Abstract
Case series
Patients: Male, 48 • Male, 60 • Male, 63 • Male, 69 • Male, 68 • Female, 63
Final Diagnosis: Esophageal cancer
Symptoms: None
Medication: —
Clinical Procedure: —
Specialty: Oncology
Objective:
Rare disease
Background:
Patients with esophageal achalasia are considered to be a high-risk group for esophageal carcinoma, and it has been reported that this cancer often arises at a long interval after surgery for achalasia. However, it is unclear whether esophageal carcinoma is frequent when achalasia has been treated successfully and the patient is without dysphagia. In this study, we reviewed patients with esophageal carcinoma who were detected by regular follow-up after surgical treatment of achalasia.
Case Report:
Esophageal cancer was detected by periodic upper GI endoscopy in 6 patients. Most of them had early cancers that were treated by endoscopic resection. All 6 patients had undergone surgery for achalasia and the outcome had been rated as excellent or good. Annual follow-up endoscopy was done and the average duration of follow-up until cancer was seen after surgery was 14.3 years (range: 5 to 40 years). Five patients had early cancer. Four cases had multiple lesions.
Conclusions:
In conclusion, surgery for achalasia usually improves passage symptoms, but esophageal cancer still arises in some cases and the number of tumors occurring many years later is not negligible. Accordingly, long-term endoscopic follow-up is needed for detection of malignancy at an early stage.
MeSH Keywords: Esophageal Achalasia, Esophageal Neoplasms, Follow-Up Studies
Background
Patients with esophageal achalasia are considered to be a high-risk group for esophageal carcinoma, and it has been reported that this cancer often arises at a long interval after surgery for achalasia [1,2]. However, it is unclear whether esophageal carcinoma is frequent when achalasia has been treated successfully and the patient is without dysphagia. In this study, we reviewed patients with esophageal carcinoma who were detected by regular endoscopic follow-up after surgical treatment of achalasia.
Case Reports
Thirty-two patients who were treated for esophageal achalasia at our hospital were underwent long-term and periodic upper GI endoscopic follow-up. The mean follow-up period was 11.1 years (range 1 to 40 years) in these 32 patients. Esophageal squamous cell carcinoma was detected by periodic upper GI endoscopy in 6 patients and the incidence of esophageal cancer was 18%. All 6 patients had undergone surgery [3,4] for achalasia and the outcome had been rated as excellent or good [5]. Annual follow-up endoscopy was done and the average duration of follow-up until cancer was seen after surgery was 14.3 years (range: 5 to 40 years). Five patients had early cancer [6] (pT1a-EP∼MM) and the tumor type was 0-IIc or 0-IIb, and 1 had T2 cancer and type was 0-Is (Table 1).
Table 1.
Clinical characteristics of the patients.
| Age/Sex | Type/Grade of Achalasia | Operation | Passage | Duration of cancer (yrs) | Number of lesions | Location | Tumor Type | Tumor Depth | Tumor Size (mm) | Treatment for Cancer |
|---|---|---|---|---|---|---|---|---|---|---|
| 48/Male | F/II | Heller-Dor | Excellent | 5 | 1 | Lt | 0-IIb | LPM | 6 | EMR |
| 60/Male | St/II | Heller-Dor | Excellent | 6 | 2 | Mt | 0-IIc | EP | 30 | CRT |
| 2 | Mt | 0-IIc | EP | 24 | ESD | |||||
| 63/Male | St/II | Heller-Dor | Excellent | 40 | 2 | Mt | 0-IIc | MM | 23 | ESD |
| Mt | 0-IIc | EP | 8 | ESD | ||||||
| 69/Male | F/II | Heller-Dor | Good | 27 | 2 | Mt | 0-IIc | EP | 18 | Esophagectomy |
| Lt | 0-Is | MP | 17 | Esophagectomy | ||||||
| 68/Male | F/II | Fundic patch | Good | 23 | 3 | Mt | 0-IIc | EP | 30 | ESD |
| Mt | 0-IIc | EP | 24 | ESD | ||||||
| Lt | 0-IIc | EP | 10 | ESD | ||||||
| 63/Female | St/I | Heller-Dor | Excellent | 14 | 1 | Mt | 0-IIc | EP | 12 | ESD |
Case 1
The patient was a 48-year-old man. The Heller-Dor operation was done for Grade II achalasia [7] and an excellent outcome was achieved according to Payne’s criteria [5]. Endoscopic follow-up was performed annually and a 0–IIb lesion was detected in the lower esophagus at 5 years after surgery. EMR was performed. Subsequently, there has been no recurrence or metachronous cancer.
Pathological findings: The depth of tumor invasion was T1a-EP (Tis) with ly0 and v0. Thickening of the epithelium and an increase of blood vessels in the mucosal or submucosal layers were seen.
Case 2
The patient was a 60-year-old man. The Heller-Dor operation was performed for Grade II achalasia when he was 36 years old and postoperative outcome was judged to be excellent. Six years later, 0–IIc early cancer was diagnosed by annual follow-up endoscopy. This was treated with chemoradiation and the lesion showed a complete response. Follow-up endoscopy was continued, and another 0–IIc early cancer was detected in the lower esophagus at 24 years after the operation for achalasia. We diagnosed metachronous multiple esophageal cancer and performed ESD to remove the lesion. Pathological findings revealed the depth of tumor invasion was T1a-EP (Tis) with ly0 and v0. There was epithelial thickening, as well as cellular infiltration and scarring of the mucosal and submucosal layers.
Case 3
The patient was a 63-year-old man. Gastric patch surgery was done for Grade II achalasia 39 years previously. Because dysphagia occurred again at 25 years after the first operation, the Heller-Dor operation was performed. The outcome was excellent and this status was maintained. Follow-up endoscopy was done every year. Forty years after his first operation, synchronous esophageal cancers were detected in the middle and lower esophagus by annual endoscopy. The lesions were diagnosed as early cancer, and ESD was performed.
Pathological findings: The depth of invasion was T1a-MM (ly0 and v0) for lesion 1 and T1a-LPM (ly0 and v0) for lesion 2. Thickening of the epithelium and increased vascularity of the mucosal or submucosal layer were seen at the sites of both lesions.
Case 4
The patient was a 69-year-old man. The Heller-Dor operation was performed for Grade II achalasia when he was 42 years old and postoperative outcome was judged to be good. Twenty-seven years later, 0-Is cancer and 0–IIc early cancer was diagnosed in the middle and lower esophagus by annual follow-up endoscopy (Figure 1A–1D). This was treated with esophagectomy. Pathological findings revealed the depth of tumors invasion were T2 and T1a-EP (Tis) with ly0 and v0. There was epithelial thickening, as well as cellular infiltration and scarring of the mucosal and submucosal layers (Figure 2A, 2B).
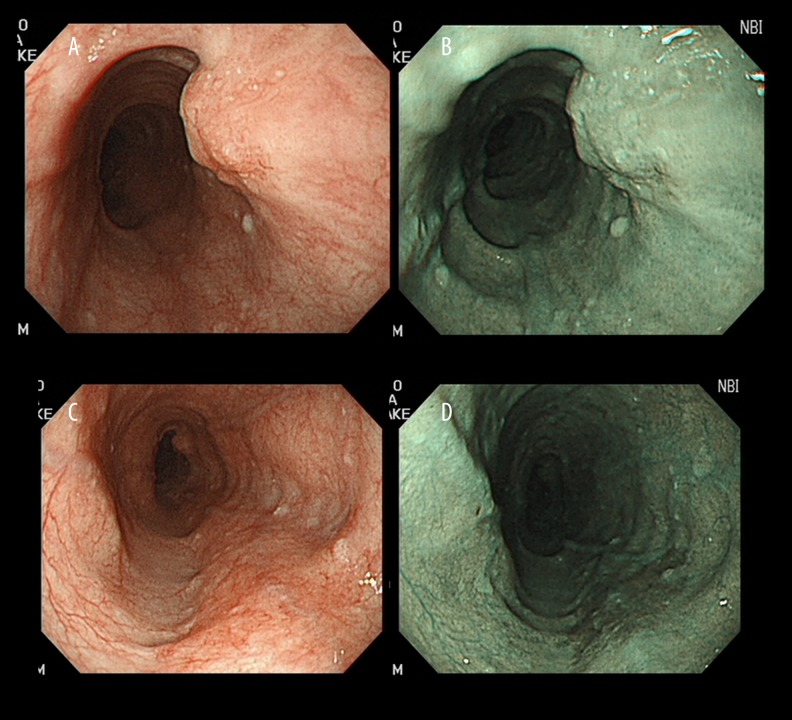
Figure 1.
(A) Case 4. Conventional endoscopy shows a protruding lesion (0–Is) located 37 cm from the incisors (lesion 1). (B) There are few brownish areas at the lesion on narrow-band imaging. (C) Case 4. Conventional endoscopy shows a flat lesion (0–IIb) located 30 cm from the incisors. (D) There is a brownish area at the lesion on narrow-band imaging (lesion 2).
Figure 2.
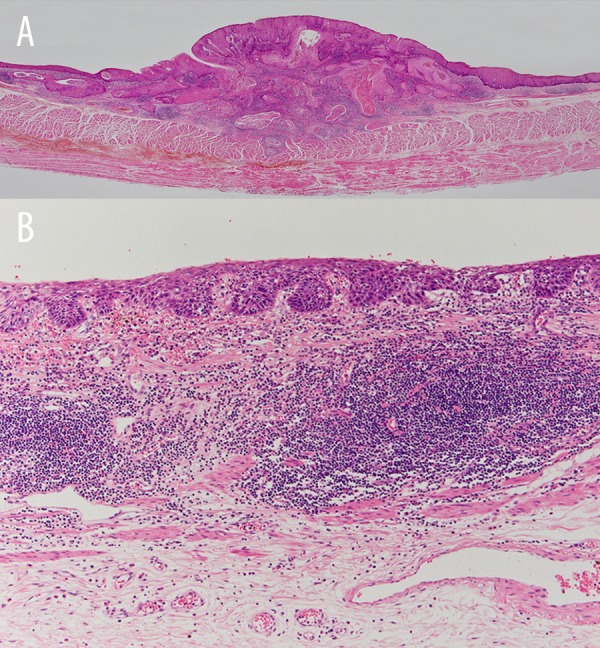
(A) Case 4. Microscopic findings. Tumor depth was T2, ly0, v0 for lesion (lesion 1). (B) T1a-LPM, ly0, v0 for lesion 2 (lesion 2). Epithelial thickening and increased vascularity in the mucosal or submucosal layers were seen at both lesions.
Case 5
The patient was a 68-year-old man. Fundic patch surgery was done for Grade II achalasia 45. The outcome was excellent and this status was maintained. Follow-up endoscopy was done every year. Twenty-three years after the operation, synchronous esophageal cancers were detected in the middle and lower esophagus by annual endoscopy. The lesions were diagnosed as early cancer, and ESD was performed.
Pathological findings showed that the depth of invasion was T1a-EP (ly0 and v0) for all lesions. Thickening of the epithelium and increased vascularity of the mucosal or submucosal layer were seen at the sites of both lesions.
Case 6
The patient was a 63-year-old woman. The Heller-Dor operation was performed for Grade I achalasia when she was 49 years old and postoperative outcome was judged to be excellent. Fourteen years later, 0–IIc early cancer was diagnosed in the middle esophagus by annual follow-up endoscopy (Figure 3A–3C). This was treated with ESD. Pathological findings showed that the depth of tumors invasion were T1a-EP (Tis) with ly0 and v0. There was epithelial thickening, as well as cellular infiltration and scarring of the mucosal and submucosal layers (Figure 4).
Figure 3.
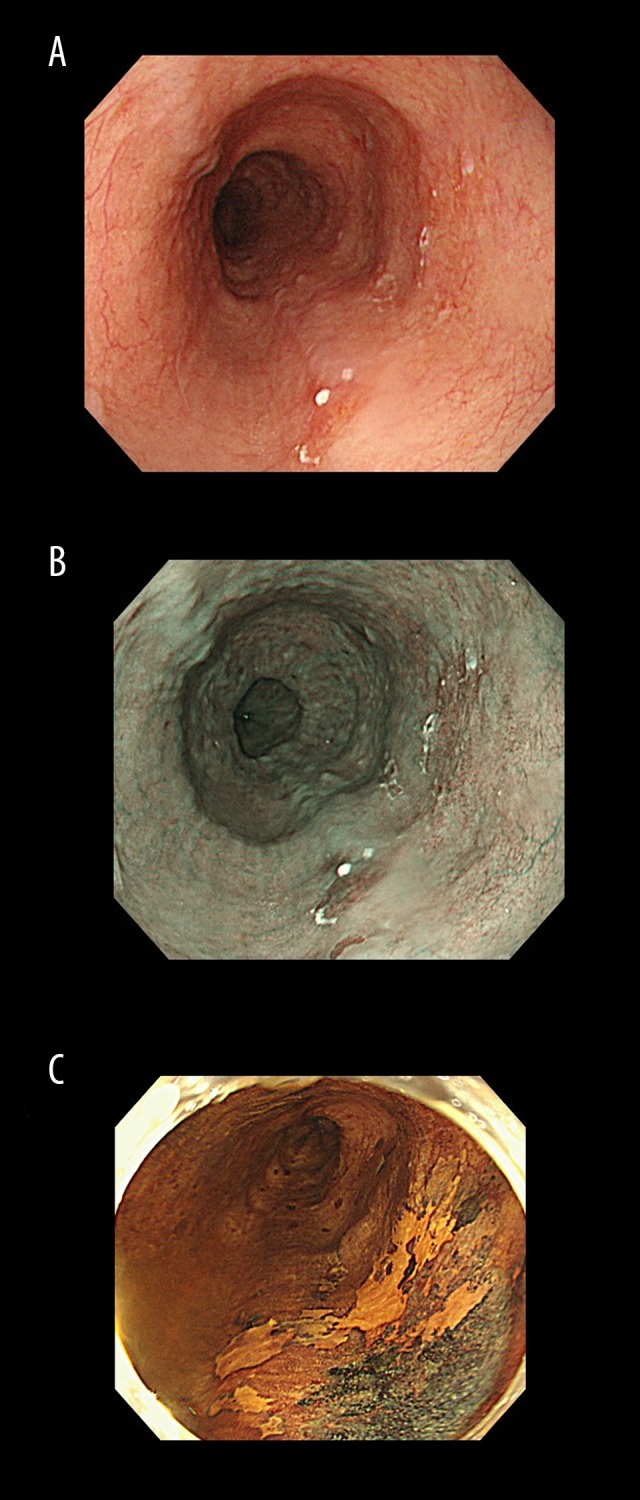
(A) Case 6. Endoscopic findings. Conventional endoscopy shows slightly depressed lesion (0-IIc) at 29–30 cm from the incisor teeth. (B) Case 6. There is a brownish area at the lesion on narrow-band imaging. (C) Case 6. Chromoendoscopy reveals that the lesion is not stained by iodine.
Figure 4.
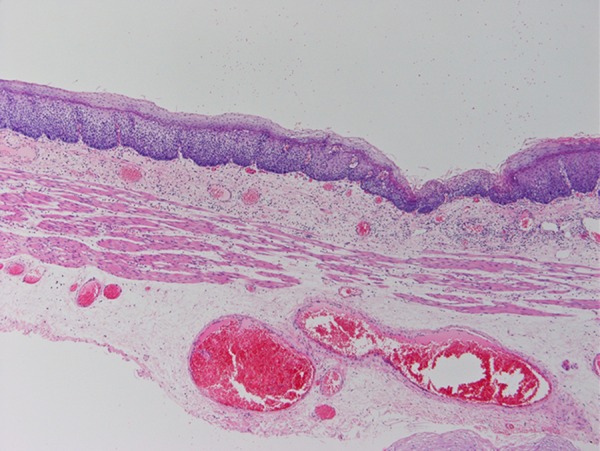
Case 6. Pathological findings: The depth of tumors invasion were T1a-EP (Tis) with ly0 and v0. There was epithelial thickening, as well as cellular infiltration and scarring of the mucosal and submucosal layers.
Discussion
In patients with esophageal achalasia, esophageal carcinoma occurs at a high frequency, so we need to be aware of the risk of this cancer when performing treatment and follow-up of achalasia. The prevalence of esophageal cancer was 18% among of our follow-up patients. In previous reports, the prevalence of esophageal cancer has ranged from 2.3 to 9.2% [8–10], and it has been reported that the incidence rate of this cancer is high during follow-up after treatment for achalasia.
There have been few reports on the results of follow-up after curative surgery for achalasia. It was reported that the frequency of esophageal cancer decreases after surgery for achalasia [11], but it was also reported that incidence of this cancer after surgery was 2.9% [12]. Therefore, we consider that surgery for achalasia does not necessarily decrease the risk of esophageal cancer. Chino et al. reviewed a series of reports and concluded that it takes 17–21.5 years for occurrence of esophageal cancer after the onset of achalasia symptoms. Arima et al. reported that 15.1 years elapsed until the occur-rence of esophageal cancer after surgery for achalasia, while Leeuwenburgh et al. found cancer at 11 years after the operation. These reports indicate that esophageal cancer can occur many years after the initial detection or treatment of achalasia.
The Heller-Dor operation has been the standard surgical treatment for achalasia at our hospital since 1985, and we attempt esophageal preservation before performing esophagectomy in patients with advanced achalasia [13]. Good results have been reported for this procedure. Bonavina et al. [14] studied the results of the Heller-Dor operation and found that the outcome was excellent-to-good in 92.8% by Payne’s criteria [5]. Similarly, over 90% of patients had an excellent outcome at our hospital. Thus, few patients complain of passage symptoms after surgery, and all of our patients who developed esophageal cancer after achalasia surgery had an excellent result by Payne’s criteria. This suggests that the potential for malignant transformation persists even after surgery improves passage symptoms. Because we performed regular follow-up endos-copy, the cancer was detected at an early stage in all of our patients. This suggests that surveillance by follow-up endos-copy to detect esophageal cancer is an important aspect of postoperative management for achalasia.
Three of these 6 patients were chronic alcohol drinkers and 3 of them had a smoking habit, and it is reasonable to assume that there was some influence of these living habits on the occurrence of esophageal cancer in these patients.
Conclusions
Surgery for achalasia usually improves passage symptoms. After surgery, esophageal cancer arose in some cases, with a number of tumors occurring many years later. Accordingly, long-term endoscopic follow-up is useful for detection of malignancy at an early stage.
References:
- 1.Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: A prospective study. Am J Gastroenterol. 2010;105:2144–49. doi: 10.1038/ajg.2010.263. [DOI] [PubMed] [Google Scholar]
- 2.Chino O, Kise Y, Ishii A, et al. Basaloid squamous carcinoma of the esophagus developed from achalasia: Report of a case. Esophagus. 2008;5:157–62. [Google Scholar]
- 3.Dor J, Humbert P, Dor V, Figarella J. L’intéret de la technique de Nissen modifiée dans la prevention de reflux aprés cardiomyotomie extramuquense de Heller. Mem Acad Chir. 1962;88:877–83. [in French] [Google Scholar]
- 4.Jekler J, Lhotka J. Modified Heller procedure to prevent postoperative re-flux esophagitis in patients with achalasia. Am J Surg. 1967;113:251–54. doi: 10.1016/0002-9610(67)90233-4. [DOI] [PubMed] [Google Scholar]
- 5.Payne WS, King RM. Treatment of achalasia of the esophagus. Surg Clin N Am. 1983;63:963–70. doi: 10.1016/s0039-6109(16)43097-5. [DOI] [PubMed] [Google Scholar]
- 6.Japan esophageal society . Japanese classification of esophageal cancer. 11th ed. Tokyo: Kanehara; 2015. [Google Scholar]
- 7.Japan esophageal society . Descriptive rules for achalasia of the esophagus. 4th ed. Tokyo: Kanehara; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandler RS, Ekbom A, Eisen GM, et al. The risk of esophageal cancer in patients with achalasia. JAMA. 1995;271:1359–62. [PubMed] [Google Scholar]
- 9.Streitz JM, Ellis FH, Gibb SP, et al. Achalasia and squamous cell carcinomaof the esophagus: Analysis of 241 patients. Ann Thorac Surg. 1995;59:1604–9. doi: 10.1016/0003-4975(94)00997-l. [DOI] [PubMed] [Google Scholar]
- 10.Loviscek LF, Cenoz MC, Badaloni AE, et al. Early cancer in achalasia. Dis Esophagus. 1998;11:239–47. doi: 10.1093/dote/11.4.239. [DOI] [PubMed] [Google Scholar]
- 11.Wychulis AR, Woolam GL, Anderson HA, et al. Achalasia and carcinoma of the esophagus. JAMA. 1971;215:1638–41. [PubMed] [Google Scholar]
- 12.Arima M, Kouzu T, Arima H, et al. Soperficial esophageal cancer (m1) associated with postoperative achalasia of the esophagus, Report of a case. Stomach and Intestine. 1995;30:1379–85. [Google Scholar]
- 12.Ota M, Ide H, Nakamura T, et al. Esophagus-preserving surgery for advanced end-stage achalasia. Esophagus. 2004;1:127–30. [Google Scholar]
- 14.Bonavina L, Nosadini A, Bardini R, et al. Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg. 1992;127:222–26. doi: 10.1001/archsurg.1992.01420020112016. [DOI] [PubMed] [Google Scholar]