Abstract
Background
Past research has shown discrepancies between the time of symptom onset for patients with acute coronary syndrome (ACS) as documented in the medical record (MR) and patients’ recall of the time assessed through subject interviews done later by researchers.
Purpose
To determine if there were differences between the time of symptom onset documented in the MR and subject interview taking into consideration gender, age group, and recall period for patients admitted to the emergency department (ED) for symptoms suggestive of ACS.
Methods
A secondary analysis was conducted on data from the PROMOTION (Patient Response tO Myocardial Infarction fOllowing a Teaching Intervention Offered by Nurses) trial, a multi-center randomized clinical trial to reduce patient prehospital delay to treatment in ACS.
Results
Of the 3,522 subjects with CAD enrolled into the trial, 3,087 subjects completed 2-year follow-up. Of these, 331 subjects sought treatment in the ED for ACS symptoms and 276 patients (83%) had complete information on the time of symptom onset from both sources. Of the 276 patients, 25 (9%) had differing times > 48 hours, thus were excluded. The median difference between the two sources was 45.0 minutes. When both times were examined, there were no significant differences in time by gender (p = 0.720) or by age group (p = 0.188). The median number of days between the date of symptom onset and the interview was 29.5 days. There was a significant correlation between differences in the time of symptom onset and the length of recall period (rs = 0.148, p = 0.023). In multivariable modeling, a longer recall period was associated with greater median differences in the symptom onset time (b = 13.2, p = 0.023).
Conclusion
These results suggest that the time of symptom onset obtained at the time of the index event and documented in the MR is not interchangeable with data obtained later by research staff, especially if the interview is not conducted near the time of the index event.
Keywords: symptom onset, medical record, interview, congruence, acute coronary syndrome
Introduction
The time of symptom onset for patients with acute coronary syndrome (ACS) is frequently used to calculate total ischemic time, defined as the time of symptom onset to the time of the first coronary artery balloon inflation.1 Total ischemic time could be influenced by patient-related delays, such as when patients fail to recognize and act upon symptoms of ACS, or hospital-related delays, such as when clinicians fail to diagnose patients in a timely manner once they enter the health care system. Either type of delay influences whether patients with ACS are eligible for acute reperfusion therapy. The longer the total ischemic time, the larger the infarction and worse the patient outcomes are. For example, total ischemic time has been shown to correlate better with infarct size and mortality compared to the door-to-balloon time interval in patients with ACS.1
Total ischemic time has been identified as one criterion of quality care for patients with ACS. Thus, accuracy in collecting and documenting this time interval by clinicians to maximize patient outcomes and demonstrate quality care is important. The time of the first coronary balloon inflation is relatively easy to define and obtain from the medical record (MR). However, a challenge remains in how consistent hospitals across the country operationally define the time of symptom onset with patients with symptoms of ACS. In fact, the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Task Force on Clinical Data Standards advocates a consistent definition for the time of symptom onset as the time when the patient first notes ischemic symptoms lasting 10 minutes or longer.2
In addition, cardiovascular researchers who investigate pre-hospital delay in patients with ACS frequently use the time of symptom onset to calculate prehospital delay time as an outcome variable for their research. When designing their studies, researchers have to decide whether to obtain these data from the MR, to interview subjects themselves, or to combine the two sources in order to obtain more complete data. Each source has the potential for measurement error. Some researchers consider the MR to be the “gold standard” since these data are collected and documented in “real time”, and thus are less subject to recall bias. However, the MR is designed for clinical use; and data obtained from this source may be limited by legibility, completeness, and accessibility. Past studies have shown that the percentage of missing or incomplete symptom onset data in the MR for patients with acute myocardial infarction ranged from 14% to 40%.3–7 Furthermore, patients who are older and are female are more likely to have missing or incomplete time of symptom onset data in the MR.3
Other researchers prefer interviewing subjects first-hand to obtain the time of symptom onset, either in-person or by telephone after the index event. However, subject interviews done late in the course of care can be challenging. For example, subjects need to be willing, able, and available to participate. In addition, data collected by subject interviews done after the ACS event may also be lacking in completeness. For example, two studies reported the percentage of missing or incomplete data regarding the time of symptom onset from subject interviews ranged from 12–13%.6–7 Furthermore, using a combination of the two data sources is costly and resource intensive.
The question then is whether these data sources are interchangeable. Four studies conducted over a decade reported sizeable disagreements between the symptom onset time assessed during the index event as documented in the MR and the symptom onset time obtained by interview later after the event.4–7 However, two of the those studies were limited to patients with acute myocardial infarction and did not include patients with unstable angina (part of the full ACS spectrum).6–7 In addition, there have been a few changes in the past decade that warrant further investigation of this issues. For example, recently, there has been increased emphasis on assessing symptoms more broadly for atypical presentations (symptoms other than chest pain or pressure such as shortness of breath, diaphoresis, nausea, and pain or discomfort in the jaw, neck, back, arm, or upper abdomen). National initiatives from the American Heart Association such as Go Red for Women®8–9, which includes atypical symptom presentations in women, have broadened interview techniques by clinicians who assess patients in the acute setting. Also, outcomes-based quality improvement initiatives such as the American College of Cardiology/American Heart Association Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry®/Get with the Guidelines™ (GWTG)10 program now track total ischemic time in relation to patient outcomes as a measure of quality of care in patients with ACS. Individual hospital reports for these initiatives include the percentage of missing data on issues such as the time of symptom onset thereby providing hospitals an opportunity to implement corrective measures to improve data collection and documentation. Given these new developments, the study reported here was designed to determine if there were currently differences between the times of symptom onset in the MR and subject interview, taken into consideration gender, age group, and recall period based on the date of the interview with patients admitted to the emergency department (ED) for symptoms suggestive of ACS.
Methods
This secondary analysis was conducted on data from the PROMOTION (Patient Response tO Myocardial Infarction fOllowing a Teaching Intervention Offered by Nurses) trial. The PROMOTION trial,11 a randomized clinical trial, tested a face-to-face intervention designed to reduce patient delay in seeking treatment for ACS symptoms. Patients with a history of cardiac disease were enrolled, randomized to usual care or intervention and then followed for 2 years for occurrence of ACS symptoms. Patients were instructed to call the investigators (after the acute event was over) when they sought treatment for symptoms they believed were cardiac in origin. In the event that patients did not contact the investigators after an ED visit, patients were also telephoned every 6 months by investigators to discuss whether there had been any unreported ED visits for ACS. Patients who sought treatment for symptoms for presumed ACS were interviewed using techniques the investigators had developed to assist patients most closely determine the time of symptoms onset.
Sample
Of the 3,522 patients with a history of CAD were enrolled in the PROMOTION study, 3,087 (88%) completed 2-year follow-up.11 Of these, 565 had ED admissions with symptoms suggestive of ACS.12 Of the 565, 331 (59%) were diagnosed with ACS (and these were included in the current study).12 Among these 331 patients, 11 (3%) were missing time of symptom onset in the MR and 48 (15%) were missing the time of symptom onset from subject interviews; thus 55 patients (17%) were missing data from either MR or subject interview.
A total of 276 patients (83%) had complete data from both sources. Of these patients for 25 (9%), there was a difference of more than 48 hours in time of symptom onset reported in the MR and the interview. Because of this difference was so large, these patients were not included in the analysis. The remaining sample of 251 ACS patients is the focus of this report.
Data Analysis
Patient sample characteristics were assessed using descriptive statistics. Differences in time of symptom onset between the MR and interview were calculated in minutes (min) and were categorized as <30 min, 30–<60 min, 60–<90 min, and 90 min to 48 hours. Age at enrollment in the study was categorized as ≤65 years, 66–79 years, and ≥80 years. Gender and age groups’ time differences were assessed visually with boxplots and with Wilcoxon rank sum and Kruskal-Wallis nonparametric tests. Recall period for subject interviews was calculated as the number of days between the date of symptom onset and the date of subject interview. Recall period and differences in the time of symptom onset were graphically assessed using a scatterplot and LOESS smoother (LOcally WEighted Scatter-plot Smoother) and analyzed with Spearman rank correlations (rs). Multivariable median regression modeling13 was used to assess the associations of gender, age groups, and length of recall period (after log-transformation) with the time of symptom onset, adjusting for randomized group assignment and site. All analyses were performed in SAS v9.3 (SAS Institute, Cary, NC). A two-sided p < 0.05 was considered statistically significant.
Results
The mean age at enrollment of the 251 patients at enrollment was 66.8 years (SD = 11.8). About a third (35%) were female. Fifteen (6%) patients had missing dates for interviews, so their recall period could not be calculated. Of the 236 who had dates for interviews, the median number of days between the date of symptoms onset and the interview was 29.5 days (M = 83.9 days, SD = 129.4 days). Table 1 gives the characteristics of the patient sample.
Of the 251 subjects with complete data, the median difference between the two data sources for the time of symptom onset was 45.0 min (M = 303.1 min, SD = 530.3 min). See Table 2. There was no significant difference in the time of symptom onset between males and females (p = 0.72) for the two sources. The median difference between the two data sources in the time of symptom onset by age groups were 40.0 min for ≤65 years old, 40.0 min for 66–79 years old, and 132.5 min for ≥80 years old; although these did not differ statistically (p = 0.188).
Greater differences in the time of symptom onset between the MR and the interview were associated with longer recall periods (see Figure 1). Specifically, there was a significant positive correlation between differences in the time from symptom onset and recall (rs = 0.148, p = 0.023). Using multivariable median regression (see Table 3), there were no significant associations with differences between the two data sources in the time of symptom onset, except for log-transformed length of recall period (p = 0.023). Longer recall periods were significantly associated with greater differences in the time of symptom onset between the MR and interviews, adjusting for other model covariates (b = 13.2, 95% CI =[1.9, 24.6]). For example, interviews conducted 3 days after the event were associated with an 18–minute difference; interviews done 7 days afterwards were associated with a 27-minute difference. If the recall period was greater than approximately 9 days the difference between the two data sources exceeded 30 minutes.
Figure 1.
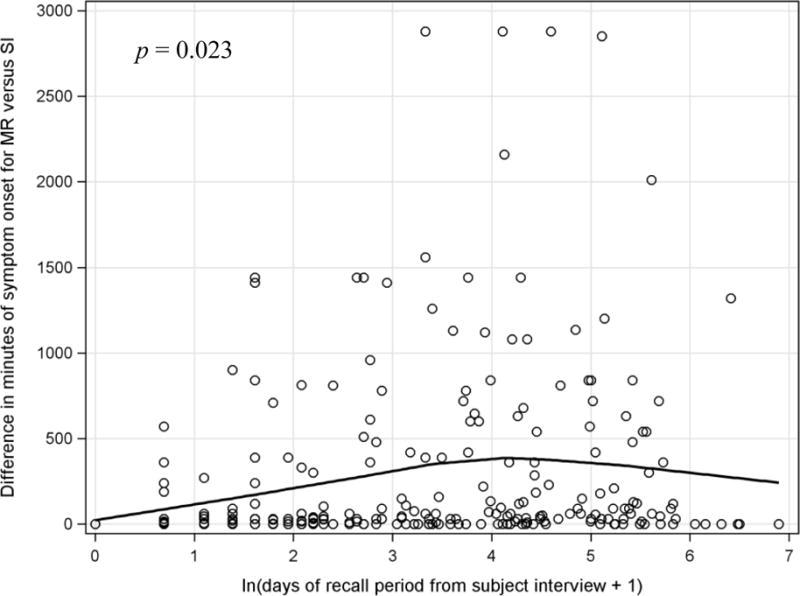
Scatterplot of time of symptom onset differences for medical record (MR) relative to subject interview (SI) versus length of recall period from subject interview for the 251 ACS patients with time of symptom onset of 48 hours or less
Discussion
We found significant discrepancies between the MR and patient interview in time of symptom onset, but with no definitive indication of which was more accurate. Notably, a longer recall period was associated with a greater difference in the two sources of information. Based on these findings, nearly half (49%) of the patients in this study had more than a 1-hour difference between the two data sources. As determined in this study, a median difference of 45 minutes between the two data sources is clinically meaningful given that past studies have shown that for every 30 minutes of prehospital delay there is a 7.5 % increase in mortality.14
We also found that in this study the percentage of missing symptom onset data was much lower in the MR as compared to subject interviews done after the index event (3% versus 15%, respectively). In addition, this percentage of missing data in the MR in this study is markedly lower than that reported in prior studies (3% in current study versus 14–40%).3–7 It is possible that the emergency department clinicians were educated in advance of the PROMOTION study about the importance of documenting the time of symptom onset. However, the percentage of missing data from subject interviews in this study was about the same as reported in past studies (15% in current study versus 12–13%).5–6 One explanation for a higher percentage of missing data from subject interviews is that the median length of time between the index event and the subject interview was about a month (29.5 days). Although the interviews were conducted by trained researchers, the length of time between the actual event and the interview probably influenced patients’ ability to remember the time of symptom onset. Thus, we recommend that data from subject interviews not be used to collect the time of symptom onset if the interviews are not conducted within 72 hours of the hospital admission.
No differences by age or gender were noted related to discrepancies between the MR and the subject interview. One explanation for a lack of significant differences between the two data sources based on gender and age is that assessment techniques may have improved in patient groups that are more likely to have atypical symptoms (women and the elderly).
Strengths and Limitations
One strength of the study was that it is a multi-center international study that reported a low percentage of missing or incomplete data from the MR as compared to past studies in the literature. However, one limitation of this study is that the time of symptom onset from both data sources was from subject report provided retrospectively after the symptoms had occurred. Thus no direct observations were done to determine the exact time of symptom onset in real time.
Implications for Clinical Practice
Clinicians in acute and critical care settings face several challenges with obtaining an accurate time of symptom onset for patients presenting with suspected ACS, and must do so within a time sensitive context. Clinicians are first charged with ensuring that symptoms of ischemia are assessed broadly, beyond chest pain as a single symptom, to avoid missing a potential ACS diagnosis. Secondly, clinicians may encounter patients that have difficulty articulating their symptom experience based on the questions asked. For example, some patients may have symptoms that evolve gradually, making it difficult for them to pinpoint the exact time of onset. Other patients may have difficulty quantifying vague or atypical symptoms. To overcome these challenges there is need for a standardized evidence-based assessment procedure for patients with suspected ACS.15, 16 Use of a standardized procedure would decrease the variability in clinical practice and provide evidence-based care for all patients with suspected ACS. For example, DeVon and colleagues have developed a 13-item ACS symptom checklist to be used for both clinical assessment and research.17 The instrument has established reliability and validity for use as a rapid triage assessment tool and is suitable for integration in an electronic health record (EHR).17
Furthermore, incorporation of a standardized assessment procedure in the EHR has other potential advantages such as improving completeness of documentation of symptoms, including the time of symptom onset. Clinicians in acute and critical care settings have an opportunity and an obligation to be champions in designing and utilizing efficient assessment data collection processes. Input by clinicians can include which data elements should be entered as structured data (e.g. quantifiable data such as systolic blood pressure or pain intensity level), discrete data in predefined categories (e.g. presence or absence of certain ACS symptoms), or as textual data (e.g. narrative data entered as free text).18 Clinicians can also provide input into clinical decision support tools, such as “Smart” computer assisted data entry options which prompt clinicians to enter discrete data or double-check data entered (e.g. the EHR can pre-calculate the time of symptom onset to hospital arrival). Options for rephrasing assessment questions could be used if a patient has difficulty answering a specific question related to symptoms. Furthermore, “real-time” flags can be provided alerting the clinician that data are missing thus providing an opportunity to increase completeness of assessment and documentation during the initial patient encounter.18
Conclusion
The findings from this study provide important information on assessing the time of cardiac symptom onset. The two data sources (MR versus subject interviews done after the acute event) are clearly not interchangeable, especially if the interviews are done more than 3 days after the index event. These findings indicate that documentation of symptom onset time in the MR has improved compared to previous studies. However clinicians in acute and critical care settings should remain vigilant about accurate assessment and documentation of cardiac symptoms, especially in those patients with less discrete symptom onset.
Supplementary Material
Acknowledgments
This project was partially supported by Grant P20MD002289 (Wallace, PI) from NIMHD/NIH. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institute for Minority Health and Health Disparities or the National Institutes of Health.
Contributor Information
Leslie L Davis, Assistant Professor of Nursing, University of North Carolina, Greensboro, School of Nursing, 308 Moore Building, PO Box 26170, Greensboro, NC, 27402-6170.
Thomas P McCoy, Univ of North Carolina, Greensboro, NC.
Barbara Riegel, Univ of Pennsylvania, Philadelphia, PA.
Sharon McKinley, Deakin University, Victoria, Australia.
Lynn V Doering, Univ of California, Los Angeles, CA.
Kathleen Dracup, Univ of California, San Francisco, CA.
Debra K Moser, Univ of Kentucky, Lexington, KY and University of Ulster, Newtownabbey, UK.
References
- 1.Denktas AE, Anderson HV, McCarthy J, Smalling RW. Total ischemic time: the correct focus of attention for optimal ST-segment elevation myocardial infarction care. J Am Coll Cardiol: Cardiovasc Intv. 2011;4:599–604. doi: 10.1016/j.jcin.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 2.Cannon C, Brindis R, Weintraub W, et al. 2013 ACCF/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards. J Am Coll Cardiol. 2013;61(9):992–1025. doi: 10.1016/j.jacc.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yarzebski J, Goldberg R, Gore J, Alpert J. Temporal trends and factors associated with extent of delay to hospital arrival in patients with acute myocardial infarction: the Worcester Heart Attack Study. Am Heart J. 1994;128(2):255–263. doi: 10.1016/0002-8703(94)90477-4. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RJ, McGovern PG, Guggina T, Savageau J, Rosamond WD, Luepker RV. Prehospital delay in patients with acute coronary heart disease: Concordance between patient interviews and medical records. Am Heart J. 1998;135:293–299. doi: 10.1016/S0002-8703(98)70096-1. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg R, Osganian S, Luepker R, et al. Prehospital delay in individuals with acute coronary disease: Concordance of medical records and follow-up phone interviews. Cardiology. 2002;97(3):159–165. doi: 10.1159/000063333. [DOI] [PubMed] [Google Scholar]
- 6.DeVon H, Ryan C, Zerwic J. Is the medical record an accurate reflection of patients’ symptoms during acute myocardial infarction? West J Nurs Res. 2004;26(5):547–560. doi: 10.1177/0193945904265452. [DOI] [PubMed] [Google Scholar]
- 7.Fukuoka Y, Dracup K, Ohno M, Kobayashi F, Hirayama H. Symptom severity as a predictor of reported differences of prehospital delay between medical records and structured interviews among patients with AMI. Eur J Cardiovasc Nurs. 2005;4(2):171–176. doi: 10.1016/j.ejcnurse.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA, on behalf of the American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, Council on High Blood Pressure Research, and Council on Nutrition, Physical Activity and Metabolism Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263. doi: 10.1161/CIR.0b013e318287cf2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Go Red for Women® 2015 Fact Sheet. http://www.localheart.org/idc/groups/branding-public/@wcm/@cmc/documents/downloadable/ucm_468266.pdf Accessed March 29, 2016.
- 10.ACTION Registry® - GWTG™. http://cvquality.acc.org/NCDR-Home/Registries.aspx Accessed March 29, 2016.
- 11.Dracup K, Paul SM, McKinley S, Riegel B, Moser DK, Meischke H, Doering LV, Davidson P, Baker H, Pelter M. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circulation: Cardiovascular Quality and Outcomes. 2009;2(6):524–532. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelter MM, Riegel B, McKinley S, Moser DK, Doering LV, Meischke H, Davidson P, Baker H, Yang W, Dracup K. Are there symptom differences in patients with coronary artery disease presenting to the emergency department ultimately diagnosed with or without acute coronary syndrome? Am J Emerg Med. 2012;30(9):1822–8. doi: 10.1016/j.ajem.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hao L, Naiman DQ. Quantile Regression. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- 14.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 15.Canto JG, Canto EA, Goldberg RJ. Time to standardize and broaden the criteria of acute coronary syndrome presentations in women. Can J Cardiol. 2014;30(7):721–8. doi: 10.1016/j.cjca.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 16.DeVon HA, Ryan CJ, Ochs AL, Shapiro M. Symptoms across the continuum of acute coronary syndrome: Differences between men and women. Am J of Crit Care. 2008;17(1):14–25. [PMC free article] [PubMed] [Google Scholar]
- 17.DeVon HA, Rosenfeld AG, Steffen A, Daya M. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J Am Heart Assoc. 2014;3:e000586. doi: 10.1161/JAHA.113.000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells BJ, Nowacki AS, Chagin K, Kattan MW. Strategies for handling missing data in electronic health record derived data. Generating Evidence and Methods to Improve Patient Outcomes. 2013;1(3) doi: 10.13063/2327-9214.1035. article 7. Available at: http://dx.doi.org/10.13063/2327-9214.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


