Abstract
Objective: This study estimated prevalence rates of loneliness, identified characteristics associated with loneliness, and estimated the impact of loneliness on quality of life (QOL) and patient satisfaction. Method: Surveys were mailed to 15,500 adults eligible for care management programs. Loneliness was measured using the University of California Los Angeles (UCLA) three-item scale, and QOL using Veteran’s RAND 12-item (VR-12) survey. Patient satisfaction was measured on a 10-point scale. Propensity weighted multivariate regression models were utilized to determine characteristics associated with loneliness as well as the impact of loneliness on QOL and patient satisfaction. Results: Among survey respondents (N = 3,765), 28% reported severe and 27% moderate loneliness. The strongest predictor of loneliness was depression. Physical and mental health components of QOL were significantly reduced by loneliness. Severe loneliness was associated with reduced patient satisfaction. Discussion: Almost 55% of these adults experienced loneliness, negatively affecting their QOL and satisfaction with medical services. Screening for loneliness may be warranted.
Keywords: loneliness, quality of life, patient satisfaction, Medicare Supplement
Introduction
Loneliness is generally defined as a discrepancy between an individual’s desired and actual social relationships, whether in their quality or quantity (Aartsen & Jylha, 2011; Dahlberg & McKee, 2014; Luo, Hawkley, Waite, & Cacioppo, 2012; van Beljouw et al., 2014). While not an experience unique to old age, loneliness is common among older adults, with 12% to 46% reporting at least some level of loneliness (Aartsen & Jylha, 2011; Dahlberg & McKee, 2014; Ellwardt, Aartsen, Deeg, & Steverink, 2013; Golden et al., 2009; Hawkley, Thisted, Masi, & Cacioppo, 2010; Holwerda et al., 2014; Lim & Kua, 2011; Netz, Goldsmith, Shimony, Arnon, & Zeev, 2013; Perissinotto, Cenzer, & Covinsky, 2012; Steptoe, Shankar, Demakakos, & Wardle, 2013; Victor & Bowling, 2012; van Beljouw et al., 2014). Loneliness among older adults is a concern of many countries around the world and has been documented in research studies in the United States (Hawkley et al., 2010; Perissinotto et al., 2012), the United Kingdom (Dahlberg & McKee, 2014; Steptoe et al., 2013), Ireland (McHugh & Lawlor, 2013; Schnittger, Wherton, Prendergast, & Lawlor, 2012), France (Amieva et al., 2010), Norway (Aanes, Hetland, Pallesen, & Mittelmark, 2011), the Netherlands (Ellwardt et al., 2013; van Beljouw et al., 2014), Finland (Aartsen & Jylha, 2011), Sweden (Taube, Kristensson, Sandberg, Midlov, & Jakobsson, 2014), Singapore (Lim & Kua, 2011), and Israel (Netz et al., 2013). Although estimates of loneliness vary due to differences in older populations studied as well as measures and definitions of loneliness used, prevalence rates for loneliness are remarkably consistent and stable over time across the scientific literature (Cacioppo, Hughes, Waite, Hawkley, & Thistel, 2006; Hawkley et al., 2010; Victor & Bowling, 2012). Longitudinal studies indicate that recovery from loneliness is possible and generally associated with improved health and/or social relationships (Aartsen & Jylha, 2011; Victor & Bowling, 2012).
Characteristics associated with loneliness generally include older age, widowhood/single status, lower income, poor health, functional limitations, hearing or vision impairments, depression, cognitive impairment, and loss of social networks/support (Aartsen & Jylha, 2011; Cacioppo et al., 2006; Cohen-Mansfield & Parpura-Gill, 2007; Dahlberg & McKee, 2014; Golden et al., 2009; Hawkley et al., 2010; Lim & Kua, 2011; Netz et al., 2013; Perissinotto et al., 2012; Pronk et al., 2011; Schnittger et al., 2012; Steptoe et al., 2013; Taube et al., 2014; van Beljouw et al., 2014; Victor & Bowling, 2012). Clinical outcomes associated with loneliness include depression, reduced sleep quality, increased blood pressure, physical inactivity, functional decline, cognitive impairment, and increased mortality (Aanes et al., 2011; Amieva et al., 2010; Buchman et al., 2010; Cacioppo et al., 2006; Cohen-Mansfield & Parpura-Gill, 2007; Dahlberg & McKee, 2014; Ellwardt et al., 2013; Hawkley et al., 2010; Holwerda et al., 2014; Lim & Kua, 2011; Luo et al., 2012; McHugh & Lawlor, 2013; Netz et al., 2013; Perissinotto et al., 2012; Steptoe et al., 2013; Taube et al., 2014; van Beljouw et al., 2014; Victor & Bowling, 2012). Directionality and causality for the associations of various health indicators with loneliness are not always consistent in the literature. However, an increased number of longitudinal studies indicate that loneliness precedes depression (Cacioppo et al., 2006; Lim & Kua, 2011), sleep difficulties (McHugh & Lawlor, 2013), high blood pressure (Hawkley et al., 2010), physical inactivity (Hawkley, Thisted, & Cacioppo, 2009), functional decline (Buchman et al., 2010), cognitive impairment (Amieva et al., 2010; Ellwardt et al., 2013; Holwerda et al., 2014), and increased mortality (Luo et al., 2012; Perissinotto et al., 2012; Steptoe et al., 2013).
Relatively few studies have focused on the impact of loneliness on the quality of life (QOL). In these studies, measures and definitions of QOL were not consistent; however, results generally indicated that loneliness decreased QOL (Dahlberg & McKee, 2014; Golden et al., 2009; Lim & Kua, 2011; Taube et al., 2014; van Beljouw et al., 2014). In addition, the impact of loneliness on patient satisfaction with medical services (e.g., physician or insurance plans) has not been examined, although several studies have shown that anxiety decreases patient satisfaction specifically with mental health services (Hundt et al., 2013; Stein et al., 2011).
Most of the literature examining loneliness has focused on general populations of older adults in the United States and other countries. We found no studies investigating the prevalence of loneliness and its consequences among older adults with Medicare Supplement plans (i.e., Medigap). While most (about 90%) of those with fee-for-service Medicare coverage (about 77% of all Medicare beneficiaries) have some type of supplemental insurance coverage, only about 28% (about 10.2 million adults) have purchased Medigap coverage (Kaiser Family Foundation, 2013). We hypothesize that patient demographics, health status, and benefit levels likely differ by Medigap source and plan type and, therefore, may affect prevalence of loneliness, characteristics, and outcomes associated with the condition.
Thus, the primary objective of our study was to document the prevalence of loneliness within a Medicare Supplement population eligible for care management programs in the United States and determine characteristics associated with moderate and severe loneliness. The secondary objective was to examine the impact of loneliness on both physical and mental dimensions of QOL and patient satisfaction with doctors, health care, and Medicare Supplement plans.
Method
Sample Selection
In 2013, approximately 3.5 million Medicare insureds were covered by an AARP® Medicare Supplement plan insured by UnitedHealthcare Insurance Company (for New York residents, UnitedHealthcare Insurance Company of New York). These plans are offered in all 50 states, Washington, D.C., and various U.S. territories. A randomly selected sample of 15,500 of these insureds in 4 states (North Carolina, New York, Ohio, and Texas) was surveyed. The sampling strategy included an eligibility criterion for care management programs (i.e., oversampling those with more intensive health needs).
Those surveyed were 65 years or older at the time of survey distribution. To be eligible, survey respondents were required to have a minimum of 3 months of Medicare Supplement plan eligibility. Those who did not answer all three survey questions on loneliness (1%) or complete at least 50% of the QOL questions (2%) were excluded. The final study sample included 3,765 survey respondents.
Survey
A modified version of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey, which is funded and overseen by the U.S. Agency for Healthcare Research and Quality (AHRQ), was used as the basis for our survey. The survey is designed to query patients and health care consumers to report on and evaluate their experiences and satisfaction with Medicare delivery systems, including physicians, health plans, and supplemental health plans. The survey is in the public domain and has become the national standard for measuring and reporting on patient experiences.
This self-reported survey measures the insured’s demographics, socioeconomic factors, health status, and perception of experiences and satisfaction with the different components of health care services. The CAHPS survey was adapted for distribution to our population with additional questions to screen for loneliness and characterize the impact of loneliness on health status and QOL.
Loneliness was measured using the validated UCLA three-item scale with responses never/hardly ever, some of the time, and often (Hughes, Waite, Hawkley, & Cacioppo, 2004). The questions were scored 1 to 3, then summed to a score ranging from 3 to 9. Loneliness was subsequently categorized as follows: no loneliness (score = 3), moderate loneliness (score = 4 or 5), and severe loneliness (score = 6-9).
The 12-item Veteran’s RAND (VR-12) health status/QOL scale, which has been validated for use in older populations, was used to examine the impact of loneliness on QOL (Selim et al., 2009). Physical (PCS) and mental (MCS) health component scores were calculated. For these scales, a score was calculated if at least 50% of the items in the scale were completed (commonly referred to as the “half-scale” rule). QOL scale scores ranged from 0 (worst possible QOL) to 100 (best possible QOL). To compare with the general U.S. population or other Medicare populations, the scores were transformed to “standardized scores” with a mean of 50 and a standard deviation of 10 (Kosinski, Bayliss, Bjorner, & Ware, 2000).
Patient satisfaction with doctors, health care, and AARP Medicare Supplement plans was measured on a 10-point scale using the following survey questions:
“What number would you use to rate your doctor?”
“What number would you use to rate your health care in the last 6 months?”
“What number would you use to rate your AARP Medicare Supplement Insurance Plan?”
The satisfaction scores were not normally distributed, with more respondents having higher scores. Consequently, scores were dichotomized at the 80th percentile (20/80) to represent high satisfaction versus lower satisfaction for use in subsequent logistic regression analyses.
Covariates
Covariates were included to characterize those with loneliness and to adjust for factors that may influence QOL or patient satisfaction. These covariates included survey measures of demographics, socioeconomic factors, health status, and other characteristics taken from health plan eligibility and claims files. Demographic questions included age, gender, and race. Urban and other locations and income levels (low, lower middle, upper middle, high) were geocoded from zip codes. Health status items from the survey included body mass index (BMI) as well as vision, hearing, and balance/walking problems. Calculated BMIs were divided into the following standard weight categories: underweight (BMI < 18.5), normal weight (BMI = 18.5-24.9), overweight (BMI = 25-29.9), obese (BMI = 30-39.9), and morbidly obese (BMI ≥ 40; National Heart, Lung, and Blood Institute Obesity Task Force, 1998). Medicare Supplement plan types were grouped by cost-sharing levels and included first-dollar coverage plans with no copayments or deductibles (Plans C, F, and J) and all other. Level of engagement in the care management program was identified as engaged, disengaged, eligible but never engaged or no access to the program. Health literacy was measured with the single validated question asking for confidence level in filling out medical forms (Wallace, Rogers, Roskos, Holiday, & Weiss, 2006). Access to care was measured as the number of primary care physicians per 1,000 in the individual’s hospital service area. Level of medical services utilization from medical claims was calculated as the hierarchical condition category (HCC) score (Pope et al., 2011). This score is used by Centers for Medicare & Medicaid Services (CMS) to risk adjust medical payments across various medical plans according to the health status of the different insured populations. The HCC score was categorized by quartiles (25th, 50th, and 75th percentiles) for use in subsequent regression models. The demographic, socioeconomic, and health status covariates considered are listed in Table 1.
Table 1.
Demographic Characteristics Among Those With No, Moderate, and Severe Loneliness (Unadjusted).
| All |
No loneliness |
Moderate loneliness |
Severe loneliness |
||
|---|---|---|---|---|---|
| N = 3,765 % | n = 1,716 % | n = 1,004 % | n = 1,045 % | p value | |
| CM engagement status | |||||
| Engaged | 33.6 | 30.8 | 34.7 | 37.2 | .007 |
| Disengaged | 2.2 | 1.8 | 2.3 | 2.7 | |
| Never engaged | 22.5 | 24.2 | 22.2 | 19.9 | |
| Program not available | 41.7 | 43.2 | 40.8 | 40.2 | |
| Gender | |||||
| Female | 56.1 | 51.1 | 57.4 | 63.2 | <.0001 |
| Male | 43.9 | 49.0 | 42.6 | 36.8 | |
| Age (M) | 80.8 | 80.1 | 81.5 | 81.3 | <.0001 |
| 65-69 | 8.9 | 9.7 | 7.9 | 8.6 | .001 |
| 70-74 | 14.4 | 15.9 | 12.7 | 13.8 | |
| 75-79 | 19.8 | 21.1 | 18.9 | 18.4 | |
| 80-84 | 26.6 | 26.8 | 27.8 | 25.2 | |
| 85 plus | 30.3 | 26.5 | 32.8 | 34.1 | |
| Race | |||||
| White | 90.9 | 91.1 | 91.6 | 90.1 | .56 |
| Income group | |||||
| High | 50.3 | 51.3 | 50.9 | 48.0 | .13 |
| Upper middle | 22.8 | 23.0 | 24.0 | 21.3 | |
| Lower middle | 16.6 | 16.2 | 14.8 | 19.0 | |
| Low | 8.0 | 7.3 | 8.0 | 9.4 | |
| Location | |||||
| Urban | 87.2 | 86.6 | 87.8 | 87.8 | .57 |
| Acute care hospitals per 1,000 (M) | 2.6 | 2.5 | 2.6 | 2.6 | .01 |
| PCPs per 100,000 (M) | 71.4 | 70.4 | 72.7 | 71.8 | .009 |
| Plan type | |||||
| First-dollar coverage (no copays) | 75.2 | 78.4 | 72.7 | 72.4 | <.0001 |
| Baseline health status | |||||
| Community HCC score (M) | 2.6 | 2.6 | 2.5 | 2.6 | .03 |
| HCC score ≤ 1.657 | 25.0 | 25.4 | 25.9 | 23.5 | .31 |
| HCC score ≤ 2.449 | 25.0 | 24.1 | 27.1 | 24.4 | |
| HCC score ≤ 3.253 | 25.0 | 25.2 | 24.2 | 25.5 | |
| HCC score > 3.253 | 25.0 | 25.3 | 22.8 | 26.6 | |
| Three-item loneliness score (M) | 4.5 | 3.0 | 4.4 | 6.9 | <.0001 |
| Quality of life (VR-12; unadjusted) | |||||
| PCS | 33.9 | 36.4 | 33.4 | 30.3 | <.0001 |
| MCS | 50.3 | 56.0 | 49.9 | 41.3 | <.0001 |
| Depression | |||||
| Yes | 37.7 | 14.8 | 38.9 | 74.1 | <.0001 |
| Vision problems | |||||
| Yes | 9.0 | 5.5 | 8.0 | 15.7 | <.0001 |
| Hearing problems | |||||
| Yes | 16.8 | 11.8 | 18.1 | 23.6 | <.0001 |
| Walking/balance problems | |||||
| Yes | 63.3 | 52.8 | 65.2 | 78.9 | <.0001 |
| Falls | |||||
| Yes | 36.4 | 28.6 | 39.6 | 46.1 | <.0001 |
| Health literacy | |||||
| Extremely | 34.4 | 43.5 | 31.6 | 22.1 | <.0001 |
| Quite a bit | 28.0 | 27.3 | 30.6 | 26.5 | |
| Somewhat | 16.7 | 13.5 | 16.9 | 21.8 | |
| A little bit | 5.9 | 4.3 | 6.8 | 7.6 | |
| Not at all | 11.1 | 7.6 | 10.1 | 17.9 | |
| BMI | |||||
| Underweight (BMI < 18.5) | 4.0 | 3.9 | 3.8 | 4.5 | .33 |
| Normal (BMI = 18.5-24.9) | 34.9 | 34.4 | 36.8 | 33.8 | |
| Overweight (BMI = 25-29.9) | 31.6 | 33.6 | 29.7 | 30.2 | |
| Obese (BMI = 30-39.9) | 21.6 | 21.0 | 22.0 | 22.2 | |
| Morbid obese (BMI ≥ 40) | 3.4 | 2.9 | 3.4 | 4.2 | |
Note. CM = care management; PCP = primary care physician; HCC = hierarchical condition category; VR-12 = Veteran’s RAND 12-item; BMI = body mass index; PCS = physical component score; MCS = mental component score.
Propensity Weighting for Survey Non-Response Bias
Propensity weighting was used to adjust for potential selection bias often associated with survey response to enhance the generalizability of these findings. The propensity weighting utilized available information about the demographic, socioeconomic, and health status variables described above that could potentially influence survey response. This information was used to estimate the underlying probability of survey response for each individual. We then used that estimated probability to create and apply a weighting variable to the data, to make those who did respond better resemble all eligible insureds who received the survey. The utility of such propensity weighting models to adjust for external validity threats is described elsewhere (Fairies, Haro, Obenchain, & Leon, 2010; Seeger, Williams, & Walker, 2005).
Statistical Models
Survey respondents were categorized into three possible groups based on their response to the loneliness questions: (a) no loneliness, (b) moderate loneliness, and (c) severe loneliness. Propensity weighted multivariate logistic regression modeling was used to determine significant characteristics associated with moderate and severe loneliness.
QOL physical and mental health component scores were calculated for each of the three loneliness categories, propensity weighted and regression adjusted for possible confounding variables listed in Table 1. Similarly, propensity weighted multivariate logistic regression models were used to examine the impact of loneliness along with other covariates on patient satisfaction with doctors, health care, and AARP Medicare Supplement plans.
Results
The overall response rate for the survey was 27% (N = 4,190). After the exclusion criteria were applied, 90% of survey respondents qualified for the study (N = 3,765). The unadjusted characteristics of the study sample are shown in Table 1. Overall, survey respondents were mostly female (56.1%), 75 years or older (76.7%), high income (50.3%), White race (90.9%) and 33.6% had engaged in a care management program. Problems with walking/balance were prevalent (63.3%), and 36.4% reported a fall in the previous 12 months.
Among survey respondents, the prevalence of moderate loneliness was 27% and severe loneliness was 28%. Overall, almost 55% in this sample experienced at least some level of loneliness.
Characteristics Associated With Severe and Moderate Loneliness
The strongest predictor of both severe and moderate loneliness was depression (Table 2). Other characteristics associated with severe loneliness included being female, having vision, hearing and walking/balance problems, having poorer health (high HCC scores), and urban location. High health literacy and first-dollar coverage insurance plans (indicating higher socioeconomic status) were protective against loneliness.
Table 2.
Characteristics Associated With Loneliness: Severe Loneliness and Moderate Loneliness.
| Characteristics associated with loneliness | Odds ratio | p value |
|---|---|---|
| Severe loneliness | ||
| Depression | 14.22 | <.0001 |
| Disengaged in CM | 2.05 | <.0001 |
| Vision problems | 1.82 | <.0001 |
| Problems with walking/balance | 1.77 | <.0001 |
| Female | 1.71 | <.0001 |
| Hearing problems | 1.69 | <.0001 |
| Urban location | 1.54 | <.0001 |
| Engaged in CM | 1.47 | <.0001 |
| Age 70-74 | 1.28 | .02 |
| HCC score in third quartile | 1.25 | .004 |
| Age 85+ | 1.23 | .03 |
| Age 75-79 | 1.23 | .04 |
| Lower middle income | 1.16 | .04 |
| First-dollar coverage insurance plans | 0.73 | <.0001 |
| High health literacy | 0.66 | <.0001 |
| Moderate loneliness | ||
| Depression | 3.43 | <.0001 |
| Hearing problems | 1.43 | <.0001 |
| Problems with walking/balance | 1.37 | <.0001 |
| Age 85+ | 1.27 | .003 |
| Female | 1.27 | <.0001 |
| Age 80-84 | 1.22 | .02 |
| Urban location | 1.19 | .02 |
| Engaged in CM | 1.15 | .01 |
| PCPs per 1,000 | 1.00 | <.0001 |
| Lower middle income | 0.86 | .02 |
| High health literacy | 0.83 | <.0001 |
| Overweight (BMI = 25-29.9) | 0.81 | .0001 |
| First-dollar coverage insurance plans | 0.77 | <.0001 |
| Underweight | 0.76 | .01 |
Note. Results are weighted to account for survey non-response. CM = care management; HCC = hierarchical condition category; PCP = primary care physician; BMI = body mass index.
Similarly, other characteristics associated with moderate loneliness included being older, being female, and having hearing and walking/balance problems, although odds ratios (ORs) were consistently lower than those demonstrated for severe loneliness. High health literacy, overweight, and first-dollar coverage insurance plans were protective.
Impact of Loneliness on QOL
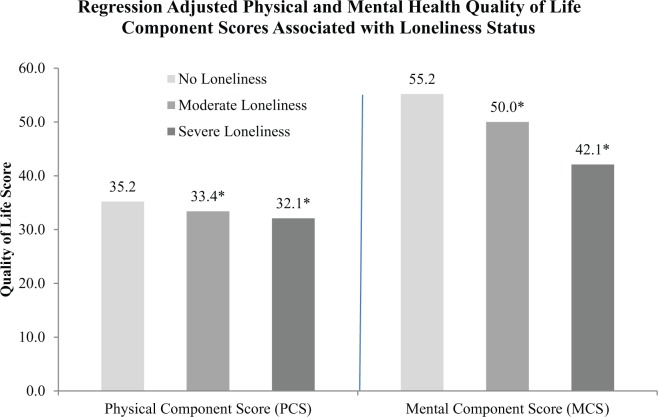
Severe and moderate loneliness significantly reduced both PCS and MCS components of QOL (Figure 1). Compared with the group with no loneliness, the PCS was reduced by 5% and 9% by moderate and severe loneliness, respectively (p < .0001), after regression adjustment for confounding variables. As expected, the magnitude of impact on loneliness on the MCS was considerably greater. The adjusted MCS was reduced by 9% and 24% by moderate and severe loneliness, respectively (p < .0001).
Figure 1.
Impact of Loneliness on Quality of Life: Physical (PCS) and Mental (MCS) Health Component Scores.
Note: Compared to no loneliness PCS scores were reduced by 5% and 9% for moderate and severe loneliness respectively. MCS scores were reduced by 9% and 24%, respectively.
*p<0.0001; regression adjusted for confounding variables listed in Table 1 and weighted to account for survey non-response.
Impact of Loneliness on Patient Satisfaction
The strongest predictor of dissatisfaction with doctors, health care, and Medicare Supplement plans was severe loneliness (Tables 3, 4, and 5). One of the strongest predictors of increased satisfaction with medical services was high health literacy. Other characteristics associated with increased patient satisfaction included more inclusive insurance coverage (first-dollar coverage plans), poorer health (high HCC scores), and problems with walking/balance (perhaps an indicator of visible health issues). Being older, overweight, obese or morbidly obese and minority as well as moderate loneliness were associated with increased dissatisfaction with medical services delivery.
Table 3.
Satisfaction With Doctors.
| Characteristic | Odds ratio | p value |
|---|---|---|
| Problems with walking/balance | 1.44 | <.0001 |
| High health literacy | 1.38 | <.0001 |
| HCC score second quartile | 1.25 | .0005 |
| HCC score third quartile | 1.22 | .002 |
| Vision problems | 1.18 | .02 |
| First-dollar coverage insurance plans | 1.17 | .001 |
| PCP per 1,000 | 1.00 | .002 |
| Overweight (BMI = 25-29.9) | 0.88 | .01 |
| Urban location | 0.83 | .009 |
| Engaged in CM | 0.82 | .0002 |
| Age 70-74 | 0.81 | .03 |
| Moderate loneliness | 0.69 | <.0001 |
| Age 75-79 | 0.61 | <.0001 |
| Age 80-84 | 0.58 | <.0001 |
| Age 85+ | 0.53 | <.0001 |
| Severe loneliness | 0.38 | <.0001 |
Note. Results are weighted to account for survey non-response. HCC = hierarchical condition category; PCP = primary care physician; BMI = body mass index; CM = care management.
Table 4.
Satisfaction With Health Care.
| Characteristic | Odds ratio | p value |
|---|---|---|
| High health literacy | 1.57 | <.0001 |
| HCC score third quartile | 1.22 | .002 |
| First-dollar coverage insurance plans | 1.16 | .001 |
| Hearing problems | 0.89 | .03 |
| Engaged in CM | 0.86 | .002 |
| Urban location | 0.81 | .001 |
| Moderate loneliness | 0.70 | <.0001 |
| Morbid obesity (BMI ≥ 40) | 0.66 | .0002 |
| Age 85+ | 0.65 | <.0001 |
| Age 80-84 | 0.62 | <.0001 |
| Severe loneliness | 0.36 | <.0001 |
Note. Results are weighted to account for survey non-response. HCC = hierarchical condition category; CM = care management; BMI = body mass index.
Table 5.
Satisfaction With AARP Medicare Supplement Insurance.
| Characteristic | Odds ratio | p value |
|---|---|---|
| High health literacy | 2.03 | <.0001 |
| Low income | 1.58 | <.0001 |
| Upper middle income | 1.48 | <.0001 |
| First-dollar coverage insurance plans | 1.45 | <.0001 |
| Lower middle income | 1.43 | <.0001 |
| HCC score third quartile | 1.36 | <.0001 |
| Problems with walking/balance | 1.30 | <.0001 |
| Age 75-79 | 1.29 | .01 |
| HCC score fourth quartile | 1.17 | .03 |
| PCP per 100,000 | 1.00 | .0006 |
| Hearing problems | 0.88 | .04 |
| Moderate loneliness | 0.82 | .001 |
| Urban location | 0.82 | .02 |
| Obesity (BMI = 30-39.9) | 0.80 | .001 |
| Minority | 0.74 | <.0001 |
| Severe loneliness | 0.59 | <.0001 |
Note. Results are weighted to account for survey non-response. HCC = hierarchical condition category; PCP = primary care physician; BMI = body mass index.
Discussion
Among this sample of older, sicker adults eligible for care management programs, almost 55% suffered at least some level of loneliness: 27% with moderate and 28% with severe loneliness. The prevalence of loneliness in this population is somewhat higher than in older populations cited in the scientific literature but similar to the 60% moderate and severe loneliness reported by Taube et al. (2014) in older frail adults. While other chronic conditions (e.g., diabetes or heart disease) common among older adults have medical solutions, loneliness is difficult to define and/or diagnose and even more complicated to provide medical or other interventions. Depression is the characteristic most highly associated with loneliness in our study and others, yet depression is generally treated without regard to loneliness (van Beljouw et al., 2014).
Loneliness was also characterized by vision, hearing, and mobility impairments, which can dramatically affect social connectedness by limiting the ability to drive (Perissinotto et al., 2012; Schnittger et al., 2012), walk (Buchman et al., 2010; Hawkley et al., 2009), or hear conversations (Pronk et al., 2011). However, without generalized screening tools, recommended medical or psychological protocols, or established interventions or solutions, loneliness has received limited attention from medical and mental health professionals.
Loneliness significantly affected both physical and mental dimensions of QOL. PCSs were reduced by 5% and 9% by moderate and severe loneliness. To date, no studies have documented the impact of loneliness on physical dimensions of QOL. However, these findings are consistent with studies documenting that loneliness is associated with functional decline (Aartsen & Jylha, 2011; Buchman et al., 2010; Cohen-Mansfield & Parpura-Gill, 2007; Golden et al., 2009; Lim & Kua, 2011) and reduced physical activity (Dahlberg & McKee, 2014; Hawkley et al., 2009; Lim & Kua, 2011; Luo et al., 2012; Netz et al., 2013; Perissinotto et al., 2012).
Our results indicated a greater impact on the mental health component scores with reductions of 9% and 24% by moderate and severe loneliness. Only Lim and Kua (2011; using the Short Form Health Survey 12-item (SF-12)) can be directly compared with our QOL results based on the VR-12. These researchers focused only on the mental components of QOL, demonstrating an 11.5% decrease on the MCS score when they grouped fairly and very lonely respondents with a single loneliness question.
Severe loneliness was the strongest predictor of patient dissatisfaction with the delivery of medical services, including doctors, general health care, or Medicare Supplement plans. Patient satisfaction (weighted and regression adjusted) was decreased by 40% to 63% with severe loneliness and by 20% to 30% with moderate loneliness. To date, no studies have considered the impact of loneliness on patient satisfaction. However, our results are consistent with other studies that have demonstrated that anxiety (Hundt et al., 2013; Stein et al., 2011) and mental health treatments (Chen et al., 2006; Hasler et al., 2004; Lippens & Mackenzie, 2011) are often associated with reduced patient satisfaction. In these studies, symptom improvement and social support played a significant role in both treatment satisfaction and perceived effectiveness (Hasler et al., 2004; Hundt et al., 2013; Lippens & Mackenzie, 2011; Shea et al., 2007).
More recently, patient satisfaction has become a measure of quality of care in the United States (Chen et al., 2006; Hundt et al., 2013; Stein et al., 2011) as well as other countries (Hasler et al., 2004; Lippens & Mackenzie, 2011). Furthermore, provider and health insurance reimbursement rates in the United States are often tied to patient satisfaction. Some researchers have suggested that lonely individuals look to their medical professionals for social support and understanding, resulting in increased doctor and emergency room visits (Geller, Janson, McGovern, & Valdini, 1999), simply for the social contact (Hawkley et al., 2010). Thus, medical professionals may need additional training to develop an awareness of and sensitivity for the additional mental health needs among older populations.
In contrast, high health literacy was one of the strongest promoters of high patient satisfaction and protective against loneliness. Health literacy affects physician–patient communication, as those with inadequate health literacy are less likely to ask questions and/or to adhere to medication protocols, and more likely to misunderstand physician recommendations and to have poorer health outcomes (Aboumatar, Carson, Beach, Roter, & Cooper, 2013; Shea et al., 2007; Williams, Davis, Parker, & Weiss, 2002; Zhang, Terry, & McHorney, 2014). These results indicate that educational programs and/or improved health communications targeted to appropriate reading abilities could improve health literacy among older adults with the potential to improve patient satisfaction and medical outcomes and reduce loneliness.
No loneliness interventions have proven to be generally successful—a testament to the difficulty in targeting loneliness as a condition (Hawkley et al., 2010). While loneliness, social isolation, social support, and depression are often interrelated, they are distinct constructs requiring interventions focused on different elements of social interactions (Golden et al., 2009; Hawkley et al., 2009; Hawkley et al., 2010; Perissinotto et al., 2012). Some success has been demonstrated for problem-solving therapies that empower these individuals to seek solutions to their unique circumstances and consequently improve depression and perceptions of disability (Choi et al., 2014).
Other interventions have included promoting involvement in social settings (e.g., senior centers) with mixed success (Cohen-Mansfield & Perach, 2014). Increased physical activity appears to be protective against loneliness; however, few interventions have incorporated elements of physical activity programs (Dahlberg & McKee, 2014; Hawkley et al., 2009; Luo et al., 2012). Various technologies (e.g., computers, tablets) have been used in research studies with promise (Hagan, Manktelow, Taylor, & Mallett, 2014), but costs and limited exposure to these technologies among older adults have limited their acceptance.
Our study sample of AARP Medicare Supplement members included a sampling strategy to oversample those eligible for a case management program; thus, our results will not generalize to all Medicare Supplement populations. Our response rate was relatively low at 27%; however, we utilized propensity weighting to adjust for survey response bias among this older, sicker study group. While our methods are robust, sources of bias among respondents may not have been completely eliminated. Strengths of the study include the use of the validated UCLA-3 screening scale for loneliness and the validated VR-12 QOL measure. In the United States, the UCLA three-item scale has become more widely used among researchers and may provide a suitable tool for medical professionals to consistently screen for loneliness within populations that are accessible (e.g., through doctor visits, care management programs, etc.). The VR-12 QOL scale has been validated for older populations and, along with patient satisfaction, provides us with insight into patient perceptions of the quality of medical care delivery and the burden that loneliness puts on QOL.
Conclusion
Loneliness is a common problem among older adults: More than 55% of this older, sicker subgroup of older adults experienced some level of loneliness. Our learnings suggest that loneliness significantly affects QOL and patient satisfaction with medical services. While medical interventions for other less prevalent chronic conditions are common, surprisingly few interventions for loneliness currently exist, especially considering the high prevalence of loneliness among at-risk older populations. Taking into account the potential for improvements in QOL and patient satisfaction, screening for loneliness may be warranted, along with tailored interventions that provide emotional support, enhanced coping strategies, and/or problem-solving therapies.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Aanes M. M., Hetland J., Pallesen S., Mittelmark M. B. (2011). Does loneliness mediate the stress-sleep quality relation? The Hordaland Health Study. International Psychogeriatrics, 23, 994-1002. [DOI] [PubMed] [Google Scholar]
- Aartsen M., Jylha M. (2011). Onset of loneliness in older adults: Results of a 28 year prospective study. European Journal of Ageing, 8, 31-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aboumatar H. J., Carson K. A., Beach M. C., Roter D. L., Cooper L. A. (2013). The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. Journal of General Internal Medicine, 28, 1469-1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amieva H., Stoykova R., Matharan F., Helmer C., Antonucci T. C., Dartiques J. F. (2010). What aspects of social network are protective for dementia? Not the quantity but the quality of social interactions is protective up to 15 years later. Psychosomatic Medicine, 72, 905-911. [DOI] [PubMed] [Google Scholar]
- Buchman A. S., Boyle P. A., Wilson R. S., James B. D., Leurgans S. E., Arnold S. E., Bennett D. A. (2010). Loneliness and the rate of motor decline in old age: The rush memory and aging project, a community-based cohort study. BMC Geriatrics, 10, 77-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J. T., Hughes M. E., Waite L. J., Hawkley L. C., Thistel R. A. (2006). Loneliness as a specific risk factor for depressive symptoms; cross-sectional and longitudinal analyses. Psychology and Aging, 21, 140-151. [DOI] [PubMed] [Google Scholar]
- Chen H., Coakley E. H., Cheal K., Maxwell J., Costantino G., Krahn D. D., . . .Levkoff S. E. (2006). Satisfaction with mental health services in older primary care patients. American Journal of Geriatric Psychiatry, 14, 371-379. [DOI] [PubMed] [Google Scholar]
- Choi N. G., Marti C. N., Bruce M. L., Hegel M. T., Wilson N. L., Kunik M. E. (2014). Six-month post-intervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depression and Anxiety, 31, 653-661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J., Parpura-Gill A. (2007). Loneliness in older persons: A theoretical model and empirical findings. International Psychogeriatrics, 19, 279-294. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J., Perach R. (2014). Interventions for alleviating loneliness among older adults: A critical review. American Journal of Health Promotion, 29(3), e109-e125. [DOI] [PubMed] [Google Scholar]
- Dahlberg L., McKee K. J. (2014). Correlates of social and emotional loneliness in older people: Evidence from an English community study. Aging & Mental Health, 18, 504-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellwardt L., Aartsen M., Deeg D., Steverink N. (2013). Does loneliness mediate the relation between social support and cognitive functioning in later life? Social Science & Medicine, 98, 116-124. [DOI] [PubMed] [Google Scholar]
- Fairies D. E. L., Haro J. M., Obenchain R. L., Leon A. C. (Eds.). (2010). Analysis of observational healthcare data using SAS. Cary, NC: SAS Institute. [Google Scholar]
- Geller J., Janson P., McGovern E., Valdini A. (1999). Loneliness as a predictor of hospital emergency department use. Journal of Family Practice, 48, 801-804. [PubMed] [Google Scholar]
- Golden J., Conroy R. M., Bruce I., Denihan A., Greene E., Kirby M., Lawlor B. A. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24, 694-700. [DOI] [PubMed] [Google Scholar]
- Hagan R., Manktelow R., Taylor B. J., Mallett J. (2014). Reducing loneliness amongst older people: A systematic search and narrative review. Aging & Mental Health, 18, 683-693. [DOI] [PubMed] [Google Scholar]
- Hasler G., Moergeli H., Bachmann R., Lambreva E., Buddeberg C., Schnyder U. (2004). Patient satisfaction with outpatient psychiatric treatment: The role of diagnosis, pharmacotherapy and perceived therapeutic change. Canadian Journal of Psychiatry, 49, 315-321. [DOI] [PubMed] [Google Scholar]
- Hawkley L. C., Thisted R. A., Cacioppo J. T. (2009). Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychology, 28, 354-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley L. C., Thisted R. A., Masi C. M., Cacioppo J. T. (2010). Loneliness predicts increased blood pressure: Five-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging, 25, 132-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holwerda T. J., Deeg D. J. H., Beekman A. T., van Tilburg T. G., Stek M. L., Jonker C., Schoevers R. A. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam Study of the Elderly (AMSTEL). Journal of Neurology, Neurosurgery, & Psychiatry, 85, 135-142. [DOI] [PubMed] [Google Scholar]
- Hughes M. E., Waite L. J., Hawkley L. C., Cacioppo J. T. (2004). A short scale for measuring loneliness in large surveys. Research on Aging, 26, 655-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hundt M. E., Armento M. E., Porter B., Cully J. A., Kunik M. E., Stanley M. (2013). Predictors of treatment satisfaction among older adults with anxiety in a primary care psychology program. Evaluation and Program Planning, 37, 58-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2013, April). Medigap: Spotlight on enrollment, premiums, and recent trends. Retrieved from http://kaiserfamilyfoundation.files.wordpress.com/2013/04/8412-2.pdf
- Kosinski M., Bayliss M., Bjorner J. B., Ware J. E. (2000). Improving estimates of SF-36® health survey scores for respondents in missing data. Medical Outcomes Trust Monitor, 5, 8-10. [Google Scholar]
- Lim L. L., Kua E. H. (2011). Living alone, loneliness, and psychological well-being of older persons in Singapore. Current Gerontology & Geriatrics Research, 2011, Article 673181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippens T., Mackenzie C. S. (2011). Treatment satisfaction, perceived treatment effectiveness, and dropout among older users of mental health services. Journal of Clinical Psychology, 67, 1197-1209. [DOI] [PubMed] [Google Scholar]
- Luo Y., Hawkley L. C., Waite L. J., Cacioppo J. T. (2012). Loneliness, health, and mortality in old age: A National Longitudinal Study. Social Science & Medicine, 74, 907-914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh J. E., Lawlor B. A. (2013). Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. British Journal of Health Psychology, 18, 546-555. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute Obesity Task Force. (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—The evidence report. Obesity Research, 6(Suppl. 2), 51-209. [PubMed] [Google Scholar]
- Netz Y., Goldsmith R., Shimony T., Arnon M., Zeev A. (2013). Loneliness is associated with increased risk of sedentary life in older Israelis. Aging & Mental Health, 17, 40-47. [DOI] [PubMed] [Google Scholar]
- Perissinotto C. M., Cenzer I. S., Covinsky K. E. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172, 1078-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope G. C., Kautter J., Ingber M. J., Freeman S., Sekar R., Newhart C. (2011). Evaluation of the CMS-HCC Risk Adjustment Model. Retrieved from http://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/downloads/evaluation_risk_adj_model_2011.pdf
- Pronk M., Deeg D. J., Smits C., van Tilburg T. G., Kuik D. J., Festen J. M., Kramer S. E. (2011). Prospective effects of hearing status on loneliness and depression in older persons: Identification of subgroups. International Journal of Audiology, 50, 887-896. [DOI] [PubMed] [Google Scholar]
- Schnittger R. I., Wherton J., Prendergast D., Lawlor B. A. (2012). Risk factors and mediating pathways of loneliness and social support in community-dwelling older adults. Aging & Mental Health, 16, 335-346. [DOI] [PubMed] [Google Scholar]
- Seeger J. D., Williams P. L., Walker A. M. (2005). An application of propensity score matching using claims data. Pharmacoepidemiology & Drug Safety, 14, 465-476. [DOI] [PubMed] [Google Scholar]
- Selim A. J., Rogers W., Fleishman J. A., Qian S. X., Fincke B. G., Rothendler J. A., Kazis L. E. (2009). Updated US population standard for the Veterans RAND 12-item Health Survey (VR-12). Quality of Life Research, 18, 43-52. [DOI] [PubMed] [Google Scholar]
- Shea J. A., Cuerra C. E., Ravenell K. L., McDonald V. J., Henry C. A., Asch D. A. (2007). Health literacy weakly but consistently predicts primary care patient dissatisfaction. International Journal for Quality in Health Care, 19, 45-49. [DOI] [PubMed] [Google Scholar]
- Stein M. B., Roy-Byrne P. P., Craske M. G., Campbell-Sills L., Lang A. J., Golinelli D., . . .Sherbourne C. D. (2011). Quality of and patient satisfaction with primary health care for anxiety disorders. Journal of Clinical Psychiatry, 72, 970-976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A., Shankar A., Demakakos P., Wardle J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences of the United States of America, 110, 5795-5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taube E., Kristensson J., Sandberg M., Midlov P., Jakobsson U. (2014). Loneliness and health care consumption among older people. Scandinavian Journal of Caring Sciences. doi: 10.1111/scs.12147. [DOI] [PubMed] [Google Scholar]
- van Beljouw I. M. J., van Exel E., de Jong Gierveld J., Comijs H. C., Heerings M., Stek M. L., van Marwijk H. W. (2014). “Being all alone makes me sad”: Loneliness in older adults with depressive symptoms. International Psychogeriatrics, 9, 1-11. [DOI] [PubMed] [Google Scholar]
- Victor C. R., Bowling A. (2012). A longitudinal analysis of loneliness among older people in Great Britain. Journal of Psychology, 146, 313-331. [DOI] [PubMed] [Google Scholar]
- Wallace L. S., Rogers E. S., Roskos S. E., Holiday D. B., Weiss B. D. (2006). Screening items to identify patients with limited health literacy skills. Journal of General Internal Medicine, 21, 874-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M. V., Davis T., Parker R. M., Weiss B. D. (2002). The role of health literacy in patient-physician communication. Family Medicine, 34, 383-389. [PubMed] [Google Scholar]
- Zhang N. J., Terry A., McHorney C. A. (2014). Impact of health literacy on medication adherence: A systematic review and meta-analysis. The Annals of Pharmacotherapy, 48, 741-751. [DOI] [PubMed] [Google Scholar]