). 71 patients with femoral fractures died either in casualty or later in the ward, giving a total mortality rate of 7%.
The number of patients with femoral fractures who presented at KCH increased by 132% from 2009 to 2014 (from 95 to 220). A statistically significant regression equation showing this increasing trend was found (F(1,4) = 11.7, p = 0.03), with a R2 of 0.745. If this trend continues, the number of adults with femoral fractures who are admitted to KCH will double again in just 8 years (with an estimated number of admissions in 2023 of 436) (Figure 2). Over the same time period, there was no change (non-significant tendency for reduction) in the number of operations performed for femoral fractures (R2 = 0.286, F(1,4) = 1.60; p = 0.3) (Figure 2).
Figure 2.
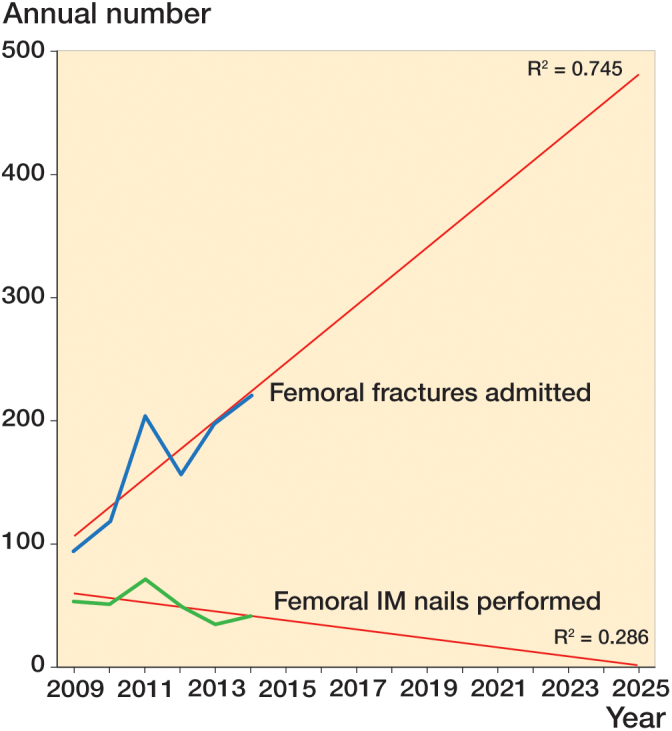
Observed annual number of adult femoral fractures admitted to KCH (top, blue), and the annual number of femoral IM nails performed at KCH (bottom, green). The straight lines in red are the regression-line estimations with projections for the coming years. An increasing gap is apparent between femoral trauma burden and delivery of service.
To rule out a general decrease in surgical activity as being the cause of the lack of increase in operations for femoral fracture (to meet the increase in demand), we plotted the total annual number of orthopedic operations from 2008 through 2014 (Figure 3). This number more than doubled from 454 operations in 2008 to 969 in 2011, and has since remained at this level. The regression-line estimation showed a statistically significant increase in the number of operations done at KCH over the whole time period (R2 = 0.777, F(1,5) = 17.46; p = 0.009).
Figure 3.
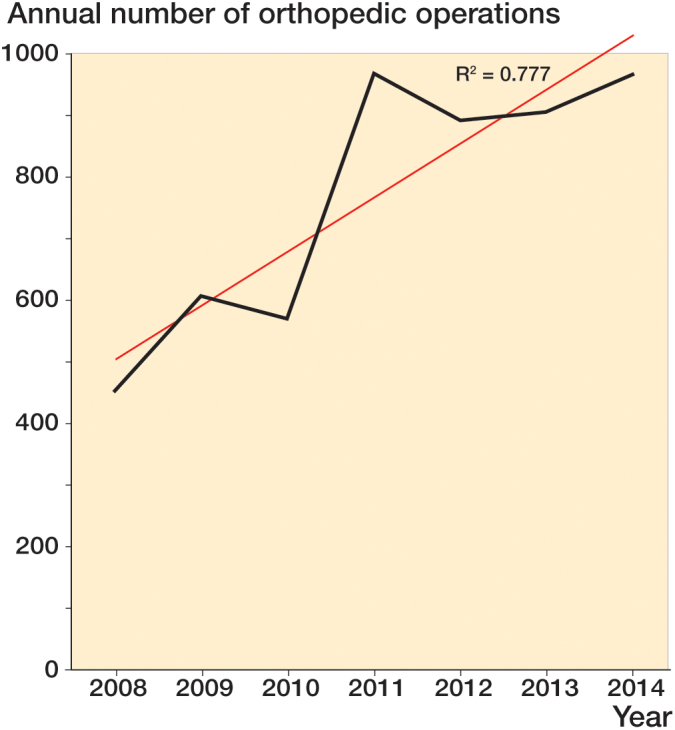
The annual number of orthopedic operations performed at KCH from 2008 through 2014 (black) shows a rapid increase in surgical activity after international support for the KCH surgery training program started in 2008, but this appears to have reached a plateau from 2011 onwards due to the availability of only 1 theater. The regression-line estimation (red) shows a statistically signifi cant increase in surgical activity over the whole period (p = 0.009).
Discussion
Our findings revealed a rapidly increasing gap between the incidence and the operative intervention of femoral fractures at Kamuzu Central Hospital in Lilongwe, Malawi, despite the general increase in orthopedic operative volume. The number of patients with femoral fractures who present at KCH has risen by 132% in just 5 years, and is projected to double again in just 8 years. Despite this, the number of operations done for femoral fractures was relatively unchanged. The high mortality of 7% in patients with femoral fractures in this study emphasizes the seriousness of this growing challenge. The KCH trauma database unfortunately did not record the reason for these deaths, but deaths in casualty in our setting are usually due to poly trauma and a lack of available blood products from the blood bank. No anti-thrombotic medication is available for patients at KCH, and death in the ward in patients with femoral fracture can often be attributed to venous thromboembolism (Young et al. 2013).
Since 2009, there has been no increase in the number of operating theaters at KCH, with only one theater per day for orthopedic surgery for the entire catchment population of KCH, which is about 6 million people. Through international collaborations, we have managed to increase the capacity of orthopedic surgery somewhat within the existing physical infrastructure by training staff, upgrading equipment, and improving the supply of surgical implants. However, the lack of operating theater capacity has limited any further increase in the number of operative interventions. We have previously shown the increasing burden of serious open fractures and how increased use of limb-saving procedures has reduced the rate of amputations in the same period of time (Young et al. 2016). When combined, these findings suggest a shift in priority away from operative treatment of femoral fractures, which have an alternative (albeit far inferior) nonoperative management option, towards limb-saving surgery. This clearly has a negative effect on the capacity to treat other serious injuries.
The limitations of our study are those inherent in any registry-based study. One important limitation is that the KCH trauma database does not discriminate between different locations of femoral fractures. The inclusion of low-energy proximal femur fractures most likely explains the higher than expected mean age of the patients. We have previously reported that the median age of people undergoing surgery for femoral shaft fractures at KCH was 30 years (Young et al. 2013). Whereas femoral shaft fractures are generally high-energy fractures in young adults, proximal femur fractures are more likely to be due to low-energy falls in the elderly population. This also explains the difference in the median age of men (36 years) and women (60 years) in this study. Men were more likely to have a high-energy injury (where RTIs accounted for 55%) than women (where RTIs accounted for 25%). However, even if a substantial proportion of the femoral fractures registered in the present study were proximal femur fractures, none of these would have been operated either. Operative intervention is the established treatment of choice for all femoral fractures in adults, irrespective of anatomical location, but today all these are initially treated with traction at KCH. While at the beginning of the study period many femoral shaft fractures would have been operated within 3 weeks of injury (Young et al. 2013), currently only patients with fractures not amenable to traction therapy—or that have failed traction therapy—are considered for operation due to lack of capacity. In the study period, 83 patients were “discharged from casualty” (Table). We do not have details of why these patents were discharged with a femoral fracture, but the reasons included requests for transfer to a private or local hospital and presentation with an old neglected fracture that did not need emergency admission.
Projections for the future should always be interpreted with caution, especially when based on only 6 years of data. However, our findings do illustrate the front-line impact of the growing epidemic of injuries in the region, with an increasing gap between the burden of trauma and the capacity to deliver a surgical service in Malawi. No reliable national statistics are available for Malawi, but if the WHO estimates hold true, this would indicate that more than 110,000 people are injured on Malawi’s roads every year, and that thousands end up with permanent disability (WHO 2015). The Lancet Global Surgery Commission recommended in its 2015 report that a minimum rate of 5,000 surgeries per 100,000 population should be available to ensure equitable service delivery in LMICs (Meara et al. 2015). This is an aspirational goal in Malawi, but with the right support of surgical training centers and infrastructure in Malawi, delivery of surgical services could be scaled up considerably in the near future (Young et al. 2016). For this to be possible, it is imperative that the central training hospitals should be allowed to retain the staff they train until a critical mass of surgeons is employed to sustain the training programs.
In a setting with limited resources, such as in Malawi, a resource-intensive speciality such as orthopedic trauma surgery cannot be decentralized to the district hospitals from the start. A more sustainable approach would be to build up sufficient operative surgical capacity in the central training hospitals, and to have these central hospitals serve as “short-stay trauma centers” for the district hospitals. In Malawi, the district hospitals already transfer patients to and from the central hospital with their ambulances on an almost daily basis. Short-stay trauma centers could efficiently treat trauma victims from the district and send them back to the district hospital within a few days. This would free up beds in the central hospital and use the capacity in the districts for rehabilitation close to the patient’s home and family. This strategy, in an environment with limited resources, would result in increased operative intervention for the whole population without having to bear the high cost of setting up centers that are capable of orthopedic surgery at smaller hospitals.
As orthopedic surgical training programs evolve in Malawi, training hospitals must retain orthopedic personnel until these programs become self-sustaining and mature. Sending newly qualified orthopedic consultants to hospitals lacking the right orthopedic surgical infrastructure would probably lead to 1 of 2 short-term results: (1) a lack of professional fulfillment, leading to an inevitable exodus from the public health system, or (2) large public financial investment having to be made to improve the surgical infrastructure and levels of equipment at other hospitals across the country. Even in the second scenario, the investment is likely to be too small and to lack sustainable re-supply of surgical implants, with a substantial risk that these scarce funds are entirely wasted.
It is an obvious goal to have fully trained surgeons at all hospitals in Malawi, but this will take many years. In the immediate future, a better way of using the scarce human resources, once sufficient numbers of surgeons become available, is through regular surgical outreach visits from the central hospitals to the district hospitals, to perform simple surgery and identify patients requiring higher-level orthopedic surgical care at the central hospital.
In summary, the burden of femoral fractures in Malawi is rapidly increasing and the available surgical capacity cannot meet the current demand or the projected demand. Urgent investment in infrastructure and surgical education is needed to meet the rise in trauma in Malawi. The limited funds for orthopedic trauma care in Malawi are better invested in central training hospitals to develop a sustainable mass of trained orthopedic surgeons, with good infrastructure and equipment. The centralization of orthopedic surgical care delivery at training hospitals would lead to better access to surgical care and early return of patients to district hospitals for rehabilitation. This would increase surgical throughput and efficiency with a view to expanding the orthopedic surgical workforce to meet the national need.
We thank Dr Eva Dybvik and Professor Stein Atle Lie, biostatisticians at the Norwegian Arthroplasty Register, for their advice on the use of regression-line equations.
Patients admitted to KCH for femoral fracture from 2009 through 2014
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | total | |
|---|---|---|---|---|---|---|---|
| Patients admitted with fractures, n | 365 | 494 | 829 | 681 | 697 | 713 | 3,779 |
| Femoral fractures, n | 95 | 118 | 204 | 156 | 199 | 220 | 992 |
| Death declared in casualty, n (%) | 6 (6.3) | 4 (3.4) | 6 (2.9) | 4 (2.6) | 11 (5.5) | 8 (3.6) | 39 (3.9) |
| Discharged from casualty | 11 | 16 | 14 | 7 | 14 | 21 | 83 |
| Admitted femoral fractures | 77 | 95 | 184 | 145 | 174 | 191 | 866 |
| Female patients | |||||||
| n (%) | 13 (17) | 26 (27) | 44 (24) | 50 (35) | 51 (29) | 57 (30) | 241 (28) |
| mean (SD) age | 42 (18) | 50 (21) | 52 (25) | 59 (21) | 56 (19) | 54 (22) | 54 (22) |
| mean (SD) LOS, days | 4.5 (2.1) | 12 (9.3) | 27 (33) | 27 (21) | 32 (17) | 38 (26) | 31 (23) |
| Male patients | |||||||
| mean (SD) age | 41 (19) | 37 (16) | 39 (19) | 46 (22) | 41 (19) | 45 (20) | 42 (19) |
| mean (SD) LOS, days | 11 (15) | 13 (11) | 30 (24) | 24 (17) | 33 (44) | 36 (24) | 30 (30) |
| Deaths in admitted patients, n (%) | 2 (2.6) | 0 (0) | 13 (7.1) | 5 (3.5) | 5 (2.9) | 7 (3.7) | 32 (3.7) |
| Total mortality from femoral fracture, n (%) | 8 (8.4) | 4 (3.4) | 19 (9.3) | 9 (5.8) | 16 (8.0) | 15 (6.8) | 71 (7.2) |
LOS – length of hospital stay
References
- Meara J G, Leather A J M, Hagander L, Alkire B C, Alonso N, Ameh E A, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 2015; 386 (9993): 569–624. [DOI] [PubMed] [Google Scholar]
- Mkandawire N, Ngulube C, Lavy C.. Orthopaedic clinical officer program in Malawi: a model for providing orthopaedic care. Clin Orthop Relat Res 2008; 466 (10): 2385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton G C, Coffey C, Sawyer S M, Viner R M, Haller D M, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 2009; 374 (9693): 881–92. [DOI] [PubMed] [Google Scholar]
- Peden M. World report on road traffic injury prevention. World Health Organization; Geneva: 2004 [Google Scholar]
- Samuel J C, Akinkuotu A, Villaveces A, Charles A G, Lee C N, Hoffman I F, et al. Epidemiology of injuries at a tertiary care center in Malawi. World J Surg 2009; 33 (9): 1836–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Global status report on road safety 2015. World Health Organization, Geneva; 2015 [Google Scholar]
- Young S, Lie S A, Hallan G, Zirkle L G, Engeseter L B, Havelin L I.. Low infection rates after 34,361 intramedullary nail operations in 55 low- and middle-income countries. Acta Orthop 2011; 82 (6): 737–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Beniyasi F J, Munthali B, Banza L.. Infection of the fracture hematoma from skeletal traction in an asymptomatic HIV-positive patient. Acta Orthop 2012; 83 (4): 423–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Banza L N, Hallan G, Beniyasi F, Manda K G, Munthali B S, et al. Complications after intramedullary nailing of femoral fractures in a low-income country. Acta Orthop 2013; 84 (5): 460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Banza L, Mkandawire N.. The impact of long term institutional collaboration in surgical training on trauma care in Malawi [Internet]. SpringerPlus. 2016; 5 (1): 1–5. Available from: http://dx.doi.org/10.1186/s40064-016-2050-7 [DOI] [PMC free article] [PubMed] [Google Scholar]