Abstract
Theorists have long argued that personality disorder (PD) is best understood in terms of general impairments shared across the disorders as well as more specific instantiations of pathology. A model based on this theoretical structure was proposed as part of the DSM-5 revision process. However, only recently has this structure been subjected to formal quantitative evaluation, with little in the way of validation efforts via external correlates or prospective longitudinal prediction. We used the Collaborative Longitudinal Study of Personality Disorders dataset to: (1) estimate structural models that parse general from specific variance in personality disorder features, (2) examine patterns of growth in general and specific features over the course of 10 years, and (3) establish concurrent and dynamic longitudinal associations in PD features and a host of external validators including basic personality traits and psychosocial functioning scales. We found that general PD exhibited much lower absolute stability and was most strongly related to broad markers of psychosocial functioning, concurrently and longitudinally, whereas specific features had much higher mean stability and exhibited more circumscribed associations with functioning. However, both general and specific factors showed recognizable associations with normative and pathological traits. These results can inform efforts to refine the conceptualization and diagnosis of personality pathology.
Keywords: Personality Disorders, Personality Traits, Psychosocial Functioning, Longitudinal Studies, Bi-factor Model, Multilevel Structural Equation Modeling
There is widespread dissatisfaction with the structure of the Diagnostic and Statistical Manual of Mental Disorders’ (DSM) personality disorder (PD) model (Krueger & Eaton, 2010; Krueger, Skodol, Livesley, Shrout, & Huang, 2007; Widiger & Clark, 2000). High co-morbidity and within-diagnosis heterogeneity suggest that a model based on empirically identifiable dimensions that cut across traditional categories would better match the natural structure of PD (Skodol, 2012; Widiger & Trull, 2007). Theory and several lines of converging evidence argue for the importance of considering shared variation across all PDs (i.e., general features) separately from more circumscribed individual differences in their manifestation (i.e., specific or stylistic features) (Bornstein, 1998; Hopwood, 2011; Kernberg, 1984; Parker et al., 2004; Pincus, 2005; Tyrer & Johnson, 1996). PDs not only show high cross-sectional co-morbidity, they also share trajectories of symptomatic improvement in longitudinal studies (Grilo et al., 2004; Lenzenweger, 1999). Although the shared course is generally one of symptom decline, differential levels of stability across features (McGlashan et al., 2005), enduring patterns of psychosocial dysfunction (Gunderson et al., 2011; Skodol, Pagano, et al., 2005; Zanarini et al., 2012), and individual differences in rates of decline (Lenzenweger, Johnson, & Willett, 2004) complicate the picture. The nuance embedded in the configurations of stability and change may hold important information for elucidating the structure of PD phenomena.
Personality Disorder Structure
Extensive psychiatric comorbidity suggests that organizing mental illness into discrete disorders fails to capture its natural structure (Hyman, 2011; Krueger & Markon, 2006). For the PDs diagnostic covariation is particularly high (Widiger & Rogers, 1989), suggesting that the shared features of PD, independent of stylistic differences in its manifestation, are important for understanding, assessing, diagnosing, and treating, personality pathology (Kernberg, 1984; Livesley, 1998; Parker et al., 2004). Accordingly, several proposals for a general definition have been furthered involving adaptive failures in key domains of functioning (Bender et al., 2011).
Notable among such proposals is the alternative DSM-5 model for PD (American Psychiatric Association, 2013; Krueger, 2013; Skodol, 2012; Skodol et al., 2015), in which Criterion A defines general impairments in PD, focusing on self and interpersonal functioning, and Criterion B uses pathological personality trait dimensions to define individual differences in the stylistic manifestation of PD. This alternative model, which is now listed in Section III (Emerging Models and Measures) of the DSM-5, has sparked a field-wide dialogue about the reformulation of PD diagnosis and driven empirical investigations into general and specific features of PD (e.g., Few et al., 2013; Hopwood et al., 2012; Morey, Benson, & Skodol, 2016).
Efforts to distinguish general and specific features via separate instruments (Livesley, 2006; Verheul et al., 2008) is challenging due to psychometric and conceptual overlap in the scales comprising the measures. While general PD scales are significant predictors of important outcomes, when included in regression models they frequently offer only modestly incremental prediction (if any) beyond scales that blend both pathological behavior and stylistic differences in expression of that behavior in their content (Bastiaansen, De Fruyt, Rossi, Schotte, & Hofmans, 2013; Creswell et al., 2016; Few et al., 2013; Hopwood et al., 2012). Although this may be expected because general and specific measures relevant to PD typically overlap in content by virtue of their focus on problematic personality features, it becomes difficult to study and validate theoretical models that distinguish between general and specific features in PD.
An alternative approach is to use quantitative techniques to develop structural models that include general and specific features of PD that are statistically distinct. Specifically, a bi-factor approach in which a general factor is estimated distinctly from specific stylistic factors provides a quantitative avenue to directly examine shared and unique variance in personality pathology. However, this approach has only rarely been investigated (Jahng et al., 2011; Sharp et al., 2015; Wolf et al., 2011). Although prior studies included general and specific PD models, they were not designed to broadly validate this approach, and therefore had either no or only a few circumscribed covariates.
Personality Disorder Stability
Stability, which is generally considered a major aspect of PD, can be quantified in various ways (Lenzenweger, Hallquist, & Wright, in press; Morey & Hopwood, 2013). Absolute stability describes the average direction and rate of change in a sample. Low absolute stability implies that the sample as a whole changes over time. Differential stability involves the consistency of relative position among members of the sample, as measured by retest correlations or autoregressive terms. Low differential stability implies individual differences in the direction or rate of change within a sample.
Findings across multi-wave studies of PD (e.g., Cohen et al., 2005; Lenzenweger, 2006; Skodol, Gunderson, et al., 2005; Zanarini et al., 2005) suggest considerably less absolute and differential stability than expected based on longstanding definitions of PD. Significant reductions in absolute levels of PD symptoms have been observed in intervals as brief as one to two years in naturalistic studies (Grilo et al., 2004; Shea et al., 2002; Zanarini, Frankenburg, Hennen, & Silk, 2003) with larger declines over longer follow-up periods (e.g., Gunderson et al., 2011; Zanarini, Frankenberg, Reich, & Fitzmaurice, 2012). Significant absolute change is also found in non-clinical samples, arguing against mere selection effects (Johnson et al., 2000; Lenzenweger, 1999). Similarly, estimates of differential stability, especially when based on diagnostic interview assessments, suggest individuals shift to some degree in their relative positions over time (Lenzenweger, 1999; Samuel et al., 2011; Wright et al., 2015).
However, gross estimates of stability mask considerable nuance in these findings (Morey & Hopwood, 2013). For one, even as the DSM-defined symptom counts decline, relevant domains (e.g., relational and occupational) of psychosocial impairment may exhibit remarkable absolute stability (Gunderson et al., 2011; Skodol, Pagano, et al., 2005). Also, most estimates of stability are based on diagnoses or symptoms organized by DSM-defined disorder, an organization that lacks structural validity. Although there is relatively little research on the topic, examining stability at the level of individual criteria suggests that PDs reflect an amalgam of features that differ in their relative stability (McGlashan et al., 2005; Zanarini et al., 2007).
Establishing the relative stability or instability of various components is a crucial but understudied aspect of developing an evidence-based structure for PD. Moreover, distinguishing PD dimensions based on their stability will direct clinical research efforts toward understanding the mechanisms by which dysfunction is maintained over time. For instance, were the general factor found to have high absolute stability over time, it would suggest that it should be understood as an enduring personality feature in its own right. In contrast, absolute change would indicate that although general features are central to the PD construct, they reflect more dynamic impairments. By the same token, specific factors may capture an individual’s characteristic approach to the world, in which case they would be expected to demonstrate absolute stability, even in the face of declining severity. Alternatively, if unstable, they may reflect fluctuations of style in the context of a shifting identity (Wright et al., 2013). Further, by testing for associations between changes in PD model features and functioning variables, the mechanisms by which dysfunction and PD are maintained can be better understood. Distinguishing the course and correlates of general and specific factors would also be useful for developing interventions of PD that target common and specific features (Kazdin, 2005). Thus, longitudinal data offer considerable power to clarify the nature of PD structure features and validate different aspects of candidate models toward a more clinically useful diagnostic scheme.
The Current Study
The current investigation combines contemporary latent variable modeling techniques with multi-wave assessments of PD to accomplish three interrelated aims. First, we refine a model initially proposed by Hopwood and colleagues (2011) that includes both general and specific factors using a latent variable approach that accounts for measurement error. Personality traits and functioning variables assessed in parallel aid in the interpretation of the resulting structure and serve as cross-sectional validators of the model. Second, we examine patterns of absolute stability to determine whether it is general or specific aspects of PD that are responsible for observed declines in symptoms. Third, we examine the longitudinal associations, both in prospective prediction and shared change, between general and specific factors and functioning variables. We use the Collaborative Longitudinal Personality Study (CLPS) dataset (Skodol, Gunderson, et al., 2005), which followed a large group of individuals (N=733) diagnosed with PDs or with major depressive disorder and no PD over the course of ten years.
Based on prior cross-sectional work with this sample and others, we anticipated that the general features of the disorders would largely drive concurrent associations between PD and functioning, with little in the way of significant associations with specific factors. For absolute stability we generated two alternative hypotheses. One possibility is the general PD factor accounts for the well-documented longitudinal symptomatic decline shared across PDs, while specific PD factors remain stable reflecting an individual’s core personality style. Alternatively, the specific features abate and general PD features remain relatively stable given longitudinal stability in dysfunction. Either is plausible, and the current methodology allows for determining which is the case, as well as ruling out the possibility that both decline in synchrony. Finally, we predicted that PD factors would not only concurrently associate with dysfunction, but that they would also prospectively predict differential change in dysfunction. We expected that the opposite would not be true, such that dysfunction would not predict changes in PD features.
Method
Sample and Procedure
Participants were 733 individuals recruited from one of four cities in the northeastern United States with one of four PDs from among avoidant, borderline, obsessive-compulsive, and schizotypal, or major depressive disorder without PD. Of these, 506 were European-American, 108 African-American, 94 Hispanic, 16 Asian-American, and 10 reported other ethnicities; 467 were women and 266 were men. Participants were nominated by treating clinicians and screened into the study based on scores on structured diagnostic interviews. Participants were assessed at multiple time points, including the baseline, 2- (n = 605), 4- (n = 596), 6- (n = 522), and 10-year (n = 431) follow-ups focused upon in this study. The study was naturalistic, so although many patients received treatment at various points during the study, this was not controlled nor was it required for participation. Extensive additional detail about the sample and procedure can be found in Skodol, Gunderson, and colleagues (2005).
Measures
Personality Disorder Symptoms
The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini, Frankenburg, Sickel, & Yong, 1996), a semistructured interview, assesses each of the 10 personality disorders on DSM-IV Axis II with acceptable reliability (median inter-rater κ = .92; median retest κ = .68; Zanarini, Frankenburg, Chauncey, & Gunderson, 1987; Zanarini et al., 2000). All study participants were assessed with the DIPD-IV at baseline to determine study eligibility, and blinded assessments recurred at 2-, 4-, 6-, and 10-year follow-ups.
Basic Personality Traits
The Revised NEO Personality Inventory (NEO-PI-R; Costa & McCrae, 1992) is a self-report questionnaire designed to assess the Five Factor Model traits neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness as well as 30 lower-order facets. The NEO-PI-R was administered at baseline, 2-, 4- and 6-year study follow-ups. Internal consistency coefficients for the FFM domains in this sample ranged from .88 to .92 at baseline.
Pathological Personality Traits
The Schedule for Nonadaptive and Adaptive Personality (SNAP; Clark, 1993) is a 375-item, self-report questionnaire designed to assess 15 personality characteristics in both the normal (3 traits) and abnormal (12 traits) range. Median internal consistency values of .89 for the higher order scales and .84 for the lower order scales were observed in the CLPS sample (Morey et al., 2003). The SNAP was administered at baseline and 10-year follow-up.
Psychosocial Functioning
The Longitudinal Interval Follow-up Examination (LIFE; Keller et al., 1987), a semistructured interview, measures variables including DSM-IV Global Assessment of Functioning and social, occupational, and leisure dysfunction. The occupational and leisure dysfunction markers are derived from single items. Social functioning was indexed by averaging ratings across several kinds of relationships (e.g., romantic partner, friends, and family members). The LIFE was administered at baseline, 2-, 4- and 6-year study follow-ups.
Data Analysis
All models were estimated in Mplus Version 7.4 (Muthén & Muthén, 1998–2015) and used the observed DIPD-IV dimensions for the 10 DSM PDs as indicators for latent PD factors in the measurement model. We used multilevel SEM (MSEM; Muthén, 1994) because by collapsing across assessment waves, many fewer estimated parameters are needed to achieve a stable and adequately fitting model. Similarly, because a standard SEM would treat each wave as unique when estimating differential stability and associations with external variables, there is the potential to find significant differences of minor substantive import in specific parameters across waves, leading to interpretations that are unlikely to generalize. Such differences are particularly likely in a large sample, spanning a broad mix of developmental stages (i.e., any given two-year period would be expected to be similar for the parameters of interest). By this token, the repeated waves contribute to a more reliable estimate of concurrent and longitudinal associations. This approach carries the assumption of stationarity and equilibrium (i.e., that regression paths, variances, and covariances are the same across waves) in the effects. Although this is a reasonable assumption for the middle waves, it may not be the case for the baseline wave, which might differ due to selection effects, and 10-year follow-up, which is separated from the previous wave by four years instead of two. We therefore reran all models excluding baseline or 10-year follow up as sensitivity analyses. Only a within-person model was estimated, as the goal was not to distinguish between within- and between-person structures, but rather use MSEM to create a flexible and stable modeling framework. Between-person variance was not removed from the analyzed covariance matrix, although all parameters and standard errors were corrected for dependencies in the data due to nesting within participants.
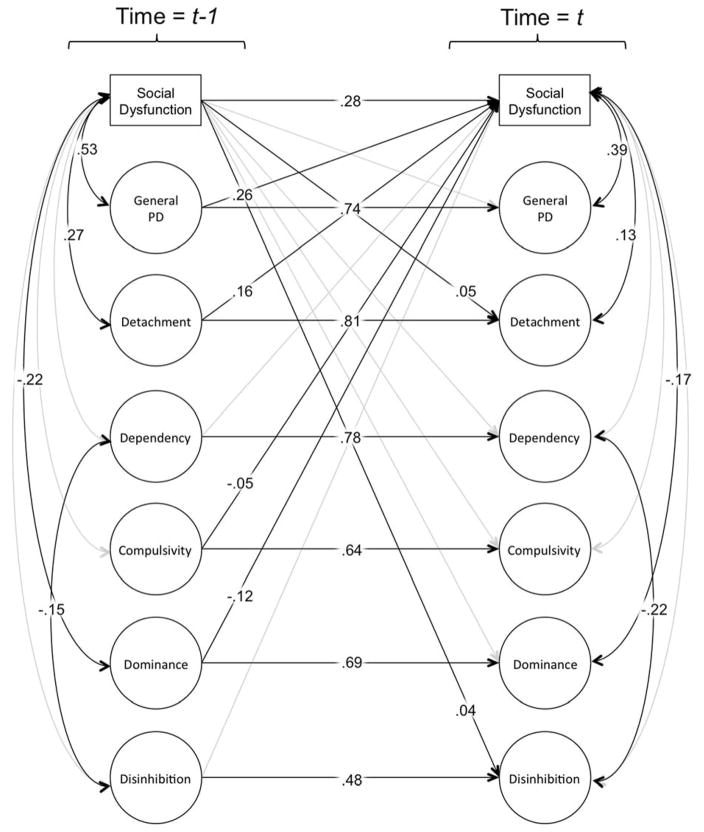
Initially we estimated a MSEM measurement model that pooled across all assessment waves. Concurrent validity and factor interpretation was established by regressing the basic (NEO-PI-R scales) and pathological personality traits (SNAP scales) on the general and all specific factors simultaneously. To test absolute change (i.e., mean differences between waves), we coded each wave using a dummy variable (1=wave), and predicted the latent PD factors. We subsequently estimated autoregressive cross-lagged models (see Figure 3 for an example diagram) to establish associations between PD factors and functioning, including concurrent associations, prediction of change between waves, and covariation in change.
Figure 3.
Diagram of multilevel autoregressive/cross-lagged change structural equation model for Social Dysfunction and latent personality disorder domains. For ease of communication, only the latent personality disorder dimensions, the observed functioning variable, and estimated regression paths and covariances are depicted. All coefficient values reflect standardized estimates. Grayed paths were non-significant at p < .05. Covariances among variables at t−1 reflect cross-sectional associations at a given assessment, whereas covariance among variables at t reflect associations among changes in variables between time-points.
All models were estimated using robust maximum likelihood estimation (MLR estimator) with the resulting Yuan-Bentler χ2, as well as fit indices and standard errors corrected for non-normality. Due to the large size of the sample (Participant N = 733; Observation N = 3,665) and large number of variables included in the models, the χ2 test was de-emphasized, and instead models were judged as acceptable when three out of four of the following indexes met these cutoffs for good/adequate fit: root mean square error of approximation (RMSEA) < .06/.08; comparative fit index (CFI) ≥ .95/≥ .90; Tucker-Lewis index (TLI) ≥ .95/≥ .90; and standardized root mean squared residual (SRMR) < .06/.08 (Brown, 2015).
Missing Data Handling
All participants had full data on the observed PD symptom dimensions and three out of four of the functioning scales at baseline. At subsequent assessments missing data was as follows: 2-year 17%, 4-year 19%, 6-year 29%, and 10-year follow-up 41% missing. Missing data was due partially to attrition and partially due to study design features. The missingness resulting from attrition was assumed to be missing at random (Little, 2013), and was addressed using the current best-practice approach of full information maximum likelihood (FIML) modeling (Graham, 2009). Due to study design, not all participants received the NEO-PI-R (administered n=610), nor was it administered at the final wave, and the LIFE Employment item was not administered at a given wave to those currently unemployed for reasons unrelated to their mental health. These missing data were assumed to be missing completely at random, and therefore similarly handled using FIML estimation.
Results
Measurement Model
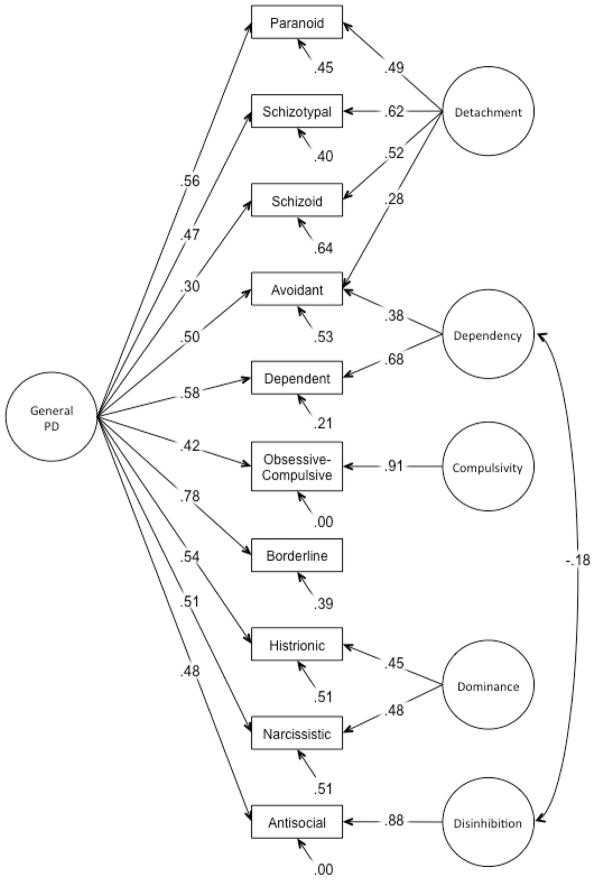
We initially estimated a measurement model with a general factor, on which all 10 DIPD-IV scales freely loaded. In this model the specific factors were as follows: Factor 1 had free loadings from schizotypal, paranoid, and schizoid PD, Factor 2 from avoidant and dependent PDs, Factor 3 from histrionic, borderline, narcissistic, and antisocial PDs, and Factor 4 was solely indicated by obsessive-compulsive PD. In evaluating this model, we found that borderline PD did not load significantly on the specific factor, nor was there an alternative loading suggested by a modification index, and was allowed to only load on the general factor. This is consistent with other research that shows borderline PD to primarily be a marker of general PD (Sharp et al., 2015). Subsequently antisocial PD was no longer found to have a sizeable loading with narcissistic and histrionic PDs on this factor, and was therefore treated as a single indicator specific factor labeled Disinhibition. Thus narcissistic and histrionic PDs were retained as the indicators of a specific factor now interpreted as Dominance. For the factor indicated by schizotypal, schizoid and paranoid PD, we also allowed a loading from avoidant PD based on modification indices, and it was labeled Detachment. We labeled the factor with loadings from dependent and avoidant PD, Dependency. Residual variation in obsessive-compulsive PD was also treated as a single indicator specific factor, consistent with findings of its uniqueness relative to other PDs (e.g., O’Connor, 2005). Finally, we allowed the Dependency and Disinhibition factors to freely correlate based on a large modification index. The revised measurement model had good fit (χ2(26) = 196.28, p < .001; RMSEA = .048; CFI = .96; TLI = .92; SRMR = .036). The final standardized MSEM model is depicted in Figure 1.
Figure 1.
Diagram of multilevel confirmatory factor analysis model of general and specific personality disorder dimensions. Diagramed parameters are from fully standardized model, and thus all factor variances = 1.0. Model was estimated based on data from baseline, 2-year, 4-year, 6-year, and 10-year follow-up assessments. Model fit was as follows: χ2(26) = 196.28, p < .001; RMSEA = .048; CFI = .96; TLI = .92; SRMR = .036.
Concurrent Regressions
As a first step toward validating and more precisely interpreting the general and specific factors, we regressed NEO-PI-R and SNAP scales on the PD factors simultaneously. All models achieved good fit by our criteria, and regression paths are summarized in Table 1 (NEO-PI-R facet coefficients can be found in the supplemental material). We found that general PD was positively associated with Neuroticism, and negatively associated with Agreeableness and Conscientiousness, consistent with the major trait differences between those with and without PD diagnoses (e.g., Morey et al., 2002). General PD also exhibited significant positive associations with all SNAP scales except Positive Temperament and Exhibitionism. Detachment was associated negatively with Extraversion, Agreeableness, and Openness, and was most strongly associated with SNAP Detachment, Mistrust, and Eccentric Perceptions. The Dependency factor associated negatively with Extraversion and Conscientiousness but positively with Agreeableness and Neuroticism. Additionally, Dependency associated most strongly with SNAP Dependency, as well as negatively with Positive Temperament, Exhibitionism, and Entitlement. Dominance was so named in part due to positive associations with SNAP Positive Temperament, Exhibitionism, and Entitlement, and NEO-PI-R Extraversion, as well negative associations with Agreeableness, Neuroticism, and Negative Temperament. As expected, Compulsivity exhibited a positive association with Conscientiousness and SNAP Workaholism. Disinhibition exhibited fewer significant associations with NEO-PI-R domains and facets, although it had the only significant positive associations with SNAP Disinhibition and Impulsivity, consistent with the Externalizing nature of these features. Disinhibition was negatively associated with SNAP Negative Temperament and Neuroticism. Due to the generally non-significant or modest associations with the broad range of traits, the Disinhibition factor is best interpreted with caution, as it may contain relatively little in the way of unique variance relative to residual error.
Table 1.
Contemporaneous associations of personality disorder factors with basic and pathological personality traits
| General PD
|
Detachment
|
Dependency
|
Dominance
|
Disinhibition
|
Compulsivity
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | β | SE | β | SE | β | SE | |
| NEO-PI-R Scales | ||||||||||||
| Extraversion | −.09* | .04 | −.43*** | .04 | −.35*** | .03 | .11* | .05 | .02 | .03 | .02 | .02 |
| Agreeableness | −.31*** | .03 | −.24*** | .04 | .20*** | .05 | −.22*** | .04 | −.05 | .03 | −.06 | .03 |
| Conscientiousness | −.28*** | .04 | .05 | .04 | −.21*** | .05 | .06 | .04 | −.03 | .03 | .17*** | .03 |
| Neuroticism | .55*** | .03 | .04 | .04 | .31*** | .03 | −.13** | .05 | −.10*** | .03 | −.05* | .02 |
| Openness | .00 | .03 | −.24*** | .04 | −.11** | .04 | .06 | .04 | −.08* | .03 | .00 | .03 |
| SNAP Scales | ||||||||||||
| Negative Temperament | .61*** | .03 | .01 | .04 | −.06 | .03 | −.24*** | .03 | −.13*** | .03 | .03 | .03 |
| Positive Temperament | −.06 | .04 | −.15*** | .04 | −.33*** | .04 | .19*** | .04 | .06 | .04 | .18*** | .03 |
| Disinhibition | .34*** | .04 | .00 | .04 | −.03 | .04 | .10* | .05 | .23*** | .03 | −.15*** | .03 |
| Mistrust | .56*** | .03 | .34*** | .04 | −.10** | .03 | −.17*** | .04 | −.05 | .03 | .01 | .02 |
| Manipulativeness | .40*** | .03 | .06 | .04 | −.03 | .03 | .12* | .05 | .14*** | .03 | −.05 | .03 |
| Aggression | .56*** | .03 | .07 | .04 | −.21*** | .03 | −.13** | .05 | .01 | .04 | .05 | .03 |
| Self-Harm | .67*** | .02 | .03 | .04 | .16*** | .03 | −.34*** | .04 | −.03 | .03 | −.14*** | .02 |
| Eccentric Perceptions | .51*** | .03 | .22*** | .05 | −.24*** | .05 | −.13** | .04 | −.09** | .03 | .03 | .03 |
| Dependency | .29*** | .03 | −.03 | .04 | .48*** | .04 | .05 | .03 | .01 | .03 | −.03 | .03 |
| Exhibitionism | .07 | .04 | −.15*** | .04 | −.28*** | .04 | .42*** | .05 | .07 | .04 | .03 | .03 |
| Entitlement | .07* | .04 | .07 | .04 | −.35*** | .04 | .28*** | .05 | .03 | .03 | .11*** | .03 |
| Detachment | .23*** | .04 | .43*** | .04 | .24*** | .03 | −.13** | .04 | .03 | .03 | .07** | .03 |
| Impulsivity | .31*** | .04 | −.09* | .04 | −.03 | .04 | .02 | .03 | .11** | .04 | −.14*** | .03 |
| Propriety | .12*** | .03 | .18*** | .04 | .03 | .04 | −.08 | .05 | −.03 | .03 | .17*** | .03 |
| Workaholism | .23*** | .04 | .01 | .04 | −.15*** | .04 | −.08 | .04 | −.08* | .03 | .33*** | .03 |
Note. Beta coefficients are standardized, and reflect the contemporaneous associations pooled across assessments and estimated from a multilevel structural equation model.
p < .05;
p < .01;
p < .001
In terms of concurrent associations with functioning (see Table 3 second to right column), as anticipated the largest effects were for general personality pathology. However, Detachment additionally1 predicted worse functioning in each domain, whereas Dominance predicted better functioning in each domain.
Table 3.
Coefficients for autoregressive/cross-lagged change models.
| Autoregressive Paths | Cross-Lagged Paths | Covariation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
PD
 Functioning Functioning |
Functioning
 PD PD |
Concurrent | Change/Innovation | |||||||
|
| ||||||||||
| β | SE | β | SE | β | SE | r | SE | r | SE | |
| Social | .28*** | .03 | ||||||||
| General PD | .74*** | .02 | .26*** | .03 | .04 | .02 | .53*** | .02 | .39*** | .03 |
| Detachment | .81*** | .03 | .16*** | .03 | .05* | .02 | .27*** | .03 | .13** | .04 |
| Dependency | .78*** | .04 | −.01 | .03 | −.01 | .02 | .03 | .03 | .02 | .04 |
| Dominance | .69*** | .06 | −.12*** | .03 | −.07 | .04 | −.22*** | .04 | −.17*** | .04 |
| Disinhibition | .48*** | .04 | .02 | .02 | .04* | .02 | .02 | .03 | −.02 | .02 |
| Compulsivity | .64*** | .02 | −.05** | .02 | .02 | .03 | −.03 | .03 | −.02 | .02 |
| Employment | .30*** | .05 | ||||||||
| General PD | .75*** | .02 | .17*** | .04 | .05 | .03 | .44*** | .03 | .35*** | .04 |
| Detachment | .83*** | .03 | .13*** | .03 | .03 | .03 | .17*** | .05 | −.02 | .06 |
| Dependency | .78*** | .04 | .03 | .04 | −.01 | .03 | .01 | .04 | −.04 | .06 |
| Dominance | .69*** | .08 | −.13** | .05 | −.09 | .05 | −.23*** | .05 | −.10 | .06 |
| Disinhibition | .48*** | .05 | .06 | .03 | .02 | .03 | .07* | .03 | .02 | .03 |
| Compulsivity | .64*** | .02 | −.04 | .02 | −.01 | .04 | −.02 | .05 | −.04 | .03 |
| Leisure | .22*** | .03 | ||||||||
| General PD | .74*** | .02 | .18*** | .03 | .07** | .02 | .39*** | .03 | .28*** | .03 |
| Detachment | .82*** | .03 | .09** | .03 | .06* | .02 | .17*** | .03 | .10** | .04 |
| Dependency | .78*** | .04 | .05 | .03 | .02 | .03 | .09** | .03 | .04 | .04 |
| Dominance | .69*** | .08 | −.16*** | .04 | −.03 | .04 | −.24*** | .04 | −.13** | .05 |
| Disinhibition | .48*** | .05 | .02 | .03 | .01 | .02 | −.07** | .03 | −.08*** | .02 |
| Compulsivity | .64*** | .02 | −.04 | .02 | .02 | .04 | .00 | .05 | −.01 | .02 |
| GAF | .35*** | .04 | ||||||||
| General PD | .73*** | .03 | −.26*** | .033 | −.06** | .02 | −.51*** | .03 | −.37*** | .03 |
| Detachment | .81*** | .04 | −.14*** | .023 | −.07** | .02 | −.24*** | .03 | −.08* | .04 |
| Dependency | .78*** | .08 | .06* | .029 | −0.02 | .02 | .03 | .03 | −.01 | .05 |
| Dominance | .68*** | .05 | .14*** | .038 | .08* | .04 | .32*** | .04 | .22*** | .05 |
| Disinhibition | .48*** | .05 | .02 | .024 | −.05** | .02 | −.01 | .03 | .04 | .02 |
| Compulsivity | .65*** | .02 | .08*** | .016 | −0.01 | .03 | .02 | .04 | .04 | .02 |
Note. All reported regression paths and covariances are standardized. Coefficients estimated from a multilevel structural equation model with values pooled across assessments. GAF = Global Assessment of Functioning. Higher values on the PD factors reflect greater levels of PD. Higher values on Social, Employment, and Leisure domains reflect worse functioning; higher values on GAF reflect better functioning.
p < .05;
p < .01;
p < .001
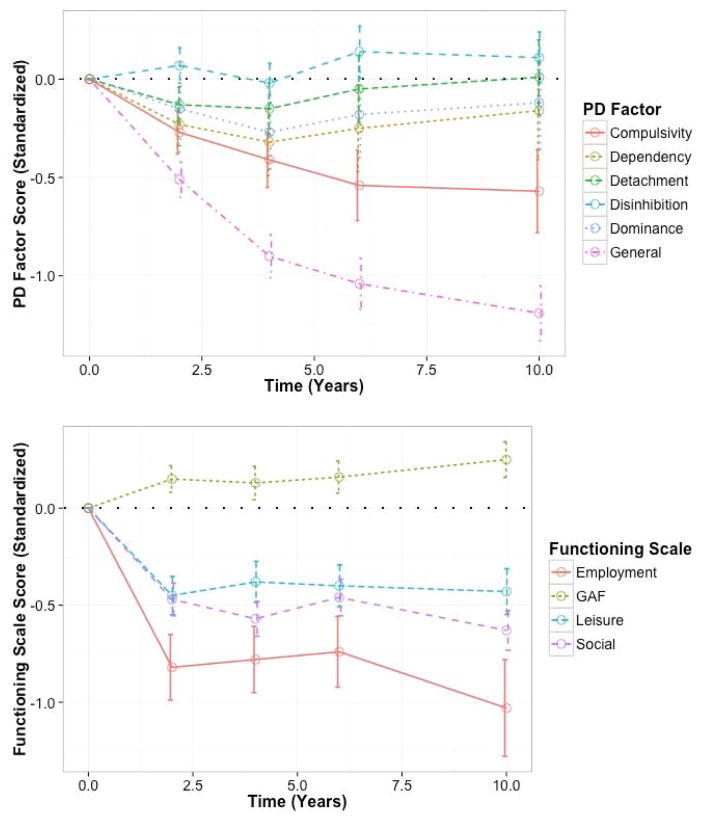
Absolute Change
We next examined absolute or mean change in each PD factor. Values for change since initial assessment as well as plotted means can be found in Table 2 and Figure 2, respectively (see also supplementary Table S2 for values on observed metric). Corresponding values for functioning domains are provided for comparison in the same table and figure. We found significant declines in General PD, with a drop of .5 SDs over the first two years of follow-up, followed by a slowing rate of decline that more than doubled the initial drop over the next eight years. In contrast, rates of change in specific factors were either non-significant, in the case of Detachment, Dominance, and Disinhibition, or much more modest, in the case of Compulsivity and Dependency. This suggests that the observed diagnostic instability and declines in symptoms of PD are largely driven by changes in general PD rather than stylistic factors.
Table 2.
Absolute change in personality disorder factors and functioning scales
| Baseline
|
2 Year
|
4 Year
|
6 Year
|
10 Year
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | Std M | M | SE | Std M | M | SE | Std M | M | SE | Std M | M | SE | Std M | |
| PD Factors | |||||||||||||||
| General PD | 0.00 | -- | 0.00 | −0.42 | 0.04 | −0.51 | −0.73 | 0.05 | −0.90 | −0.85 | 0.06 | −1.04 | −0.97 | 0.07 | −1.19 |
| Detachment | 0.00 | -- | 0.00 | −0.14 | 0.05 | −0.13 | −0.16 | 0.07 | −0.15 | −0.05 | 0.09 | −0.05 | 0.01 | 0.10 | 0.01 |
| Dominance | 0.00 | -- | 0.00 | −0.06 | 0.06 | −0.15 | −0.09 | 0.06 | −0.27 | −0.06 | 0.04 | −0.18 | −0.04 | 0.04 | −0.12 |
| Disinhibition | 0.00 | -- | 0.00 | 0.08 | 0.05 | 0.07 | −0.02 | 0.06 | −0.02 | 0.16 | 0.07 | 0.14 | 0.13 | 0.08 | 0.11 |
| Dependency | 0.00 | -- | 0.00 | −0.23 | 0.06 | −0.23 | −0.32 | 0.10 | −0.32 | −0.25 | 0.13 | −0.25 | −0.16 | 0.14 | −0.16 |
| Compulsivity | 0.00 | -- | 0.00 | −0.53 | 0.08 | −0.31 | −0.74 | 0.10 | −0.44 | −0.86 | 0.11 | −0.51 | −0.89 | 0.12 | −0.53 |
| Functioning | |||||||||||||||
| Social | 0.00 | -- | 0.00 | −0.47 | 0.04 | −0.44 | −0.57 | 0.05 | −0.54 | −0.46 | 0.05 | −0.44 | −0.63 | 0.05 | −0.60 |
| Employment | 0.00 | -- | 0.00 | −0.98 | 0.08 | −0.82 | −0.94 | 0.08 | −0.78 | −0.91 | 0.09 | −0.74 | −1.05 | 0.09 | −1.03 |
| Leisure | 0.00 | -- | 0.00 | −0.53 | 0.06 | −0.45 | −0.44 | 0.06 | −0.38 | −0.44 | 0.06 | −0.40 | 0.47 | 0.06 | −0.43 |
| GAF | 0.00 | -- | 0.00 | 1.99 | 0.46 | 0.15 | 1.53 | 0.52 | 0.13 | 2.09 | 0.56 | 0.16 | 3.35 | 0.60 | 0.25 |
Note. Means estimated in a multilevel structural equation modeling framework, and therefore initial means are fixed to zero, with subsequent means reflecting deviations from initial value. Bolded values are significant at p < .05. Higher values on the PD factors reflect greater levels of PD. Higher values on Social, Employment, and Leisure domains reflect worse functioning; higher values on GAF reflect better functioning. M = unstandardized mean; Std M = mean in standard units.
Figure 2.
Plots of estimated personality disorder (PD) factor scores (top panel) and observed functioning scores (bottom panel). Error bars reflect 95% confidence intervals. Higher values on the PD factors reflect greater levels of PD. Higher values on Social, Employment, and Leisure domains reflect worse functioning; higher values on GAF reflect better functioning.
Functioning exhibited sharp initial declines followed by remarkable stability across all domains (see also Gunderson et al., 2011; Skodol, Pagano, et al., 2005). Indeed, following initially significant declines between assessment waves, differences between subsequent waves were largely non-significant.
Autoregressive/Cross-Lagged Models
Finally, we examined whether one’s standing on general and specific PD factors was predictive of change in functioning, and whether rates of change in PD factors and functioning were associated. In these models, each functioning variable and PD factor at a given wave (t) was regressed on itself (autoregression) at one wave prior (t−1), and the autoregression coefficient is interpreted as the stability in relative position (i.e., rank-ordering) of participants across waves. The residuals are therefore interpreted as change in relative position. Additionally, the functioning variables and the PD factors (t) were regressed on each other, respectively (i.e., cross-lagged), at the wave prior (t−1). Because of the autoregressive paths, these coefficients test the degree to which one’s standing on a predictor variable at a given time-point (t−1) predicts change in the outcome between the same and the subsequent time-point (i.e., between t−1 and t). The factor covariances at t−1 provide an estimate of concurrent associations among constructs, and therefore the contemporaneous association among PD factors and functioning scales. The covariances among the factor disturbances (i.e., residuals) at t estimate the degree of association in change in the PD factors and functioning scales between waves. Thus, these reflect dynamic associations, or the degree to which one’s change in standing on one variable is coupled with change in standing on the other. Table 3 catalogues relevant parameters for each model. Models all fit the data well based on the criteria outlined above. Starting with the autoregressive paths, we found that the PD factors demonstrated high stability (β’s = ~.6–.8), such that with the exception of the Disinhibition factor (β’s = ~.5) the values met or exceeded the levels of differential stability in pathological traits, and were on par with normative trait dimensions (Morey & Hopwood, 2013). The Disinhibition and Compulsivity factors had relatively lower stability, likely due to the fact that their scores contained both specific and error variance. Functioning was much less stable on average (β’s = ~.3). Although this could be due to the fact that the functioning domains were measured with observed variables, and even single indicators for some, estimating functioning as a single latent factor and running the same model resulted in only marginal improvement in stability (β = .44, SE = .05).
For the cross-lagged paths, the pattern of results suggested that the same factors that are significant predictors of contemporaneous functioning also predict change in functioning between waves. That is, general PD consistently predicted worsening in functioning, as did Detachment, whereas Dominance was generally protective, as was Compulsivity in the case of social functioning and GAF. In contrast, functioning was mostly not a significant predictor of change in PD. GAF, though, did significantly predict change in several PD factors, albeit with much more modest effects. This pattern generally suggests that PD drives levels of functioning as opposed to the other way around. Finally, we found that change between waves in general PD and functioning covaried significantly for all functioning scales. Additionally, change in Detachment was positively associated with change in all variables except Employment, whereas the opposite was true for Dominance. In other words, as individuals increased in Detachment they functioned more poorly, but as they increased in Dominance their functioning improved.
We tested the sensitivity of these model results in two ways. First, autoregressive/cross-lagged models were re-estimated excluding either the first or last wave as a sensitivity test, and we found that results were the same with only minor differences (in the second or third decimal point), and would lead to identical conclusions. Second, we estimated linear growth models and regressed individual differences in functioning trajectories on individual differences in PD factor trajectories. The results were entirely consistent with the associations of change in the cross-lagged models, suggesting these results are robust to methodology and model specification.
Discussion
Over the past two decades research into the structure and temporal stability of PDs has flourished, but these have largely remained separate areas of inquiry. Here we brought these two together by refining and elaborating a measurement model of PD that differentiates between general and specific features, extending the work of Hopwood et al. (2011), in a sample assessed five times over ten years. In so doing we provide important validation for a structural model of PD that includes both general and specific features, as well as gain new insights into the stability of PD. Broadly our findings point to the importance of shared variance for understanding the relationship between PD and psychosocial dysfunction, as well as its stability over time. We additionally found that the specific features serve to augment or attenuate the impact of general PD features. Moreover, our findings suggest that stylistic elements of PD may remain, even as general PD wanes over time.
Interpreting the General and Specific Model of PD
Due in part to high rates of diagnostic covariation (Bornstein, 1998) and in part to theory (e.g., Kernberg, 1984), there has been substantial interest in identifying and understanding the shared and specific features of personality pathology (Bender et al., 2011; Hopwood et al., 2011; Livesley, 1998; Parker et al., 2004; Pincus, 2011). As with prior studies (Jahng et al., 2011; Sharp et al., 2015), here we found robust evidence for a general factor with moderate to strong loadings from each of the PDs, suggesting it truly reflects the shared aspects of these disorders. Further, the pattern of external correlates suggests that these impairments truly are general (in the case of the SNAP), and further reflect impairments in personality maturation (in the case of the NEO-PI-R) (Wright, Pincus, & Lenzenweger, 2011).
However, the core makeup of the general factor remains somewhat ambiguous. One possible interpretation is that it reflects borderline personality organization (Kernberg, 1984), with core impairments involving maladaptive self and other representations and identity formation (Bender et al., 2011). Similar to Sharp et al. (2015) and Williams, Scalco, and Simms (2015) we find that after accounting for borderline PD’s association with the general factor, it no longer shares variance with the other PDs. That is to say, in these data, as in other samples (Sharp et al., 2015; Williams et al., 2015), because we find that borderline PD is the strongest marker of the general factor, and the remaining variance in borderline PD is largely unshared with other PDs, the general factor may reflect the core features of that construct, which are also shared across other PDs (Bender & Skodol, 2007; Fonagy et al., 2002; Kernberg, 1984). Indeed, this may argue against retaining a specific borderline diagnosis. It is interesting to consider that the DSM-III’s criteria for borderline PD were selected, in part, for their ability to patients diagnosed as having borderline personality organization from those who were not by residents in a psychiatric service run by Dr. Otto Kernberg (Spitzer, Endicott, & Gibbon, 1979).
An alternative possibility is that the general factor of PDs is largely equivalent to the general factor that has emerged from models of common mental disorders (e.g., Caspi et al., 2014; Laceulle et al., 2015; Lahey et al., 2012), or what has been termed the ‘p-factor’. Some have argued, based on patterns of external associations (Kotov et al., 2010) and amount of shared variance accounted for (Kahn et al., 2005), that the p-factor may best be understood as largely reflecting the broader personality trait of neuroticism (Lahey et al., 2012). Consistent with this perspective, other prominent theories of borderline PD define it largely in terms of affective dysregulation (Linehan, 1993). Yet beyond neuroticism, in terms of basic traits, general PD was substantially negatively associated with agreeableness and conscientiousness. That PDs in general are associated with these three traits is well established (Morey et al., 2002; Saulsman & Page, 2004), and lends credibility to the results as a whole. Shared variance in these three traits has been hypothesized to arise from individual differences in responsivity of the serotonergic system (DeYoung, 2006), giving rise to global deficits in regulation of affect, interpersonal relatedness, and goal directed behavior.
We also found the specific factors to be interpretable based on prior studies of PD structure that do not consider a general factor and the external correlates of PD. For instance, obsessive-compulsive PD frequently serves as the principal indicator for a unique factor (O’Connor, 2005), and dependent and avoidant PDs also most frequently load on the same factor, here named Dependency (Kotov et al., 2011; Wright & Simms, 2015). Schizotypal, schizoid, and paranoid PDs are frequently, although not always, associated structurally, and their shared variance is often interpreted to represent schizotypy or Psychoticism (Kotov et al., 2016). In our model avoidant PD also serves as an indicator for the factor, suggesting that Detachment best captures the shared variance of these indicators, not Psychoticism. Interestingly, once the general factor was included in the model, the remaining Cluster B PDs differentiated into two factors we labeled Dominance and Disinhibition. This differentiation is supported by other structural work without general variance removed, suggesting histrionic and narcissistic PDs are the strongest markers for an antagonistic domain, whereas the antisocial PD marks an externalizing-disinhibition domain (Kotov et al. 2011; Wright & Simms, 2015).
Stability and Change in General and Specific Components of PD
We next moved to examining the absolute change in each of the factors identified above. The general factor declined significantly and with large effect sizes over time, whereas Dominance, Detachment, and Disinhibition did not significantly decline, and declines in Compulsivity and Dependency were significant but modest. Taken together, these findings suggest the core or shared features of PD are the most malleable component, whereas stylistic individual differences are significantly more stable. These results clarify prior findings from the CLPS and other prospective longitudinal PD studies that have found similar rates of declines across all PDs (e.g., Lenzenweger, 2006; Zanarini et al., 2005), by suggesting shared mechanisms of change over time across the DSM-defined disorders. Thus, while it may be helpful to tailor treatments to individual styles, which represent an important source of heterogeneity in patients with PD, in general effective treatments should target core features that seem to cut across a variety of presentations. Several others have argued that treatment approaches with established validity (largely developed for borderline PD) are unlikely to contain specific ameliorative factors for DSM PD diagnoses, but rather operate via shared pathways (e.g., Paris, 2015; Livesley, Dimaggio, & Clarkin, 2016). These data offer exciting validation of this perspective on PD treatment.
Despite the dramatic decreases in absolute change in general PD, we found high differential stability in this factor as well as most of the specific factors. The exception was Disinhibition, which likely is a methodological artifact due to (a) having a single indicator that blends specific and error variance, and (b) not being a set of features that were heavily sampled in these data (i.e., Compulsivity, also a single indicator variable, had higher differential stability).
The functioning scales differed from the PD factors in their pattern of change. In terms of absolute change, sharp average initial improvements were followed by remarkable mean stability. In contrast, as a group these scales had much lower differential stability, even when modeled as a latent variable. This suggests that in terms of functioning, it is not actually that the sample is stable after the initial decrease, but rather that there is high individual-level fluctuation between assessment points, leading to low differential stability, but with a mean that changes little. So, some individuals improve and others decline between waves, and then they largely shift position with the next wave.
Concurrent and Longitudinal Associations with Functioning
As expected, general PD features exhibited the strongest concurrent associations with all functioning domains. Nevertheless, some specific factors were incrementally associated with functioning. Detachment was found to further amplify impairments in psychosocial functioning, whereas Dominance buffered against these same impairments. These same patterns of associations were found when prospectively predicting change in functioning, and the couplings of change in PD factors and functioning.
At first pass it may seem puzzling that general PD and functioning have the strongest associations, concurrently and longitudinally, but highly discrepant patterns of absolute and differential change. Taken together, these diverse patterns highlight the distinctiveness of absolute and differential change. Descriptively, individuals decline on average while largely maintaining their relative position to each other on general PD features, whereas individuals shift relative position in functioning between time-points. At any given time point, those individuals higher in general PD will have greater dysfunction and are likely to experience declines in functioning between assessments; the opposite is true for those low in general PD. Individual differences in rates of change between assessments track together to some degree for general PD and dysfunction. But what causes these discrepancies? One possibility is that on average the participants are limited by the ability to achieve lasting improvements in psychosocial functioning. Although initial acuity abates, and there is significant marked improvement detectable in the sample (i.e., high absolute stability), this is unsustainable for some individuals (i.e., low differential stability). For instance, employment is obtained, but it is consistently of a lower quality job that lacks stability and security such that the individual cycles in and out of work, family relations are strained and distanced during the more acute period of disorder subsequently experiencing periods of rapprochement and discord, and so on. An alternative but not mutually exclusive interpretation is that PD may push individuals into more adverse environments that result in lower average and less stable achievement. That is, these functioning domains generally involve a transaction between the individual and environment, and therefore gains made at the individual level are only part of the transactional equation. These possibilities signal a need for finer-grained functioning and contextual data.
Vis-à-vis these functional outcomes, the specific factors performed quite distinctly from general PD and from each other. Detachment was an additional risk factor whereas Dominance was protective. The remaining factors were largely unassociated or exhibited the occasional protection or risk. We do not take these findings to suggest that stylistic manifestations are unimportant, but rather that they are unlikely to have major direct effects on these broad outcomes net of general PD. It may be that more specific outcomes would illuminate their importance. Additionally, there is reason to believe that specific features may have a moderating role on general impairments. Studies of personality heterogeneity within diagnoses (including BPD) suggest that differences in personality style moderate important outcomes and course (e.g., Cain et al., 2012; Thomas et al., 2014; Wildes et al., 2012; Wright et al., 2013). Further, it is hard to imagine that specific factors will not be important for tailoring effective treatment. Consider a patient high in Dependency vs. one high in Dominance, the former will likely approach clinicians differently and require different specific interventions than the latter. Although plausible, this observation is in need of future research given the paucity of systematic process-based treatment research as well as research on personality-intervention matching.
Limitations
The CLPS design in which a majority of individuals were diagnosed with at least one of four PDs may have had an effect on our estimated structure and patterns of change over time in unknown ways. This may have been especially problematic for antisocial PD, which was not a selected diagnosis, and therefore it may have led to reduced estimates of stability over time. Our analytic approach, which fit the same structure across five waves and 10 years of data, guarded against undue influence of sampling issues on the structure. Additionally, the effects are unlikely to affect the general factor so much as the specific factors. Therefore, this model may best be understood as providing a stronger test and support for the general factor than for this particular set of specific factors.
Also, we relied on DSM PD dimensions as indicators in our model, which are known to be heterogeneous. Although common factor models still serve to parse shared variance into homogeneous factors, greater sensitivity, and likely greater differentiation, would have been achieved studying structure starting from the symptom level. A full symptom based model, though, would be prohibitively large with the 79 criteria modeled as individual indicators.
An additional issue worth considering is that our measures of functioning were not nearly as comprehensive and in depth as the PD assessments. This could have contributed to the lower estimates of stability. Therefore our estimates of the prospective effect of functioning on PD factor change may be an underestimate. Finally, the assessments did not include major and minor life events, as might allow for the test of certain hypothesized mechanisms of change.
Implications and Future Directions
The PD field is currently engaged in a debate about how best to reformulate the definition and diagnosis of personality pathology. This debate has largely been spurred on by the proposed revisions to the extant DSM PD model, now included as the alternative model for PDs in Section III of DSM-5. There are direct parallels between the structure adopted here and the alternative model. Namely, both attempt to distinguish between features general to PD (Criterion A in the DSM-5 alternative model) and those that account for specific individual differences in its manifestation (Criterion B). Here we partial these distinct sources of variance statistically, whereas the DSM uses a general definition of self and interpersonal impairments and individual differences in pathological personality traits. A challenge facing the Section III model, as currently articulated, is that the indicators of Criterion A and B are highly overlapping in content, and as a result have a high degree of conceptual and psychometric redundancy. One potential way forward is to reduce the redundancy by deleting a portion of the model. However, our findings suggest that there is value in working to distinguish between the shared processes and stylistic differences in their manifestations in order to better understand processes of change over time and associations with external variables.
Achieving this distinction will be challenging, but likely more so from a psychometric than a conceptual stand point. We emphasize that the association between basic personality traits and PDs is not a privileged one, and the association is equally strong with symptom syndromes (e.g., Kotov, Gamez, Schmidt, & Watson, 2010; Wright & Simms, 2015). In this regard personality traits are important diagnostically and prognostically. They therefore represent variables of considerable psychiatric importance that likely deserve inclusion in any diagnostic manual. On the one hand, placing them within a PD model makes strong conceptual sense, but on the other it might lead to greater utility and conceptual clarity to define PD exclusively in terms of the general features, and allow for a distinct coding of personality style using traits that are applicable to all patients.
More broadly, a major lingering question is, how can the notion of “general PD” be integrated within a comprehensive empirically supported model of psychopathology? Testing and validating bi-factor models of common mental disorders has been a popular activity in recent years (Caspi et al., 2014; Laceulle et al., 2015; Lahey et al., 2012), but none of these studies have included PDs in their mixture of indicators. We similarly did not have at our disposal multiple waves of clinical syndromes, precluding a more complete model here. That the “p-factor,” (Caspi et al., 2014) as it is sometimes referred to in clinical syndrome based models, and our general PD factor tap in to similar if not the same aspects of maladaptivity is possible. In those few quantitative structural models of psychopathology that have included both clinical syndromes and PD (e.g., Kotov et al., 2011; Markon, 2010; Wright & Simms, 2015), PDs have spread across identified domains, suggesting that there may be little to argue for distinguishing them from clinical syndromes. At the same time, clinical theories (Bender & Skodol, 2007; Hopwood et al., 2013; Kernberg, 1984; Parker et al., 2004) would suggest that PDs share particular pathological processes that might differentiate them other forms of psychopathology. This assertion should be subjected to direct testing via models that (a) compare joint versus distinguishable general factors for PD and other forms of psychopathology, and (b) if such a distinction is supported then testing for distinguishable patterns of covariates.
Our findings also point to the importance of continued longitudinal work in this area. Major questions remain, such as what are the mechanisms that contribute to marked declines in severity, even as stylistic elements remain? On the one hand, it is easy to point to basic personality trait change, which is well documented to follow the maturity principle that posits increases in emotional stability, agreeableness, conscientiousness, and social dominance as a function of development (Roberts, Walton, & Viechtbauer, 2006). Yet the processes driving change in basic traits are also poorly understood. Better assessments of environmental and social factors, such as major and minor life events, are needed to test transactional hypotheses about change. As an example, the protective effects of Dominance and Compulsivity that serve to mitigate one’s general level of functioning may operate through shared or distinct pathways, or both. For instance, Dominance and Compulsivity may share effects on overall industriousness, but differ in terms of social engagement and lack of impulsivity. Uncovering and understanding these processes would serve to identify specific intervention targets.
Conclusion
In summary, we found that general and specific features of PD can be distinguished using quantitative structural modeling. General PD exhibited lower absolute stability and was most strongly related to broad markers of psychosocial functioning, concurrently and longitudinally, whereas specific features had higher mean stability and exhibited more circumscribed associations with functioning. However, both general and specific factors showed recognizable associations with normative and pathological traits. These findings show that there is value in distinguishing between the general and specific of PD. However, future work should (a) structurally model general and specific variance with a broader set of markers in order to flesh out specific domains, (b) address the psychometric challenges associated with the overlap in content associated with Criterion A and B in the DSM-5 Section III model, (c) examine associations between general PD and structural features from symptom syndromes, and (d) collect data that is amenable to uncovering mechanisms of change in longitudinal data.
Supplementary Material
General Scientific Summary.
This study suggests that personality disorders (PDs) are made up of shared features general to all PDs, as well as relatively more specific stylistic features, and that it is declines in the shared features that account for the observed improvement in these disorders over time. In contrast, the specific features are much more stable.
Acknowledgments
This research was supported by the National Institute of Mental Health (MH50837, MH50838, MH50839, MH50840, MH50850, L30 MH101760). The views contained are solely those of the authors and do not necessarily reflect those of the funding source.
Footnotes
Because the factors in this model are with only one exception uncorrelated, correlations with external variables are largely the same to partial standardized regression coefficients (Cohen, Cohen, Aiken, & West, 2003).
Contributor Information
Aidan G.C. Wright, University of Pittsburgh
Christopher J. Hopwood, Michigan State University
Andrew E. Skodol, University of Arizona
Leslie C. Morey, Texas A & M University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Bastiaansen L, De Fruyt F, Rossi G, Schotte C, Hofmans J. Personality disorder dysfunction versus traits: Structural and conceptual issues. Personality Disorders: Theory, Research, and Treatment. 2013;4(4):293–303. doi: 10.1037/per0000018. [DOI] [PubMed] [Google Scholar]
- Bender DS, Morey LC, Skodol AE. Toward a model for assessing level of personality functioning in DSM-5, part I: A review of theory and methods. Journal of Personality Assessment. 2011;93:332–346. doi: 10.1080/00223891.2011.583808. [DOI] [PubMed] [Google Scholar]
- Bender DS, Skodol AE. Borderline personality as a self- other representational disturbance. Journal of Personality Disorders. 2007;21:500–517. doi: 10.1521/pedi.2007.21.5.500. [DOI] [PubMed] [Google Scholar]
- Bernstein RF. Reconceptualizing personality disorder diagnosis in the DSM–V: The discriminant validity challenge. Clinical Psychology: Science and Practice. 1998;5:333–343. [Google Scholar]
- Bornstein RF. Reconceptualizing personality disorder diagnosis in the DSM-V: The discriminant validity challenge. Clinical Psychology: Science and Practice. 1998;5:333–343. [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. 2. New York, NY: Guilford Publications; 2015. [Google Scholar]
- Cain NM, Ansell EB, Wright AGC, Hopwood CJ, Thomas KM, Pinto AN, … Grilo CM. Interpersonal pathoplasticity in the course of major depressi on. Journal of Consulting and Clinical Psychology. 2012;80(1):78–86. doi: 10.1037/a0026433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor CJ, Harrington H, Israel S, … Moffitt TE. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA. Manual for the Schedule of Nonadaptive and Adaptive Personality. Minneapolis: University of Minnesota Press; 1993. [Google Scholar]
- Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. Journal of personality disorders. 2005;19(5):466–486. doi: 10.1521/pedi.2005.19.5.466. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. NEO Personality Inventory Revised professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Creswell KG, Bachrach RB, Wright AGC, Pinto AL, Ansell EB. Predicting problematic alcohol use with the DSM-5 alternative model of personality pathology. Personality Disorders: Theory, Research, and Treatment. 2016;7(1):103–111. doi: 10.1037/per0000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeYoung CG. Higher-order factors of the Big Five in a multi-informant sample. Journal of personality and social psychology. 2006;91(6):1138–1151. doi: 10.1037/0022-3514.91.6.1138. [DOI] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, … MacKillop J. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. Journal of abnormal psychology. 2013;122(4):1057–1069. doi: 10.1037/a0034878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonagy P, Gergely G, Jurist EL, Target M. Affect regulation, mentalization, and the development of self. New York, NY: Other Press; 2002. [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual review of psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Sanislow CA, Gunderson JG, Pagano ME, Yen S, Zanarini MC, … McGlashan TH. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Journal of consulting and clinical psychology. 2004;72(5):767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ. Personality traits in the DSM–5. Journal of Personality Assessment. 2011;93(4):398–405. doi: 10.1080/00223891.2011.577472. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Malone JC, Ansell EB, Sanislow CA, Grilo CM, McGlashan TH, … Morey LC. Personality Assessment in DSM--5: Empirical support for rating Severity, Style, and Traits. Journal of Personality Disorders. 2011;25(3):305–320. doi: 10.1521/pedi.2011.25.3.305. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM-IV personality disorders. Journal of Abnormal Psychology. 2012;121(2):424–432. doi: 10.1037/a0026656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SE. The diagnosis of mental disorders: the problem of reification. Annual Review of Clinical Psychology. 2010;6:155–179. doi: 10.1146/annurev.clinpsy.3.022806.091532. [DOI] [PubMed] [Google Scholar]
- Jahng S, Trull TJ, Wood PK, Tragesser SL, Tomko R, Grant JD, … Sher KJ. Distinguishing general and specific personality disorder features and implications for substance dependence comorbidity. Journal of abnormal psychology. 2011;120:656–669. doi: 10.1037/a0023539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: a community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102(4):265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Treatment outcomes, common factors, and continued neglect of mechanisms of change. Clinical Psychology: Science and Practice. 2005;12(2):184–188. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby M, … Zimmerman M. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. 2016 doi: 10.1037/abn0000258. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Kernberg OF. Severe personality disorders: Psychotherapeutic strategies. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF. Personality disorders are the vanguard of the post-DSM-5.0 era. Personality Disorders: Theory, Research, and Treatment. 2013;4(4):355–362. doi: 10.1037/per0000028. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR. Personality traits and the classification of mental disorders: Toward a more complete integration in DSM–5 and an empirical model of psychopathology. Personality Disorders: Theory, Research, and Treatment. 2010;1(2):97–118. doi: 10.1037/a0018990. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Skodol AE, Livesley WJ, Shrout PE, Huang Y. Synthesizing dimensional and categorical approaches to personality disorders: refining the research agenda for DSM-V Axis II. International Journal of Methods in Psychiatric Research. 2007;16(1):S65–S73. doi: 10.1002/mpr.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laceulle OM, Vollebergh WA, Ormel J. The structure of psychopathology in adolescence replication of a general psychopathology factor in the TRAILS Study. Clinical Psychological Science. 2015;3:850–860. [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF. Stability and change in personality disorder features: The longitudinal study of personality disorders. Archives of General Psychiatry. 1999;56:1009–1015. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. The longitudinal study of personality disorders: History, design considerations, and initial findings. Journal of Personality Disorders. 2006;20(6):645–670. doi: 10.1521/pedi.2006.20.6.645. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Hallquist MN, Wright AGC. Understanding stability and change in the personality disorders: Methodological and substantive issues underpinning interpretive challenges in the road ahead. In: Livesley J, Larstone R, editors. Handbook of personality disorders. 2. New York: Guilford; in press. [Google Scholar]
- Lenzenweger MF, Johnson MD, Willett JB. Individual Growth Curve Analysis Illuminates Stability and Change in Personality Disorder Features: The Longitudinal Study of Personality Disorders. Archives of General Psychiatry. 2004;61(10):1015–1024. doi: 10.1001/archpsyc.61.10.1015. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Little TD. Longitudinal structural equation modeling. New York, NY: Guilford Press; 2013. [Google Scholar]
- Livesley WJ. Suggestions for a framework for an empirically based classification of personality disorder. Canadian Journal of Psychiatry. 1998;43:137–147. doi: 10.1177/070674379804300202. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. General Assessment of Personality Disorder (GAPD) Department of Psychiatry, University of British Columbia; 2006. [Google Scholar]
- Livesley WJ, Dimaggio G, Clarkin JF. Integrated treatment for personality disorder: A modular approach. New York: Guilford; 2016. [Google Scholar]
- McGlashan TH, Grilo CM, Sanislow CA, Ralevski E, Morey LC, Gunderson JG, … Pagano M. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: toward a hybrid model of axis II disorders. American Journal of Psychiatry. 2005;162:883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Morey LC, Benson KT, Skodol AE. Relating DSM-5 section III personality traits to section II personality disorder diagnoses. Psychological Medicine. 2016;46:647–655. doi: 10.1017/S0033291715002226. [DOI] [PubMed] [Google Scholar]
- Morey LC, Gunderson JG, Quigley BD, Shea MT, Skodol AE, McGlashan TH, et al. The representation of borderline, avoidant, obsessive-compulsive, and schizotypal personality disorders by the five-factor model. Journal of Personality Disorders. 2002;16:215–234. doi: 10.1521/pedi.16.3.215.22541. [DOI] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ. Stability and change in personality disorders. Annual review of clinical psychology. 2013;9:499–528. doi: 10.1146/annurev-clinpsy-050212-185637. [DOI] [PubMed] [Google Scholar]
- Muthén BO. Multilevel covariance structure analysis. Sociological Methods & Research. 1994;22:376–398. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: 1998–2015. [Google Scholar]
- O’Connor BP. A search for consensus on the dimensional structure of personality disorders. Journal of Clinical Psychology. 2005;61:323–345. doi: 10.1002/jclp.20017. [DOI] [PubMed] [Google Scholar]
- Parker G, Hadzi-Pavlovic D, Both L, Kumar S, Wilhelm L, Olley A. Measuring disordered personality functioning: To love and work reprised. Acta Psychiatrica Scandinavica. 2004;110:230–239. doi: 10.1111/j.1600-0447.2004.00312.x. [DOI] [PubMed] [Google Scholar]
- Paris J. A concise guide to personality disorders. Washington, D.C: American Psychological Association; 2015. [Google Scholar]
- Pincus AL. A contemporary integrative interpersonal theory of personality disorders. In: Clarkin J, Lenzenweger M, editors. Major theories of personality disorder. 2. New York: Guilford; 2005. pp. 282–331. [Google Scholar]
- Pincus AL. Some comments on nomology, diagnostic process, and narcissistic personality disorder in the DSM-5 proposal for personality and personality disorders. Personality Disorders: Theory, Research, and Treatment. 2011;2(1):41–53. doi: 10.1037/a0021191. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Hopwood CJ, Ansell EB, Morey LC, Sanislow CA, Markowitz JC, … Grilo CM. Comparing the temporal stability of self-report and interview assessed personality disorder. Journal of abnormal psychology. 2011;120(3):670–680. doi: 10.1037/a0022647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23(8):1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- Sharp C, Wright AGC, Fowler JC, Freuh C, Allen JG, Oldham J, Clark LA. The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology. 2015;124(2):387–398. doi: 10.1037/abn0000033. [DOI] [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, … Keller MB. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. American Journal of Psychiatry. 2002;159(12):2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- Skodol AE. Personality disorders in DSM-5. Annual Review of Clinical Psychology. 2012;8:317–344. doi: 10.1146/annurev-clinpsy-032511-143131. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, … Stout RL. The collaborative longitudinal personality disorders study (CLPS): Overview and implications. Journal of Personality Disorders. 2005;19(5):487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Morey LC, Bender DS, Oldham JM. The alternative DSM-5 model for personality disorders: A clinical application. American Journal of Psychiatry. 2015;172:606–613. doi: 10.1176/appi.ajp.2015.14101220. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Pagano ME, Bender DS, Tracie Shea M, Gunderson JG, Yen S, … McGlashan TH. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive–compulsive personality disorder over two years. Psychological Medicine. 2005;35(03):443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality and borderline schizophrenia: The development of criteria. Archives of General Psychiatry. 1979;36(1):17–24. doi: 10.1001/archpsyc.1979.01780010023001. [DOI] [PubMed] [Google Scholar]
- Tyrer P, Johnson T. Establishing the severity of personality disorder. American Journal of Psychiatry. 1996;153:1593–1597. doi: 10.1176/ajp.153.12.1593. [DOI] [PubMed] [Google Scholar]
- Thomas KM, Hopwood CJ, Donnellan MB, Wright AGC, McDevitt-Murphy ME, … Morey LC. Personality heterogeneity in PTSD: Distinct temperamental and interpersonal typologies. Psychological Assessment. 2014;26(1):23–34. doi: 10.1037/a0034318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheul R, Andrea H, Berghout CC, Dolan C, Busschbach JJV, van der Kroft PJA, … Fonagy P. Severity Indices of Personality Problems (SIPP-118): Development, factor structure, reliability, and validity. Psychological Assessment. 2008;20:23–34. doi: 10.1037/1040-3590.20.1.23. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Clark LA. Toward DSM—V and the classification of psychopathology. Psychological Bulletin. 2000;126(6):946–963. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Rogers JH. Prevalence and comorbidity of personality disorders. Psychiatric Annals. 1989:132–136. [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. American Psychologist. 2007;62(2):71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Crosby RD, Ringham RM, Dapelo MM, Gaskill JA, Forbush KT. The clinical utility of personality subtypes in patients with anorexia nervosa. Journal of Consulting and Clinical psychology. 2011;79(5):665–674. doi: 10.1037/a0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams TF, Scalco MD, Simms LJ. Examining the structural and construct validity of general and specific dimensions of personality pathology. 2015 doi: 10.1017/S0033291717002227. Manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Brown TA. The structure of personality disorders in individuals with posttraumatic stress disorder. Personality Disorders: Theory, Research, and Treatment. 2011;2(4):261–278. doi: 10.1037/a0023168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Calabrese WR, Rudick MM, Yam WH, Zelazny K, Rotterman J, Simms LJ. Stability of the DSM-5 Section III pathological personality traits and their longitudinal associations with functioning in personality disordered individuals. Journal of Abnormal Psychology. 2015;124(1):199–207. doi: 10.1037/abn0000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Beeney JE, Pilkonis PA. Borderline personality pathology and the stability of interpersonal problems. Journal of Abnormal Psychology. 2013;122(4):1094–1100. doi: 10.1037/a0034658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Morse JQ, Scott LN, Stepp SD, Nolf KA, Pilkonis PA. Clarifying interpersonal heterogeneity in borderline personality disorder using latent mixture modeling. Journal of Personality Disorders. 2013;27(2):125–143. doi: 10.1521/pedi.2013.27.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The structure of psychopathology: toward an expanded quantitative empirical model. Journal of Abnormal Psychology. 2013;122:281–294. doi: 10.1037/a0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. Development of personality and the remission and onset of personality pathology. Journal of Personality and Social Psychology. 2011;101(6):1351–1358. doi: 10.1037/a0025557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. Journal of personality disorders. 2005;19(5):505–523. doi: 10.1521/pedi.2005.19.5.505. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry. 2003;160:274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and axis II comparison subjects: a 16-year prospective follow-up study. American Journal of Psychiatry. 2012;169(5):476–483. doi: 10.1176/appi.ajp.2011.11101550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. American Journal of Psychiatry. 2007;164(6):929–935. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The diagnostic interview for DSM-IV personality disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, … Gunderson JG. The collaborative longitudinal personality disorders study: Reliability of axis I and II diagnoses. Journal of personality disorders. 2000;14(4):291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.