Abstract
Background and Aims
This study focused on the difference between perceived and desired physician empathy (pPE and dPE) in the eye of patients with inflammatory bowel disease (IBD). It was investigated if a discrepancy (ΔPE) correlates with trust and satisfaction of patients. At the same time the aim was to gain detailed information about the subjective burden of disease and the resources of IBD patients, in order to better understand them.
Methods
A modified version of the German Version of the Consultation and Relational Empathy (CARE) measure was completed as a paper-and-pencil questionnaire by IBD patients attending our facility (n = 32) and as an online survey by IBD patients at other locations throughout Germany (n = 89). Patients were in average 36.3±12 years old.
Results
The mean (SD) rating of pPE was 3.93 (0.96) on a scale of 1 to 5 (“poor” to “excellent”); however, the mean (SD) dPE was 4.38 (0.48) on the same scale. ΔPE correlated with perceived empathy and with patients’ satisfaction with treatment and trust in their health care providers. Patients reported quite a high subjective burden (mean [SD]: 2.93 [.63]) and named family, friends, and support groups as resources.
Conclusions
Rather than assessing patient satisfaction with treatment and trust in their physician only with perceived PE, we suggest ΔPE as a useful additional parameter.
Introduction
Inflammatory bowel disease (IBD) represents a group of chronic conditions with a relapsing-remitting course. Most patients are young: 20% of patients develop the first symptoms during childhood, and 5% are diagnosed before their 10th year. In the last century, a psychosomatic origin of the disease was suggested. Nowadays, the pathogenesis is better understood, and a current concept of the disease is a breakdown of the intestinal epithelial barrier with infiltration by cells of the innate and adaptive immune systems, which release a number of cytokines. These cytokines may pass the blood-brain barrier and cause neurologic and behavioral changes [1]. The early onset and need for lifelong treatment are responsible for a high burden of disease and reduced quality of life [2]. Patients often tend to deny their condition and become inconsistent with their schedule of follow-up visits and laboratory tests and less adherent to medical therapy [3]. Consequently, IBD patients represent a challenging group for the treating gastroenterologists and surgeons.
Empathy has received much attention as a research topic in the past decades and yet there is no general agreement about its definition. For this study, we used the concept of empathy defined by Mercer and Reynolds [4]. These authors have identified four components of empathy: an emotional component (the ability to share patients’ feelings), a moral component (the physician’s intrinsic motivation for empathic behavior), a cognitive component (the ability to identify and understand patients’ feelings), and a behavioral component (the physician’s ability to show understanding and even partly share patients’ feelings and the will to find solutions). The fourth component is probably the most important, because it represents the “feedback” that patients actually receive.
There are reports that pain and fear can be reduced if patients perceive high physician empathy (PE) [5]. Also, PE enables patients to better cope with their disease and situation [6]. In cancer patients, high perceived PE correlates with a lower rate of depression and higher satisfaction with treatment [7]. So far, the relevance of PE has been investigated in several studies that focused mainly on cancer patients [8] and diabetes patients [9]. In the recent literature, some studies examined the role of PE in hand and trauma surgery [10, 11]. To our knowledge, however, no study has focused on PE in IBD patients. A PubMed search with the terms “inflammatory bowel disease AND “physician empathy” delivered two results [3, 12]; and a search with the terms “inflammatory bowel disease” AND “empathy,” five [3, 12, 13, 14, 15]. The publication by Burish (2014) reports on the recent ECCO-Epicom study on quality of care in Eastern and Western Europe; one of the items on the questionnaire used in this study was “empathy,” which the study defined as “interest in how IBD impacts the quality of life of patients” and “showing appropriate courtesy” [13].
Most studies have used physician self-reports to measure empathy, but it is not clear how closely such instruments correlate with patients’ perceptions. The Consultation and Relational Empathy (CARE) measure is the only one that assesses empathy from the patients’ perspective [16] and has proven reliability and validity. In this study, we wanted to explore how IBD patients perceive PE (perceived PE, pPE) and how relevant empathy is to them (desired PE, dPE), because PE can be a resource for patients and can even improve their compliance [17]. Consequently, we decided to use a modified, German-language version of the CARE measure [18, 19]. Because we were interested in evaluating whether PE is meeting the expectations of IBD patients, we reworded the items of the CARE measure to gather information about dPE. We assumed that congruence (i.e. alignment or a positive difference) between pPE and dPE would correlate with satisfaction and trust, whereas a negative difference would imply the opposite. Of course, the precondition is that PE is relevant to patients. If PE is low but unimportant to patients, one might find that they are nonetheless satisfied.
Thus, this study aimed to gather more detailed information about IBD patients’ psychosocial stress and resources and their trust in their physicians and satisfaction with their treatment, in order to better understand them and possibly improve the physician-patient partnership (PPP). In addition, we assessed what qualities other than empathy are important to patients, how satisfied they are with their current situation, what subjective burden they carry, and which resources are available to them.
Methods
A total of 121 participants were included. The sample consisted of two groups of patients: 1) IBD patients presenting as outpatients at our IBD clinic (Hospital of the University of Munich at LMU) were consecutively enrolled in the study from September 2013 to February 2014, n = 32 (26.4%); 2) IBD patients were recruited nationwide from November 2013 to February 2014 through patient support groups identified via the German IBD Network (http://www.kompetenznetz-ced.de), n = 89 (73.5%). A diagnosis of IBD was confirmed in 113 participants (20.4% ulcerative colitis, 76.1% Crohn’s disease); although 3.5% of participants did not yet have a final clear diagnosis, they were included in the analyses because IBD was highly suspected. Thirty patients were male (24.8%) and 91 female (75.2%). Their age ranged from 17 to 80 years (M [SD] = 36.32 [12.74]); 88.4% of participants were German, 56.2% were in a stable relationship, and 62% had no children (Table 1).
Table 1. Demographics of the survey population.
| n | % | ||
|---|---|---|---|
| gender | female | 91 | 75% |
| male | 30 | 25% | |
| age | 17–20 | 8 | 7% |
| 21–30 | 40 | 33% | |
| 31–40 | 29 | 24% | |
| 41–50 | 23 | 19% | |
| 51–60 | 14 | 12% | |
| >60 years | 5 | 4% | |
| no information | 2 | 1% | |
| nationality | German | 107 | 88% |
| Other | 14 | 12% | |
| marital status | Stable partnership | 68 | 56% |
| Single | 53 | 44% | |
| children | yes | 45 | 62% |
| no | 75 | 37% | |
| no information | 1 | 1% |
At the end of their consultation, outpatients at the IBD clinic completed a paper-and-pencil version of the CARE measure anonymously and in a separate room. They also filled out a questionnaire about their demographic information, disease history, previous medical experience, and the characteristics of the consultation they had just received. Specifically, the questionnaire assessed the patients’ overall satisfaction with the visit, the physician’s communication skills, and the degree of empathy shown by their physician. Moreover, patients were asked about the attributes, behaviors, and skills they wish to find in their health care providers, their level of subjective burden and resources, and their previous experiences with other physicians (S1 Questionnaire used for the survery translated into English).
The patients recruited at other locations in Germany completed an online version of the same instruments. Administrators of self-help groups were identified via the German IBD Network and asked to send a link to the instruments to patients on their address lists. Participation was voluntary. Patients were invited to leave their email address if they wished to receive the results of the study. All participants were blinded to any specific study hypothesis, and none of the variables was mentioned in the survey cover letter. They were asked to rate their last consultation with their treating physician.
The CARE measure was first described by Mercer in 2004 [4], then modified and translated into German by Neumann [18, 19]; this study used the latter version. The German CARE measure includes five cognitive and five affective items, which are rated on a Likert scale ranging from 1 to 5 (1 = poor; 5 = excellent). To gather information for our research question, we modified the German version of CARE by introducing two self-developed items that cover particular aspects of IBD and used two different versions of each item to determine pPE and dPE. The two additional items for IBD were: “Is your physician able to let you comfortably speak about embarrassing symptoms of your disease?” and “Does your physician examine you with care and respect?” These two elements were developed on the basis of a literature review, previous qualitative data obtained by the researchers, and advice from a panel of stakeholders.
Additionally, the questionnaire included two open questions that asked patients to describe a relevant negative experience and mention important attributes of a good doctor. Also, it included two items about satisfaction with the physician and three about trust in their physician. These items were also specifically created by the authors of this survey and had not previously been validated; we found a Cronbach’s alpha of .78 for “satisfaction” and .76 for “trust.”
We added an additional seven self-developed items to define a subscale for the subjective burden of IBD. Participants rated every item on a scale of 1 to 4 (1 = “not stressful at all,” 4 = “very stressful”).
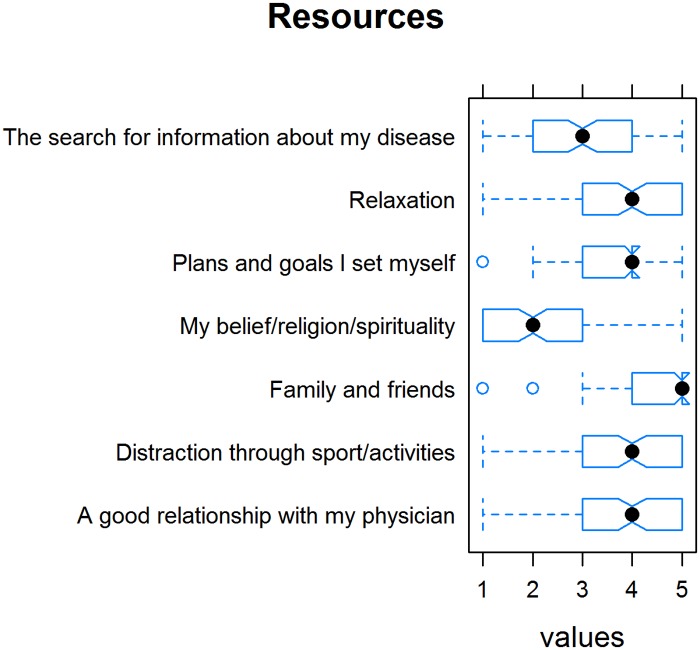
In a further, free-text part of the questionnaire, patients were asked to name stressors associated with the disease and resources that helped them cope with it (family and friends, a good relationship with their physician, plans and goals, distraction through sports/activities, relaxation, religion/spirituality, looking for and obtaining information about the disease).
The study was approved by the IRB of the medical faculty of the LMU Munich (Nr. 343–13). Patients gave written informed consent to participate in the study. All authors had access to the study data and reviewed and approved the final manuscript.
Statistics
Groups and scales were described by means (M) and standard deviations (SD) and by absolute and relative frequencies. Group results were compared with Welch’s or the Mann-Whitney U test for independent samples where appropriate. Normal distribution was tested with the Kolmogorov-Smirnov or Shapiro-Wilk test. Spearman’s rank correlation (rho) was used for correlations. According to Cohen’s classification, r > .10 is a small, r >.30 a medium, and r > .50 a large effect size (S1 Raw Data).
Results
Difference (ΔPE) between perceived physician empathy (pPE) and desired physician empathy (dPE)
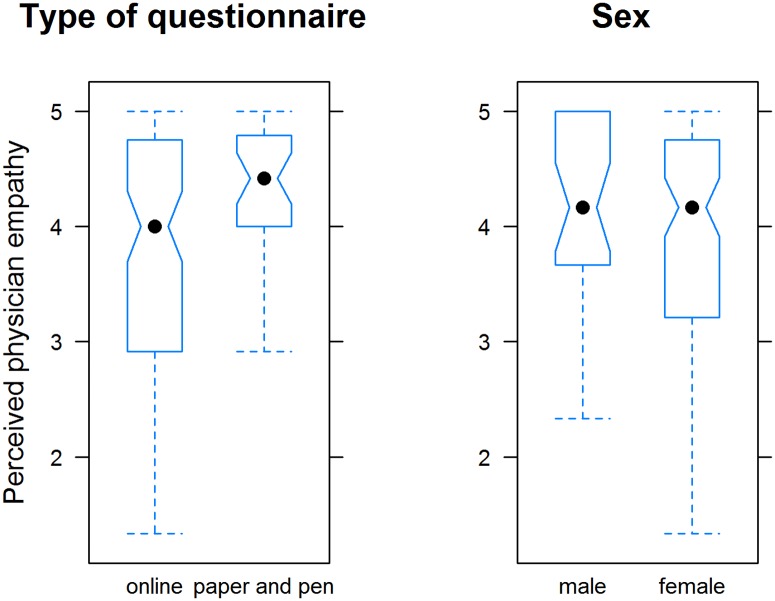
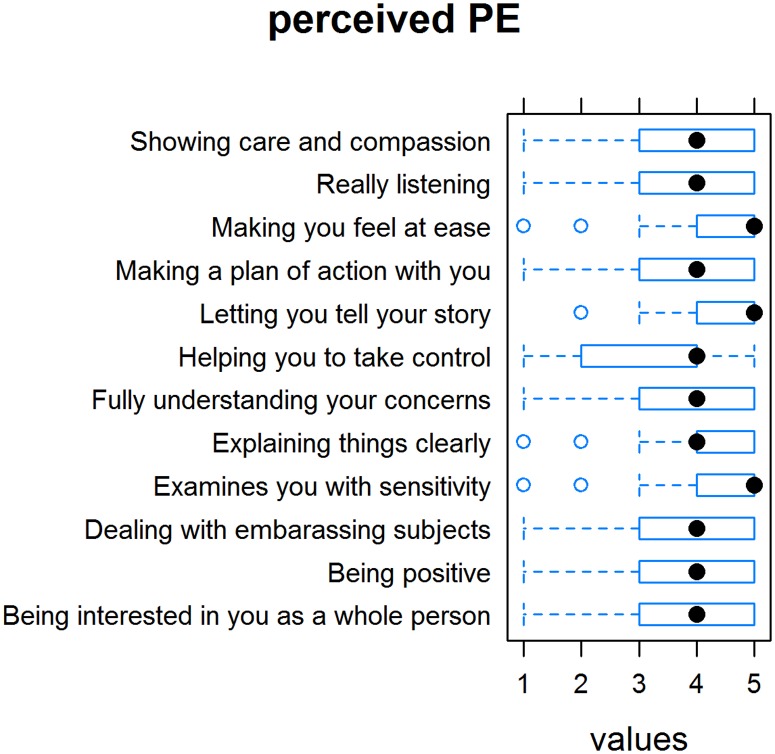
The mean (SD) pPE score was 3.93 (0.96) (Fig 1). Patients who completed the paper-and-pencil questionnaire rated pPE higher (4.33) than patients who took the online survey (3.80; p<0.001). Men generally rated pPE slightly higher than women (4.15 versus 3.86); however, the difference was not significant. In our modified version of the CARE measure, the scores were highest for the items “Does your physician behave in a way that you feel comfortable with?” and “Does your physician examine you with care and respect?” and lowest for the items “Does your physician help you in finding a way to deal with your disease?” and “Does your physician show interest for you as a person and for your background?” (Fig 2).
Fig 1. Perceived physician empathy as assessed by the Consultation and Relational Empathy (CARE) measure; Tukey’s box plots.
Left: The questionnaire was administered as either an online or a paper-and-pen version; the difference was statistically significant (p <0.001; Mann-Whitney U test). Right: Sex of patients; no difference.
Fig 2. Ratings of “perceived empathy” items on the Consultation and Relational Empathy (CARE) measure.
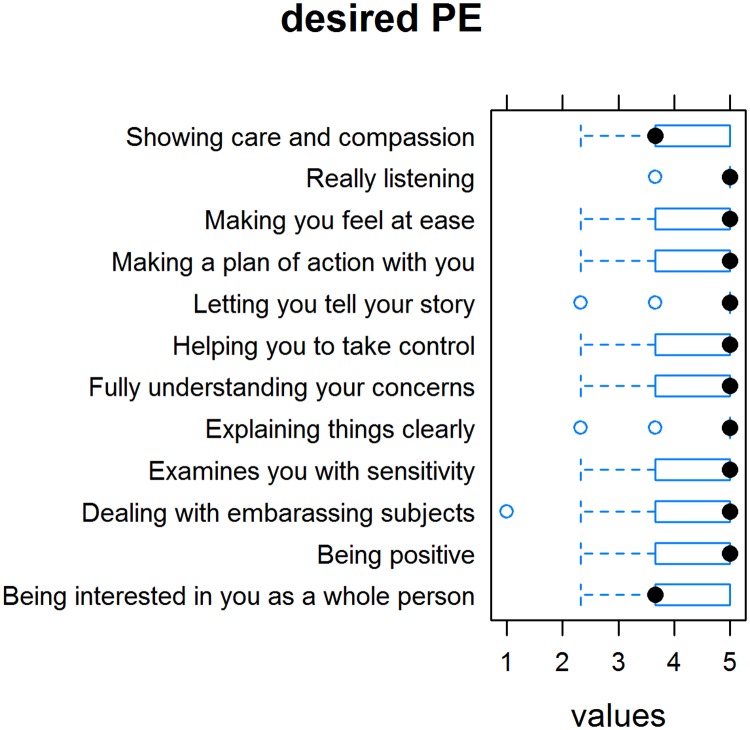
The mean (SD) score for dPE was 4.38 (0.48) (Fig 3). We found no differences between the paper-and-pencil and online groups or between men and women. Among the dPE indicators, patients gave the highest rating to the item “The physician really listens to me.” It was significantly more important for women than for men that a physician made them feel comfortable when dealing with embarrassing subjects/examinations.
Fig 3. Rating of “desired empathy” items on the Consultation and Relational Empathy (CARE) measure.
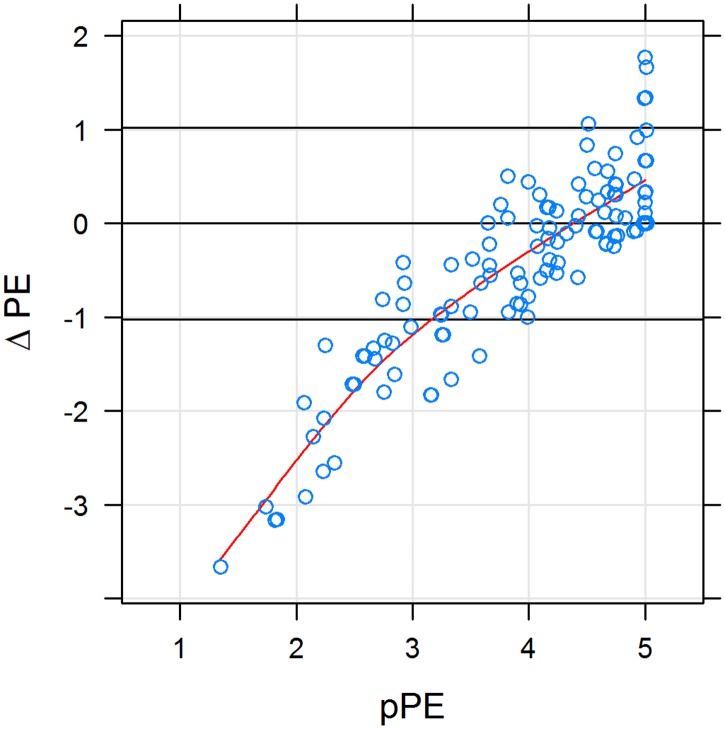
In 28 participants, ΔPE (= pPE-dPE) was 1 SD below zero, meaning that these patients wished to be treated more empathically by their physician than they currently perceived (dPE > pPE; ΔPE < 0; negative difference) (Fig 4). As Fig 1 shows, the higher the pPE score, the smaller the difference between dPE and pPE (ΔPE ≥ 0). In 5 cases, ΔPE was 1 SD above zero, meaning that these patients perceived PE to be higher than they had desired. It goes without saying that patients evaluated such situations positively.
Fig 4. Difference between desired and perceived physician empathy (ΔPE) as a function of perceived physician empathy (pPE).
X-Y scatterplot; horizontal lines denote equality between desired and perceived physician empathy plus or minus 1 standard deviation. Red curve is a cubic spline fit. Perceived physician empathy and ΔPE were strongly correlated (Spearman’s rho = 0.83; p < 10−15). Desired and perceived physician empathy were balanced if perceived physician empathy was > 4. In 28 subjects, ΔPE was 1 SD below zero, and in 5 cases it was 1 SD above.
A total of 51 patients (66.2%) reported negative experiences with other physicians in the past. Only 11 (14.3%) reported having only positive experiences. Twelve patients had never seen other health care providers before (15.6%). Twenty patients reported that they had not found previous health care providers to be competent enough, and 14 reported that previous providers had not taken enough time for them. Seven patients felt that they had not been well enough informed about their disease, and four had the impression that the doctor did not listen when they spoke. Table 2 summarizes these answers.
Table 2. Free-text responses to questions about patients’ perceptions of previous negative experiences with physicians (translated into English by the authors).
| Category | Example responses | n |
|---|---|---|
| Poor medication/ treatment |
|
20 |
| Lack of time |
|
14 |
| Lack of interest; not taken seriously |
|
11 |
| Too little information |
|
7 |
| Not very empathic |
|
6 |
| Does not listen |
|
4 |
| Change of physician |
|
3 |
| Waiting times |
|
2 |
| Comprehensibility |
|
1 |
| Miscellaneous |
|
1 |
Further attributes and behaviors of a good care provider
Patients were asked to state in free text what is particularly important to them besides empathy (see Table 3 for example responses and the number of responses).
Table 3. Patients’ free-text responses to questions about the desired qualities of health care providers (translated into English by the authors).
| Category | Example responses | n |
|---|---|---|
| Accessibility |
|
9 |
| Cooperation/ responsibility of physicians |
|
9 |
| Individual care/ treatment concept |
|
8 |
| Shorter wait times, more time for patients |
|
7 |
| Taking patients seriously |
|
3 |
| Considers other illnesses |
|
2 |
| Work atmosphere |
|
2 |
| New/alternative treatment methods |
|
2 |
| Acceptance |
|
2 |
| No wishes |
|
2 |
| Miscellaneous |
|
9 |
The most common response was wanting their physicians to be more accessible via telephone or email (n = 9) and to cooperate better e.g. with their family practitioner (n = 9). Also, they wanted more time with their provider (n = 7), to have the feeling that they were being taken seriously (n = 3), to receive information from their health care providers about other therapeutic options (n = 2), and for their providers to be open to trying alternative treatments (n = 2).
Trust in health care providers and satisfaction with treatment
The congruence between pPE and dPE correlated positively with trust and satisfaction (Spearman’s rho = .47 and .32, respectively). Trust and satisfaction were quantified with two and three additional items, respectively.
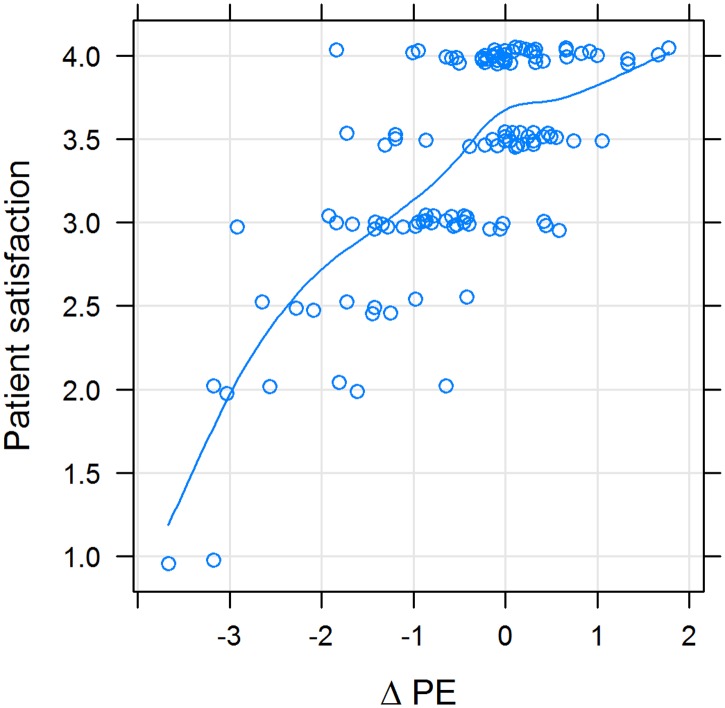
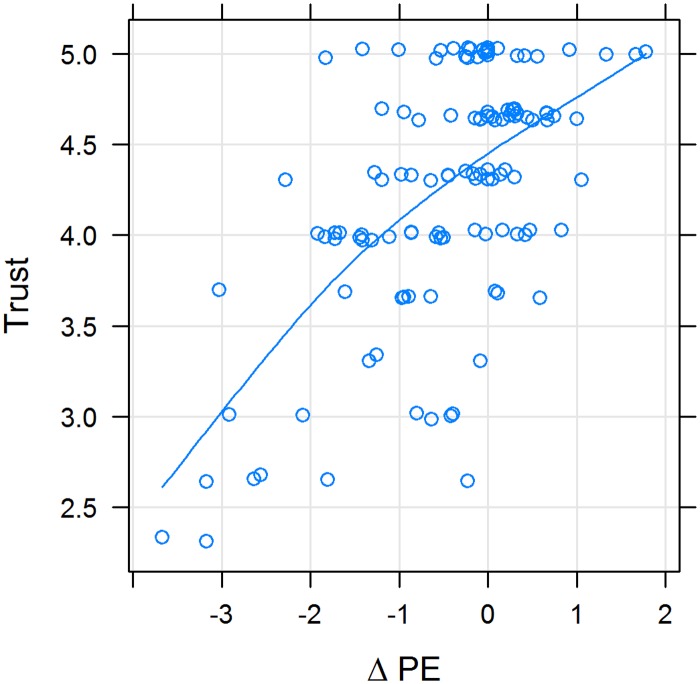
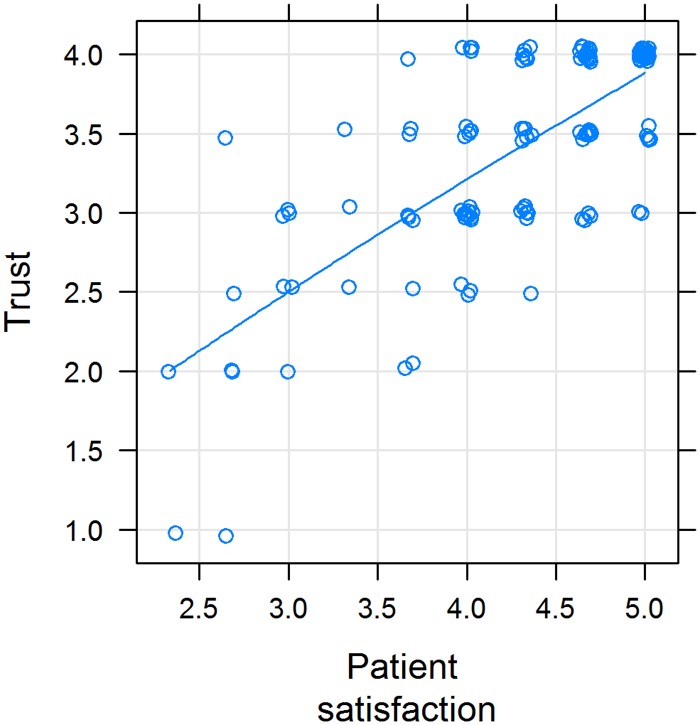
Figs 5 and 6 show that the smaller the difference between pPE and dPE, the higher the rating of satisfaction and trust. Values of ΔPE above zero have less influence on satisfaction and trust, i.e. the slope of the line is less steep (Figs 5 and 6). Also, satisfaction and trust correlate with another (Fig 7).
Fig 5. Patient satisfaction with the physician as a function of the difference between desired and perceived physician empathy (ΔPE); X-Y scatterplot.
Variables were positively correlated (rho = 0.47; p < 10−10). The line represents a cubic smoothing spline fit. If ΔPE was negative, patient satisfaction was low and rose steeply; and if it was positive, patient satisfaction rose less steeply.
Fig 6. Association between trust in the physician (Trust) and the difference between desired and perceived physician empathy (ΔPE); X-Y scatterplot.
Variables were positively correlated (rho = 0.32; p < 10−7). The line represents a cubic smoothing spline fit.
Fig 7. Association between trust in the physician (Trust) and patient satisfaction; X-Y scatterplot.
Variables were positively correlated (rho = 0.66; P value < 2.2e-16). The line represents a cubic smoothing spline fit.
Subjective burden and resources of IBD patients
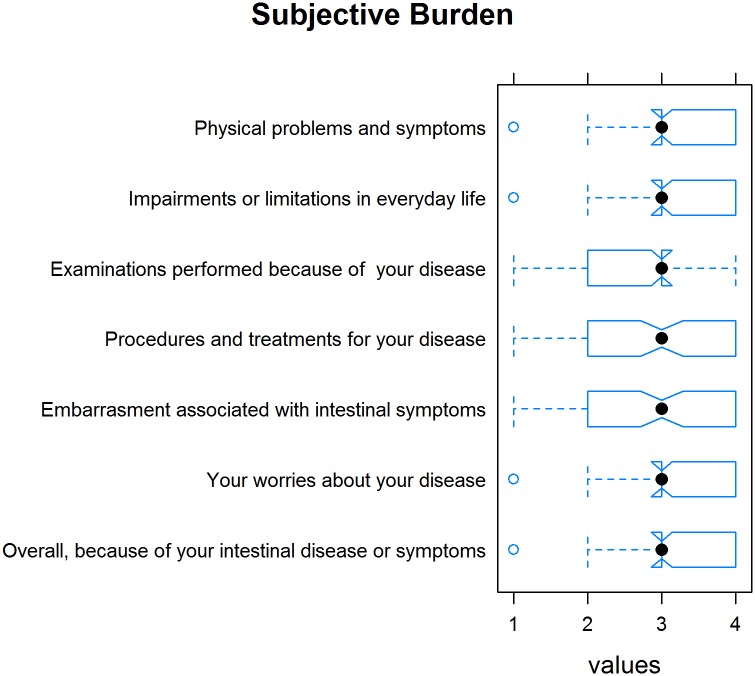
The mean (SD) sum of all subjective burden-related items (on a scale of 1 = “not stressed” to 4 = “very stressed”) was 2.93 (.63), indicating that IBD is perceived as quite stressful by patients. Fig 8 depicts the burden-related items and their ratings (Fig 8).
Fig 8. Tukey’s box plots with a notch depicting the subjective burden of various aspects of the disease and their ratings.
Concerning their resources, 62.8% of patients see “family and friends” as a resource; 36.4%, “a good patient-physician partnership”; and 52.9%, “belief/religion/spirituality.” Ten patients mentioned other patient self-help groups and social media groups as a good resource, seven their hobbies and their pets. Fig 9 summarizes the mean ratings for individual resources. Participants were asked to mention in a free-text item the resources that are particularly important to them. Table 4 summarizes their answers.
Fig 9. Tukey’s box plots with a notch depicting patient resources and their ratings.
Table 4. Patients’ free-text responses to questions about their resources for coping with the disease (translated into English by the authors).
| Category | Example responses | n |
|---|---|---|
| Exchange with other people affected |
|
9 |
| Hobbies |
|
9 |
| Acceptance |
|
8 |
| Distraction |
|
7 |
| Integration of the disease in everyday life |
|
3 |
| Professional support |
|
2 |
| Positive attitude |
|
2 |
| Information search |
|
2 |
| Miscellaneous |
|
2 |
Discussion
To our knowledge, the present study is the first to focus on the role of perceived and desired physician empathy (pPE and dPE, respectively) from the perspective of patients with IBD and on the correlations of PE with trust and satisfaction in this group. We performed a literature research before designing our study and found no similar studies in this field. The aim of our study was to identify both potential ways to optimize the physician-patient partnership (PPP) and a possible incongruence between the current and desired PE in the eye of IBD patients. We chose to concentrate on PE as an important aspect of physician-patient communication and used a modified version of the CARE measure that allowed us to focus more on the patients’ perspective rather than that of physicians.
When asked about the desirable qualities of a good physician, both physicians and patients mentioned empathy [4]. The patients in our study found that their current health care providers are empathic (3.9 of 5); however, they wish that their physicians showed more empathy (4.4 on a scale of 1 to 5). To make sure that this finding is not due to a methodological bias, we asked participants whether they had had any different experiences in the past. Most reported that they had been treated by several different physicians and that they were not satisfied with those experiences. Therefore, we conclude that the high level of PE reported in this survey cannot be extended to all physicians. The results of the ECCO-Epicom study indicate a difference between Eastern and Western Europe [13], but the current study was performed solely in Germany. Moreover the online survey found lower PE values than the paper-and-pencil survey. This might be due to the different time frame in which patients completed the survey (the paper-and-pencil group completed it directly after a consultation; the online group, at some unspecific time) and to the fact that online surveys might appear more “anonymous” than a survey performed at a physician’s office directly after a consultation. However, it is also possible that the physicians involved in this study acted particularly empathically, perhaps because they were aware of the survey. The German version of the CARE measure was validated partly by asking several patients to rate the same physician, whereas in our paper-and-pencil survey patients were asked to rate only the one experience they had just had (instead of rating their health care providers more generally). Several of the on-site patients (n = 32) probably rated the same physician, because only three physicians were involved in this study. It is not possible to identify the physicians who were assessed by the online participants. This difference between the groups might be a limitation of the study.
PE is very relevant to patients. We found a significant positive correlation between the participants’ level of subjective burden and their rating of the relevance of PE, which underlines the role of PE as a resource for patients. Women in particular attached great importance to not feeling embarrassed when they have to talk about classical IBD symptoms such as diarrhea, nausea, abdominal pain, and gas bloating. In this study the physicians being judged in the paper-and-pencil arm were male. The patients in the internet group were not asked to mention the gender of their health care providers. There are commonly no IBD-Nurses in Germany, who might take over these special subjects. Consequently, physicians might learn from this study that it is particularly important to try to reduce female patients’ feelings of embarrassment when they talk about such symptoms. Physicians can encourage patients to speak openly about these subjects by asking appropriate questions, for example. Adequate communication training in medical education could be very helpful.
Competence, information about alternative treatments, and patient-centered treatment were also mentioned as being very important to patients. These findings are similar to those of a recent study on prostate cancer patients undergoing radiation [20]. Additionally, participants mentioned the importance of organizational details such as being able to reach the doctor easily, good communication between their IBD specialist and family practitioner, and waiting times that are not too long. Some of these points were given as an explanation why they had chosen previously to change their treating physician.
We expected to find that patients would be unhappy with their treatment if pPE and dPE were incongruent. Two thirds of patients showed such an incongruence; however, the incongruence seems only to be relevant when dPE is higher than pPE (i.e. when ΔPE is negative). This was the case in 27.3% of patients. In all other cases, pPE was the same or even higher than the dPE. The congruence between pPE and dPE correlated positively with trust and satisfaction. Trust and satisfaction also correlated positively with each other. These findings are similar to those of a recent Norwegian study on quality of care in IBD patients, which found a high satisfaction rate (86%) [21]. Dissatisfaction was mostly related to communication aspects, showing the need for improvement of physician-patient communication.
In our study, patients identified IBD as a source of subjective burden: the mean subjective burden was 2.9 on a scale of 1 to 4. IBD patients often have depression [22]. Interestingly, a recent study reported that depression has a similar pathophysiology to that of IBD, i.e. they are both clinical expressions of activated immune-inflammatory, oxidative, and nitric oxid stress pathways, which may explain the frequent co-occurrence of these two conditions [23]. Another recent study found a strong relationship between perceived stress and gastrointestinal symptoms [24]. This association might explain our finding that the level of subjective burden correlated negatively with patient satisfaction and positively with the importance of PE for patients. “A good patient-physician partnership” (PPP) was a resource in just over a third of the IBD patients in the present study. Therefore, strategies aimed at improving the PPP might help patients to better bear the burden of disease and might increase their satisfaction with their treatment and PPP. PE seems to be able to influence pain, fear [25], how well patients cope with their disease [26], and cancer patients’ levels of depression and satisfaction with life [18]. For this reason, we focused on gathering information about how patients perceive their current PPP, particularly the empathy of their health care providers.
To the best of our knowledge, this study is to the first to evaluate ΔPE in IBD patients. A strength of the study is the use of a patient-centered measure, the CARE. The study does have various limitations, though. First, the generalization of our findings to other hospitals is limited, because we included patients at only one hospital. The additional use of an online survey improves the generalizability. However, the internet may allow patients to give a more liberal evaluation, because they do not have to worry that their physician will learn about their opinions. Therefore, the comparison of paper-and-pencil survey and online results might be biased. The recent study by the ECCO-Epicom group found a significant difference between Eastern and Western Europe, so our result can probably be seen to be relevant only in Germany [13]. Furthermore, generalization within Germany also is limited because of the fairly small sample size. In addition, the study did not take into account confounders of the relationship between physicians and patients such as type of health insurance, income level, common culture of physician and patient, and the patient’s social environment. For example, physicians have been found to spend more time with patients who have private health insurance, which may influence patients’ perception of PE [27]. The CARE is a validated method to measure physician empathy. However, the German version used in this study has been validated only in cancer patients. Furthermore, we added two items to evaluate the particular needs of IBD patients; although these items were not validated, they had a Cronbach’s alpha of .96. Also, the items used to measure satisfaction and trust were formulated for the test and were not previously validated; the Cronbach’s alpha was .76 and .78 for these items, respectively. A further potential bias is that the on-site physicians were aware that the survey was being performed and consequently might have behaved more empathically than usual.
Conclusion
We identified a wide range of personal attributes, behaviors, and skills of IBD specialist physicians that can make a real difference to patient care. The difference between desired and perceived PE might predict satisfaction with and trust in the treating physician. This aspect needs to be considered in medical education and daily clinical practice.
Supporting Information
(DOCX)
(DOCX)
Acknowledgments
The authors wish to express their gratitude to Prof. Max Schnurr, who was one of the IBD health care providers who participated in this study, together with PD Dr. Veit Gülberg and Prof. Matthias Siebeck.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Nyuyki KD, Pittman QJ, Toward a better understanding of the central consequences of intestinal inflammation. Ann N Y Acad Sci. 2015. September;1351:149–54. 10.1111/nyas.12935 [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto T, Yanai S, Toya Y, Internet-orientated Assessment of QOL and Actual Treatment Status in Japanese Patients with Inflammatory Bowel Disease: The 3I survey. J Crohns Colitis. 2015. June;9(6):477–82. 10.1093/ecco-jcc/jjv052. Epub 2015 Mar 26. [DOI] [PubMed] [Google Scholar]
- 3.Mocciaro F, Di Mitri R, Russo G, Leone S, Quercia V, Motivational interviewing in inflammatory bowel disease patients: a useful tool for outpatient counselling. Dig Liver Dis. 2014. October;46(10):893–7. 10.1016/j.dld.2014.07.009. Epub 2014 Jul 30. [DOI] [PubMed] [Google Scholar]
- 4.Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52:S9–12. [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds WJ, Scott B. Do nurses and other professional helpers normally display much empathy? J Adv Nurs. 2000. January;31(1):226–34. [DOI] [PubMed] [Google Scholar]
- 6.Mercer SW, Neumann M, Wirtz M, Fitzpatrick B, Voit G, General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ Couns. 2008. November;73(2):240–5. 10.1016/j.pec.2008.07.022 [DOI] [PubMed] [Google Scholar]
- 7.Neumann M, Bensing J, Wirtz M, The impact of financial incentives on physician empathy: a study from the perspective of patients with private and statutory health insurance. Patient Educ Couns. 2011. August;84(2):208–16. 10.1016/j.pec.2010.07.012. Epub 2010 Aug 14. [DOI] [PubMed] [Google Scholar]
- 8.Nicolai J, Buchholz A, Seefried N, When do cancer patients regret their treatment decision? A path analysis of the influence of clinicians' communication styles and the match of decision-making styles on decision regret. Patient Educ Couns. 2015. December 2 pii: S0738-3991(15)30136-1. 10.1016/j.pec.2015.11.019. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Del Canale S, Louis DZ, Maio V, The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012. September;87(9):1243–9. [DOI] [PubMed] [Google Scholar]
- 10.Menendez ME, Chen NC, Mudgal CS, Jupiter JB, Ring D, Physician Empathy as a Driver of Hand Surgery Patient Satisfaction. J Hand Surg Am. 2015. September;40(9):1860–5.e2. 10.1016/j.jhsa.2015.06.105. Epub 2015 Jul 29. [DOI] [PubMed] [Google Scholar]
- 11.Steinhausen S, Ommen O, Antoine SL, Koehler T, Pfaff H, Neugebauer E, Short- and long-term subjective medical treatment outcome of trauma surgery patients: the importance of physician empathy. Patient Prefer Adherence. 2014. September 18;8:1239–53. 10.2147/PPA.S62925. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maunder RG, de Rooy EC, Toner BB, Greenberg GR, Steinhart AH, McLeod RS et al. Health-related concerns of people who receive psychological support for inflammatory bowel disease. Can J Gastroenterol. 1997. Nov-Dec;11(8):681–5. [DOI] [PubMed] [Google Scholar]
- 13.Burisch J, Vegh Z, Pedersen N, Health care and patients' education in a European inflammatory bowel disease inception cohort: an ECCO-EpiCom study, J Crohns Colitis. 2014. August;8(8):811–8. 10.1016/j.crohns.2013.12.023. Epub 2014 Jan 16. [DOI] [PubMed] [Google Scholar]
- 14.Belling R, Woods L, McLaren S, Stakeholder perceptions of specialist Inflammatory Bowel Disease nurses' role and personal attributes. Int J Nurs Pract. 2008. February;14(1):67–73. 10.1111/j.1440-172X.2007.00661.x [DOI] [PubMed] [Google Scholar]
- 15.Ikas G, [Information programs for patients during gastroenterological rehabilitation]. Z Gastroenterol. 2002. April;40 Suppl 1:S100–S2. [DOI] [PubMed] [Google Scholar]
- 16.Mercer SW, Maxwell M, Heaney D, Watt GC, The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004. December;21(6):699–705. Epub 2004 Nov 4. 10.1093/fampra/cmh621 [DOI] [PubMed] [Google Scholar]
- 17.Kim SS, Kaplowitz S, Johnston MV, The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004. September;27(3):237–51. 10.1177/0163278704267037 [DOI] [PubMed] [Google Scholar]
- 18.Neumann M, Wirtz M, Bollschweiler E, Mercer SW, Warm M Wolf J et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. 2007. December;69(1–3):63–75. Epub 2007 Sep 11. 10.1016/j.pec.2007.07.003 [DOI] [PubMed] [Google Scholar]
- 19.Neumann M., Wirtz M., Bollschweiler E, Warm M, Wolf J, Pfaff H, Psychometric Evaluation of the German Version of the 1Consultation and Relational Empathy”(CARE). Measure at the Example of Cancer Patients. Psychotherapie, Psychosomatik, Medizinische Psychologie 2008, 58(1), 5–15. 10.1055/s-2007-970791 [DOI] [PubMed] [Google Scholar]
- 20.Foley KA, Feldman-Stewart D, Groome PA, Brundage MD, McArdle S, Wallace D et al. What Aspects of Personal Care Are Most Important to Patients Undergoing Radiation Therapy for Prostate Cancer? Int J Radiat Oncol Biol Phys. 2016. February 1;94(2):280–8. 10.1016/j.ijrobp.2015.10.023. Epub 2015 Oct 19. [DOI] [PubMed] [Google Scholar]
- 21.Jelsness-Jørgensen LP, Bernklev T, Hovde Ø, Patients' perceptions of quality of care and follow-up in inflammatory bowel disease. Scand J Gastroenterol. 2016. April;51(4):434–41. 10.3109/00365521.2015.1102319. Epub 2015 Dec 4. [DOI] [PubMed] [Google Scholar]
- 22.Yanartas O, Kani HT, Bicakci E, Kilic I, Banzragch M, Acikel C et al. The effects of psychiatric treatment on depression, anxiety, quality of life, and sexual dysfunction in patients with inflammatory bowel disease. Neuropsychiatr Dis Treat. 2016. March 24;12:673–83. 10.2147/NDT.S106039. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin-Subero M, Anderson G, Kanchanatawan B, Berk M, Maes M, Comorbidity between depression and inflammatory bowel disease explained by immune-inflammatory, oxidative, and nitrosative stress; tryptophan catabolite; and gut-brain pathways. CNS Spectr. 2015. August 26:1–15. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Targownik LE, Sexton KA, Bernstein MT, Beatie B, Sargent M, Walker JR, The Relationship Among Perceived Stress, Symptoms, and Inflammation in Persons With Inflammatory Bowel Disease. Am J Gastroenterol. 2015. July;110(7):1001–12; quiz 1013. 10.1038/ajg.2015.147. Epub 2015 Jun 16. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds WJ, Scott B, Do nurses and other professional helpers normally display much empathy? J Adv Nurs. 2000. January;31(1):226–34. [DOI] [PubMed] [Google Scholar]
- 26.Mercer SW, Neumann M, Wirtz M, Fitzpatrick B, Voit G. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ Couns. 2008. November;73(2):240–5. 10.1016/j.pec.2008.07.022 [DOI] [PubMed] [Google Scholar]
- 27.Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents, Acad Med. 2011. August;86(8):996–1009. 10.1097/ACM.0b013e318221e615 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.