Abstract
Introduction
The epidermal growth factor receptor (EGFR) T790M mutation remains one of the major mechanisms of resistance to EGFR tyrosine kinase inhibitors (TKI) treatment. Cases of de novo EGFR T790M mutations prior to TKI treatment have been reported, but most of them were somatic mutations. In this study, we report a case of primary de novo dual EGFR mutations containing a germline T790M mutation in a NSCLC patient. We further describe a case series of NSCLC patients who had primary dual or multiple EGFR mutations.
Methods
EGFR mutation status was analyzed in 427 patients with lung adenocarcinomas. Clinical, demographic data and sequencing electropherograms were collected on patients with two or more EGFR mutations identified prior to EGFR TKI treatment. Peripheral blood mononuclear cells were sequenced for germ-line EGFR mutation on two patients with primary T790M mutation.
Results
55 out of 427 (13%) patients with lung adenocarcinomas were found to have EGFR mutations; twelve of which were identified to have either dual or multiple EGFR mutations. Five of these 12 patients (42%) had primary de novo T790M mutation and three of them showed similar heights of the mutant and wild-type peaks on sequencing electropherogram, suggesting the possibility of germline mutation. One case of germline EGFR T790M mutation was confirmed via sequencing a peripheral blood sample.
Conclusions
Dual or multiple EGFR mutations comprised 2.8% of lung adenocarcinomas in our study. Primary de novo EGFR T790M mutation are presented with high frequency (5/12; 42%) in patients carrying dual or multiple EGFR mutations.
Keywords: Dual EGFR Mutations, T790M germline mutation, Lung Adenocarcinoma
Introduction
Exon 19 deletions and point mutations in L858R are the most common somatic activating mutations in the epidermal growth factor receptor (EGFR) gene that confer sensitivity to EGFR tyrosine kinase inhibitors (TKI) in lung cancer1. However, despite the initial response to EGFR TKIs, all patients will eventually develop resistance. One of the most common mechanisms of resistance is acquisition of a second mutation at exon 20 which causes a T790M substitution.2,3. Although most of these cases are acquired resistance through somatic mutations, a small number of germline EGFR T790M have been reported, and are estimated to occur in 1% of non-small cell lung cancer cases4,5,6. These germline EGFR T790M mutations are believed to predispose patients to lung cancer, as preclinical studies have shown the germline T790M mutation to be a weak oncogene that often requires a secondary mutation to potentiate cancer development5,6.
In Asia, a few cases of dual EGFR mutations containing primary de novo T790M substitution prior to TKI treatment have been described7,8, however none were identified to be germline mutations. In contrast, thus far germline EGFR T790M mutations have only been described In Caucasian patients with lung cancer5,6. Several family members of European descent with hereditary bronchioalveolar carcinoma were identified to have germline T790M mutations9. Our group previously reported a case of a 72 year-old patient with a solitary T790M mutation who had a germline T790M mutation in her peripheral blood mononuclear cells (PBMC)10. Recently, two USA cases with germline T790M mutations were reported in never smoking female Caucasian patients5,6. In this brief report, we describe another case of a Caucasian female patient with lung adenocarcinoma who had a germline EGFR T790M mutation and concurrent somatic L858R mutation. We further describe a case series of patient demographics and tumor characteristics associated with primary EGFR T790M mutations in NSCLC patients.
Material and methods
Patient Selection and Data Collection
Following Institutional Review Board approval at MD Anderson Cancer Center, clinical and demographic data were collected on all patients with lung adenocarcinomas between May 2005 and Aug 2009 identified to have two or more EGFR mutations. Of 2 patients identified to have a primary de novo T790M mutation, peripheral blood mononuclear cells were isolated and assessed for germline EGFR mutation status.
Tumor and Germline Genotyping
DNA sequences for EGFR (exons 18–21) extracted from paraffin-embedded tissue (NSCLC tumors) or PBMC (for germline assessment) were amplified using standard PCR primers and sequenced. All sequence variants were confirmed by independent PCR amplifications from at least 2 independent DNA extractions, and sequenced in both directions.
Results
Frequency of primary de novo dual or multiple EGFR Mutations in patients with lung adenocarcinomas
We evaluated 427 patients treated at the MD Anderson Cancer Center Thoracic Clinic with lung adenocarcinomas between May 2005 and Aug 2009. Among these NSCLC patients, 55 patients were identified to have de novo EGFR mutations in their tumors. Twelve patients (12/427, 2.8%) were found to have either dual or multiple EGFR mutations, of whom 5 patients had primary de novo T790M mutations. The clinical and demographic information of patients with primary de novo T790M mutations are shown in Table 1. The information of patients who had dual or multiple EGFR mutations without T790M mutations are included in Supplementary Table 1. All of the mutations were tested in tumor samples, except patient # 4 and # 5 whose peripheral blood samples were also available for germline mutation testing.
Table 1.
Summary of lung cancer patients with dual or multiple EGFR mutations containing primary EGFR T790M mutations.
| Patient # | Mutations | Age | Sex | Ethnicity | Pk Yrs/quit Yrs |
Histology | Stage at Diagnosis |
Metastasis | Family History | Other Cancers |
Germline Mutation |
Treatment History | TTP on EGFR TKI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | G719S [18]; T790M [20] |
51 | F | Caucasian | 0 | Adenocarcinoma | IV/T4N2M1 | Lungs, Skeletal | F: Lung Ca (nS), pA: Lung Ca (nS), pU: Lung Ca (nS) | None | NA | Palliative radiation, then lost to f/u, EGFR TKI treatment history unavailable | Unavailable |
| 2 | [del 19]; T790M [20] |
71 | M | Caucasian | 0 | Adenocarcinoma | IV/T2N3M1 | Left choroid, Skeletal, Adrenals | B: “Bone cancer” | None | NA | Taxotere/Carboplatin × 2 cycles, discontinued due to presumed Taxotere reaction → Alimta/Carboplatin × 1 discontinued due to Carboplatin reaction→ Alimta × 3 cycles →Erlotinib × 1.5 months → Gemzar × 1 | 1.5 months |
| 3 |
T790M [20]; L858R [21] |
62 | F | Caucasian | 0 | Bronchioalveolar Carcinoma | IV/T2N0M1 | Bilateral lungs | S: Lung Ca (nS), M: Lung Ca (S), F: Lung Ca (S) | SCC of skin | NA | Multiple wedge resections → Erlotinib for more than 5 years by now | > 5 years |
| 4 |
T790M [20]; L858R [21]; [del 19] |
53 | F | Caucasian | 0 | Adenocarcinoma | IIIA/T4N0M0 | None | F: Lung Ca (S), B: Glioblastoma, M: Uterine Ca, pU: H+N Ca (S), mGF: Colon Ca, mA: Breast Ca, mC: Breast Ca | Papillary thyroid carcinom a | No | Carbo/Taxotere × 6 cycles, stereotactic XRT, no evidence of disease to date | No TKI initiated to date |
| 5 (proband) |
T790M [20]; L858R [21] |
34 | F | Caucasian | 0 | Adenocarcinoma | IV/T4N3M1 | Skeletal, Liver, Pulmonary | See family Pedigree | None | Yes | Erlotinib × 1 month → Cetuximab/Cis/Alimta × 1 month | 1 month |
Abbreviation Legend: F – Father, M – Mother, B – Brother, S – Sister, GF – Grand Father, GM – Grandmother, A – Aunt, U – Uncle, p – Paternal, m – Maternal, Pk-Pack, TTP-Time to Progression, TKI-Tyrosine Kinase Inhibitor, nS – Never Smoker, S – Smoker
Case of a Germline EGFR T790M Mutation in a Caucasian Female
A 34 year-old never-smoking Caucasian female presented to local emergency room in July 2009 for a persistent cough. The chest x-ray showed a large right-sided pleural effusion and pathology from the pleural fluid revealed metastatic adenocarcinoma of the lung. A PET/CT revealed extensive hyper-metabolic activity in the pulmonary parenchymal, lymph nodes (right hilar, precarinal, right supraclavicular), and multiple liver and osseous metastases (Figure 1A). At the time of initial treatment, the EGFR mutation T790M had not yet been identified, and her poor performance status prevented initial chemotherapy administration. She was therefore started empirically on Erlotinib monotherapy with close monitoring. After one month of erlotinib treatment, her performance status had improved, but the dyspnea was worse and a repeat CT confirmed disease progression (Figure 1B and 1C). She was taken off erlotinib and started on cetuximab, cisplatin and alimta. Unfortunately, she was admitted to hospital after one cycle of treatment due to progressive dyspnea; and was unable to tolerate further treatment and entered into hospice. Sequencing of her tumor specimen obtained prior to treatment revealed dual mutations of both EGFR T790M and L858R (Figure 2 A and 2B). Mutation analysis of her peripheral blood mononuclear cells also identified a germline T790M mutation, with equivalent heights of the mutant and wild-type peaks (Figure 2C). The proband’s family pedigree is presented (Figure 3).
Figure 1.
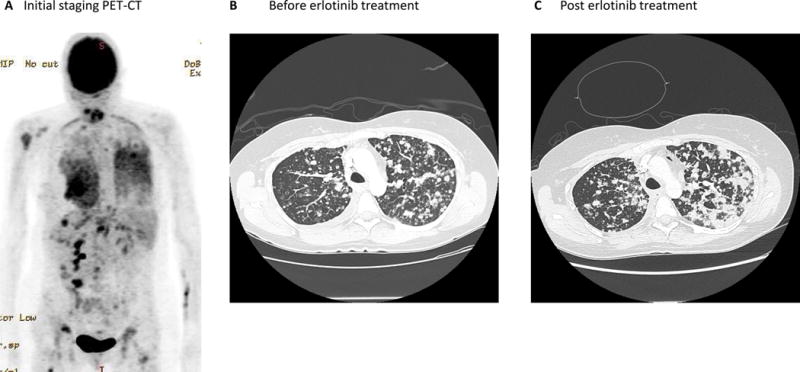
PET-CT and CT scans of proband patient with germline EGFR T790M mutation.
Figure 2.
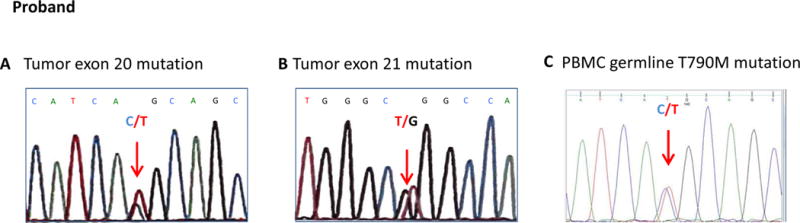
The results from PCR sequencing on proband’s tumor sample (A and B) and peripheral blood cells (C)
Figure 3.
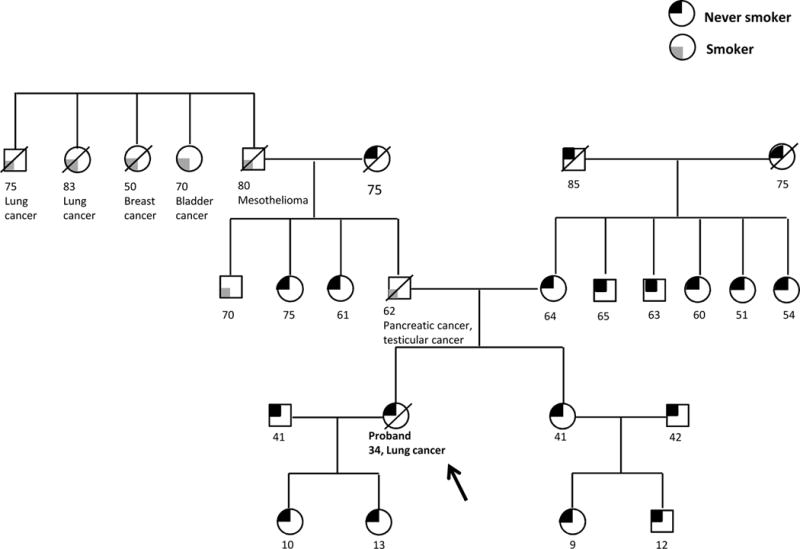
Pedigree of family with germline T790M mutation. Age, smoking history and other cancer history are recorded.
Discussion
The occurrence of germline EGFR T790M mutations is a rare event and has only been reported in case reports.5,6. These cases have been predominantly identified in Caucasian females with never-smoking histories and adenocarcinoma histology. Our case report is consistent with this clinical presentation. From the literature, about 73% of lung cancers that arise in patients with germline EGFR T790M mutations appear to also carry second EGFR mutations5. One hypothesis suggests that germline T790M mutation by itself may be a weak oncogene that requires a secondary mutation to potentiate cancer development5. Among the secondary mutations, concurrent L858R mutations are the most common5. To evaluate this, we interrogated our lung cancer database of 427 patient samples that had been genotyped for EGFR mutations. 3% (12/427) of patients were found to carry dual or multiple EGFR mutations before EGFR TKI treatment and 5 out of these 12 patients carried primary de novo T790M mutation. All of the patients who had a primary de novo EGFR T790M mutation had a concurrent second mutation. The clinical and demographic features of these 5 patients who carried primary EGFR T790M are summarized in Table 1. The proband patient reported in our case report is listed as patient #5 in the Table. The sequencing electropherogram of other 4 patients were shown in Figure 4. Interestingly, patients #1, #2 and #3 showed almost identical heights of peak in the mutant and non-mutant alleles, suggesting the likelihood of germline mutations. Unfortunately, we are unable to confirm the presence of germline mutations due to the unavailability of blood or normal tissue specimens in these patients. The sequencing data of patient #4 showed different heights of peak in the mutant and non-mutant alleles. The peripheral blood sample from this patient (#4) was available, which did not identify germline T790M mutation (data not shown). Four out of five patients with dual mutations containing primary de novo T790M had family histories of lung cancer, although some of the family members were smokers. Among those five patients who had primary de novo EGFR T790M mutations in addition to sensitive EGFR mutations, three patients received EGFR TKI treatments (Table 1). Two patients developed disease progression after 1–1.5 months of EGFR TKI treatment. The third patient had multiple wedge resections of her cancers and is stable with good disease control for over 5 years on erlotinib therapy. AlthoughT790M mutations have most commonly developed as a resistance mechanism after TKI treatment, rare cases of de novo T790M mutations have been reported in the literature11–13. Studies have suggested that EGFR T790M mutation might be present in small populations of tumor cells before EGFR TKI treatment, and the tumor cells harboring the T790M mutation are likely enriched after drug treatment12. Consistent with this suggested theory, our data demonstrated that primary de novo EGFR T790M mutation are presented with high frequency (5/12; 42%) in patients carrying dual or multiple EGFR mutations.
Figure 4.
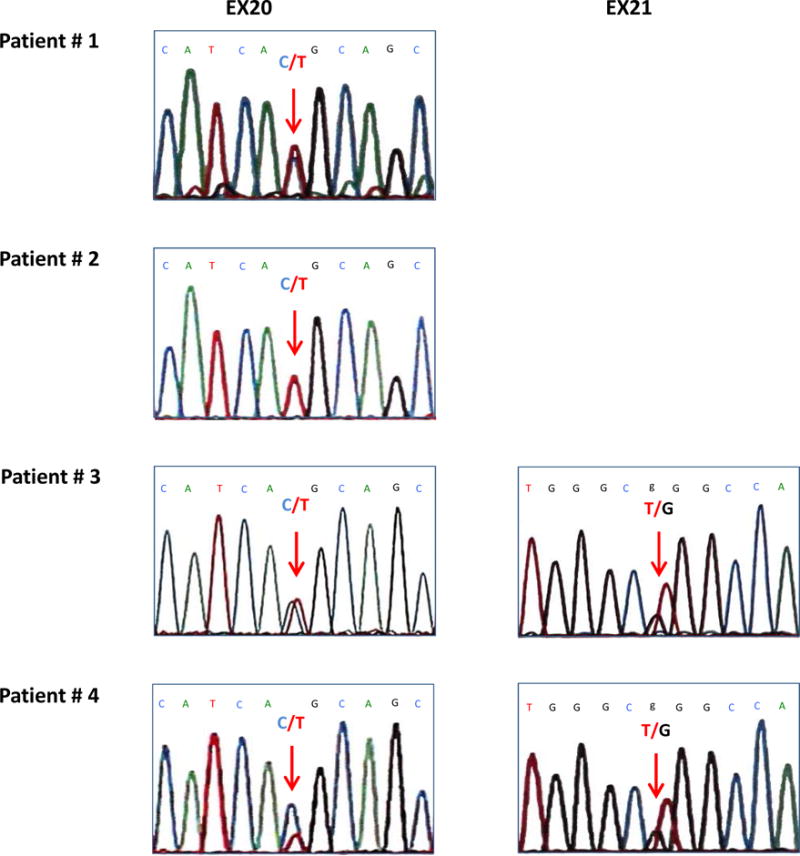
The results from PCR sequencing on additional patients who carried primary EGFR T790M mutation on patients’ tumor samples.
Several groups in Asia have reported small subsets of NSCLC patients with dual EGFR mutations7,8,14. It was estimated that complex mutations occurred in 13–18% of Asian patients with EGFR mutations15,16. Our study found similar findings, demonstrating that 12 of 55 patients (22%) carried dual or multiple EGFR mutations. It has been hypothesized that since these dual mutations are found in-cis that it confers a ‘second-hit’ growth advantage to the cancer cells14. In murine models, the expression of EGFR T790M has been reported to induce lung adenocarcinomas, suggesting that this mutation alone can be tumorigenic, although a control with wild-type EGFR overexpression is missing17. However, mice expressing the EGFR T790M transgene alone developed tumors with much longer latency than mice expressing either EGFR L858R+T790M or EGFR L858R alone17. Although more definitive studies are required, this is highly suggestive that primary de novo EGFR T790M mutations, whether somatic or germline, can lead to lung adenocarcinomas and that a secondary EGFR mutation further potentiates this and leads to an earlier onset of malignancy18.
From a clinical perspective, there are several interesting features observed in the cases of germline T790M mutations. To date, all cases have been reported in Caucasian patients except for two cases that were found in patients of East Indian descent19. From the cases where family histories were reported, the onset of lung cancer appears to occur at a younger age in each subsequent generation and appears to be inherited in an autosomal dominant pattern5,6. Our proband patient was diagnosed with lung cancer at age of 34 and the other case was reported in a 29 years old female, representing the two youngest patients in the literature5. This acceleration of disease onset in patients with younger ages in subsequent generations might due to anticipation; a phenomenon that has been described in inherited diseases such as Huntington disease and Fragile X syndrome, in which the disease arises at younger ages or with augmented severity in subsequent generations. DNA instability in subsequent generations is likely cause of anticipation. In addition, environmental factors may also play a role. Similar to sporadic EGFR mutations, germline T790M mutations are predominantly found in women. This might be explained by a growing body of evidence showing functional interactions between the estrogen and EGFR pathways20. Studies suggest that women have more altered activity in DNA repair compared to men and it is well documented that women that smoke are more prone to develop KRAS mutations21. Further studies are necessary to understand the roles of gender and biology of germline T790M mutation in lung cancer development.
EGFR T790M mutation was previously considered to be an acquired resistant mutation to EGFR TKI therapy. However our study along with previously published cases suggested that primary de novo EGFR T790M mutations may occur as high a frequency as 35–42% in patients with dual or multiple EGFR mutations, which support the theory that patients with EGFR mutation might harbor unseen T790M mutations at presentation and that the resistance mutation is only identified after clonal selection occurs after EGFR TKI therapy4,11,12.
In a separate issue, germline EGFR T790M mutations were reported to be present in approximately 50% of all patients with primary EGFR T790M, although this statistic was generated from a very limited number of patients due to the rarity of disease4. However, it is reasonable to consider performing germline testing in all patients with primary de novo EGFR T790M mutations. This would subsequently lead to potentially screening first-degree relatives of lung cancer patients with germline EGFR T790M mutations and monitoring them, given the increased risk of developing lung cancer.
Conclusion
We report a case of germline EGFR T790M mutation along with a case series of NSCLC patients with dual/multiple EGFR mutations. Primary de novo EGFR T790M mutation is found at a higher frequency in patients who carry dual or multiple EGFR mutations. Sensitive detection method such as next generation sequencing will be helpful in identifying these less frequent mutations. Although this occurs in a rare population of patients, it is important to identify these patients rapidly and enroll them onto clinical trials with 3rd generation TKIs or EGFR T790M specific targeted therapy. Further study is essential to further our understanding of this disease and its resistance mechanisms.
Supplementary Material
Supplementary Table 1. Summary of lung cancer patients with dual or multiple EGFR mutations excluding primary EGFR T790M mutations.
Clinical Practice Points.
We report a confirmed case of germline EGFR T790M mutation along with a case series of dual/multiple EGFR mutations in NSCLC patients with lung adenocarcinoma.
Primary or de novo EGFR T790M mutations are found at a higher frequency in patients who carry dual or multiple EGFR mutations.
Germline EGFR T790M mutations are rare but increase lung cancer susceptibility.
Screening relatives of lung cancer patients with germline EGFR T790M mutation maybe important given the increased risk of developing lung cancer.
Acknowledgments
Grant support: This study is supported by NIH–T32 Research Training in Academic Medical Oncology (Y.L. and C.V.P).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pao W. Defining clinically relevant molecular subsets of lung cancer. Cancer Chemother Pharmacol. 2006;58(Suppl 1):s11–5. doi: 10.1007/s00280-006-0310-x. [DOI] [PubMed] [Google Scholar]
- 2.Pao William, M VA, Politi Katerina A, Riely Gregory J, Somwar Romel, Zakowski Maureen F, Kris Mark G, Varmus Harold. Acquired Resistance of Lung Adenocarcinomas to Gefitinib or Erlotinib Is Associated with a Second Mutation in the EGFR Kinase Domain. Plos Medicine. 2005;2:227–235. doi: 10.1371/journal.pmed.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kobayashi Susumu, B TJ, Dayaram Tajhal, Jänne Pasi A, Kocher Olivier, Meyerson Matthew, Johnson Bruce E, Eck Michael J, Tenen Daniel G, Halmos Balázs. EGFR Mutation and Resistance of Non–Small-Cell Lung Cancer to Gefitinib. New England Journal of Medicine. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- 4.Oxnard GR, Miller VA, Robson ME, et al. Screening for germline EGFR T790M mutations through lung cancer genotyping. J Thorac Oncol. 2012;7:1049–52. doi: 10.1097/JTO.0b013e318250ed9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gazdar A, Robinson L, Oliver D, et al. Hereditary lung cancer syndrome targets never smokers with germline EGFR gene T790M mutations. J Thorac Oncol. 2014;9:456–63. doi: 10.1097/JTO.0000000000000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu HA, Arcila ME, Harlan Fleischut M, et al. Germline EGFR T790M mutation found in multiple members of a familial cohort. J Thorac Oncol. 2014;9:554–8. doi: 10.1097/JTO.0000000000000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toyooka Shinichi, K K, Mitsudomi Tetsuya. EGFR Mutation and Response of Lung Cancer to Gefitinib. New England Journal of Medicine. 2005;352:2136. doi: 10.1056/NEJM200505193522019. [DOI] [PubMed] [Google Scholar]
- 8.Tam Issan Yee-San, L EL-H, Tin Vicky Pui-Chi, Chua Daniel Tsin-Tien, Sihoe Alan Dart-Loon, Cheng Lik-Cheung, Chung Lap-Ping, Wong Maria Pik. Double EGFR mutants containing rare EGFR mutant types show reduced in vitro response to gefitinib compared with common activating missense mutations. Molecular Cancer Therapeutics. 2009;8:2142–2151. doi: 10.1158/1535-7163.MCT-08-1219. [DOI] [PubMed] [Google Scholar]
- 9.Bell Daphne W, G I, Okimot Ross A, Godin-Heymann Nadia, Sordella Raffaella, Mulloy Roseann, Sharma Sreenath V, Brannigan Brian W, Mohapatra Gayatry, Settleman Jeff, Haber Daniel A. Inherited susceptibility to lung cancer may be associated with the T790M drug resistance mutation in EGFR. Nature Genetics. 2005;37:1315–1316. doi: 10.1038/ng1671. [DOI] [PubMed] [Google Scholar]
- 10.Prudkin Ludmila, T X, Wistuba Ignacio I. Germ-Line and Somatic Presentations of the EGFR T790M Mutation in Lung Cancer. Journal of Thoracic Oncology. 2009;4:139–141. doi: 10.1097/JTO.0b013e3181915f92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piotrowska Z, Sequist LV. Epidermal Growth Factor Receptor-Mutant Lung Cancer: New Drugs, New Resistance Mechanisms, and Future Treatment Options. Cancer journal. 2015;21:371–7. doi: 10.1097/PPO.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 12.Inukai M, Toyooka S, Ito S, et al. Presence of epidermal growth factor receptor gene T790M mutation as a minor clone in non-small cell lung cancer. Cancer research. 2006;66:7854–8. doi: 10.1158/0008-5472.CAN-06-1951. [DOI] [PubMed] [Google Scholar]
- 13.Ayoola A, Barochia A, Belani K, et al. Primary and acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small cell lung cancer: an update. Cancer investigation. 2012;30:433–46. doi: 10.3109/07357907.2012.666691. [DOI] [PubMed] [Google Scholar]
- 14.Yokoyama Toshihiko, K M, Goto Yasuhiro, Fukui Takayuki, Yoshioka Hiromu, Yokoi Kohei, Osada Hirotaka, Imaizumi Kazuyoshi, Hasegawa Yoshinori, Shimokata Kaoru, Sekido Yoshitaka. EGFR point mutation in non-small cell lung cancer is occasionally accompanied by a second mutation or amplification. Cancer Science. 2006;97:753–759. doi: 10.1111/j.1349-7006.2006.00233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tam IY, Leung EL, Tin VP, et al. Double EGFR mutants containing rare EGFR mutant types show reduced in vitro response to gefitinib compared with common activating missense mutations. Molecular cancer therapeutics. 2009;8:2142–51. doi: 10.1158/1535-7163.MCT-08-1219. [DOI] [PubMed] [Google Scholar]
- 16.Huang SF, Liu HP, Li LH, et al. High frequency of epidermal growth factor receptor mutations with complex patterns in non-small cell lung cancers related to gefitinib responsiveness in Taiwan. Clinical cancer research : an official journal of the American Association for Cancer Research. 2004;10:8195–203. doi: 10.1158/1078-0432.CCR-04-1245. [DOI] [PubMed] [Google Scholar]
- 17.Regales Lucia, B MN, Gong Yixuan, Politi Katerina, Sawai Ayana, Le Carl, Koutcher Jason A, Solit David B, Rosen Neal, Zakowski Maureen F, Pao William. Development of New Mouse Lung Tumor Models Expressing EGFR T790M Mutants Associated with Clinical Resistance to Kinase Inhibitors. Plos One. 2007;2:1–10. doi: 10.1371/journal.pone.0000810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chmielecki J, Foo J, Oxnard GR, et al. Optimization of dosing for EGFR-mutant non-small cell lung cancer with evolutionary cancer modeling. Science translational medicine. 2011;3:90ra59. doi: 10.1126/scitranslmed.3002356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girard N, Lou E, Azzoli CG, et al. Analysis of genetic variants in never-smokers with lung cancer facilitated by an Internet-based blood collection protocol: a preliminary report. Clin Cancer Res. 2010;16:755–63. doi: 10.1158/1078-0432.CCR-09-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stabile LP, Lyker JS, Gubish CT, et al. Combined targeting of the estrogen receptor and the epidermal growth factor receptor in non-small cell lung cancer shows enhanced antiproliferative effects. Cancer Res. 2005;65:1459–70. doi: 10.1158/0008-5472.CAN-04-1872. [DOI] [PubMed] [Google Scholar]
- 21.Ben Aissa A, Mach N. Is lung cancer in women different? Rev Med Suisse. 2012;8:1108–11. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Summary of lung cancer patients with dual or multiple EGFR mutations excluding primary EGFR T790M mutations.


