Abstract
Aim
The use of microsurgical technique and loupes magnification as a support to traditional surgery can help surgical performance and prevent complications in thyroid surgery.
Patients and methods
Between January 2004 and December 2014, 782 patients with thyroid diseases were operated by our team with microsurgical technique and loupes magnification 4.5x. All patients had pre and postoperative vocal cords assessment and calcemia and the collected data were analysed.
Results
Among the 782 patients, only six patients (0.77%) had unilateral vocal fold immobility treated with medical therapy, phoniatric and neck physiotherapy. All six patients showed complete laryngeal recovery of motility 6/8 weeks after treatment. There were not cases of permanent monolateral or bilateral vocal cord palsy. In 84 patients there were signs and symptoms of hypocalcemia. In 81 patients (10.36%) the restoring of biochemical parameters and the resolution of symptoms occurred between 2 and 6 weeks and in 3 cases (0.38%) there was permanent hypocalcemia more than six months.
Conclusion
The use of microsurgical technique and loupes magnification in thyroid surgery are safety and effective procedures, that require an appropriate training in reconstructive microsurgery, but may significantly reduce post-operative complications. Here, we report for the first time the largest series of thyroid surgery performed with the use of microsurgical technique and loupes magnification, analysing the postoperative morbidity. In view of our results, we suggest the routine use of 4.5X loupes and microsurgical technique in thyroid surgery.
Keywords: Microsurgery, Loupes magnification, Thyroid, Hypocalcemia, Recurrent laryngeal nerve injury, Vocal cord palsy, Hypoparathyroidism
Introduction
Thyroid surgery has been characterized in the last years by significant innovations which are well codified and standardized. Although the mortality rate is remarkably reduced (0.065%) compared to the early 1900s (1), thyroid surgery is still not free from risk of complications such as those related to the injury of laryngeal nerves and parathyroid glands (2, 3). The two most common early complications of thyroid surgery are hypocalcemia (20–30%) and recurrent laryngeal nerve injury (5–11%) (2). Bilateral recurrent nerve paralysis resulting in adduction of the vocal cords is a rare life-threatening complication occurring in less than 0.1% of cases that requires emergency management (2). To prevent or reduce the incidence of these events it is of primary importance an excellent anatomical knowledge of the neck as well as the application of a meticulous surgical technique (4–6). Thus, the rate of these complications is directly related to the extent of thyroidectomy and to a radical thyroid excision (without macroscopic thyroid residual) as well as to the surgeon’s experience (7).
Microsurgical technique with the use of microscope is usually performed to make microvascular anastomosis of limb replantation and free flap in many surgical specialities (8–10). Starting from 1975, and to the best of our knowledge, only few works have been published about the use of microsurgical technique and magnification as a support to traditional thyroid surgery; interestingly, though, the results show that such treatment approach helps surgical performance and prevents complications, especially in reinterventions, thyroiditis, cancer and cervical lymphadenectomy (4, 11–19). Therefore, to better support microsurgical technique and magnification in thyroid surgery it is important to present additional studies with a larger number (n) of patients.
Our experience in many areas of general surgery and reconstructive microsurgery (8, 20–27), has prompted us to consider the benefits related to the application of microsurgical technique and the use of loupes in neck surgery. Therefore, the aim of the present retrospective study was to review ten years of thyroid surgery performed with use of loupes magnification and microsurgical technique by our team in a single institution and analyze the outcomes with respect to those reported in the literature with other surgical techniques.
Patients and methods
Patient enrollement
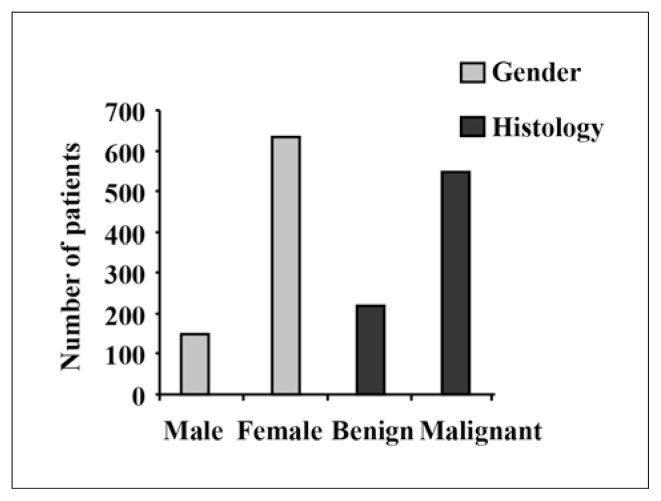
During the ten years study period, from January 2004 to December 2014, a group of 782 patients (633 females and 149 males; age range: 22–82) (Figure 1) was identified as eligible to undergoing surgery for thyroid disease at the Department of General Microsurgery, “Fabia Mater” Hospital in Rome, Italy. Informed consent was obtained by each patient for both the operation with loupes and data analysis; the clinical protocol for this study was approved by the local Independent Ethical Committee of the Institution. Clinical information was collected on sex, age, thyroid disease, and histology. In particular, the incidence of complications related to injuries of inferior laryngeal nerves and parathyroid glands after surgery was analised.
Fig. 1.
Graph showing the gender and histology by patients number.
Thyroid surgery
In all patients, thyroid surgery was performed with microsurgical technique and loupes magnification 4.5X with focal range of about 17 inches. Surgery was carried out by the same microsurgical team with a high level of expertise in thyroid surgery and microsurgical technique. There must be emphasized that all the two microsurgeons used loupes magnification 4.5× not only during the dissection of the recurrent laryngeal nerve and parathyroid glands but for the entire period of surgery, that is, from the skin incision until the final suture. The operators wear also a led coaxial light to increase operative field brightness. The operative time was between 60 and 180 minutes (mean 90 minutes). The mean postoperative stay was 3 days (range 2–5 days) and the mean follow-up was 20 days (range 14–180 days). Thanks to the results obtained (more than 50 thyroidectomies per year), our Institution has been accredited in 2014 as the Reference Center of the Italian Association of Endocrine Surgery Unit (www.clubdelleuec.it) for the surgical treatment of thyroid diseases.
Pre- and postoperative evaluations
All patients had pre and postoperative mirror vocal cords assessment. To improve the quality of the assessment, all patients had pre and postoperative (about 4–8 weeks) fiber-optic naso-laryngoscopy combined with videostrobolaryngoscopy and voice evaluation (28, 29). All patients received, from the day after surgery until normalization of serum calcium, 1gram (gr) of calcium carbonate and 1microgram (mcg) of vitamin D supplement for each day; serum calcium and ionized calcium have been dosed at day 1, 2 and 7 after surgery. We consider permanent hypocalcemia a low serum dose of calcium after six months to surgery. We did not record cases of operative or postoperative mortality in our series.
Results
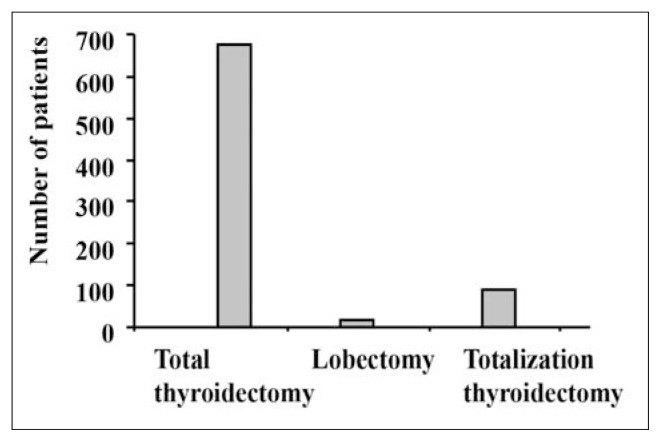
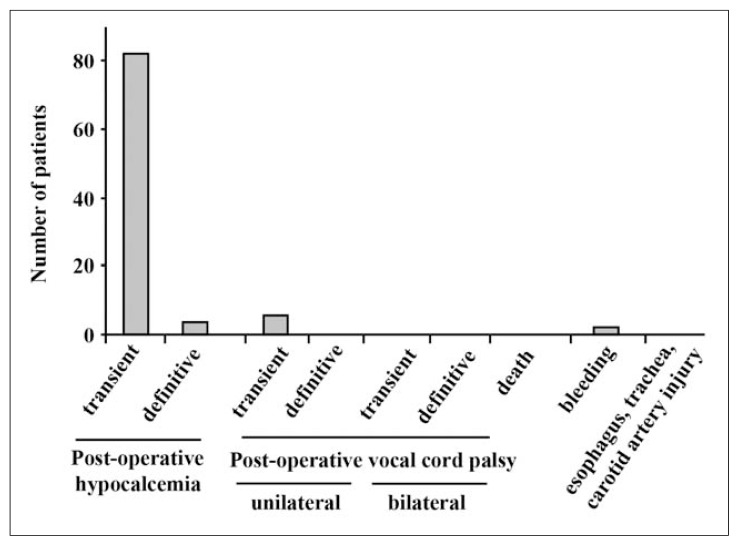
The 782 patients underwent surgery for benign disease (n=548, 70%) and neoplastic disease (n=234, 30%) (Figure 1). The diagnosis of the benign disease included multinodular goiter, toxic multinodular goiter, Graves’ disease and thyroiditis, while the diagnosis of the neoplastic diseases was differentiated tumor (n=218), medullary carcinoma (n=3), insular carcinoma (n=2), anaplastic cancers (n=2) and tumor of unknown malignant potential (n=9) (Table 1). The patients underwent total thyroidectomy (n=676), lobectomy (n=16) and totalization (also known as completation) thyroidectomy (n=90) (Figure 2), of which 43 unilateral and 47 bilateral for a total of 1505 “nerves at risk”. Totalization thyroidectomy was applied in 32 patients (out of the 90), already treated in other hospitals, for neoplasms arising within residual thyroid. In 75 patients with thyroid cancer at high risk and/or enlargement of cervical lymphadenopathy, the thyroidectomy was associated with lymphadenectomy (central and lateral compartment). There were no cases of operative or postoperative deaths in our series. Due to the clinical relevance of such microsurgical approach, compared to more traditional ones, we paid particular attention to the incidence of complications related to injuries of inferior laryngeal nerves and parathyroid glands. Indeed, the two most common early complications of thyroid surgery are hypocalcemia (20–30%) and recurrent laryngeal nerve injury (5–11%) (2). Bilateral recurrent nerve paralysis resulting in adduction of the vocal cords is a rare life-threatening complication occurring in less than 0.1% of cases that requires emergency management (2). In our series there were no cases of unilateral or bilateral permanent vocal cord palsy (Figure 3) except for one patient with preoperative unilateral vocal cord palsy (indirect laringoscopy) without modification of voice quality. In this case, we performed total thyroidectomy and resection of the recurrent nerve infiltrated by high risk carcinoma. In the same time it was applied microsurgical reinnervation by ansa cervicalis (branch innervating the sternothyroid muscle) to recurrent laryngeal nerve, as reported (30). At 6-month follow-up there were no phoniatric alterations and reinnervated vocal cord was tensioned and stopped at laringoscopy. Postoperatively, 8 syntomatic patients (1,02%) with dysphonia were recorded and they had early phoniatric evaluation within 10 days. Six of these patients (0.76% of total thyroid operated) had unilateral vocal fold immobility with dysphonia but without dysphagia while two patients had ipercinetic vocal cord that already was present preoperatively. Patients with unilateral vocal fold immobility were treated with medical therapy associated with phoniatric speech therapy and neck physiotherapy. The aim of physiotherapy is to relax the neck muscle groups as a result of postoperative contracture (due to surgical stress, surgical operating position and postoperative attitude of defense of the neck) alongside the rehabilitation speech therapy for better and more rapid recovery of the vocal function. All patients showed complete laryngeal recovery of motility in 6/8 weeks.
Table 1.
DESCRIPTIVE CHARACTERISTICS OF HISTO-LOGICAL FINDINGS BY PATIENTS NUMBER.
| Number of patients | Percentage (%) | |
|---|---|---|
| Malignant disease | 234 | |
| Differentiated carcinoma | 218 | 27.9 |
| Medullary carcinoma | 3 | 0.4 |
| Insular carcinoma | 2 | 0.2 |
| Unknown malignant potential | 9 | 1.1 |
| Anaplastic cancers | 2 | 0.2 |
| Benignant disease | 548 | |
| Multinodular goiter | 490 | 62.8 |
| Toxic multinodular goiter | 5 | 0.6 |
| Graves’ disease | 25 | 3.2 |
| Thyroiditis | 28 | 3.6 |
Fig. 2.
Graph showing the surgical treatments of the 783 patients.
Fig. 3.
Graph showing the post-operative complications by patients number.
Regarding the injuries of parathyroid glands, 698 patients (89,2%) did not show signs and symptoms of hypocalcemia while 84 patients (10,7%) presented signs of paresthesias and numbness of the fingertips and perioral area and Chvostek’s sign positivity, associated with alteration of biochemical parameters of serum calcium and ionized calcium. None of the patients presented Trousseau’s sign or tetany. In 81 (10.36% of all patients) the restoring of the biochemical parameters and the resolution of symptoms occurred between 2 and 6 weeks (mean 20 days) and only in 3 cases (0.38% of all patients) there was permanent hypoparathyroidism with permanent hypocalcemia (Figure 3). Bleeding complication, occurring within the first few hours after surgery, were observed only in one patient, and we proceeded to immediate revision of hemostasis. Of note, the only 3 cases of permanent hypoparathyroidism and the bleeding case occurred in the first three years of the study, meaning that the surgical experience acquired by the operative surgeons strongly improved the outcome of the following surgical treatment. No morbidity regarding bilateral inferior laryngeal nerves palsy, esophagus, trachea, or carotid artery was ever observed in this series (Figure 3).
Discussion
In this retrospective study we analysed the outcomes of 782 patients that underwent thyroid surgery by using microsurgical technique and loupes magnification 4.5x, between January 2004 and December 2014 in our Institution in Rome, Italy.
The microsurgical technique for the total thyroidectomy that we adopted in our Department of Microsurgery was based on the experience made in the early years of 1900 by Frank Howard Lahey (5)who stressed the importance of the systematic identification and preparation of the recurrent nerves for the purpose of their protection. It is surprising that the same author in 1938 first reported the concept that anyone performing thyroid surgery should have a magnification loupes 2.5x, with a focal range of about 18 inches; in particular, he wrote: “… it is a very valuable means by which one can see the striations in nerves and distinguish them from vessels” (31). For this reason, we adopted microsurgical technique and loupes magnification in all thyroid surgery, instead of standard surgical technique. As reported above, the two most common early complications of thyroid surgery are hypocalcemia and recurrent laryngeal nerve (RLN) injury, respectively 20–30% and 5–11% (2). In agreement with the concept that microsurgical technique allows to remarkably reduce the complications of thyroid surgery, in our series there were no cases of unilateral or bilateral permanent vocal cord palsy, six patients (0,76%) had transient unilateral vocal fold immobility with dysphonia without dysphagia, 10,36% of patients reported transient hypocalcemia while only 0,38% reported permanent hypocalcemia (Figure 3).
The microsurgical technique and the use of loupes are essential in identifying the thin branches of the inferior laringeal nerve, which is particularly exposed at risk in the last extralaryngeal 2 centimeters (cm), especially to perform a real total excision of thyroid parenchyma. Thus, closed to the Zuckerkandl tubercle and fascial layers, there is a frequent site of injury due to transection, clamping, ligation, traction, diathermy injury and ischaemia (7, 32). At that level, great caution must be taken in ligating and dividing such structures, in particular the arterial branches located behind the nerve, to prevent the bleeding whose hemostasis would damage the nerve. For this purpose, we used microsurgical ligatures with absorbable suture 4/0 and 6/0 so as to avoid thermal nerve damage and local edema, avoiding the use of bipolar diathermy. To ensure the integrity of the external branch of the superior laryngeal nerve we paid special attention during dissection of upper vascular pole, tying first the anterior branch of the artery and then the posterior branches, leaving no residual thyroid tissue at ligatures, in agreement with the literature (33). Particular care should be taken during the dissection of the recurrent nerve near the trunk of the inferior thyroid artery (34), avoiding devascularization of the parathyroid glands and dissecting the arterial branches with thin ties near their entry into the gland. In addition, increased complications can also occur during re-surgery on parenchymal residues (2, 35). In our series, nonetheless we treated 90 patients (58 benign and 32 malign) coming from other hospitals, re-surgery using loupes magnification and microsurgical technique did not affect patients’ motility of the vocal cords.
A technique that has been proposed to prevent RLN injuries and to aid nerve localization before visualization is the intra-operative neuromonitoring (IONM) (36). According to some authors, IONM reduces the rate of transient inferior laryngeal nerve palsy, it is useful in the case of thyroid re-surgery, and can help in the identification of the RLN during dissection before visualization (37). However, the role and the utility of IONM during thyroid surgery is still under debate (38) and, at the moment, there is not consensus regarding the prevention of RLN injury (39). In our experience, the use of IONM did not reduce the risks of laryngeal nerves injury (data not shown), suggesting that IONM doesn’t improve the surgeon’s capability to identify and dissect the nerve, but rather it can be helpful in the reoperations and in the cervical lymphadenectomy. Moreover, IONM should not be considered standard of care and should not play a “coroner” role. Higgins in a meta-analysis study of a large series (64699 nerves-at-risk), compared the role IONM of RLN versus RLN identification alone on true vocal fold palsy rates after thyroidectomy, demonstrating no statistically significant difference (40). In a recent systematic review with meta-analysis of studies comparing IONM of RLN versus visualization alone during thyroidectomy of 35513 nerves-at-risk, the authors demonstrated no statistically significant difference in the incidence of RLN palsy when using IONM versus RLN visualization alone (38). In comparison, the advantages of the magnified vision are clearly evident in video-assisted surgery, and recently it has been proposed the use of three-dimensional minimally invasive video-assisted thyroidectomy for a better perception of depth and easy recognising of anatomic structures, especially concerning the upper and lower vascular pedicle, the parathyroids and the laryngeal nerves (41). To the best of our knowledge, there are only five previous studies reporting microscope-assisted thyroidectomy (4, 12–14, 16). The largest study to date is a series of 573 procedures published over a decade ago by Nielsen who reported 0.6% permanent RLN injury (13). Other authors prospectively compared microscopic with conventional thyroidectomy and found the former to result in significantly lower rates of transient hypocalcaemia and reduced rates of RLN injury (16). Recently, in one of the largest microscope-assisted thyroidectomy series to date and the first from a United Kingdom institution, the authors suggested that microscopic dissection may help to prevent inadvertent injury to adjacent structures during crucial dissection steps (notably around the parathyroid glands and their vascular pedicles) and as such proposed microscope-assisted thyroidectomy as a reliable, safe and potentially advantageous method (4). Microscope-assisted thyroidectomy has also been championed for its ergonomic benefits to the surgeon. The operating microscope has been proposed as a method to maintain an upright posture with neutral cervical position during thyroid surgery, so reducing occupational musculoskeletal risk (18). The authors, though, noted a significant increase in operating time especially in case of lateral neck dissection. Nielsen also reported slight increases in operating time (11) while, in a more recent prospective controlled trial, a direct comparison of thyroidectomy performed with and without the operating microscope found no significant differences in operating time (16). Based on our more than thirty years’ experience in other fields of general microsurgery (limb replantation, microvascular free flap, vasectomy reversal and seminal tract reconstruction, inferior laryngeal nerve reconstruction, etc.) (8, 20–27), we believe that the use of the operating microscope during thyroid surgery might be replaced by 4.5× loupes which allows a larger operating field with consequent benefits in surgical procedures and patients outcome. Moreover, the use of the operating microscope also allows recording which has obvious benefits for both teaching purposes and for a medico-legal standpoint (4). In this regard, in 2013 it was developed by the Director of our Microsurgical Department a prototype of high-definition head-on camera (Italian patent request n. RM2013A000601), that the operating surgeon can wear during the operation, able to record the images of the operative field directly and coaxial with his vision. This system records in full high definition at the same focal distance of operator’s loupes (about 17 inches), and is equipped with an anti-vibration optical system and an integrated software for images transfer. To the best of our knowledge, this system is the first in the world able to disclose the difference between the eye vision and the magnified loupes vision of operator, finally demonstrating the undoubted advantages of optical magnification in all surgical specialties and in particular in thyroid surgery.
It is now widely accepted that the rate of thyroid surgery complications is directly related to the extent of thyroidectomy (42) and to the radical thyroid excision as well as to the surgeon’s experience (7). This surgery requires a meticulous dissection of delicate structures, such as laryngeal nerves and parathyroid glands, whose damage can have serious repercussions on the patients life quality. The application of microsurgery in thyroid surgery, as well as in other areas of general surgery, requires experience with microsurgical instruments and confidence with magnifying optical devices. This technique makes no changes to the surgical steps of the traditional technique, but adds the use of dedicated instruments particularly thin and precise as well as optical magnification for the success of the interventions. Indeed microsurgical technique is not essential for identification of the recurrent nerve, rather it is essential for the identification and respect of superior and inferior laryngeal nerve, for the nerve dissection along its cervical course till the larynx, for safeguarding parathyroid glands with their vascularity, for meticolous hemostasis and for performing a “real” total parenchimal excision (11). Moreover, this treatment approach allows completeness of total thyroidectomy with reduced tissue trauma and respect of the strap muscles integrity. Furthermore, the application of microsurgical technique improves complete parenchymal excision. Radical excision avoids, in the case of benign disease, the risk of recurrence and helps the endocrinologist to assess the hormone therapy, and, in the case of cancer, avoids the risk of re-surgery.
Conclusions
To the best of our knowledge this is the first largest series in the literature specifically analysing postoperative morbidity in thyroid surgery with the use of loupes magnification and microsurgical technique suggesting that such treatment approach might significantly reduce thyroid post-operative complications. Although we did not have a control group of patient undergoing standard thyroid surgery, we are pretty confident that the use of microsurgical technique and loupes magnification could have remarkably reduced the post-operative complications, in agreement with the first observation made with the use of magnification (31) and in accordance with the few literature reported using microsurgical techniques and magnification (11–19) and compared to the literature reporting the use of other surgical techniques.
Acknowledgments
We thank Gabriella D’Orazi for critical reading of the manuscript.
Financial and material support was not applied to this study.
Footnotes
Disclosure
The authors declare no conflicts of interest.
Funding received: this study was not supported by grants.
References
- 1.Gómez-Ramírez J, Sitges-Serra A, Moreno-Llorente P, et al. Mortality after thyroid surgery, insignificant or still an issue? Langenbecks Arch Surg. 2015;400:517–522. doi: 10.1007/s00423-015-1303-1. [DOI] [PubMed] [Google Scholar]
- 2.Christou N, Mathonnet M. Complications after total thyroidectomy. J Visc Surg. 2013;150:249–256. doi: 10.1016/j.jviscsurg.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Selberherr A, Scheuba C, Riss P, et al. Postoperative hypoparathyroidism after thyroidectomy: Efficient and cost-effective diagnosis and treatment. Surgery. 2015;157:349–353. doi: 10.1016/j.surg.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Williams SP, Wilkie MD, Tahery J. Microscope-assisted thyroidectomy: Our experience in one hundred and twenty-one consecutive cases. Clin Otolaryngol. 2014;39:289–315. doi: 10.1111/coa.12284. [DOI] [PubMed] [Google Scholar]
- 5.Lahey FH. Routine dissection and demonstration of recurrent laryngeal nerve in subtotal thyroidectomy. Surg Gyn & Obst. 1938;66:775. [Google Scholar]
- 6.Trésallet C, Chigot JP, Menegaux F. How to prevent recurrent nerve palsy during thyroid surgery? Annal Chir. 2006;131:149–153. doi: 10.1016/j.anchir.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Hayward NJ, Grodski S, Yeung M, et al. Recurrent laryngeal nerve injury in thyroid surgery: a review. ANZ J Surg. 2013;83:15–21. doi: 10.1111/j.1445-2197.2012.06247.x. [DOI] [PubMed] [Google Scholar]
- 8.Ortensi A, Marchese V, Lentini A, et al. Reconstructive microsurgery. G Chir. 1997;18:688–691. [PubMed] [Google Scholar]
- 9.Germain MA, Legagneux J. Vascular microsurgery and progress of free flap surgery. Ann Chir. 2001;126:960–968. doi: 10.1016/s0003-3944(01)00645-9. [DOI] [PubMed] [Google Scholar]
- 10.Holm C, Mayr M, Hoefter E, et al. Assessment of the patency of microvascular anastomoses using microscope-integrated near-infrared angiography: A preliminary study. Microsurgery. 2009;29:509–514. doi: 10.1002/micr.20645. [DOI] [PubMed] [Google Scholar]
- 11.Attie JN, Khafif RA. Preservation of parathyroid glands during total thyroidectomy. Improved technic utilizing microsurgery. Am J Surg. 1975;130:399–404. doi: 10.1016/0002-9610(75)90472-9. [DOI] [PubMed] [Google Scholar]
- 12.Cavallaro G, Taranto G, Chiofalo MG, et al. Usefulness of microsurgery to isolation of recurrent laryngeal nerve and parathyroid during thyroidectomy operations. Microsurgery. 1998;18:460–461. doi: 10.1002/(sici)1098-2752(1998)18:8<460::aid-micr6>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen TR, Andreassen UK, Brown CL, et al. Microsurgical technique in thyroid surgery. A 10-year experience. Laryngol Otol. 1998;112:556–560. doi: 10.1017/s0022215100141076. [DOI] [PubMed] [Google Scholar]
- 14.Doikov IY, Yovchev IP, Konsulov SS. Microsurgical technique as a method for prevention of recurrent laryngeal nerve injury in thyroid surgery. Review of seven consecutive cases. Folia Med (Plovdiv) 2001;43:5–9. [PubMed] [Google Scholar]
- 15.Testini M, Nacchiero M, Piccinni G, et al. Total thyroidectomy is improved by loupe magnification. Microsurgery. 2004;24:39–42. doi: 10.1002/micr.10195. [DOI] [PubMed] [Google Scholar]
- 16.Seven H, Calis AB, Vural C, Turgut S. Microscopic thyroidectomy: a prospective controlled trial. Eur Arch Otorhinolaryngol. 2005;262:41–44. doi: 10.1007/s00405-004-0740-1. [DOI] [PubMed] [Google Scholar]
- 17.Pata G, Casella C, Mittempergher F, et al. Loupe magnification reduces postoperative hypocalcemia after total thyroidectomy. Am Surg. 2010;76:1345–1350. [PubMed] [Google Scholar]
- 18.Davidson BJ, Guardiani E, Wang A. Adopting the operating microscope in thyroid surgery: safety, efficiency, and ergonomics. Head Neck. 2010;32:154–159. doi: 10.1002/hed.21157. [DOI] [PubMed] [Google Scholar]
- 19.Alshahrani MA, Alzahrani FR, Alghamdi AS, et al. Impact of neuromonitoring of recurrent laryngeal nerve and surgical loupes on the outcome of thyroidectomy. Saudi Med J. 2013;34:824–828. [PubMed] [Google Scholar]
- 20.Cancrini F, Urciuoli P, Di Matteo FM, et al. Treatment of hemorrhoids with circular mechanic stapler. Chir Ital. 2001;53:95–99. [PubMed] [Google Scholar]
- 21.Urciuoli P, Ghinassi S, Iavarone C, et al. Thyroid anaplastic tumor: our experience. Chir Ital. 2003;55:835–840. [PubMed] [Google Scholar]
- 22.Custureri F, D’Orazi V, Peparini N, et al. Choice of the surgical treatment in early gastric cancer. Hepatogastroenterol. 2004;51:1210–1214. [PubMed] [Google Scholar]
- 23.Ortensi A, Salsano F, Trinchi S, et al. Microsurgical distant sympathectomy in chronic vasospastic sindrome of the hand. Int Surg. 2005;90:88–92. [PubMed] [Google Scholar]
- 24.Urciuoli P, D’Orazi V, Livadoti G, et al. Treatment of renal angiomyolipoma: surgery versus angioembolization. G Chir. 2013;34:326–331. [PMC free article] [PubMed] [Google Scholar]
- 25.Pasta V, Sottile D, Urciuoli P, et al. Rare chondrosarcoma of the breast treated with quadrantectomy instead of mastectomy: a case report. Oncol Lett. 2015;9:1116–1120. doi: 10.3892/ol.2014.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pasta V, Monti M, Cialini M, et al. Primitive sarcoma of the breast: new insight on the proper surgical managment. JECCR. 2015;34:72. doi: 10.1186/s13046-015-0190-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.D’Orazi V, Panunzi A, Paoloni M, et al. Microsurgical approach for unusual and unexpected malignant fibrous histiocytoma of the forearm: A case report. Mol Clin Oncol. 2015;3:1251–1254. doi: 10.3892/mco.2015.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeannon JP, Orabi AA, Bruch GA, et al. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009;63:624–629. doi: 10.1111/j.1742-1241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 29.Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical Practice Guideline: Improving Voice Outcomes after Thyroid Surgery. Otolaryngol Head Neck Surg. 2013;148:S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 30.Crumley R. Update: ansa cervicalis to recurrent laryngeal nerve anastomosis for unilateral laryngeal paralysis. Laryngoscope. 1991;101:384–387. doi: 10.1002/lary.1991.101.4.384. [DOI] [PubMed] [Google Scholar]
- 31.Lahey FH, Hoover WB. Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg. 1938;108:545–562. doi: 10.1097/00000658-193810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serpell JW. New operative surgical concept of two fascial layers enveloping the recurrent laryngeal nerve. Ann Surg Oncol. 2010;17:1628–1636. doi: 10.1245/s10434-010-0928-0. [DOI] [PubMed] [Google Scholar]
- 33.Monfared A, Gorti G, Kim D. Microsurgical anatomy of the laryngeal nerves as related to thyroid surgery. Laryngoscope. 2002;112:386–392. doi: 10.1097/00005537-200202000-00033. [DOI] [PubMed] [Google Scholar]
- 34.Yalçin B. Anatomic configurations of the recurrent laryngeal nerve and inferior thyroid artery. Surgery. 2006;139:181–187. doi: 10.1016/j.surg.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 35.Lefevre JH, Tresallet C, Leenhardt L, et al. Reoperative surgery for thyroid disease. Langenbecks Arch Surg. 2007;392:685–691. doi: 10.1007/s00423-007-0201-6. [DOI] [PubMed] [Google Scholar]
- 36.Duclos A, Lifante JC, Ducarroz S, et al. Influence of Intraoperative Neuromonitoring on Surgeons’ Technique During Thyroidectomy. World J Surg. 2011;35:773–778. doi: 10.1007/s00268-011-0963-4. [DOI] [PubMed] [Google Scholar]
- 37.Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136:1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 38.Pisanu A, Porceddu G, Podda M, et al. Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. Journal Surg Res. 2014;188:152–161. doi: 10.1016/j.jss.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 39.Dionigi G, Van Slycke S, Boni L, et al. Limits of Neuromonitoring in Thyroid Syrgery. Ann Surg. 2013;258:E1–E2. doi: 10.1097/SLA.0b013e318294559d. [DOI] [PubMed] [Google Scholar]
- 40.Higgins TS, Gupta R, Ketcham AS, et al. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope. 2011;121:1009–1017. [Google Scholar]
- 41.Mercante G, Battaglia P, Manciocco V, et al. Three-dimensional minimally invasive video-assisted thyroidectomy: preliminary report. JECCR. 2013;32:78. doi: 10.1186/1756-9966-32-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pelizzo MR, Variolo M, Bernardi C, et al. Complications in thyroid resurgery: a single institutional experience on 233 patients from a whole series of 4,752 homogeneously treated patients. Endocrine. 2014;47:100–106. doi: 10.1007/s12020-014-0225-y. [DOI] [PubMed] [Google Scholar]