Abstract
Background
The age and degree of comorbidity among transplant candidates is increasing. Knowledge of survival benefit in relation to recipient age and comorbidity is important, considering the scarcity of organs available for transplantation. The aim of the present study was to analyze the chances and survival benefit of transplantation among patients in different age groups and with different degrees of comorbidity score at the time of entering the waiting list.
Methods
Data from the Danish Nephrology Registry and Scandiatransplant were merged. Charlson Comorbidity Index scores were derived from the National Danish Admissions Registry. Study period is from January 1, 1995, to December 31, 2011. A multistate model was used to analyze the chance of having a renal transplantation and the effect of transplantation in different patients groups.
Results
Patients older than 65 years and patients with high comorbidity score had a decreased chance of being transplanted. However, if patients older than 65 years were transplanted with deceased donor, the mortality risk was reduced by 55% (hazard rate, 0.45 (0.26-0.75). In patients with a comorbidity score of 5 or greater, receiving a deceased donor transplant reduced the mortality risk by 72% (hazard rate, 0.28 (0.20-0.39). The overall survival benefit was 62% versus 70% in deceased versus living donor transplanted patients.
Conclusions
Poor health and old age reduced the chance of being transplanted. However, patients older than 65 years and patients with high comorbidity still had a survival benefit from renal transplantation.
Renal transplantation is considered the best renal replacement treatment for patients with end-stage renal disease (ESRD).1,2 Although no prospective studies, randomizing patients to either treatment with dialysis or renal transplantation have been performed, several retrospective registry studies have compared survival among waiting list (WL) patients to transplanted patients and found that even after correction for the difference in age, sex, and renal diagnosis, the mortality in WL patients is significantly higher than in transplanted patients.1-10 The main problem in retrospective registry studies is the possibility of selection bias. Although all transplantation candidates undergo the same evaluation before being accepted on the WL, it is not known if the patients who never receive a transplant were actually as healthy as the patients who were transplanted. In general, large registry studies have no or very limited information on comorbidity in transplant candidates.11,12 The Danish Nephrology Registry (DNR) in combination with the Scandiatransplant registry contains detailed data concerning all ESRD patients, including comorbidity data derived from the Danish National Patient Register, which records all hospital and outpatient discharge diagnoses. Comorbidity data are available both at time of WL entry and transplantation.
Patients older than 60 years are the fastest-growing group of patients with ESRD.13 In Denmark, as in many other countries, there has been a tendency to accept more patients on the WL regardless of age and comorbidity. Because of the disparity between the supply and demand for kidney transplantation, some of the patients on the WL die while they are waiting for a kidney, and others are permanently withdrawn from the WL due to progression of comorbidity. The allocation of kidneys toward patients who may benefit the most is thus an increasingly important issue.
The aims of this study were therefore to use data regarding comorbidity at the time of entering the WL to analyze the effect of health status on the chance of being transplanted, and to analyze the effect of transplantation on mortality in general and in subgroups according to age and comorbidity. Finally, an analysis of causes of death was performed.
MATERIALS AND METHODS
Data were derived from the DNR, which has been comprehensive since 1990. The registry forms the basis of the Danish section of the European Renal Association-European Dialysis and Transplantation Association registry. The following data were recorded: date of birth, sex, renal diagnosis using standard European Renal Association-European Dialysis and Transplantation Association terminology, date of ESRD, treatment modality (haemodialysis, peritoneal dialysis or transplantation), date of change of treatment modality, follow-up date (death, lost to follow-up), and cause of death.
The Scandiatransplant database (SCTP) was reorganized in 1994. Since then, all Danish patients placed on the WL or receiving living or deceased donor transplantation (DDT) have been registered. The following data from SCTP were recorded: date of birth, date of entry on the WL, withdrawal date, and withdrawal cause (transplantation, death, or permanent withdrawal). Withdrawal from the WL was not studied in this investigation. Data from SCTP were merged with data from DNR. Patients, who waited for their first renal transplant, and whose first registration on the SCTP WL was between January 1, 1995, and December 31, 2011, were included. All patients were followed up until death, emigration or December 31, 2011. The WL patients who received a transplant in a foreign country were included. Information on donor age, sex, body mass index (BMI), and blood type was also recorded.
The Charlson Comorbidity Index (CCI) scores were derived from the Danish National Patient Register, which has recorded all hospital discharge diagnoses since 1977.14,15 The CCI is validated in patients with ESRD patients and is linked to the Danish Registry.16 The CCI scores were available for the time of first WL registration and include 19 diagnoses associated with increased risk of death.17 All patients were automatically assigned 2 CCI points due to renal failure.
In Denmark, patients younger than 18 years have transplantation priority, meaning that they are offered the first suitable kidney available. Policies concerning adult organ allocation differ between the transplantation centres, including such factors as best tissue type match, best age match, or WL duration. In a national report from 2007, there was no difference in waiting time for adults relative to age.18
Statistical Analysis
We analyzed data by using a multistate model including both DDT and living donor transplantation (LDT). At any given time after the first WL entry, a patient is in 1 of 3 main stages: (1) still on the WL, (2) transplanted with a deceased or a living donor, or (3) dead. The transition between stages is illustrated in Figure 1. In our analyses, withdrawal from the WL, graft failure (meaning that the patient returned to dialysis treatment), or repeat transplants were ignored.
FIGURE 1.
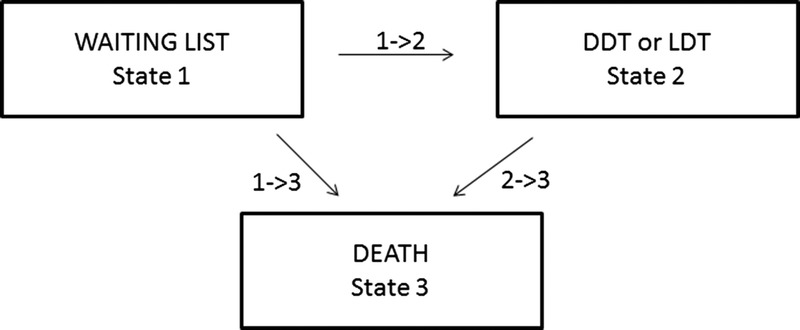
Multi state model DDT, LDT.
First, we analyzed the effects of baseline (fixed) covariates on time to transplantation (meaning the chance of being transplanted), where the cause-specific hazard is modelled by Cox regression (Figure 1, transition 1- to >2). Second, we analyzed the effects of baseline (fixed) covariates as well as the effect of time-dependent transplantation status on mortality by Cox regression (transition 1 to >3 and 2 to >3 combined). Figure 2 illustrates the model fit by plotting cumulative hazards based on a (univariate) Cox model with common baseline hazard for both LDT and DDT status against separate cumulative hazard estimates from a stratified Cox mode without covariates (for transition 1 to >3, patients are censored at time of transplantation; for transition 2 to >3, patients enter at time of transplantation [delayed entry]). Additionally, we explored interactions between transplantation status and age category, comorbid category, and cohort separately in the multivariable setting.
FIGURE 2.
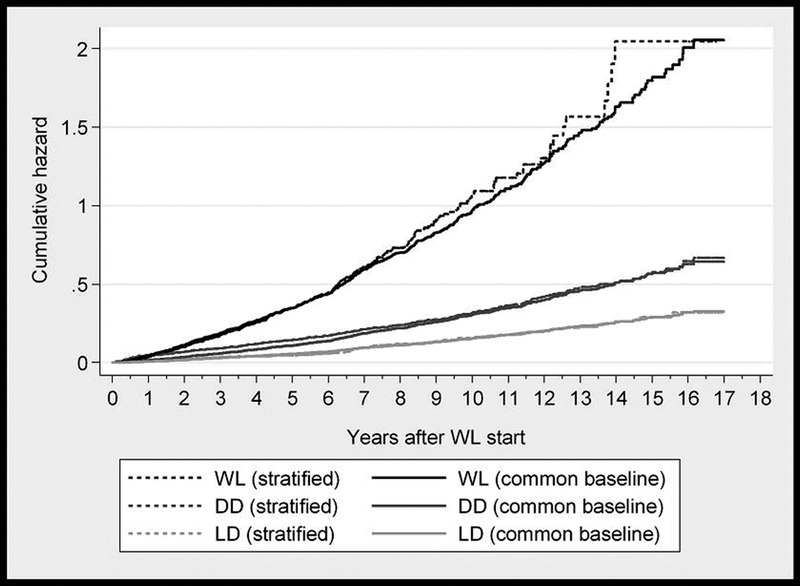
Illustration of model fit. Cumulative hazards for mortality in patients remaining on the waiting list compared to transplanted patients based on stratified versus univariate Cox regression (common baseline).
Third, we expanded the multistate model to incorporate different causes of death divided into 5 categories: infection, cancer, heart disease, vascular disease, and other cause. Last, we analyzed the effects of fixed covariates, including donor information, on mortality after transplantation by Cox regression (transition 2 to >3 alone).
RESULTS
A total of 3174 patients were included in the study, and 2349 of these patients had a first renal transplant during the study period. Transplantation with a deceased donor was performed in 1535 patients, including 1 transplantation abroad, whereas 814 patients received a transplant from a living donor, including 19 transplantations abroad. Only 1 patient was lost to follow-up due to emigration.
Patient Characteristics at Baseline
The distribution of patient baseline characteristics at the time of entering the WL, after 1, 5, and 10 years, and in transplanted versus never transplanted/WL patients is shown in Table 1. The number of patients entering the WL per year increased after 2002. A total of 37% had been on dialysis for more than 1 year before being listed for transplantation. Approximately half of the patients had no comorbidity besides their renal failure, whereas 22% had a CCI index of 5 or more. The percentage of patients older than 65 years at the time of entering the WL, increased from 2% during the first period to 8% during the last period (data not shown). The patients in the WL group were older, spend longer time in dialysis before entering the WL, and had more comorbidity at the time of entering the WL compared to the transplanted patients. Figure 3 shows the patient status after 1, 2, 3, 4, 5, and 10 years. Nearly half of the patients had a renal transplant within the first year after entering the WL, whereas 71% and 74% had been transplanted within 5 and 10 years, respectively.
TABLE 1.
Patient characteristics at the time of entering the waiting list and status after 1, 5, and 10 y and at EOS
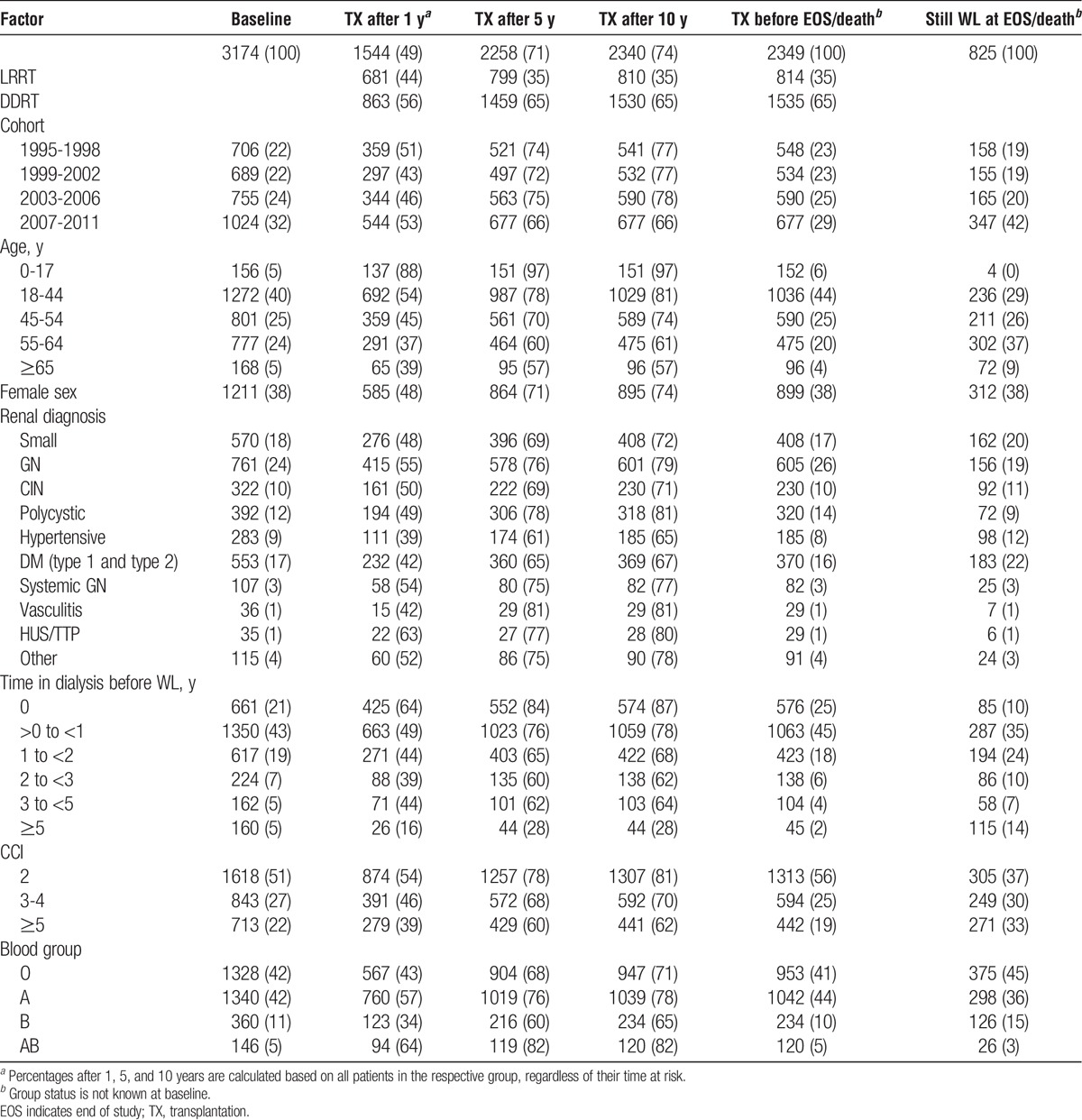
FIGURE 3.

Percentage of patients who were transplanted 1 to 5 and 10 years after entering the waiting list (based on the 3174 patients included, regardless of their time of risk).
The Chance of Receiving a Renal Transplant
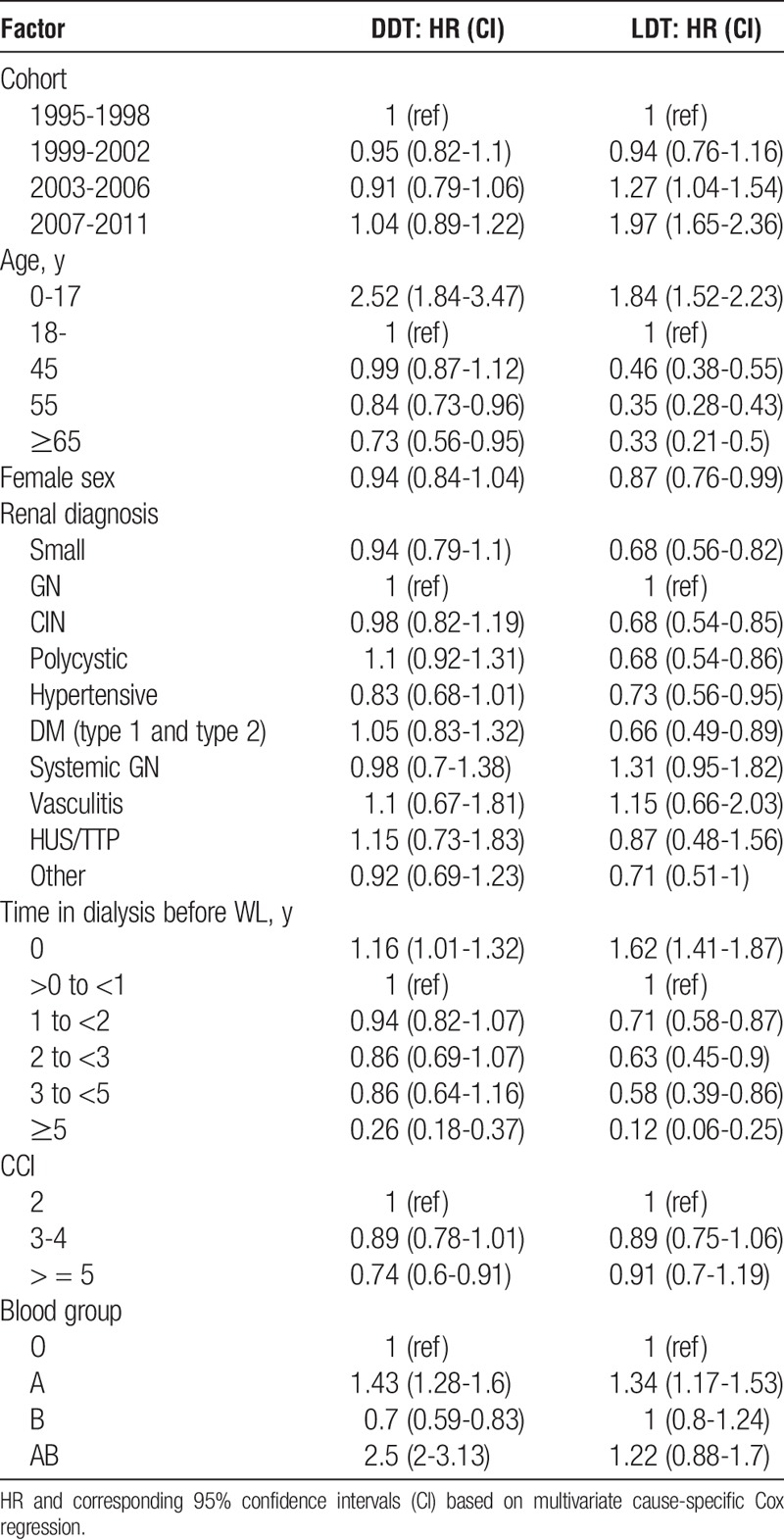
Table 2 shows the relationship between the effects of baseline (fixed) covariates and the chance of renal transplantation, defined as time to transplantation. Dividing the patients into 4 cohorts according to the year of entering the WL, the table shows that the chance of being transplanted with a deceased donor did not change during the study period, whereas the chance of being transplanted with a living donor increased significantly in the third (2003-2006) and fourth (2007-2011) cohorts. Patients younger than 18 years when entering the WL were more often transplanted with a living donor. In addition, they had a significantly higher chance of DDT, in accordance with national allocation policy. Patients older than 55 years had a significantly decreased transplantation chance compared with patients 18 to 44 years. There was a highly significantly decreased LDT chance with increasing age. Patients who were listed for transplantation before ESRD had a significantly better DDT chance compared with patients who were listed during the first year after ESRD, whereas patients who had been on dialysis for more than 5 years had a 74% decreased chance of DDT compared to patients who were listed within the first year. The DDT chance was significantly lower in patients with a CCI of 5 or more, but this was not the case for LDT. Patients with the blood type B had significantly lower chance of DDT, whereas blood type did not matter in LDT.
TABLE 2.
Time to transplantation (chance of having a transplantation)
Survival and Associated Variables
The unadjusted cumulative hazard rate (HR) for death in patients remaining on the WL compared with transplanted patients is shown in Figure 2, indicating a satisfactory model fit. The cumulative hazard was highly increased in patients who were not transplanted. A multivariable mortality analysis corrected for cohort, age, sex, renal diagnosis, time on dialysis before entering the WL, CCI, is shown in Table 3. Patients who received either LDT or DDT had a highly significant lower mortality risk with a survival benefit of 70% in LDT and 62% in DDT. The overall prognosis for all patients improved over time with a 44% mortality risk reduction in the period 2007 to 2011 compared with 1995 to 1998. This HR reduction was independent of transplantation status, because adding an interaction between transplantation status and cohort to the multivariate model did not lead to statistically significant model improvement (Likelihood ratio test: P = 0.53). Mortality risk in the 2349 patients who were transplanted during the study is shown in Table 4. Neither donor age, donor type (DDT/LDT) nor time on the WL before transplantation affected recipient mortality risk. However, donor BMI higher than 25 or lower than 18.5 was related to a significantly poorer recipient survival. Also, cohort, recipient age, time on dialysis before WL entry, diabetes, and CCI all significantly affected the mortality risk.
TABLE 3.
Mortality (time to death) in 3174 patients after entering the waiting list for renal transplantation
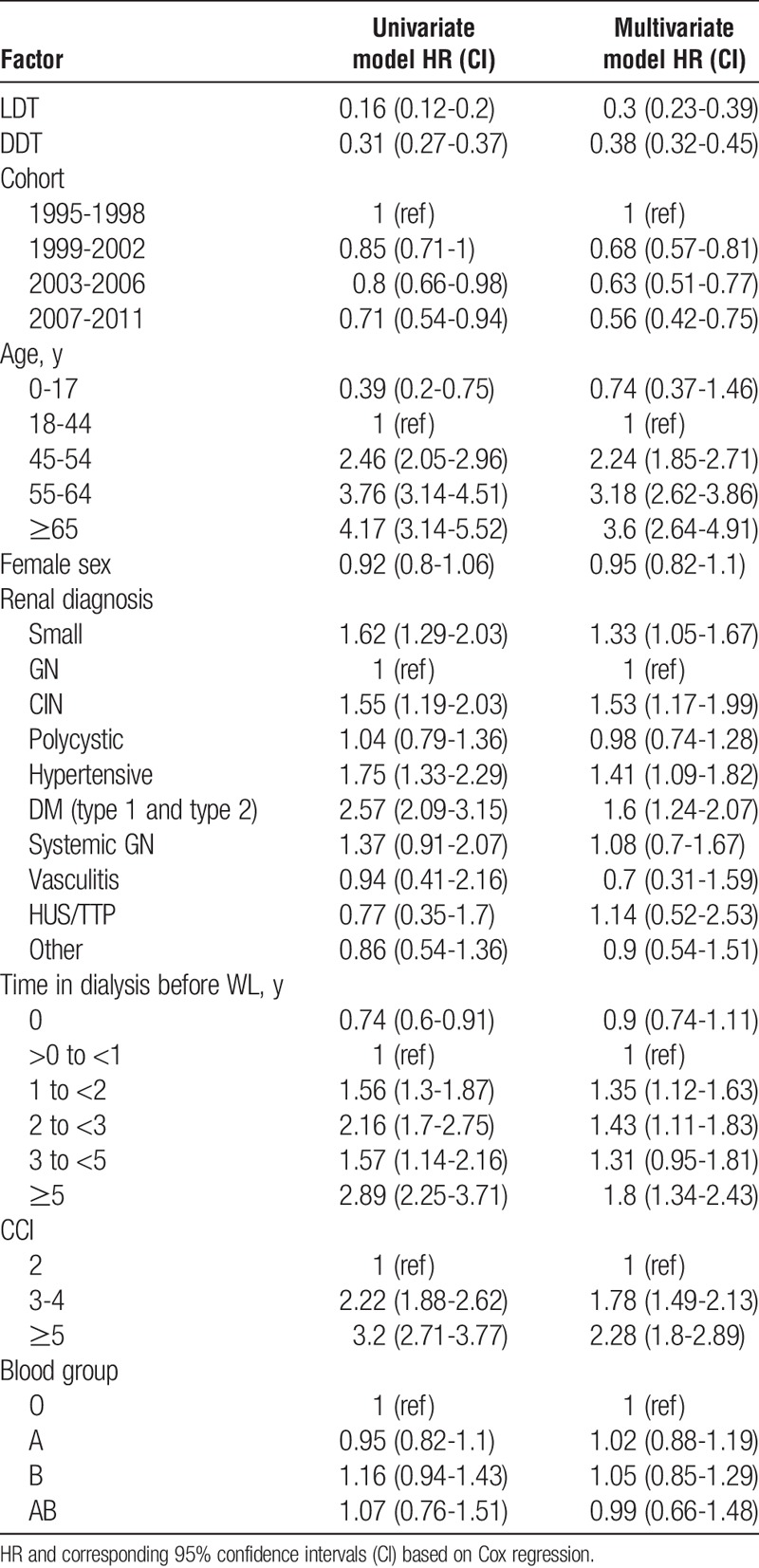
TABLE 4.
Mortality (time from TX to death) in 2349 patients who had a renal transplant

Age and Comorbidity
Adding an interaction of age category with transplantation status to the model resulted in borderline model improvement (Likelihood ratio test: P = 0.057). The corresponding HRs are shown in Figure 4. Using the transplant status 0 (WL) and age group 18 to 44 years as reference, the figure shows an increasing mortality with increasing age, but also a significantly decreased mortality in patients who changed transplant status from 0 (WL) to either 1 or 2 ( DDT or LDT). Changing the reference category to patients older than 65 years, and in the WL group, we found that the HR for DDT was 0.45 (0.26-0.75, 95% CI) and 0.58 (0.21-1.60, 95% CI) for LDT.
FIGURE 4.
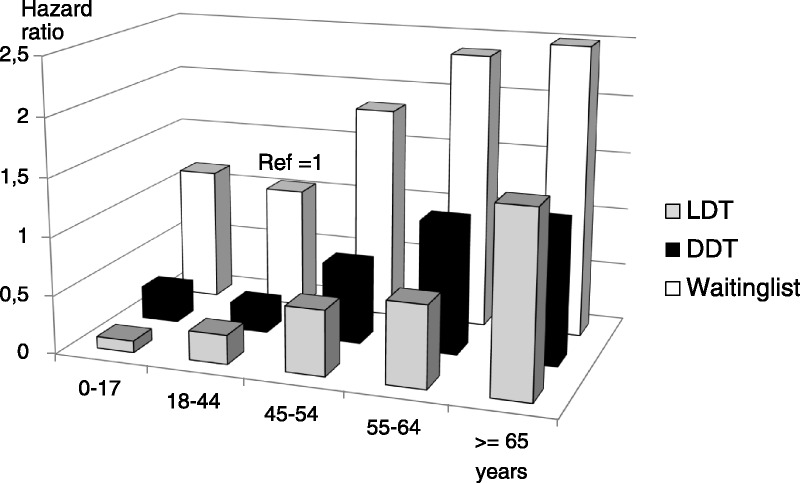
Mortality (HR) according to transplant status and age group. Multivariate analysis of 3174 patients, with patients in the age group 18 to 44 years and never transplanted as the reference (HR = 1).
Mortality risk increased significantly with increasing CCI value. The mortality risk of the 22% of the patients, who had a CCI of 5 or more at WL entry, was more than 100% higher than patients with a CCI of 2. The addition of an interaction between transplantation status and CCI category improved the model significantly (Likelihood ratio test: P = 0.02), implying a separate effect of transplantation status for each CCI group (Figure 5). Changing reference category to patients with CCI of 5 or greater and transplant status 0 (WL), we found that the HR for DDT was 0.28 (0.20-0.39) and for LDT 0.33 (0.21-0.52).
FIGURE 5.
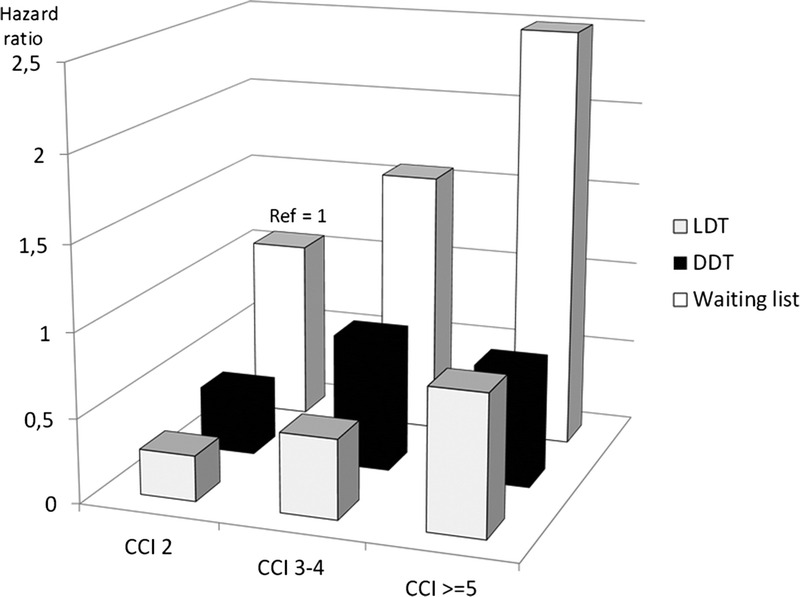
Mortality (HR) according to transplant status and CCI group Multivariate analysis of 3174 patients, with patients having a CCI of 2 and never transplanted as the reference (HR = 1).
Causes of Death
A total of 832 (26%) patients died during the study period. The causes of death were categorised in 5 main groups. The distribution in WL, DDT, and LDT patients is shown in Figure 6. The increased mortality seen in WL patients was mainly due to cardiovascular diseases and infection. The absolute risk of dying because of cancer was not significantly different in the 3 groups, although cancer represented a higher percentage of deaths among transplanted patients compared to WL patients on dialysis.
FIGURE 6.
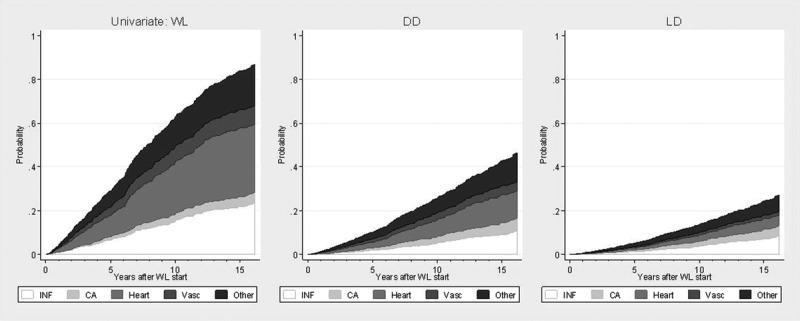
Cumulative incidence of dying due to infection, cancer, hearts diseases, vascular diseases or other causes of death in patients on the WL, DDT, and LDT based on univariate Cox regression with time-dependent transplantation status. INF indicates infection; Ca, cancer; Heart, heart diseases; Vasc, vascular diseases.
DISCUSSION
This epidemiological study of renal transplant candidates in Denmark, combining data from several national registries, demonstrated a highly significant survival benefit of renal transplantation, even in patients older than 65 years and in patients with high comorbidity score. This is in accordance with several other retrospective register studies that have reported similarly improved survival among transplanted patients. In a systematic review of 110 studies, including a total of more than 1.9 million patients, comparing outcomes in kidney transplantation with dialysis, Tonelli et al3 found that kidney transplantation was associated with substantial reductions in the risk of mortality and cardiovascular events. The review also reported an increasing relative survival benefit of transplantation over time, with a 66% mortality reduction compared with dialysis in 1985 and 83% reduction in 2005. However, most studies did not include any information on comorbidity and many studies included dialysis patients not listed for transplantation in the comparator group.
Thus, renal transplantation is considered the preferred treatment for patients with ESRD, but although WL candidates are evaluated by the same pretransplant work-up program before entering the WL, the present study showed that patients not receiving a renal transplant had significantly more comorbidity, older age, and longer time from ESRD to WL entry. Some of the patients who remain on the WLs are probably not equally good candidates for transplantation and may not have the same chance of being transplanted. By using information on comorbidity, we aimed to eliminate some of the assumed selection bias.
We have not included data on temporary withdrawal, but it is likely that patients with high comorbidity score are more often temporarily unsuitable for transplantation due to infection or other complications, although this may not always be registered in the transplant database. However, if the patients with high comorbidity index were transplanted, there was a highly decreased mortality. In the analysis of the survival benefit of transplantation in the different age groups, we found significantly improved survival even in patients older than 65 years who were transplanted with a deceased donor, but only an insignificantly lower HR for LDT. This lack of significance may be due to lack of power, since only a limited number of patients older than 65 years received a LDT.
In this study, the percentage of patients older than 65 years when entering the WL increased from 2% to 8% during the 17-year study period, whereas more than 50% of all new patients with ESRD in Denmark in 2011 were older than 65 years. In a study of more than 50 000 patients older than 60 years when listed for renal transplantation in the United States, Schold et al19 estimated the mortality risk within 5 years and compared that to the chance of transplantation within 5 years. The study concluded that among patients older than 60 years when entering the WL, 50% died before they received DDT. This is in accordance with the finding of a decreased transplantation chance among patients with high CCI score and age older than 65 years in this study. However, if patients older than 65 years were transplanted, there was a significant survival benefit, although the mortality risk was not reduced as much as in patients younger than 45 years. In a study of 5667 renal transplant candidates older than 70 years, Rao et al20 found that among the 2438 patients who were transplanted, the mortality risk deceased by 41%, compared to 55% among patients older than 65 years in the present study.
The present study demonstrates that nearly half of the patients were transplanted by either DDT or LDT within the first year after entering the WL, and 71% had been transplanted after 5 years of waiting. We found an unchanged chance of DDT during the study period but an increasing number of performed LDT during the last 2 periods. Possible causes include the introduction of AB0-incompatible living donor kidney transplantation after 2006, increasing acceptance of nonrelated living donors (friends or partners), and the general adoption of laparoscopic donor nephrectomises.
The excess mortality among nontransplanted patients was mainly due to cardiovascular disease and infection. The absolute risk of dying because of cancer was not different among the transplanted patients compared with the WL patients. In this study, we only analyzed mortality due to cancer and not the overall incidence of cancer. An increased total incidence of cancer in kidney transplanted patients has been reported in several studies.21-24 Thirty-two patients (19 in the WL group and 13 of the transplanted patients) were registered with uremia as the cause of death. Most of these will have been due to withdrawal of active therapy, because patient death due to lack of dialysis access is very rare in Danish clinical practice. In addition, dialysis patients with serious access problems can be listed as urgent in the WL. The increased mortality among nontransplanted WL patients is therefore probably due to comorbidity progression rather than dialysis technique failure.
Time from ESRD to WL entry significantly affected both transplant chance and patient survival. This variable could be a measure of a more troublesome process during the work-up program due to comorbidity and could therefore be a prognostic factor. Transplantation with living donor showed a relatively larger benefit compared to staying on the WL than having DDT. However, when we analyzed only the transplanted patients and corrected also for donor age and donor BMI, there was an insignificant difference in mortality risk in DDT compared to LDT.
We did not study either temporary or permanent withdrawals from the WL, nor was graft failure studied. Both temporary and permanent withdrawals from the WL are difficult to analyze in a registry study like this and could represent a bias when ignored, but also if included in the analyses. The problem is that we do not know if the condition that had lead to the withdrawal was related to the uremic condition and the dialysis or would have occurred, even if the patient had been transplanted. Removing patients from the analysis, when they are withdrawn from the WL, would cause bias and overestimate the effect of transplantation, because in many cases, patients are withdrawn due to illness with an associated increased risk of death. On the other hand, ignoring the withdrawals could also overestimate the effect of transplantation, because some of these patients will in fact no longer be eligible for transplantation.
The number of included patients in this study is relatively small compared with other studies from larger countries. However, the databases are 100% comprehensive and cover the entire Danish population of approximately 5.5 million people. In contrast to several other studies in this field, this study included information about comorbidity at the time of entering the WL in all patients. The CCI is based on the discharge diagnoses, which are always established by a clinician. In a study from 2003, Hemmelgarn et al16 found that the original Charlson index is a valid tool to assess comorbidity and predict survival in patients with ESRD. Because the selection bias is one of the most important drawbacks in register studies like this, information concerning comorbidity is very valuable.
CONCLUSIONS
The percentage of transplant candidates older than 65 years increased during the study period. Poor health and old age at the time of entering the WL reduced the chance of being transplanted. Nevertheless, the survival benefit of transplantation was maintained irrespective of age and comorbidity. The increased mortality in nontransplanted patients was mainly due to increased cardiovascular and infectious disease. Given that a patient can pass the standard pretransplantation work-up program, these findings do not support limiting access to transplantation on the basis of age or comorbidity.
Footnotes
The authors declare no funding or conflicts of interest.
V.R.S. participated in research design, writing of the article, and data analysis. J.H. participated in research design, writing of the article, and data analysis. S.W. participated in research design, writing of the paper and data analysis. S.S.S. participated in research design and writing of the article.
REFERENCES
- 1.Meier-Kriesche HU, Ojo AO, Port FK, et al. Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J Am Soc Nephrol. 2001;12:1293–1296. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. [DOI] [PubMed] [Google Scholar]
- 3.Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093–2109. [DOI] [PubMed] [Google Scholar]
- 4.Gill JS, Tonelli M, Johnson N, et al. The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int. 2005;68:2345–2351. [DOI] [PubMed] [Google Scholar]
- 5.Massie AB, Luo X, Chow EK, et al. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am J Transplant. 2014;14:2310–2316. [DOI] [PubMed] [Google Scholar]
- 6.Medin C, Elinder CG, Hylander B, et al. Survival of patients who have been on a waiting list for renal transplantation. Nephrol Dial Transplant. 2000;15:701–704. [DOI] [PubMed] [Google Scholar]
- 7.Meier-Kriesche HU, Port FK, Ojo AO, et al. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–1317. [DOI] [PubMed] [Google Scholar]
- 8.Rabbat CG, Thorpe KE, Russell JD, et al. Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol. 2000;11:917–922. [DOI] [PubMed] [Google Scholar]
- 9.Schold JD, Buccini LD, Goldfarb DA, et al. Association between Kidney Transplant Center Performance and the Survival Benefit of Transplantation Versus Dialysis. Clin J Am Soc Nephrol. 2014;9:1773–1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorensen VR, Mathiesen ER, Heaf J, et al. Improved survival rate in patients with diabetes and end-stage renal disease in Denmark. Diabetologia. 2007;50:922–929. [DOI] [PubMed] [Google Scholar]
- 11.Vollmer WM, Wahl PW, Blagg CR. Survival with dialysis and transplantation in patients with end-stage renal disease. N Engl J Med. 1983;308:1553–1558. [DOI] [PubMed] [Google Scholar]
- 12.Snyder JJ, Kasiske BL, Maclean R. Peripheral arterial disease and renal transplantation. J Am Soc Nephrol. 2006;17:2056–2068. [DOI] [PubMed] [Google Scholar]
- 13.Danovitch G, Savransky E. Challenges in the counselling and management of older kidney transplant candidates. Am J Kidney Dis. 2006;47:S86–S97. [DOI] [PubMed] [Google Scholar]
- 14.Andersen TF, Madsen M, Jorgensen J, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46:263–268. [PubMed] [Google Scholar]
- 15.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39:30–33. [DOI] [PubMed] [Google Scholar]
- 16.Hemmelgarn BR, Manns BJ, Quan H, et al. Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis. 2003;42:125–132. [DOI] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 18.Heaf JG. Waiting List statistics 1995-2006. 2008:55–69. [Google Scholar]
- 19.Schold J, Srinivas TR, Sehgal AR, et al. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol. 2009;4:1239–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rao PS, Merion RM, Ashby VB, et al. Renal transplantation in elderly patients older than 70 years of age: results from the Scientific Registry of Transplant Recipients. Transplantation. 2007;83:1069–1074. [DOI] [PubMed] [Google Scholar]
- 21.Birkeland SA, Lokkegaard H, Storm HH. Cancer risk in patients on dialysis and after renal transplantation. Lancet. 2000;355:1886–1887. [DOI] [PubMed] [Google Scholar]
- 22.Engels EA, Pfeiffer RM, Fraumeni JF, Jr, et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306:1891–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piselli P, Busnach G, Fratino L, et al. De novo malignancies after organ transplantation: focus on viral infections. Curr Mol Med. 2013;13:1217–1227. [DOI] [PubMed] [Google Scholar]
- 24.Vajdic CM, McDonald SP, McCredie MR, et al. Cancer incidence before and after kidney transplantation. JAMA. 2006;296:2823–2831. [DOI] [PubMed] [Google Scholar]


