Abstract
Contemporary classification systems for mental disorders assume that abnormal behaviors are expressions of latent disease entities. An alternative to the latent disease model is the complex network approach. Instead of assuming that symptoms arise from an underlying disease entity, the complex network approach holds that disorders exist as systems of interrelated elements of a network. This approach also provides a framework for the understanding of therapeutic change. Depending on the structure of the network, change can occur abruptly once the network reaches a critical threshold (the tipping point). Homogeneous and highly connected networks often recover more slowly from local perturbations when the network approaches the tipping point, allowing for the possibility to predict treatment change, relapse, and recovery. In this article we discuss the complex network approach as an alternative to the latent disease model, and we discuss its implications for classification, therapy, relapse, and recovery.
Introduction
Symptoms of mental disorders do not occur randomly; some are more likely to co-occur than others. The traditional psychiatric explanation for such co-occurrence is that symptoms reflect an underlying disease entity that causes their emergence (e.g., Guze, 1992). Just as a malignant lung tumor is the cause of co-occurring breathlessness, bloody sputum, coughing, and chest pain, so is underlying depression deemed the common cause of insomnia, loss of appetite, impaired ability to feel pleasure (anhedonia), and unremitting sadness (cf. Borsboom & Cramer, 2014). Another explanation is that symptoms reflect underlying dimensions (e.g., neuroticism), not discrete, categorical entities (e.g., Krueger & Markon, 2014). The recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013) retains an emphasis on categorical diagnoses despite their limitations (for a review, see McNally, 2011, pp. 184–211).
Psychopathologists have long debated whether disorders differ by kind (i.e., are qualitatively distinct categories) or degree (i.e., vary dimensionally). Debates between proponents of categorical and dimensional diagnosis have been contentious, yet both sides share an implicit understanding of the relation of symptom to disorder. Both assume that symptoms reflect the presence of an underlying, unobserved, latent construct, whether construed categorically or dimensionally (Bollen & Lennox, 1991; Brown & Barlow, 2005; Edwards & Bagozzi, 2000; Hofmann, 2014, 2015; Insel, 2014).
However, for inference to a latent variable as the common cause of symptom covariance to be justifiable, there cannot be any causal connections among the symptoms themselves (i.e., the axiom of local independence must hold). That is, the covariance among symptoms must disappear if one conditionalizes on the presence of the disorder (Borsboom, 2008). This holds true for symptoms of lung cancer, for example, because controlling for the presence of a tumor eliminates the correlations among coughing, chest pain, breathlessness, and chest discomfort. It also holds for Down syndrome where intellectual deficiency, a crease across the palm, short stature, and protruding tongue co-occur because they share a common cause -- three copies of chromosome 21. No direct causal relations occur between a protruding tongue and short stature, for example. But the situation is different for depression and most other psychiatric syndromes where obvious causal connections among symptoms occur, thereby undermining any inference to a latent common cause. For example, people who ruminate will likely experience insomnia, and sleep deprivation will cause fatigue the following day, thereby impairing their concentration and lowering their mood, and so forth (Borsboom & Cramer, 2013). Clearly, causal relations abide among such symptoms of depression – a conclusion forbidden by the psychometric requirements of both latent categorical and latent dimensional models of psychopathology (for reviews, see Borsboom & Cramer, 2013; Hofmann, 2014, 2015).
The complex network approach to conceptualizing psychopathology has emerged as a potentially game-changing alternative to both the latent categorical and latent dimensional approaches (Borsboom & Cramer, 2013; Schmittmann et al., 2013). According to this view, symptoms do not reflect an underlying latent disease that causes their emergence and co-occurrence. Rather, symptoms are constitutive, not reflective, of the disorder. Hence, a disorder is not the underlying cause of symptoms; it constitutes a network consisting of symptoms that interact in ways that tend to maintain themselves. Accordingly, a stressful event does not activate an underlying entity called depression, which then causes the emergence of symptoms. Rather, stressful events activate certain symptoms that in turn activate other symptoms, and when the requisite number of symptoms occurs, an episode of disorder may be diagnosable. The term symptom implies that sadness, anhedonia, loss of appetite, insomnia, and so forth, reflect the presence of an underlying disease entity that causes their emergence. Accordingly, to avoid this implication, we follow Snaith (1993) and use element instead of symptom in this article. The purpose of our article is to discuss the complex network approach to clinical science. We will first describe the essential elements of complex network analysis and then illustrate its implications for classification, treatment, and relapse. Based on this approach, disorders differ as a result of differences in the number, nature, and inter-relatedness of their elements that constitute the network. This perspective offers exciting new opportunities not only for psychopathology and nosology (Borsboom & Cramer, 2013), but also for predicting treatment outcome, relapse, and recovery. We focus on network topology (i.e., structure) as applied to psychological problems, and then shift to network dynamics (i.e., how networks evolve over time) especially in relation to the transition from health to illness and vice versa. But first we provide an overview of complex network analysis.
A Brief Introduction to Complex Networks
Network theory is a subset of graph theory, a branch of mathematics concerning the visual representation of a set of objects and the links connecting pairs of objects (Christakis & Fowler, 2009). Networks contain two components: nodes that represent objects (e.g., individual persons, neurons, symptoms, nations) and edges – lines that connect two objects representing the type of association between them (e.g., a connection between two friends in a social network). An unweighted network merely depicts whether two nodes are connected (e.g., a line between Tom and Julian indicates their friendship), whereas a weighted network also represents the strength of association (e.g., a Pearson r correlation coefficient indicating the magnitude of association between insomnia and fatigue computed over a number of individual persons).
Network theory enables computation of centrality metrics that reveal the importance of a node in the network. A highly central node is one, when activated, is likely to spread activation throughout the network via the edges connecting it to other nodes. For example, a node high on degree centrality is one with many edges connected to it (e.g., a highly popular person in a social network). A node high on strength centrality in a weighted network is one having many edges connected to it that are great in terms of their magnitude of associations (e.g., the Pearson’s r of each edge is large). A node high on betweenness centrality is one that often lies on the shortest pathway between two other nodes (e.g., a large department store that mediates the selling of items from many producers to many customers).
Complex networks comprise many nodes whose connections are neither random nor uniform in their connections (Watts & Strogarts, 1998; Barabási & Albert, 1999). That is, the structure (i.e., topology) of the network varies; some nodes cluster in subgroups, whereas others have few or weak connections with other nodes. Complex networks are the empirical norm in sociology, neuroscience, and psychopathology, as we will describe in more detail below. Repeated assessments of the nodes and edges of a network reveal how networks evolve over time (e.g., network dynamics), evinced by the trajectory or recovery from a mental disorder.
The Complex Network Perspective on Psychopathology
Although still in a nascent stage, complex network approaches have attracted the attention of researchers from many different fields.1 Following suit, clinical researchers are increasingly applying network analysis to elucidate depression (Bringmann et al., 2015; Cramer, Borsboom, Aggen, &, Kendler, 2012; Fried et al., 2016; van de Leemput et al., 2014), complicated grief (Robinaugh, LeBlanc, Vuletich, & McNally, 2014), generalized anxiety disorder (Fisher, 2015), and posttraumatic stress disorder (PTSD; McNally, 2012; McNally et al., 2015). These studies provide an initial glimpse of the complex network structure abiding among elements of these syndromes. Using large numbers of subjects, researchers have computed networks illustrating how elements of these syndromes are associated, thereby providing visual depictions of potentially causal relations among them.
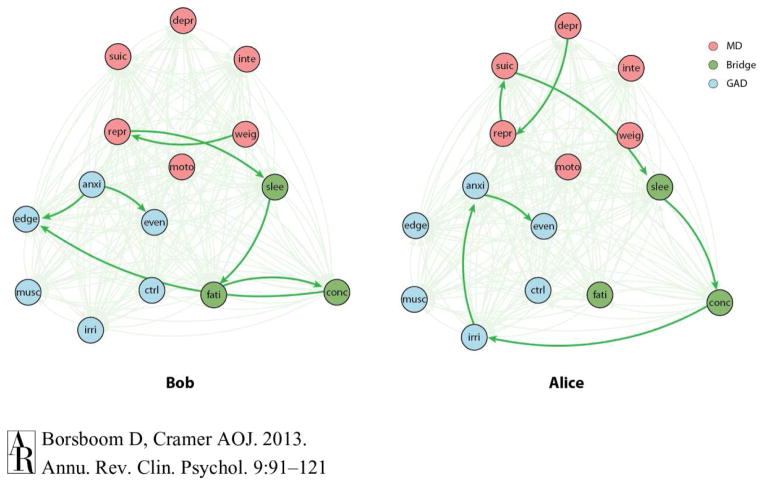
An example of how the complex network approach can be applied to specific cases is presented in Figure 1. This figure depicts hypothetical examples of individual networks for two individuals, Bob and Alice (Borsboom & Cramer, 2013). These two individual networks illustrate that there are many ways that depression and generalized anxiety disorder (GAD) can be connected through common nodes. Most relevant for deriving treatments are individual networks.
Figure 1.
Hypothetical examples of individual complex networks for two people (Bob and Alice). The red circles show the nodes of the network that are part of the “depression” network (suic: suicidality; inte: loss of interest; depr: depressed mood; repr: self-reproach; moto: psychomotor disturbances; weig: weight problems); the blue circles are the nodes that are part of the “generalized anxiety disorder” (GAD) network (anxi: chronic anxiety/worry; edge: feeling on edge; even: anxiety about more than one even; ctrl: no control over anxiety; musc: muscle tension) and the green circles are part of both networks, bridging the depression and GAD networks (slee: sleep problems; fati: fatigue; conc: concentration problems). The arrows depict hypothetical causal links and the thickness depicts the hypothetical strength of the causal relations. From: Borsboom & Cramer, 2013, Annual Review of Clinical Psychology, 9, 91–121.
An intervention that effectively targets one element often influences many other elements connected in the same network. Elements connected into networks can settle into distinct stable states (e.g., healthy versus pathological). Although there will be as many networks as there are individuals (because it is unlikely that any two individuals will share the identical network), some features of these individual networks are likely to be more common across these networks than others, which will allow categorizing individual networks based on similarity of the structure and elements.
Implications for Diagnostic Classification
What, then, are the diagnostic implications of the network perspective? First, it offers a new way of understanding disorders rather than a new way of diagnosing them. That is, the network perspective provides a new ontology for mental disorders (McNally, 2012), not an alternative to the DSM or ICD. It directs attention to the defining features of the pathology (nodes) and their functional interconnections (edges) and away from a search for an underlying common cause of the activated elements, expressed as a sum score designed to index severity (e.g., Fried & Nesse, 2015). It recommends a search for mechanisms (or biomarkers) causing specific elements (e.g., anhedonia), instead of disorders (e.g., major depression).
Second, the network perspective acknowledges heterogeneity within diagnoses, but it conceptualizes it differently than the DSM has done. Subtyping different patterns of symptoms within a diagnostic category has been the traditional approach to heterogeneity (e.g., melancholic depression, atypical depression). Rather than interpreting heterogeneity as reflective of distinct latent variables within a diagnostic category, each with its own common cause, the network perspective views heterogeneity as common patterns suggestive of causal links between features of a disorder (e.g., diurnal variation of mood and early morning awakening in the melancholic network).
Third, the network perspective offers a distinct approach to differential diagnosis. For example, consider someone who has experienced a car accident and now fears driving. The traditional approach implies that an assessor needs to determine whether fear and avoidance of driving is reflective of the underlying condition of specific phobia or posttraumatic stress disorder (e.g., McNally & Saigh, 1993). Yet, the question should not be whether the driving fear is “due to” specific phobia or PTSD, as the DSM asks; the question is what other symptoms are active and how they relate to one another. This approach is reminiscent of the pre-DSM-III functional analysis favored by behavior therapists (e.g., Goldfried & Davison, 1976) except that the latter tended to emphasize links between environmental stimuli – antecedents and consequences – and symptoms more than functional relations between symptoms, but with some notable exceptions (e.g., functional relations between obsessions and compulsions).
Fourth, as Cramer et al. (2010) demonstrated, network analysis can better address the comorbidity problem. Traditional diagnostic efforts have endeavored to purify disorders of nonspecific symptoms that appear in multiple diagnoses (e.g., sleep disturbance, concentration impairment; Spitzer, First, & Wakefield, 2007), thereby sharpening the distinction between disorders that are often comorbid. Rather than removing these nonspecific elements, the network analytic framework emphasizes them. Indeed, it views them as extremely important bridges, which, if activated, will transmit activation to features of several related disorders. Therefore, the network approach does not provide a replacement for the DSM. Rather, it provides a new way of understanding the relation between disorders and their defining features.
Implications for Therapy, Recovery, and Relapse
The complex network perspective has direct implications for understanding therapy, recovery, and relapse. Specifically, local or individual networks can provide valuable information for treatment planning and treatment targets. In fact, work on complex network models of aquatic systems by the ecologist Scheffer and his colleagues (2009, 2012) are directly relevant for transitions from mental health to mental disorder and vice versa. This approach derives from chaos theory and catastrophe theory to explain non-linear, dynamic, and transitional phenomena (e.g., Scheffer et al, 2009; Vandervert, 1991; Thom, 1977).
An important feature of a dynamic system is that it is characterized by attractor states, in which a given network achieves equilibrium and increased stability. When a network is in such a stable state, disturbances tend to disrupt the equilibrium only temporarily as the network tends to return quickly to the attractor state once the disturbance passes. However, some disturbances may push the network over a critical threshold, tipping it into a new, stable state. This can happen when a major stressor destabilizes a healthy network, tipping the person into a depression network.
The key characteristics to understanding network changes from one state to another lie in the connectivity of the nodes of the network and its homogeneity. Network connectivity refers to the degree to which the nodes are connected with each other. A network has a high level of homogeneity if the nodes show a high level of similarity. For example, in the case of depression, the nodes low self-esteem and suicidal ideation are more similar than are low self-esteem and diminished appetite (because self-esteem and suicidal ideation are both cognitive elements, whereas diminished appetite is neurovegetative). Networks that are homogenous and highly connected tend to show bi-stability (i.e., pathological vs. non-pathological).
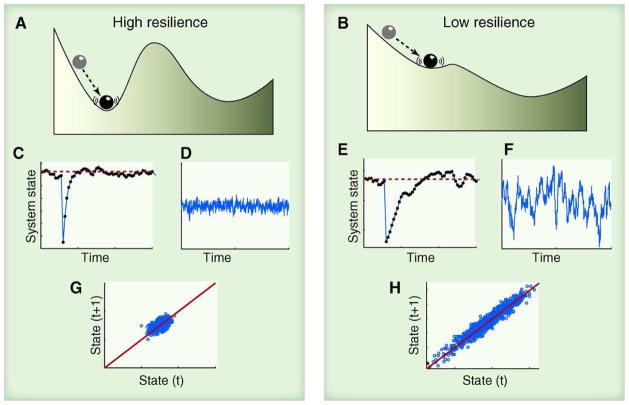
Resilience denotes how quickly a system recovers from perturbations. Highly connected and homogeneous networks tend to be resilient to change; destabilizing events alter the configuration of nodes only temporarily. Strong local connectivity among a cluster of neighboring nodes promotes local resilience because the entire network can compensate for the destabilizing effects of local perturbations. The ability of the network to compensate from local perturbations is linked to the structure of the network. Networks with highly connected nodes are more stable, as depicted by the deeper valley in Figure 2. A complex system that occupies a pathological state is resilient if attempts to change it fail (i.e., the attractor state is strong), thereby preventing the system from reaching the tipping point to move from one state to another. Weak connectivity typically causes the network to change gradually in response to external influences because weakly connected and isolated nodes tend to shift independently of one another. In contrast, a local perturbation can cause a domino effect cascading into an abrupt and systemic transition to another attractor state in the case of homogenous and highly connected systems when a tipping point is reached, (e.g., Scheffer et al., 2012).
Figure 2.
Critical slowing down as an indicator that the system has lost resilience and may therefore be tipped more easily into an alternative state (for explanation, see text). From: Scheffer et al., 2012, Science, 338, 344–348. Reprinted with permission.
From a complex network perspective, effective therapy, whether behavioral or pharmacological, attempts to de-stabilize the pathological state, moving the network over the tipping point to reach a nonpathological state. In the case of relapse, the system moves from the nonpathological to the pathological state. Importantly, Scheffer (2010) has identified certain features of dynamic systems that signify when a dynamic system is approaching a tipping point, potentially suggesting that therapists may be able to identify signals of impending relapse.
Scheffer et al. (2012) depict this phenomenon with a ball rolling across a valley and hill (Figure 2). A network is more resilient and stable if the valley is deep; it requires more effort to move the ball out of the valley and over the hill. In contrast, the network is less resilient if the valley is shallow as less effort is required to move the ball out of the valley. As a result, recovery rates after small perturbations (C and E) are slower if the basin of attraction is small (B) than when the attraction basin is large (A). Under conditions far from the tipping point, a network is resilient because the basin of attraction is large, and perturbations will not easily drive the network towards an alternative stable state.
Networks comprising highly interconnected nodes can reach a tipping point where a local perturbation causes a domino effect cascading into a systemic transition if outside disturbances satisfy a critical threshold. In mental health, these disturbances may be adverse life events or other stressors. In contrast, networks that are not highly interconnected (i.e., networks characterized by weakly or incompletely connected nodes) are more likely to change gradually in response to such perturbations. Complex systems can give the false impression of resilience after repeated recovery from small-scale perturbations when, in fact, the network is moving toward a tipping point (e.g., from non-depressed to depressed), leading to a systemic shift (which network theorists call catastrophic bifurcations). Requisite for such a sudden transition is a positive feedback loop that propels the network toward an alternative state once a critical point is passed. For example, one cognitive model of panic holds that panic attacks result from a feedback loop whereby certain bodily sensations (e.g., a skipped heartbeat) provoke a catastrophic appraisal of the sensation (e.g., “I’m having a heart attack!”), which, in turn, provokes increased heart rate and fear (Clark, 1986). Based on the cognitive model, this feedback loop eventually culminates in a panic attack.
Certain generic features of networks signify critical transitions, which indicate that the system is approaching a tipping point (Scheffer, Bascompte, Brock, et al., 2009). This could be of great value for clinical science as mathematical models of such networks might predict remission or relapse, and it may, therefore, provide a critical window for early intervention to prevent relapse or even the onset of a disorder. In the aforementioned case of the panic patient with the fear of heart palpitations, it might be possible to predict the onset of a panic attack based on the covariation pattern between frequent measurement points of the person’s heart rate and catastrophic interpretations of these symptoms over a period of time.
One important feature that signals such a transition is critical slowing down, characterized by a network’s slow recovery from local perturbations (e.g., due to external stressors). This suggests that the network has lost resilience and may therefore be tipped easily into an alternative state (e.g., from a “normal” into a “panic attack” state). Indicative of slowing down are fluctuations in the configuration of the network (D and F) measured by increased variance of changes of some elements of the network (e.g., moment-by-moment changes in heart rate in the case of a panic patient) and greater lag-1 autocorrelations (G and H) (e.g., higher correlations of heart rate measured at times t and t+1). Another example might be the change in a depression-prone student’s social system following the move a new neighborhood. From a complex network perspective, the disturbance may be temporarily offset by the support of friends and family. However, this situation may worsen when academic stress increases, forcing the student to spend more time doing homework and thereby further limiting social contact. As a result, the stress in combination with social isolation may drive the system to a tipping point, cascading from the local perturbation to a systemic perturbation resulting in depression.
Predicting transitions in complex networks requires time series data with many high-resolution observations (e.g., changes in mood and other elements that are part of the depression network). In addition, it is often unclear what variables need to be observed and when. Several different parameters may be estimated to determine the presence of early warning signals of a critical transition. For instance, increases in autocorrelation, variance, and skewness betoken potential critical transitions (Dakos et al., 2012; Scheffer, 2010; Carpenter & Brock, 2006; Guttal & Jayaprakash, 2008). This would indicate a critical slowing down of the system (i.e., the state becomes more and more similar to the past state) and an increase in time spent near the ‘saddle point’(i.e., perturbations cause the system to become closer to the boundary that separates the two states; see Figure 2). Estimates of these parameters, as well as inspection of their graphical properties, can facilitate interpretations about whether a critical transition may occur. A statistical package to predict critical transitions in complex systems has been developed by Scheffer’s Synergy Program for Analyzing Resilience and Critical Transitions (SparcS, 2012–2015). The program is freely available at: http://www.sparcs-center.org/earlywarnings.html.
Especially valuable to clinical scientists will be the capability of identifying signals that predict transitions from non-pathological states to pathological states and vice versa. Experience Sampling Methods (ESM) has been used to accomplish this in studies of depression (Bringmann et al., 2013; Hartmann et al., 2015; Kramer et al., 2014, van de Leemput et al., 2014; Telford, McCarthy-Jones, Corcoran, & Rowse, 2012). However, only van de Leemput et al. (2014) have applied this method to examine the critical transition of the depression network in a large sample. The authors recruited 535 individuals from the general population and 93 depressed patients. To calculate early warning signals for the transition from the depressed to the non-depressed state, the investigators had participants use experience sampling to rate their moods multiple times across 5–6 days. The data of the depressed patients came from two studies, which included baseline ESM measurements followed by an intervention (either a combination of pharmacotherapy and supportive counseling or allocation to either imipramine or placebo) and follow-up assessments of depressive symptoms. The results pointed to critical slowing down as indicated by early warning signs of the onset and termination of depression (i.e., elevated temporal autocorrelation, variance, and correlation between emotions). This proof-of-concept study suggests that the complex network approach can be successfully applied to treatment-relevant issues.
A combination between idiographic and nomothetic network approaches was used by Fisher, Newman, and Molenaar (2011) to examine treatment changes in the context of a dynamic network perspective within one specific diagnostic sample. Using EMA data, the authors examined 33 patients with GAD who underwent psychotherapy. Idiographic data gathered through daily diaries of patients’ anxiety were subjected to a spectral analysis. A spectral analysis enables researchers to identify regular patterns of events (harmonic oscillations) in time series data that occur at different frequencies. These idiographic data were then aggregated for nomothetic analyses of treatment outcome. The results showed that high-frequency power (power attributed to oscillations of 1 day or less) predicted treatment outcome with lesser variance between these diary reports predicting better outcome.
In summary, the analytic approaches described above reflect a subset of a growing number the statistical procedures for modeling complex networks. As indicated by Borsboom and Cramer (2013), longitudinal research will be vital to the advancement of complex network research, as the characterization of dynamic, temporal patterns in psychopathology will convey important information about how to optimize treatments. Moreover, the advent of new technologies will mitigate the burden associated with time intensive research, such as ESM, in which participants report thoughts, feelings, and symptoms at least daily. Although this requires the collection of a large amount of data over an extended period, the recent advancements in wireless-enabled wearable technology (e.g., smartwatches, smartphones, etc.) are likely to render this method feasible in the very near future.
Conclusion
The complex network approach offers an alternative to the latent disease model that assumes that symptoms arise from an underlying common cause. The network approach assumes that disorders exist as systems of inter-related psychological problems including maladaptive behaviors, cognitive biases, emotional disturbance, and physiological abnormalities (Borsboom & Cramer, 2013; Hofmann, 2014, 2015). Although the empirical evidence is limited, this approach offers a fresh new perspective on understanding psychopathology. A complex network perspective on psychopathology not only addresses the comorbidity problem (Cramer et al., 2010), but it also considers the functional connectivity between presenting problems of an individual. This, in turn, could have direct implications for therapy. Indeed, the complex network approach appears compatible with traditional and modern treatment approaches (Hayes et al., 2015; Hofmann, 2014).
Treatment change, recovery, and relapse, is consistent with the notion that complex systems can take on bi-stable states via critical transitions. This makes a complex network perspective highly relevant for clinical science. In highly connected networks relevant to mental health, transitions from one state to another are seldom linear. Rather, the change often occurs abruptly once the system reaches a tipping point. Longitudinal within-subject tracking of psychological problems will enable clinical researchers to identify critical transition points. However, this issue has been seldom discussed in the contemporary literature with some exceptions (Fisher, 2015; van de Leemput et al., 2014). Adopting this approach would pave the way toward a personalized clinical science consistent with NIMH’s call for precision medicine for our field (Insel, 2013).
In conclusion, the complex network perspective provides an approach to elucidating causation in psychopathology that differs from traditional latent categorical and dimensional approaches. Traditional approaches hold that stressful life events, for example, cause the underlying condition of depression which, in turn, causes the activation of symptoms that reflect its presence but do not causally affect one another. The notion that sleep loss does not cause fatigue or concentration impairment is clinically implausible, yet requisite for justifying inference to a latent common cause as the source of the problems. In contrast, the complex network perspective acknowledges environmental (and genetic) causes, but as triggers activating individual features of a disorder, which, in turn, activate other elements of the network. Moreover, the arrow of causation may emerge as self-reinforcing, homeostatic loops, such as hypervigilance fostering exaggerated startle responses in trauma survivors which, in turn, maintain their hypervigilance (see McNally et al., 2015). Unlike theoretical diagrams common in 20th century psychology (e.g., stimulus > organism > response models of neobehaviorism; causal flowcharts of cognitive psychology), the graphs produced by network analysis are empirically derived. Although most network research on psychopathology has involved computational procedures depicting correlational and partial correlational associations between elements of the network, these studies provide clues to possible causal relations confirmable in future longitudinal and interventional studies done within the complex network framework.
Acknowledgments
Dr. Hofmann receives support from NIH/NCCIH (R01AT007257), NIH/NIMH (R01MH099021, R34MH099311, R34MH086668, R21MH102646, R21MH101567, K23MH100259), and the Department of the Army for work unrelated to this article. He receives compensation for his work as an advisor from the Palo Alto Health Sciences and Otsuka America Pharmaceutical, Inc., and for his work as a Subject Matter Expert from John Wiley & Sons, Inc. and SilverCloud Health, Inc. He also receives royalties and payments for his editorial work from various publishers. Joshua Curtiss and Richard McNally have no disclosures to report. We thank Eiko Fried for alerting us to the article by Snaith (1993).
Footnotes
Examples include psychological assessments (Heiby, 1995a, 1995b), neuroscience and genetics (Barabási, Gulbahcem, & Loscalzo, 2011; Kim, Zhu, Chang, Bentler, & Ernst, 2007), and the social psychology of intractable ethnic conflicts (Vallacher, Coleman, Nowak, & Bui-Wrzosinska, 2010).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Barabási AL, Albert R. Emergence of scaling in random networks. Science. 1999;286:509–512. doi: 10.1126/science.286.5439.509. [DOI] [PubMed] [Google Scholar]
- Barabási AL, Gulbahce N, Loscalzo J. Network medicine: A network-based approach to human disease. Nature Reviews: Genetics. 2011;12:56–68. doi: 10.1038/nrg2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen K, Lennox R. Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin. 1991;110:305–314. doi: 10.1037/0033-2909.110.2.305. [DOI] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. Journal of Clinical Psychology. 2008;64:1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS ONE. 2011;6:1–11. doi: 10.1371/journal.pone.0027407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Lemmens LHJM, Huibers MJH, Borsboom D, Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychological Medicine. 2015;45:747–757. doi: 10.1017/S0033291714001809. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, Borsboom D, Tuerlinckx F. A network approach to psychopathology: New insights into clinical longitudinal data. PLoS ONE. 2013;8:1–13. doi: 10.1371/journal.pone.0060188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Dimensional versus categorical classification of mental disorders in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders and beyond: Comment on the special section. Journal of Abnormal Psychology. 2005;114:551–556. doi: 10.1037/0021-843X.114.4.551. [DOI] [PubMed] [Google Scholar]
- Carpenter SR, Brock WA. Rising variance: A leading indicator of ecological transition. Ecology Letters. 2006;9:311–318. doi: 10.1111/j.1461-0248.2005.00877. [DOI] [PubMed] [Google Scholar]
- Cramer AOJ, Borsboom D, Aggen SH, Kendler KS. The pathoplasticity of dysphoric episodes: Differential impact of stressful life events on the pattern of depressive symptom inter-correlations. Psychological Medicine. 2012;42:957–965. doi: 10.1017/S003329171100211X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences. 2010;33:137–193. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. Connected: The surprising power of our social networks and how they shape our lives. New York: Little, Brown and Company; 2009. [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Dakos V, Carpenter SR, Brock WA, Ellison AM, Guttal V, Ives AR, … Scheffer M. Methods for detecting early warnings of critical transitions in time series illustrated using simulated ecological data. PloS ONE. 2012;7:1–20. doi: 10.1371/journal.pone.0041010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JR, Bagozzi RP. On the nature and direction of relationships between constructs and measures. Psychological Methods. 2000;5:155–174. doi: 10.1037/1082-989x.5.2.155. [DOI] [PubMed] [Google Scholar]
- Fisher AJ. Toward a dynamic model of psychological assessment: Implications for personalized care. Journal of Consulting and Clinical Psychology. 2015;83:825–836. doi: 10.1037/ccp0000026. [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Newman MG, Molenaar PCM. A quantitative method for the analysis of nomothetic relationships between idiographic structures: Dynamic patterns create atractor states for sustained posttreatment change. Journal of Consulting and Clinical Psychology. 2011;79:552–563. doi: 10.1037/a0024069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are ‘good’ depressive symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Fried E, Nesse RM. Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Medicine. 2015;13:1–11. doi: 10.1186/s12916-015-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfried MR, Davison GC. Clinical behavior therapy. New York: Holt, Rinehart and Winston; 1976. [Google Scholar]
- Guttal V, Jayaprakash C. Changing skewness: An early warning signal of regime shifts in ecosystems. Ecology Letters. 2008;11:450–460. doi: 10.1111/j.1461-0248.2008.01160.x. [DOI] [PubMed] [Google Scholar]
- Guze SB. Why psychiatry is a branch of medicine. New York: Oxford University Press; 1992. [Google Scholar]
- Hartmann JA, Wichers M, Menne-Lothmann C, Kramer I, Viechtbauer W, Peeters F, Schruers K, van Bemmel AL, Myin-Germeys I, Delespaul P, van Os J, Simons CJP. Experience sampling-based personalized feedback and positive affect: A randomized controlled trial in depressed patients. PlosONE. 2015;10:1–16. doi: 10.1371/journal.pone.0128095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Yasinski C, Barnes JB, Bockting CLH. Network destabilization and transition in depression: New methods for studying the dynamics of therapeutic change. Clinical Psychology Review. 2015;41:27–39. doi: 10.1016/j.cpr.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiby EM. Chaos theory, nonlinear dynamical models and psychological assessment. Psychological Assessment. 1995a;7:5–9. [Google Scholar]
- Heiby EM. Assessment of behavioral chaos with a focus on transitions in depression. Psychological Assessment. 1995b;7:10–16. [Google Scholar]
- Hofmann SG. Toward a cognitive-behavioral classification system for mental disorders. Behavior Therapy. 2014;45:576–587. doi: 10.1016/j.beth.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. The potential contribution of the cognitive-behavioral model for the classification of emotional disorders. Psychopathology Review. 2015;2:100–109. doi: 10.5127/pr.035814. [DOI] [Google Scholar]
- Insel TR. Transforming diagnosis. My Blog, Tom Insel, M.D., NIMH Director. 2013 Apr 29; http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml?utm_source=rss_readers&utm_medium=rss&utm_campaign=rss-full (Retrieved February 12, 2015)
- Insel TR. The NIMH Research Domain Criteria (RDoC) Project: Precision medicine for psychiatry. American Journal of Psychiatry. 2014;17:395–397. doi: 10.1176/appi.ajp.2014.14020138. [DOI] [PubMed] [Google Scholar]
- Kim J, Zhu W, Chang L, Benter PM, Ernst T. Unified structural equation modeling approach for the analysis of multisubject, multivariate functional MRI data. Human Brain Mapping. 2007;28:85–93. doi: 10.1002/hbm.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer I, Simons CJP, Hartmann JA, Menne-Lothmann C, Viechtbauer W, Peeters F, Schruers K, van Bemmel AL, Myin-Germeys I, Delespaul P, van Os J, Wichers M. A therapeutic application of the experience sampling method in the treatment of depression: A randomized controlled trial. World Psychiatry. 2014;13:68–77. doi: 10.1002/wps.20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. The role of DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annual Review of Clinical Psychology. 2014;10:477–501. doi: 10.1146/annurev-clinpsy-032813-153732. [DOI] [PubMed] [Google Scholar]
- McNally RJ. What is mental illness? Cambridge, MA: The Belknap Press of Harvard University Press; 2011. [Google Scholar]
- McNally RJ. The ontology of posttraumatic stress disorder: Natural kind, social construction, or causal system? Clinical Psychology: Science and Practice. 2012;19:220–228. doi: 10.1111/cpsp.12001. [DOI] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno M, Borsboom D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science. 2015;3:836–849. doi: 10.3389/fpsyt.2015.00164. [DOI] [Google Scholar]
- McNally RJ, Saigh PA. On the distinction between traumatic simple phobia and posttraumatic stress disorder. In: Davidson JRT, Foa EB, editors. Posttraumatic stress disorder: DSM-IV and beyond. Washington, DC: American Psychiatric Press; 1993. pp. 207–212. [Google Scholar]
- Robinaugh DJ, LeBlanc NJ, Vuletich HJ, McNally RJ. Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. Journal of Abnormal Psychology. 2014;123:510–522. doi: 10.1037/abn0000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheffer M. Complex Systems: Forseeing tipping points. Nature. 2010;467:411–412. doi: 10.1038/467411a. [DOI] [PubMed] [Google Scholar]
- Scheffer M, Bascompte J, Brock WA, Brovkin V, Carpenter SR, Dakos V, … Sugihara G. Early-warning signals for critical transitions. Nature. 2009;461:53–59. doi: 10.1038/nature08227. [DOI] [PubMed] [Google Scholar]
- Scheffer M, Carpenter SR, Lenton TM, Bascompte J, Brock W, Dakos V, … Pascual M. Anticipating critical transitions. Science. 2012;338:344–348. doi: 10.1126/science.1225244. [DOI] [PubMed] [Google Scholar]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology. 2013;31:43–53. doi: 10.1016/j.newideapsych.2011.02.007. [DOI] [Google Scholar]
- Snaith P. What do depression ratings scale measure? British Journal of Psychiatry. 1993;163:293–298. doi: 10.1192/bjp.163.3.293. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, First MB, Wakefield JC. Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders. 2007;21:233–241. doi: 10.1016/j.janxdis.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Telford C, McCarthy-Jones S, Corcoran R, Rowse G. Experience sampling methodology studies of depression: The state of the art. Psychological Medicine. 2012;42:1119–1129. doi: 10.1017/S0033291711002200. [DOI] [PubMed] [Google Scholar]
- Thom R. Structural stability, catastrophe theory, and applied mathematics. Society for Industrial and Applied Mathematics Review. 1977;19:189–201. [Google Scholar]
- Vallacher RR, Coleman PT, Nowak A, Bui-Wrzosinska L. Rethinking intractable conflict. American Psychologist. 2010;65:262–278. doi: 10.1037/a0019290. [DOI] [PubMed] [Google Scholar]
- van de Leemput IA, Wichers M, Cramer AOJ, Borsboom D, Tuerlinckx F, Kuppens P, van Nes EH, Viechtbauer W, Giltay EJ, Aggen SH, Derom C, Jacobs N, Kendler KS, van der Maas HLJ, Neale MC, Peeters F, Thiery E, Zachar P, Scheffer M. Critical slowing down as early warning for the onset and termination of depression. Proceedings of the National Academy of Sciences. 2014;111:87–92. doi: 10.1073/pnas.1312114110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandervert LR. Society for chaos theory in psychology holds its inaugural conference. The Social Dynamics. 1991;2:9–10. [Google Scholar]
- Watts DJ, Strogatz SH. Collective dynamics of small world networks. Nature. 1998;393:440–442. doi: 10.1038/30918. [DOI] [PubMed] [Google Scholar]