Abstract
A 27-year-old pregnant woman, para 1, was transferred to our hospital at 29+3 weeks of gestation complaining of abdominal pain. She was diagnosed with hemoperitoneum based on ultrasonography. An emergency laparotomy was performed, and the bleeding was confirmed to be caused by ruptured surface blood vessels on the uterine fundus. Hemostasis with compression was successfully performed to sustain the pregnancy, and the patient delivered a full-term baby. Spontaneous hemoperitoneum during pregnancy caused by rupture of uterine blood vessels is very rare. It requires rapid diagnosis and surgical treatment because it increases the morbidity of the fetus and mother. In most incidences of spontaneous hemoperitoneum during pregnancy, a cesarean delivery is performed along with a simultaneous emergency laparotomy. However, in this case, the pregnancy was maintained to full term after surgical hemostasis, which prevented neonatal complications due to premature birth.
Keywords: Hemoperitoneum, Pregnancy, Rupture, Uterine vessel
Introduction
Spontaneous hemoperitoneum during pregnancy is very rare. In most cases, hemoperitoneum is caused by rupture of venous blood vessels. Non-obstetric causes of hemoperitoneum during pregnancy include rupture of the maternal umbilical vein, rupture of the splenic arterial aneurysm, liver rupture, and rupture of liver hemangioma or metastasis. Obstetric causes include uterine scar rupture after corneal pregnancy surgery, rupture of uterine vessels, and uterine rupture due to placenta percreta [1]. Spontaneous rupture of uterine blood vessels is very rare, and the prevalence rate is estimated to be approximately at 1 in 10,000 births. The most common locations were spontaneous rupture of uterine blood vessels occur are broad ligament (78.3%), the posterior surface of the uterus (18.3%), and the anterior uterus (3.3%) [2]. Rupture of surface uterine blood vessels is the most common form of hemoperitoneum during pregnancy, particularly during the third trimester [3]. Hemoperitoneum during pregnancy can be treated surgically. Most previously reported cases describe the use of hemostasis after a cesarean section. However, here, we report a pregnant woman with hemoperitoneum caused by spontaneous blood vessel rupture on the uterine surface who was able to deliver a full-term baby because her pregnancy was maintained by successful surgical hemostasis.
Case report
A 27-year-old pregnant woman, para 1, was transferred to the Chungbuk University Hospital Emergency Department at 29+3 weeks of gestation complaining of abdominal pain. She was taking insulin for gestational diabetes mellitus and had received tocolytics at a local obstetrics and gynecology clinic to treat preterm labor 4 days prior to the appearance of the symptom. She started experienced severe abdominal pain 4 hours after defecation.
When she arrived at the emergency department, her pulse rate was 96 beats/min and her blood pressure was normal at 130/70 mmHg. A physical examination revealed abdominal tenderness and rebound tenderness. Ultrasonography indicated that the fetus was healthy and in the breech presentation, with an estimated fetal weight of 1.6 kg and fetal heart rate of 140 to 150 beats/min. No abnormal findings were observed in the amniotic fluid index or placenta. An ultrasonography examination revealed free fluids around the liver and spleen. A blood test revealed that the hemoglobin and hematocrit levels were reduced to 7.9 g/dL and 23.4%, respectively. Based on the blood test and ultrasonography findings, the patient was diagnosed with hemoperitoneum. Therefore, a laparotomy was performed under general anesthesia.
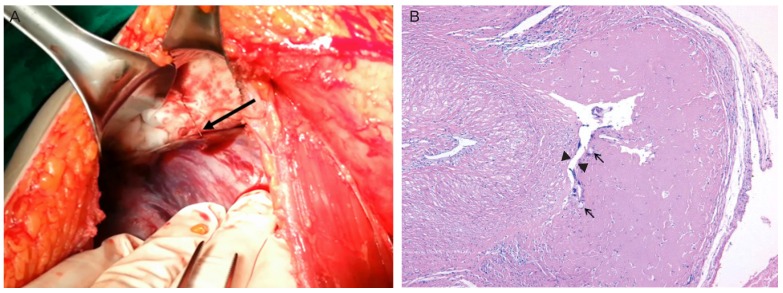
During surgery, a transverse incision was made that revealed a 2-L intraperitoneal hematoma, which was removed. Because examination of the broad ligament and the anterior portion of the uterus did not receal the bleeding source, a lower midline incision was performed, which revealed active bleeding of the surface blood vessels on the anterior uterine fundus (Fig. 1A). The lesions were sutured using Vicryl 5-0 sutures to stop bleeding. However, post-suture bleeding was observed around the suture sites due to the wide distribution of blood vessels.
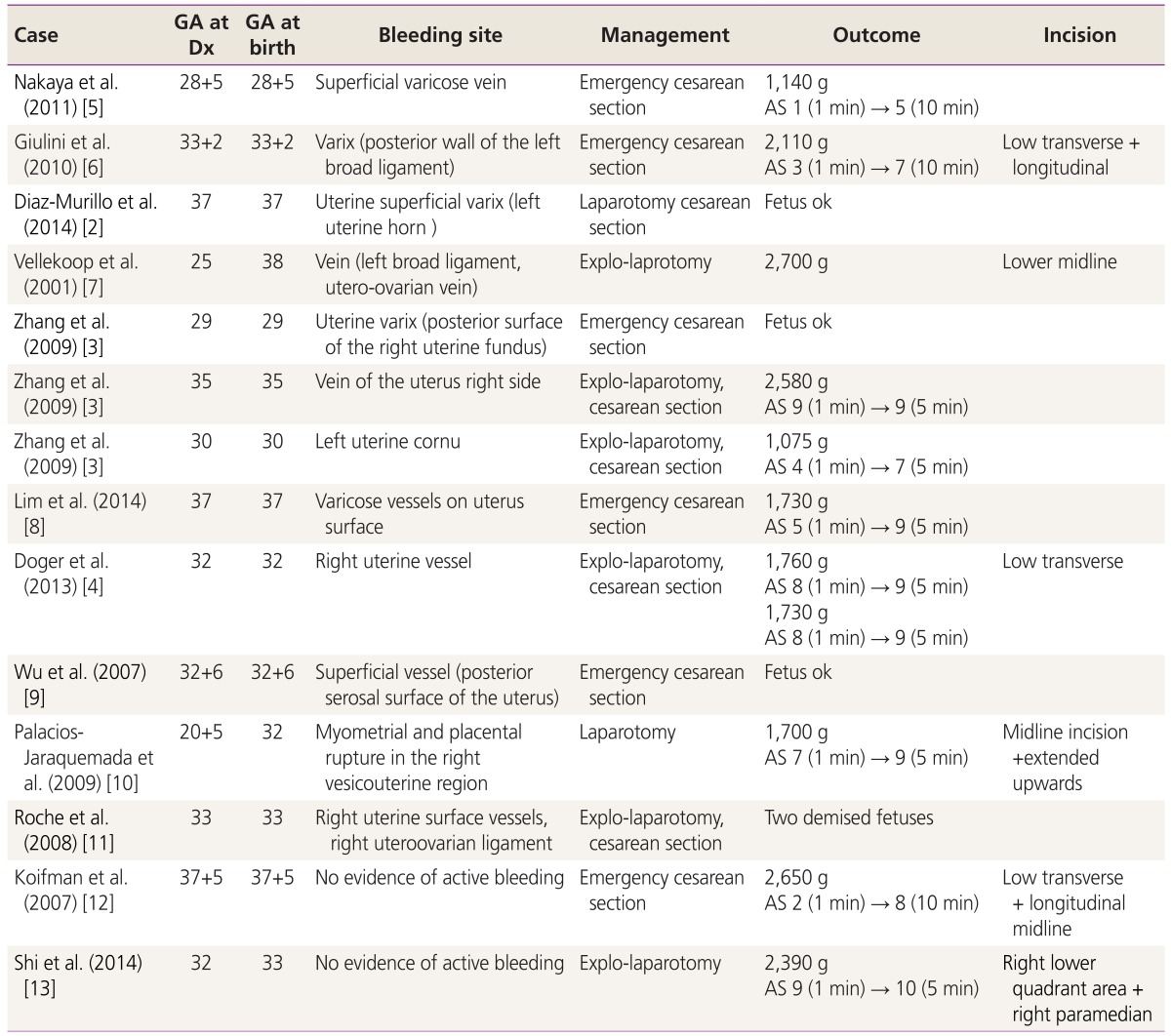
Fig. 1. (A) Active bleeding is seen from the uterine surface vessels (arrow). (B) Cross section (arrow) of the sutures between the myometrium and necrosis of the vessel wall boundary (arrow head), which could be due to the blocked blood flow.
Because suturing alone failed to stop the bleeding, a liquid hemostatic agent was used. However, the use of a liquid fibrin sealant (Tisseel, Baxter Healthcare Corporation, Westlake Village, CA, USA) also failed to stop the bleeding because the agent could not be sustained due to the high pressure of the ruptured vessels. Therefore, a fibrin sealant patch (TachoSil, Baxter Healthcare Corporation) was used, together with compression, for 5 minutes on the bleeding vessels, which finally stopped the bleeding. During surgery, 4 units of red blood cells were transfused. After the surgery, the fetus was normal, and the mother recovered without any complications such as preterm labor. Thereafter, the patient underwent routine follow up evaluations at the out-patient clinic.
The patient was hospitalized at 39+3 weeks of gestation for a planned cesarean section due to the breech presentation of the fetus. An ultrasound examination revealed an estimated fetal weight of 3,350 g, amniotic fluid index of 18 cm, and a normal placenta in the right side of the uterus. The suturing materials remained on the uterine fundus after delivery. Congestion of the blood vessels was observed around the sutures. A cesarean section was performed using a transverse incision. A healthy baby was born weighing 3,240 g, with an Apgar scores of 10 at 1 minute and 10 at 5 minutes. The placenta was not completely expulsed and was therefore, manually removed. Because severe bleeding was present at the removal site of the placenta, a hysterectomy was performed. The postoperative histopathological analysis confirmed placenta accreta. The blood vessels were widely distributed on the surface of the uterine fundus, and the closure sutures were observed around the blood vessels. However, the placental tissue was not visible (Fig. 1B).
Discussion
Hemoperitoneum caused by rupture of uterine blood vessels during pregnancy is very rare. According to a 1950 report on a study in the United States, the maternal mortality due to hemoperitoneum during pregnancy was 49%. After more than 50 years, the mortality rate has decreased to 3.6% due to medical advancements such as cardiopulmonary resuscitation, anesthesia, and surgical procedures [3].
Hemoperitoneum caused by rupture of uterine blood vessels during pregnancy is very rare. According to a 1950 report on a study in the United States, the maternal mortality due to hemoperitoneum during pregnancy was 49%. After more than 50 years, the mortality rate has decreased to 3.6% due to medical advancements such as cardiopulmonary resuscitation, anesthesia, and surgical procedures [4]. In addition, if the uterine muscle is contracted due to increased pressure in the inferior vena cava and iliac vessel resulting from the hormonale or anatomical effects of pregnancy, the blood pressure in the intra-uterine vessels might be sufficiently elevated to induce rupture [2]. In this case report, the patient felt a sudden pain after defecation, which suggests that a defecation-induced pressure increase might have caused the blood vessel rupture.
Hemoperitoneum during pregnancy requires rapid diagnosis to prevent mortality of the mother and fetus. However, chemical peritonitis due to hemoperitoneum can affect premature uterine contraction. In addition, labor pain from pushing during the second phase of delivery and can mask the other clinical manifestations of hemoperitoneum [5], which makes diagnosis difficult.
We performed a literature search in Medline and PubMed using the key words uterine vessel rupture, spontaneous, hemoperitoneum, and pregnancy, to find papers published in the past 10 years. The causes and management of spontaneous hemoperitoneum post second trimester were reviewed (Table 1) [2,3,4,5,6,7,8,9,10,11,12,13].
Table 1. Review of cases being reported.
GA, gestational age; Dx, diagnosis; AS, Apgar score.
A total of 11 cases ranging in gestational age from 28+5 weeks to 37+5 weeks were reviewed. In most cases, the mothers complained of abdominal pain without vaginal bleeding. They were diagnosed with either preterm labor or labor pain and were treated with tocolytics or labor was induced for delivery. The patients complained of worsening pain, with low blood pressure or tachycardia. Placenta abruption was suspected if the patient had unstable vital signs and fetal distress. Other uterine ruptures or hemoperitoneum due to unknown causes were treated with an emergency laparotomy. In most of the cases found in the literature, a cesarean section was performed along with a simultaneous emergency laparotomy.
In all the cases, the cause of bleeding was rupture of the uterine vessels, except in one patient who had an unknown cause of bleeding. In most of the cases prior to 34 weeks of gestation, hemostasis was performed after the baby was delivered by cesarean section. According to a case report by Vellekoop et al. [7], hemostasis was successfully performed using a clip because the bleeding originated from the left broad ligament and the utero-ovarian vein. The case report in this study involved bleeding from the uterine fundus and broadly distributed blood vessels on the uterine surface in addition to high blood pressure of the uterine blood vessels. Therefore, it was very difficult to stop the bleeding because post-suturing bleeding occurred at each suture site. However, we successfully achieved hemostasis using compression and an Food and Drug Administration-approved hemostatic agent widely used in surgical procedures. Increased vessel pressure is the most commonly identified cause of uterine blood vessel rupture during pregnancy. Therefore, the use of compression can effectively achieve hemostasis. Our results also suggest that a solid form of hemostatic agent rather than a liquid form should be used for hemostasis.
For cases of hemoperitoneum before 34 weeks of pregnancy, hemostasis is conducted following preterm delivery by cesarean section. However, when the bleeding occurs in vessels around the adnexa and on the anterior surface of the uterus, it might be necessary to perform hemostasis first. Careful exploration should be performed first to determine the source of bleeding and then hemostasis should be performed, rather than performing hemostasis after a cesarean section. In addition, because a sufficient visual field is necessary for accurate exploration, a lower midline incision is preferred over a transverse incision.
In the case of a pregnant woman complaining of sudden abdominal pain without vaginal bleeding, a differential diagnosis is necessary to exclude obstetrical emergencies and differentiate hemoperitoneum. Because hemoperitoneum during pregnancy is a very rare disease, currently no clear medical treatment guidelines exist. For preterm cases before 34 weeks of pregnancy, if hemostasis can be safely achieved after careful exploration and consideration of the patient and fetus, the pregnancy can be maintained so that complications from premature birth can be reduced.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Salama S, Nizard J, Camus E, Ville Y. Spontaneous haemoperitoneum after the second trimester of pregnancy. Diagnosis and management. Eur J Obstet Gynecol Reprod Biol. 2009;142:82–83. doi: 10.1016/j.ejogrb.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Diaz-Murillo R, Tobias-Gonzalez P, Lopez-Magallon S, Magdaleno-Dans F, Bartha JL. Spontaneous hemoperitoneum due to rupture of uterine varicose veins during labor successfully treated by percutaneous embolization. Case Rep Obstet Gynecol. 2014;2014:580384. doi: 10.1155/2014/580384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y, Zhao Y, Wei Y, Li R, Qiao J. Spontaneous rupture of subserous uterine veins during late pregnancy after in vitro fertilization. Fertil Steril. 2009;92:395.e13–395.e16. doi: 10.1016/j.fertnstert.2009.03.096. [DOI] [PubMed] [Google Scholar]
- 4.Doger E, Cakiroglu Y, Yildirim Kopuk S, Akar B, Caliskan E, Yucesoy G. Spontaneous rupture of uterine vein in twin pregnancy. Case Rep Obstet Gynecol. 2013;2013:596707. doi: 10.1155/2013/596707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakaya Y, Itoh H, Muramatsu K, Otome M, Kobayashi Y, Hirai K, et al. A case of spontaneous rupture of a uterine superficial varicose vein in midgestation. J Obstet Gynaecol Res. 2011;37:1149–1153. doi: 10.1111/j.1447-0756.2010.01489.x. [DOI] [PubMed] [Google Scholar]
- 6.Giulini S, Zanin R, Volpe A. Hemoperitoneum in pregnancy from a ruptured varix of broad ligament. Arch Gynecol Obstet. 2010;282:459–461. doi: 10.1007/s00404-010-1411-7. [DOI] [PubMed] [Google Scholar]
- 7.Vellekoop J, de Leeuw JP, Neijenhuis PA. Spontaneous rupture of a utero-ovarian vein during pregnancy. Am J Obstet Gynecol. 2001;184:241–242. doi: 10.1067/mob.2001.110310. [DOI] [PubMed] [Google Scholar]
- 8.Lim PS, Ng SP, Shafiee MN, Kampan N, Jamil MA. Spontaneous rupture of uterine varicose veins: a rare cause for obstetric shock. J Obstet Gynaecol Res. 2014;40:1791–1794. doi: 10.1111/jog.12402. [DOI] [PubMed] [Google Scholar]
- 9.Wu CY, Hwang JL, Lin YH, Hsieh BC, Seow KM, Huang LW. Spontaneous hemoperitoneum in pregnancy from a ruptured superficial uterine vessel. Taiwan J Obstet Gynecol. 2007;46:77–80. doi: 10.1016/S1028-4559(08)60114-X. [DOI] [PubMed] [Google Scholar]
- 10.Palacios-Jaraquemada JM, Fiorillo A, von Petery F, Colaci D, Leguizamon G. Uterine repair and successful pregnancy after myometrial and placental rupture with massive haemoperitoneum. BJOG. 2009;116:456–460. doi: 10.1111/j.1471-0528.2008.01980.x. [DOI] [PubMed] [Google Scholar]
- 11.Roche M, Ibarrola M, Lamberto N, Larranaga C, Garcia MA. Spontaneous hemoperitoneum in a twin pregnancy complicated by endometriosis. J Matern Fetal Neonatal Med. 2008;21:924–926. doi: 10.1080/14767050802353572. [DOI] [PubMed] [Google Scholar]
- 12.Koifman A, Weintraub AY, Segal D. Idiopathic spontaneous hemoperitoneum during pregnancy. Arch Gynecol Obstet. 2007;276:269–270. doi: 10.1007/s00404-006-0276-2. [DOI] [PubMed] [Google Scholar]
- 13.Shi Q, Zhou HG, Liu XR, Li JP. Spontaneous hemoperitoneum with intrahepatic cholestasis during the third trimester of pregnancy. Int J Gynaecol Obstet. 2014;127:297–298. doi: 10.1016/j.ijgo.2014.07.016. [DOI] [PubMed] [Google Scholar]