Abstract
Objective: The objective of this review was to assess published literature relating to health literacy and older adults. Method: The current review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta Analyses. Results: Eight articles met inclusion criteria. All studies were conducted in urban settings in the United States. Study sample size ranged from 33 to 3,000 participants. Two studies evaluated health-related outcomes and reported significant associations between low health literacy and poorer health outcomes. Two other studies investigated the impact of health literacy on medication management, reporting mixed findings. Discussion: The findings of this review highlight the importance of working to improve health care strategies for older adults with low health literacy and highlight the need for a standardized and validated clinical health literacy screening tool for older adults.
Keywords: older adults, aging, health literacy, health outcomes, medication adherence, cognition, health disparities
Introduction
Health literacy is an important topic in today’s health care environment (Cutilli, 2007). Ratzan and Parker (2000) define health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” (p. 4) Studies suggest that low health literacy levels are predictors of disparaging health outcomes. Patients with low health literacy use emergency services more frequently (Baker et al., 2002), have higher health care costs (Weiss & Palmer, 2004), utilize preventive services such as vaccinations and mammograms less frequently (Scott, Gazmararian, Williams, & Baker, 2002), and are associated with higher mortality rates (Baker et al., 2007). Socioeconomic status, age, race, cognition, and education level are considered contributing factors of health literacy levels, with age as one of the highest correlates of low health literacy (Cutilli, 2007).
Older adults (age 65 and older) are currently the fastest growing population in the United States. It is estimated that older adults will account for 20% of the population by 2030 (Federal Interagency Forum on Aging-Related Statistics, 2008). The 2003 National Assessment of adult literacy estimated only 3% of older adults, 65 and older, were proficient with health literacy skills (Kutner, Greenburg, Jin, & Paulsen, 2006). There are several different age-related changes that could contribute to the decrease in health literacy in older adults. Although the rate and severity of these age-related changes vary among individuals, these should be considered when assessing an older adult’s health literacy. A decline in an older adult’s cognitive ability could contribute to an older adult’s ability to comprehend and/or recall new topics (Craik & Byrd, 1982; Cornett, 2006; Kintsch, 1998). Physical impairments such as hearing and vision loss may also contribute to a decreased ability to process health information (Cornett, 2006; Speros, 2009). Psychosocial factors such as socioeconomic status and coping may negatively influence understanding health information (Cornett, 2006). Regrettably, as the gap in physical and cognitive ability between younger generations and older adults widen, it can lead to a sense of shame and embarrassment which reduces effective communication conduits and further complicates older adult health literacy (Cornett, 2006; Speros, 2009).
In an attempt to further understand health literacy in the older population, a systematic literature review was conducted. The current review includes studies specifically designed to measure the older adult population (65 years of age and older) and health literacy, related health outcomes, and interventions. Due to the limited number of articles published in this research area, the authors elected to include publications older than 5 years. Eight articles investigating older adults and health literacy met the inclusion criteria. Only one review specifically addressed health literacy and older adults; however, this review was published in 2007 (Cutilli, 2007). The remaining reviews addressed a concept analysis of the term health literacy in older adults, low health literacy and health outcomes, and health literacy among older cancer patients (Amalraj, Starkweather, Nguyen, & Naeim, 2009; Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011; Oldfield & Dreher, 2010). The most recent of these reviews, Berkman et al. (2011), comprehensively addressed a broad population (young and old) and a variety of measures related to health literacy. With respect to older adults, the authors identified and discussed five studies specifically addressing older adults. Based on review of these five studies, Berkman concluded that within these samples, older adults with low health literacy also exhibited poorer health. Given the importance for responsible health care stewardship, it is necessary for those involved in the care of older adults to understand the impact of health literacy, and the unique factors that affect older adults. As such, an updated systematic review regarding the health literacy of older adults is warranted to establish what is known and what can be done to help prepare older adults to make the best health care decisions.
Method
The current review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA; Fink et al., 2010; Moher, Liberati, Tetzlaff, Altman, & Grp, 2009). Medline was used to identify peer-reviewed literature that included a combination of free-text and thesaurus terms for concepts including “health literacy, elderly, geriatrics, older adult, and low health literacy,” combined with a qualitative and quantitative methods filter, respectively. Detailed search terms have been listed by database in Table 2. Searches were limited to January 1, 2010, through December 31, 2014, including only publications written in English and conducted within the United States. Our study overlapped the Berkman et al. (2011) review by several months to ensure no published studies were omitted. This strategy was adapted for other databases as required. A complete list of the database search construction is found in Table 1. To identify the relevant literature for this review, five electronic databases were searched: MEDLINE®, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Cochrane Library, PsychINFO, and the Educational Resources Information Center (ERIC). Citations were imported into EndNote® data management software, when possible. Duplicate studies were identified and removed. Older adults were defined as age 65 years old and older as commonly defined in industrialized countries and clinically within the United States (Hinrichsen & Molinari, 1998).
Table 2.
Summary of Health Literacy Studies.
| Reference | Sample and setting | Health literacy measurement | Methodology | Key findings: Health literacy | Associated factors |
|---|---|---|---|---|---|
| Wolf, Feinglass, Thompson, and Baker (2010) |
n = 2,956; 65+ years Medicare enrollees English speaking Multisite: Cleveland, Houston, Tampa and Fort Lauderdale/Miami |
S-TOFHLA (divided into 7 categories instead of typical 3) | Cross-sectional questionnaire Interviewer-administered survey (1 hr in-home) Compared HL to self-rated physical function, mental health, and mortality rates |
Low HL associated with older age, non-White, lower income, less education, abstinence from alcohol consumption, less frequent PA and underweight Low HLs reported more activity limitations and worse baseline physical functioning and mental health Literacy could be causally related to physical functioning; decrease cognitive skills may lead to progressively lower understanding of how to stay healthy, when to seek medical attention, and how to properly follow medical regimens to recover from acute and care for chronic health conditions |
Graded relationship between literacy scores and baseline physical functioning (lowest 3 HL scores poorer physical function compared with highest HL category) Relationship to mental health was a threshold rather than continuous (Categories 1 and 2 worse mental health compared with Category 7) All-cause mortality rate greater for those with lowest HL |
| Gerber, Cho, Arozullah, and Lee (2010) |
n = 450; 65+ years African American M = 78.2 years Caucasian M = 76.8 years Medicare recipients Chicago, IL |
S-TOFHLA | Cross-sectional questionnaire, interviewer-administered survey (in-home or medical center) Compared medication adherence by African American and Caucasian older adults |
More African Americans reported a history of hypertension (70.7% vs. 57.1%; p = .003) or diabetes (26.3% vs. 14.7%; p = .003), worse health status, lower health literacy, worse depression scores, and less social support compared with Caucasians (all, p < .001). African Americans were more likely to report running out of medications before refilling them and not always following physician instructions on how to take medications. No difference between races was observed in forgetting to take medications. |
Even after adjusting for differences in demographics, health literacy, depression, and social support, older African Americans reported following medication directions less often than older Caucasians. |
| Ganzer, Insel, and Ritter (2012) |
n = 56; 65+ years M = 80.4 years English speaking Community dwelling NYC metro area |
S-TOFHLA | Cross-sectional survey Descriptive pilot study Relationship between working memory, HL, and recall of five signs of stroke |
Over 50% of the sample had high health literacy Signs of stroke recalled M = 2.9 ± 1.33 Stroke sign recall was associated with working memory (r = .38, p < .01), health literacy (r = .44, p < .01), education (r = .36, p < .01), and dementia (r = .54, p < .01). Working memory was positively associated with education (r =.58, p < .01), income that meets expenses (r = −.34, p < .05), health literacy (r = .57, p < .01), and age (r = −.33, p < .05). Health literacy was significantly related to education (r = .46, p < .01). Using regression, health literacy was the best predictor of stroke recall (β = .56, p < .01). |
With additional regression analysis considering working memory, health literacy and dementia together, both health literacy (β = .28, p < .05) and dementia (β = .44, p < .01) were significantly associated with recall of signs of stroke. Results demonstrate that working memory and health literacy were significantly associated with recall of the signs of stroke. Only health literacy remained a significant predictor of the recall of the warning signs of stroke When MMSE (dementia) was included in regression, health literacy remained a significant predictor of recall, but dementia was more strongly associated with recall. |
| McDougall, Mackert, and Becker (2012) |
n = 45; 65+ years M = 77.11 years Community-residing older adults Central Texas metro area |
REALM | Pilot study Cross-sectional Relationship between health literacy, memory performance, and performance-based functional ability |
Health literacy not related to education (.19) or age (−.15) Education and cognition (.30) were associated significantly. Health literacy was associated with RBMT memory performance groups (normal vs. poor; .25) and DAFS-E scores (.50). |
Education was not related to health literacy |
| Patel (2010); Detroit, MI |
n = 62; 65+ years M = 73.2 years African American Primary care setting |
S-TOFHLA, NVS | Evaluated utility of NVS and S-TOFHLA | No significant differences in NVS and S-TOFHLA scores between men and women. Fifty percent of participants were deemed sufficiently literate using S-TOFHLA in comparison with 42% using NVS. Mean time to complete NVS was 11.7 min. Previous research in younger population reports completion time to be 2.9 min. |
Patient’s educational level and age were better predictors than NVS score for assessing health literacy in this population. |
| Mosher, Lund, Kripalani, and Kaboli (2012) |
n = 310, 65+ years M = 74 years Veterans from a primary care clinic English speaking Iowa City, VA Center |
REALM | Cross-sectional Face-to-face interview Examined association of health literacy with medication knowledge, adherence, and adverse drug events |
Lower health literacy was associated with less knowledge of medication names and purposes. Patients with low health literacy knew 32.2% of medications by name, as compared with 54.6% of medication names for patients with marginal health literacy, and 60.8% for patients with adequate health literacy (p < .001). Lower literacy group knew the purpose of 61.8% of their medications, compared with 77.4% and 81.4% in the marginal and adequate literacy groups, respectively (p < .001). |
Health literacy was not associated with self-reported medication adherence or adverse drug events Health literacy was not associated with number of prescribed medications |
| Cordasco, 2011 |
n = 160, age 65+ years M = 72.0 years Spanish speaking Diagnosed with diabetes for at least 1 year Clinics associated with a large safety-net hospital LA County, CA |
Spanish REALM, S-TOFHLA, and SILS | Cross-sectional One-on-one interview Evaluated accuracy of SILS in detecting IHL in monolingual Spanish speakers; investigates best predictor SILS or education level |
S-TOFHLA indicated 84% had IHL Best performing SILS question, “How confident are you filling out medical forms by yourself?” AUROC curve of 0.82; high sensitivity (fewer than 1 out of 10 with IHL will be missed), low specificity (7 out of 10 with IHL will be misclassified) Remaining two SILS questions had AUROC curves less than 0.50. Educational achievement AUROC curve was 0.88; education cutoff of 6 years or less had a specificity to 0.81 and sensitivity of 0.83 |
Use single items as screen for IHL in older U.S. monolingual Spanish speakers Should either use the “confidence with forms” SILS, being aware of its specificity limitations, or a single question assessing educational achievement |
| Bickmore et al. (2010) |
n = 33; 65+ years English speaking Boston Medical Center |
TOFHLA | Two-armed intervention trial; evaluated the use of computer animated characters as vehicles for health education and behavioral change counseling | Participants with inadequate health literacy had lower levels of computer literacy compared with participants with adequate health literacy, although this difference was only trending toward significance, likely due to the smaller sample size | Overall, there were very few differences in measures of acceptance and usability between patients with adequate and inadequate health literacy, suggesting that ECAs are approachable and usable by patients regardless of health literacy level. In the few measures in which there were significant or near-significant differences on health literacy, these were mostly in favor of patients with inadequate health literacy. |
Note. S-TOFHLA = Short Test of Functional Health Literacy in Adults; HL = health literacy; MMSE = minimum mean square error; REALM = Rapid Estimate of Adult Literacy in Medicine; NVS = Newest Vital Sign; SILS = Single Item Literacy Screening; ECA = Embodied Conversational Agents; PA = physical activity; RBMT = rivermead behavioral memory test; DAFS-E = direct assessment of functional status-extended; IHL = inadequate health literacy;
AUROC = areas under the receiving-operator characteristic.
Table 1.
Database Search Construction.
| Search | Search term construction | Articles located |
|---|---|---|
| 1. PubMed (MEDLINE) | “United States”[Mesh] AND (elderly OR geriatric*) AND “health literacy” Filter: 2010/01/01 to 2015/12/31 | 260 |
| 2. CINAHL | “health literacy” AND (elderly OR geriatric*) | 97 |
| **Variant search | ((“health literacy” AND (elderly OR geriatric*)) AND United States **US as keyword addition** | 22 |
| 3. ERIC | health literacy AND (elderly OR geriatric*) | 35 |
| **Variant search | health literacy AND (elderly OR geriatric) AND United States **US as keyword addition** | 5 |
| 4. Cochrane Library | MeSH descriptor: [United States] combined with health literacy AND (elderly OR geriatric*) | 36 |
| **Variant search | MeSH descriptor: [United States] combined with “health literacy” | 238 |
| 5. PsycINFO | “health literacy” AND (elderly OR geriatric*) AND lo.Exact(“US”) | 61 |
| **Variant search | health literacy AND (elderly OR geriatric*) AND lo.Exact(“US”) | 86 |
Note. CINAHL = Cumulative Index to Nursing and Allied Health Literature; ERIC = Educational Resources Information Center.
Key Questions
The key questions we answer in this article are as follows: For studies published regarding health literacy with participants’ age 65 years old and older, what is the evidence regarding:
how health literacy is assessed,
the demographics of study participants,
what health outcomes have been measured,
levels of medication adherence,
whether cognitive function and health literacy interventions were developed or tested.
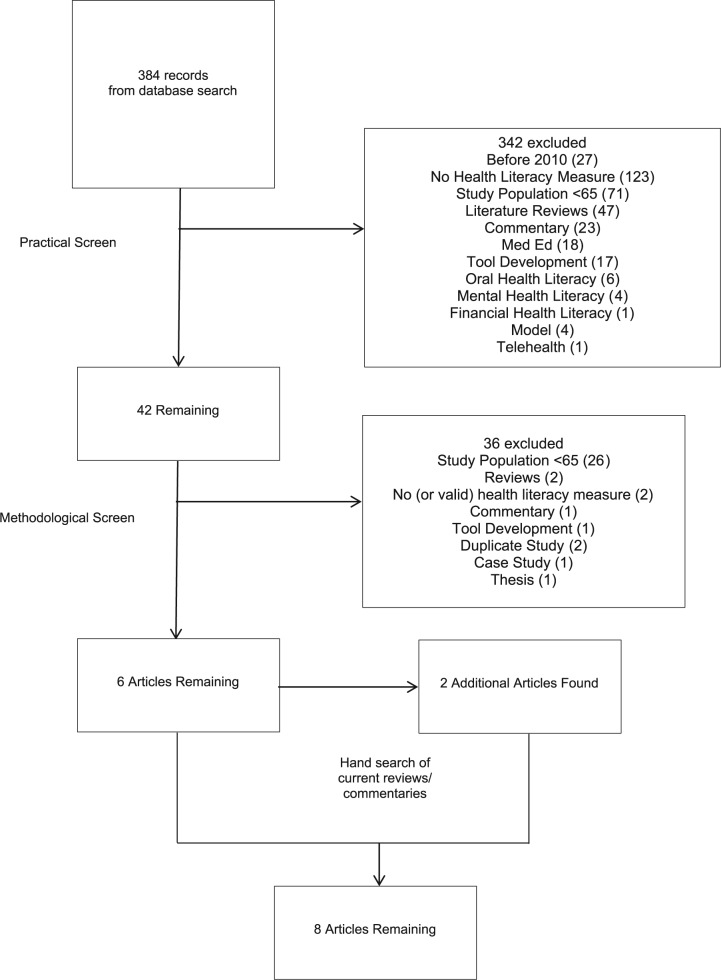
A practical screen of the literature where a broad range of potentially useable articles that could be obtained in a timely manner was conducted (Fink et al., 2010). The authors conducted the initial screen using titles and abstracts. When information was not available within the abstract, each full-text article was located and screened for the initial inclusion criteria. Inclusion criteria included the following: (a) measure of health literacy, (b) older adult population (age 65 and older), (c) empirically based research methodology, and (d) a published time period of 2010-2014. The exclusion criteria included the following: (a) review/discussion articles; (b) case studies, tool development, and medical education studies; (c) articles published prior to the Berman (2011) review; and (d) oral, financial, and mental health literacy. The methodological screen (used to assess quality of articles and selection of the best available studies) included empirical methodology to ensure the search was exhaustive and included a review of the reference sections in each of the retrieved articles, a checked of relevant articles against an index of retrieved articles, and a hand search of journals with published systematic reviews on health literacy. Two reviewers independently assessed all articles against the inclusion criteria. Any disagreements were discussed and resolved by a third reviewer. Due to the lack of evidence (only one article met our final criteria), the authors deemed it irrelevant to rate the quality of the studies, per the PRISMA guidelines. A flow diagram of the article selection process is detailed in Figure 1. Health literacy measures, characteristics of the target populations, data collection, and data results were extracted by four review authors. Articles were not excluded based on methodological quality criteria as this review was intended to review all empirical research in the subject area. No meta-analysis was conducted.
Figure 1.
Flow diagram article selection process.
Results
Study Selection
A total of 384 articles were identified for review using the primary inclusion and exclusion criteria (Figure 1). Three hundred forty-two articles were excluded due to study time period, lack of health literacy measure, population age, being a review, discussion article, case study, tool development (testing of health literacy measures, validation of health literacy measures, or comparison of new health literacy measures against older assessment tools in the general population), or medical education study. Of the 42 remaining articles, six remained after full-text evaluation of the inclusion of a health literacy measure and an older adult population. Two additional studies were included after a hand search of published systematic reviews resulting in eight total reviewed articles for the systematic review. Study setting, sample size, population, data collection method, health literacy measure, and key findings were noted for each of these studies (Table 2).
Study Characteristics
All studies discussed in the current review were conducted in urban settings. Three of the eight studies (38%) were multi-site investigations (Gerber, Cho, Arozullah, & Lee, 2010; McDougall, Mackert, & Becker, 2012; Wolf, Feinglass, Thompson, & Baker, 2010). Although all studies were conducted in the United States, the study settings were geographically diverse, including the east coast (Wolf et al., 2010), Midwest (Gerber et al., 2010; Mosher, Lund, Kripalani, & Kaboli, 2012; Patel et al., 2011), Northeast (Bickmore et al., 2010; Ganzer, Insel, & Ritter, 2012), and South (McDougall et al., 2012; Wolf et al., 2010). Half of the studies were conducted in primary care settings (n = 4; Bickmore et al., 2010; Cordasco, Homeier, Franco, Wang, & Sarkisian, 2012; Mosher et al., 2012; Patel et al., 2011), two in community settings (n = 2; Ganzer et al., 2012; McDougall et al., 2012), and two conducted in-home interviews with Medicare enrollees (n = 2; Gerber et al., 2010; Wolf et al., 2010).
Study sample size ranged from 33 to 3,000 participants. Half of the studies had a sample size of 62 or fewer participants (Bickmore et al., 2010; Ganzer et al., 2012; McDougall et al., 2012; Patel et al., 2011). Three studies had a sample size between 160 and 450 participants (Cordasco et al., 2012; Gerber et al., 2010; Mosher et al., 2012), and one study had sample size of 3,000 participants (Wolf et al., 2010). Seven of the eight studies (88%) were cross-sectional, while one was a two-arm intervention (Bickmore et al., 2010). All study populations included adults aged 65 years or older. Specific populations included Veteran Affairs (VA) patients (Mosher et al., 2012), older adults who’s primary language was Spanish (Cordasco et al., 2012), Medicare enrollees (Gerber et al., 2010; Wolf et al., 2010), community dwelling urbanites (Bickmore et al., 2010; Ganzer et al., 2012; McDougall et al., 2012), and African Americans (Cho et al., 2010; Gerber et al., 2010; Patel et al., 2011).
With respect to health literacy research, the most common assessment tools used to measure health literacy include the following: The Wide Range Achievement Test–Revised (WRAT-R), Rapid Estimate of Adult Literacy in Medicine (REALM; Davis et al., 1993), the Test of Functional Health Literacy in Adults (TOFHLA; Parker, Baker, Williams, & Nurss, 1995), and the Newest Vital Sign (NVS; Weiss et al., 2005). Table 3 provides a comprehensive description of these measures. A number of these measures were represented in literature currently reviewed. The S-TOFHLA was the measure of choice in half of the studies (Ganzer et al., 2012; Gerber et al., 2010; Patel et al., 2011; Wolf et al., 2010), while an additional study used the Spanish version of the S-TOFHLA (Cordasco et al., 2012). Three studies (38%) used the REALM (Cordasco et al., 2012; McDougall et al., 2012; Mosher et al., 2012). One study used the NVS (Patel et al., 2011), one used the three-item Single Item Literacy Screening (SILS; Cordasco et al., 2012), and one used the TOFHLA (Bickmore et al., 2010). Health literacy was evaluated with respect to demographics (age, education, race, and income), self-rated and functional health, medication adherence, mortality, memory and cognitive health, and computer literacy.
Table 3.
Health Literacy Assessment Tools.
| REALM | TOFHLA S-TOFHLA |
(SILS) | SAHLSA | NVS | METER | FHLTs | HLSI | Health LiTT | |
|---|---|---|---|---|---|---|---|---|---|
| Constructs measured | Word recognition and pronunciation of medical terms | Reading comprehension and numeracy skills | Reading and verbal comprehension, need for assistance, and confidence | Word recognition of medical terms | Reading and comprehension of a nutrition label | Word recognition of medical terms | Reading comprehension | Prose, document, quantitative, oral, and Internet-based information seeking skills | Prose, document, quantitative |
| Year Published | 1991/1993 | 1995/1999 | 2004/2006/2008/2009 | 2006/2010 | 2007 | 2009 | 2009 | 2010/2012 | 2011 |
| Administration time (min) | 3-7 long 1 short |
22 long 7 short |
1-2 | 3-6 long 2-3 short |
3-4 | 2-3 | Median 3 | >10 long 5-10 short |
18 |
| Number of items | 7/66 items | 17/50 items or 4/36 items | 4 items | 50 items or 18 items | 6 items | 70 items | 21 items | 25 items or 10 items | 30 items |
| Performance-based | X | X | X | X | X | X | X | X | |
| Self-administration | X | X | X | X | |||||
| Available in Spanish | X | Not validated | X | X | X | ||||
| Phone, mail, computer administration | X | X | X | With touch screen | |||||
| Communication (pronunciation, verbalization) | X | X | X | ||||||
| Comprehension | X | X | X | X | X | X | |||
| Quantitative | X | X | X | X | |||||
| Health information seeking | X | ||||||||
| Function | X | X | X | X | X | ||||
| Decision making/critical thinking | X | X | X | X | |||||
| Self-efficacy | X | ||||||||
| Need for assistance | X | ||||||||
| Navigation | X |
Note. REALM = Rapid Estimate of Adult Literacy in Medicine; TOFHLA = Test of Functional Health Literacy in Adults; S-TOFHLA = Short Test of Functional Health Literacy in Adults; SILS = Single Item Literacy Screening; NVS = Newest Vital Sign; SILS = Single Item Literacy Screener; SAHLSA = Short Assessment of Health Literacy for Spanish-speaking Adults; METER = Medical Term Recognition Test; FHLT = Functional Health Literacy Test; HLSI = Health Literacy Skills Instrument; Health LiTT = Health Literacy Assessment Using Talking Touchscreen Technology.
Health Literacy in Older Adults—Key Findings
Demographics
The most common demographic variables assessed in the reviewed articles include education, race, income, and age. The relationship between these measures and health literacy was mixed. Health literacy was not related to education as measured by McDougall et al. (2012). However, Wolf et al. (2010), Ganzer et al. (2012), and Cordasco (2012) all report a relationship between health literacy and education. Moreover, Cordasco et al. conclude that a single question assessing education is as effective as the best performing SILS question. Mosher et al. (2012) find health literacy and education interacted with their adverse drug event among low literacy participants, but the multivariable analysis findings were not significant. Patel et al. (2011) report that participant education level and age were better predictors than the NVS score for assessing health literacy in one population. Gerber et al. (2010) and Bickmore et al. (2010) did not address education. In the only study to address gender differences, Patel (2011) reports no difference between men and women when comparing the NVS and S-TOFHLA. With respect to race, Gerber and colleagues (2010) report African Americans had a lower level of health literacy compared with Caucasian participants (all, p < .001). Although African American participants had significantly lower health literacy, depression scores, and social support than did Whites, race remained an important factor in a multivariate model (Gerber et al., 2010). Wolf et al. (2010) report that individuals with lower health literacy were older, more likely to be non-White, and have a lower household income. Patel et al. (2011) study an African American population, while Cordasco (2011) focuses on monolingual Spanish speakers, 87% of Bickmore’s participants were African American and 20% were Hispanic; however, these authors did not consider race in their analysis. With respect to age, Wolf et al. (2010) report that their lower literate participants were more likely to be older, and this relationship was notably linear and graded. As reported above, Patel et al. (2011) find education level and age to be better predictors than the NVS score for assessing health literacy. Ganzer et al. (2012) report a relationship between age and working memory, but not between age and health literacy. McDougall et al. (2012) report no relationship between age and health literacy. Although the general literature reports a relationship between income level and health literacy, only three authors specifically investigating older adults collected this information. Wolf et al. (2010) report that individuals with lower health literacy were also more likely to have a lower income. In Gerber et al.’s (2010) multivariate analysis of forgetting to take medications, income was significant. As with similar demographic results, Ganzer et al. (2012) report a relationship between income and working memory, but not with health literacy.
Health outcomes
It seems reasonable that health literacy would be important when considering an older individuals’ health. The lack of health-related knowledge and/or skills may serve as a barrier to the engagement in healthy behaviors, preventative services, and acute as well as chronic disease management. Two studies evaluated health-related outcomes: One examined self-reported physical health while the other evaluated instrumental activities of daily living. Wolf et al. (2010), while controlling for demographic and socioeconomic factors, health behaviors, and number of chronic conditions, reported a causal association between lower health literacy levels and self-reported physical functioning, including a graded relationship between literacy scores and baseline physical functioning (Wolf et al., 2010). The authors suggest that insufficient health literacy resulting in a decrease in cognitive skills and reading fluency “may lead to progressively lower understanding of how to stay healthy, when to seek medical attention, and how to properly follow medical regimens to recover from acute and care for chronic health conditions.” They further propose that over an extended period, these insufficiencies could compound and result in a continual decline in baseline physical functioning. In addition, a multivariate analysis controlling for demographics, socioeconomic status, and baseline health (number of chronic conditions, physical functioning, activity limitations, mental health) indicated that the all-cause mortality rate was greater for those with lowest health literacy levels (Wolf et al., 2010). McDougall et al. (2012) investigate the relationship between health literacy, memory performance, and instrumental activities of daily living. Similar to Wolf et al.’s (2010) findings, health literacy exhibit the strongest relationship with participants’ instrumental activities of daily living (0.50) and was also related to cognitive impairment (0.30), memory (0.25), and age (−0.15).
Medication adherence
Medication management is an important factor in an older adult’s overall health condition. Poor medication adherence is associated with increases in morbidity, mortality, and health care costs (Gazmararian et al., 2006; Keller, Wright, & Pace, 2008). Two recent studies investigated the impact of health literacy on medication management. Mosher et al. (2012) assess the relationship between health literacy and medication knowledge, adherence, and adverse drug events. Lower health literacy was associated with less knowledge of medication names and purposes. Patients with low health literacy knew the fewest (32.2%) medications by name, as compared with 54.6% and 60.8% for participants with marginal and adequate health literacy, respectively (p < .001). Similarly, the lower literacy group knew the purpose of 61.8% of their medications, compared with 77.4% and 81.4% in the marginal and adequate literacy groups, respectively (p < .001). Health literacy was not associated with self-reported medication adherence or adverse drug events (Mosher et al., 2012).
Cognitive health
The impact of cognitive health on an individual’s health literacy should not be overlooked. This variable is especially important in an older adult population where age-related cognitive decline is the norm (Spirduso, Francis, & MacRae, 2005). Health literate individuals most certainly rely on cognitive functions to recall and process health information. Three studies addressed this topic. Wolf et al. (2010) compare health literacy with self-rated physical function, mental health status measured by the SF-36, and mortality rates. He reports a causal relationship between health literacy and cognitive health. Wolf et al.’s (2010) results suggest the relationship between health literacy and mental health is a threshold relationship not continuous or linear (Wolf et al., 2010). Lower levels of mental health were associated with lower health literacy scores, but the relationship was not continuous in nature. Participants in the two lower literacy categories exhibited poorer mental health compared with those in highest health literacy category. McDougall et al. (2012) investigate the relationship between health literacy, memory performance, cognition, and performance-based functional ability. Health literacy scores were high in this sample, with 76% of the sample scoring a perfect 66/66 on the REALM. Health literacy was associated with memory performance and performance-based functional ability, but was not associated with education or age. Education and cognition were significantly related to health literacy. Similar to McDougall (2012), more than 50% of Ganzer et al.’s (2012) sample exhibited high health literacy (a median score of 33/36 on the S-TOFHLA). Ganzer et al. were interested in the relationship between working memory, health literacy, and the recall of five signs of stroke. Approximately 1 hr after reading about the signs of stroke, participants recalled 2.9 ± 1.33 of the five signs of stroke. Stroke sign recall was associated with working memory, health literacy, education, and dementia. Working memory was subsequently associated with education, income that meets expenses, health literacy, and age. Health literacy was related to education. Using regression, health literacy was the best predictor of stroke recall (β = .56, p < .01).
Interventions
Bickmore et al. (2010) address health literacy and its connection to health information technology. In an effort to reduce disparities between insufficient and sufficient health literate older adults with respect to computer/health information technology access, the authors developed a computer interface to mimic face-to-face communication (Embodied Conversational Agents), face-to face being one of the best methods to communicate health information. Within their study, the authors evaluated health literacy and computer use. Results indicate that participants with inadequate health literacy reported poorer levels of self-reported computer literacy compared with participants with adequate health literacy. With respect to use of the Embodied Conversational Agent, participants with inadequate health literacy completed fewer home-based conversations compared with participants with adequate health literacy. Beyond this measure, there were few differences in measures of acceptance and usability between patients with adequate and inadequate health literacy. The authors suggest that these Embodied Conversational Agents were approachable and usable by patients regardless of health literacy level (Bickmore et al., 2010).
New measures
Two authors evaluated the use of newly developed health literacy measures. Patel et al. (2011) compare a new health literacy measure, NVS, with the S-TOFHLA in an older adult African American sample. The NVS has been evaluated in a younger population and was shown to be quickly administered, taking younger participants only 2.9 min to complete. Gender comparisons revealed no differences for both the NVS and S-TOFHLA. With respect to health literacy, 50% of participants were deemed sufficiently literate using S-TOFHLA in comparison with 42% using NVS. Patient’s educational level and age were better predictors than the NVS score for assessing health literacy in this population. Mean time to complete NVS was 11.7 min rendering impractical as a quick assessment of health literacy. Cordasco et al. (2012) evaluate the accuracy of SILS in detecting inadequate health literacy in monolingual Spanish speakers. The comparison measure, the S-TOFHLA, identified inadequate health literacy in 84% of the sample. The best performing SILS question was “How confident are you filling out medical forms by yourself?” Using stringent cutoffs for this question, the sensitivity was high, meaning the use of this single question to identify inadequate health literacy would miss fewer than 1 out of 10 participants. Conversely, the use of this question has low specificity, meaning 7 out of 10 participants with inadequate health literacy would be misclassified. Using this single SILS question yielded no better results than using a simple measure of educational attainment to identify a participant at risk for inadequate health literacy. The authors conclude that the single SILS question is useful as a screening tool, being aware of the specificity limitations. Conversely, one could achieve similar results screening by assessing educational achievement.
Discussion
Efforts to fully understand the variables that influence health literacy are hampered by investigators use of diverse health literacy measures. The authors reviewed each tool validation study to assess if the authors were testing a health literacy measure in the older adult population. However, no study we reviewed in the primary search reported the validation of health literacy tools for use in an older adult population. These critical missteps likely resulted in many of the mixed findings. The validation and standardization of tools has important clinical implications as the call for an integrated health literacy screening tool in primary care settings increases (Hart, Chesser, Wipperman, Wilson, & Kellerman, 2011).
The five demographic variables evaluated in the articles selected for review were education, race, gender, age, and income. The relationship of health literacy to these measures was mixed, and unfortunately not all studies evaluated the impact of these measures. The most consistently collected demographic variable was education. Data were collected in six of the eight studies, and an association between health literacy and education was noted in five of six. The results of Cordasco (2013) and Patel et al. (2011), where education was the strongest predictor of low health literacy, clearly demonstrate the significance and importance of education in shaping an individual’s health literacy. Age was examined in four of the eight studies; results were split. Wolf et al. (2010) and Patel et al. (2011) find age to be an important contributor to their participant’s health literacy; conversely, Ganzer et al. (2012) and McDougall et al. (2012) did not. The discrepancy between these studies, as well as with the larger body of health literacy research, could be in part due to age differences as well as the restricted age range in these studies. The mean ages of Wolf and Patel were approximately 73 years with standard deviations between 6.0 and 8 years, respectively. Ganzer’s (80.4 ± 7.95 years) and McDougall’s (77.11 years) samples were older. Furthermore, when considering the importance of age in the broader health literacy research, these studies were restricted to adults aged 65+ years; whereas the general health literacy research includes adults of all ages. Discrepancies may also be due in part to the large difference in sample sizes of the reviewed studies. The Gerber et al. (2010) and Wolf et al. (2010) studies both had large sample sizes while the others eight studies were quite small in comparison. The smaller studies may have been underpowered and subsequently provide a reminder to future researchers of the need for stronger evidence. Race was considered in two of the eight studies, and in both studies, race was a determining factor in low health literacy. The role of income on an individual’s health literacy was examined in three studies; two reported a relationship. Earlier studies have reported mixed findings with some indicating an association between participant’s gender and literacy (von Wagner, Knight, Steptoe, & Wardle, 2007) and others not finding an association (Paasche-Orlow, Parker, Gazmararian, Nielsen-Bohlman, & Rudd, 2005). Only one article reports that gender of participants did not play a role in their participants’ health literacy (Patel et al., 2012).
Adults with poor health literacy are more likely to report their health as poor (42%) and are more likely to lack health insurance (28%) than adults are with proficient health literacy (Berkman et al., 2011). These individuals are also less likely to obtain important preventive health activities such as mammograms, pap smears, and flu shots. They also make greater use of services designed to treat the complications of disease and use fewer services designed to prevent complications. These same individuals also tend to enter the health care system when they are sicker, consequently increasing the length of treatment and reducing positive health outcomes (Berkman et al., 2011). The two studies included in this review that evaluated health outcomes both support the assertion that health literacy affects health: Wolf et al. (2010) through measures of physical function and McDougall et al. (2012) through measures of instrumental activities of daily living. Wolf et al. (2010) were interested in determining whether the relationship between health literacy and health outcomes is continuous and graded, or threshold in nature. Results suggest a causal association between lower health literacy levels and self-reported physical functioning, including a continuous, graded relationship between literacy scores and baseline physical functioning (Wolf et al., 2010). The authors suggest that a decrease in cognitive skills and reading fluency negatively affect health literacy and “may lead to progressively lower understanding of how to stay healthy, when to seek medical attention, and how to properly follow medical regimens to recover from acute and care for chronic health conditions.” They further propose that over an extended period, these insufficiencies could compound and result in a continual decline in baseline physical functioning. It is increasingly apparent that health literacy researchers need to investigate if it is possible to improve older adult’s health literacy. If possible, it may then also be possible that empowered older adults could engage in healthy behaviors, embrace preventative services, and better manage their acute and as chronic diseases.
Similar to the health barriers experienced by low literate older adults, the literature suggests that these same individuals are less likely to properly take medications, adhere to the directions, and often do not correctly interpret medication labels or standard health messages (Berkman et al., 2011). The currently reviewed older adult health literacy research did not present strong support for these assertions. Moser’s 2012 article reports that older adults with lower health literacy knew fewer medication names and their purpose. However, health literacy was not associated with medication adherence or adverse drug effects. Moreover, Gerber et al., (2011) research suggests health literacy was not a factor in his participants following medication instructions in their sample. These inconsistent results highlight the complex and persistently undefined role of health literacy in medication adherence and patient safety.
Health literacy is associated with cognitive function across multiple domains in older adults. Unfortunately, older adults may face additional memory and cognitive challenges that can further limit their health literacy. It is commonly accepted that both working memory (Salthouse, 2010) and health literacy decline (Baker, Gazmararian, Sudano, & Patterson, 2000) with advancing age. The results of Wolf et al. (2010), McDougall (2011), and Ganzer et al. (2012) all confirm the relationship between cognition and health literacy in older adults. The purpose of a study by Ganzer et al. (2012) was to investigate working memory and health literacy, factors that have the potential to influence the recall of the signs of stroke in older adults. The successful recall of the signs of stroke could initiate prompt action to seek care and prevent the deleterious effects of stroke. The results of the study demonstrated that working memory and health literacy were significantly associated with recall of the signs of stroke. In fact, multiple regression analysis denoted health literacy as the best predictor of stroke recall. Wolf et al. (2010) report a threshold at which cognition affects health literacy and hypothesizes that a lifetime of continual cognitive decline may lead to inadequate health literacy. Declining cognitive function may lead to increasing difficulty in the ability to make appropriate health choices, determine when to seek out medical care, and how to properly follow medical treatments.
Cordasco (2011) and Bickmore et al. (2010) offer two important findings that could affect clinical and perhaps community-based settings: the use of a single item health literacy screener and the use of an embodied conversational agent as an approachable and usable vehicle to present health care information by all consumers regardless of health literacy levels (Bickmore et al., 2010; Cordasco et al., 2012). These findings could be implemented across settings (e.g., community, medical, and social service settings) to improve both identification of older adults with low health literacy levels as well the delivery of health information.
Finally, the use of specific health literacy measures for different populations is still under debate (Powers, Trinh, & Bosworth, 2010). The REALM and S-TOFHLA are the two most frequently used measures of health literacy (Chin et al., 2011). Previous research has examined processing capacity and knowledge related to health literacy measures among older adults to better understand the relationship between knowledge, mental capacity, and health literacy scores (Chin et al., 2011). In addition, the use of health literacy measures have not been successfully validated among the older adult population suggesting the use of some tools to be inappropriate due to age-related reasons (Saldana, 2012).
Limitations
The findings of this systematic review are not without limitations. As with all systematic reviews, there is a possibility for research bias. To minimize potential biases, scientific methodology was used and reported to identify studies and synthesize findings (Moher et al., 2009). Although some work has advanced the field, additional research is warranted. With more than 70,000 peer-reviewed studies investigating health literacy (we located 76,806 academic publications through a broad search) from 2010 to 2014, few studies isolated the older adult population. Limited data are available from state, regional, national, or international representation samples. A standardized definition was used for the systematic review; however, it is not uncommon for other age definitions to be used when defining older adults (e.g., 55 and older, or 60 and older; Federman et al., 2013; Federman et al., 2014; Hinrichsen & Molinari, 1998). The lack of clinical heterogeneity (similar participant characteristics) and the lack of statistical heterogeneity (findings across studies) limit the generalizability of findings (Crowther & Cook, 2007).
Conclusion
The findings of this review highlight the few number of studies specifically examining health literacy in older adults and the importance of working to improve the health literacy of older adults. In the older adult population, education clearly affects health literacy. The impact of age and income was significantly related to health literacy in the studies with a large sample size. Although only examined by two investigators, race was an important factor in both studies. Gender, while only examined in one study, was not related to literacy levels in older adults. It appears that individuals with low health literacy often experience poor physical and/or cognitive health. However, the role of health literacy in medication management needs further clarification. It appears health literacy screening in clinical care settings would be a beneficial tool in the care of older adults. The advantages of improving health literacy include improved health care decisions, communication, compliance to treatment directions, and improved health status, all of which should result in cost savings to the health care system and improved patient–provider satisfaction.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Amalraj S., Starkweather C., Nguyen C., Naeim A. (2009). Health literacy, communication, and treatment decision-making in older cancer patients. Oncology, 23, 369-375. [PubMed] [Google Scholar]
- Baker D. W., Gazmararian J. A., Sudano J., Patterson M. (2000). The association between age and health literacy among elderly persons. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 55, S368-S374. [DOI] [PubMed] [Google Scholar]
- Baker D. W., Gazmararian J. A., Williams M. V., Scott T., Parker R. M., Green D., . . . Peel J. (2002). Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health, 92, 1278-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D. W., Wolf M. S., Feinglass J., Thompson J. A., Gazmararian J. A., Huang J. (2007). Health literacy and mortality among elderly persons. Archives of Internal Medicine, 167, 1503-1509. doi: 10.1001/archinte.167.14.1503 [DOI] [PubMed] [Google Scholar]
- Berkman N. D., Sheridan S. L., Donahue K. E., Halpern D. J., Crotty K. (2011). Low Health Literacy and Health Outcomes: An Updated Systematic Review. Annals of Internal Medicine, 155(2), 97-U89. doi: Doi 10.1059/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Berkman N. D., Sheridan S. L., Donahue K. E., Halpern D. J., Crotty K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155, 97-107. doi: 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Bickmore T. W., Pfeifer L. M., Byron D., Forsythe S., Henault L. E., Jack B. W., . . . Paasche-Orlow M. K. (2010). Usability of conversational agents by patients with inadequate health literacy: Evidence from two clinical trials. Journal of Health Communication, 15(Suppl. 2), 197-210. doi: 10.1080/10810730.2010.499991 [DOI] [PubMed] [Google Scholar]
- Chin J., Morrow D. G., Stine-Morrow E. A., Conner-Garcia T., Graumlich J. F., Murray M. D. (2011). The process-knowledge model of health literacy: Evidence from a componential analysis of two commonly used measures. Journal of Health Communication, 16(Suppl. 3), 222-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho A. H., Arar N. H., Edelman D. E., Hartwell P. H., Oddone E. Z., Yancy W. S. (2010). Do diabetic veterans use the Internet? Self-reported usage, skills, and Interest in using my HealtheVet web portal. Telemedicine Journal and E-Health, 16, 595-602. doi: 10.1089/tmj.2009.0164 [DOI] [PubMed] [Google Scholar]
- Cordasco K. M., Homeier D. C., Franco I., Wang P. C., Sarkisian C. A. (2012). Health literacy screening of geriatric monolingual Spanish-speaking patients using single-item literacy screening questions and education. Health Education Journal, 71, 597-605. doi: 10.1177/0017896911411764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornett S. (2006). The effects of aging on health literacy. Retrieved from http://medicine.osu.edu/sitetool/sites/pdfs/ahecpublic/HL_Module_Elderly.pdf
- Craik F. I., Byrd M. (1982). Aging and cognitive deficits: The role of attentional resources. In Craik F. I., Trehub S. (Eds.), Aging and cognitive processes (pp. 191-211). New York, NY: Plenum Press. [Google Scholar]
- Crowther M. A., Cook D. J. (2007). Trials and tribulations of systematic reviews and meta-analyses. ASH Education Program Book, 2007(1), 493-497. [DOI] [PubMed] [Google Scholar]
- Cutilli C. C. (2007). Health literacy in geriatric patients: An integrative review of the literature. Orthopaedic Nursing, 26, 43-48. [DOI] [PubMed] [Google Scholar]
- Davis T. C., Long S. W., Jackson R. H., Mayeaux E. J., George R. B., Murphy P. W., Crouch M. A. (1993). Rapid estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine, 25, 391-395. [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. (2008). Older Americans 2008: Key indicators of well-being. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Federman A. D., Wolf M., Sofianou A., Wilson E. A., Martynenko M., Halm E. A., . . . Wisnivesky J. P. (2013). The association of health literacy with illness and medication beliefs among older adults with asthma. Patient Education and Counseling, 92, 273-278. doi: 10.1016/j.pec.2013.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federman A. D., Wolf M. S., Sofianou A., O’Conor R., Martynenko M., Halm E. A., . . . Wisnivesky J. P. (2014). Asthma outcomes are poor among older adults with low health literacy. Journal of Asthma, 51, 162-167. doi: 10.3109/02770903.2013.852202 [DOI] [PubMed] [Google Scholar]
- Fink D., Kiv A., Fuks D., Saad A., Vacik J., Hnatowicz V., Chandra A. (2010). Conducting swift heavy ion track networks. Radiation Effects and Defects in Solids, 165, 227-244. doi: 10.1080/10420150903491359 [DOI] [Google Scholar]
- Ganzer C. A., Insel K. C., Ritter L. S. (2012). Associations between working memory, health literacy, and recall of the signs of stroke among older adults. Journal of Neuroscience Nursing, 44, 236-243. [DOI] [PubMed] [Google Scholar]
- Gazmararian J. A., Kripalani S., Miller M. J., Echt K. V., Ren J., Rask K. (2006). Factors associated with medication refill adherence in cardiovascular-related diseases: A focus on health literacy. Journal of General Internal Medicine, 21, 1215-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber B. S., Cho Y. I., Arozullah A. M., Lee S. Y. D. (2011). Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. American Journal of Geriatric Pharmacotherapy, 8, 136-145. doi: 10.1016/j.amjopharm.2010.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart T. A., Chesser A., Wipperman J., Wilson R., Kellerman R. D. (2011). Health literacy assessment via STOFHLA: Paper vs computer administration. Kansas Journal of Medicine, 4, 55-61. [Google Scholar]
- Hinrichsen M. A. L., Molinari V. A. (1998). What practitioners should know about working with older adults. Professional Psychology: Research and Practice, 29, 413-427. [Google Scholar]
- Keller D. L., Wright J., Pace H. A. (2008). Impact of health literacy on health outcomes in ambulatory care patients: A systematic review. The Annals of Pharmacotherapy, 42, 1272-1281. [DOI] [PubMed] [Google Scholar]
- Kintsch W. (1998). Comprehension: A paradigm for cognition. New York, NY: Cambridge University Press. [Google Scholar]
- Kutner M., Greenburg E., Jin Y., Paulsen C. (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). Washington, DC: National Center for Education Statistics, United States Department of Education. [Google Scholar]
- McDougall G. J., Jr., Mackert M., Becker H. (2012). Memory performance, health literacy, and instrumental activities of daily living of community residing older adults. Nursing Research, 61, 70-75. doi: 10.1097/NNR.0b013e31823b18f4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., Grp P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62, 1006-1012. doi: 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Mosher H. J., Lund B. C., Kripalani S., Kaboli P. J. (2012). Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. Journal of Health Communication, 17(Suppl. 3), 241-251. doi: 10.1080/10810730.2012.712611 [DOI] [PubMed] [Google Scholar]
- Oldfield S. R., Dreher H. M. (2010). The concept of health literacy within the older adult population. Holistic Nursing Practice, 24, 204-212. doi: 10.1097/HNP.0b013e3181e90253 [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow M. K., Parker R. M., Gazmararian J. A., Nielsen-Bohlman L. T., Rudd R. R. (2005). The prevalence of limited health literacy. Journal of General Internal Medicine, 20, 175-184. doi: 10.1111/j.1525-1497.2005.40245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R. M., Baker D. W., Williams M. V., Nurss J. R. (1995). The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine, 10, 537-541. [DOI] [PubMed] [Google Scholar]
- Patel P. J., Joel S., Rovena G., Pedireddy S., Saad S., Rachmale R., . . . Cardozo L. (2011). Testing the utility of the newest vital sign (NVS) health literacy assessment tool in older African-American patients. Patient Education and Counseling, 85, 505-507. doi: 10.1016/j.pec.2011.03.014 [DOI] [PubMed] [Google Scholar]
- Powers B. J., Trinh J. V., Bosworth H. B. (2010). Can this patient read and understand written health information? The Journal of the American Medical Association, 304, 76-84. [DOI] [PubMed] [Google Scholar]
- Ratzan S. C., Parker R. M. (2000). Introduction. In Selden C. R., Zorn M., Ratzan S. C., Parker R. M. (Eds.), National library of medicine current bibliographies in medicine: Health literacy (NLM Pub. No. CBM 2000-1). Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services. [Google Scholar]
- Saldana S. (2012). Performance of health literacy tests among older adults with diabetes. Journal of General Internal Medicine, 27, 534-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse T. A. (2010). Influence of age on practice effects in longitudinal neurocognitive change. Neuropsychology, 24, 563-572. doi: 10.1037/a0019026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott T. L., Gazmararian J. A., Williams M. V., Baker D. W. (2002). Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Medical Care, 40, 395-404. [DOI] [PubMed] [Google Scholar]
- Speros C. (2009). More than words: Promoting health literacy in older adults. OJIN: The Online Journal of Issues in Nursing, 14(3). Retrieved from http://www.medscape.com/viewarticle/717469 [Google Scholar]
- Spirduso W. W., Francis K. L., MacRae P. G. (2005). Physical dimensions of aging (2nd ed.). Champaign, IL: Human Kinetics. [Google Scholar]
- von Wagner C., Knight K., Steptoe A., Wardle J. (2007). Functional health literacy and health-promoting behaviour in a national sample of British adults. Journal of Epidemiology & Community Health, 61, 1086-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B. D., Mays M. Z., Martz W., Castro K. M., DeWalt D. A., Pignone M. P., Hale F. A. (2005). Quick assessment of literacy in primary care: The newest vital sign. The Annals of Family Medicine, 3, 514-522. doi: 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss B. D., Palmer R. (2004). Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. The Journal of the American Board of Family Practice, 17, 44-47. [DOI] [PubMed] [Google Scholar]
- Wolf M. S., Feinglass J., Thompson J., Baker D. W. (2010). In search of “low health literacy”: Threshold vs. gradient effect of literacy on health status and mortality. Social Science & Medicine, 70, 1335-1341. doi: 10.1016/j.socscimed.2009.12.013 [DOI] [PubMed] [Google Scholar]