Abstract
Aims:
The principal objective of this study was to retrospectively review a series of cases of lactic acidosis (LA) in patients with type 2 diabetes mellitus (T2DM) and examine the relationship with the use of metformin. More generally, the study enabled an investigation of the profiles of patients diagnosed with LA and clinical variables associated with in-hospital mortality.
Methods:
All patients admitted to the Royal Hobart Hospital in Tasmania with LA (lactate >5.0 mmol/L and pH <7.35) over a 4-year period were included. Data extracted included patient demographics, medical history, medications, acute and chronic conditions associated with LA, and relevant pathology results. Multivariate logistic regression analysis was used to identify predictors for in-hospital mortality in patients with LA.
Results:
A total of 139 patients with LA were included in this study. Of these, 23 patients had T2DM and 11 patients were taking metformin. All metformin-treated patients had at least 1 additional medical condition (either chronic or acute) associated with an increased risk for LA. More than half (n = 72, 51.8%) of the patients with LA died during hospitalization. Multivariate logistic regression revealed older age and lower pH as the significant independent predictors (P < 0.05) for in-hospital mortality.
Conclusion:
LA was associated with high in-hospital mortality, with older age and lower pH as the significant risk factors for mortality. In patients with LA, approximately half of the patients with T2DM were receiving metformin. All the patients treated with metformin had other medical conditions that were risk factors for developing LA. The role of LA in patients treated with metformin is seemingly overemphasized.
Keywords: in-hospital mortality, lactic acidosis, metformin
1. Introduction
Lactic acidosis (LA) is defined as a state of decreased systemic pH (pH <7.35) and an elevated plasma lactate concentration (>5 mmol/L). It remains the most common cause of metabolic acidosis in hospitalized patients.[1] A recent review summarized the major causes of LA and the presumed mechanisms.[2] Typically, LA is divided into disorders associated with tissue hypoxia (Cohen and Woods classification type A) and disorders in which tissue hypoxia is absent (type B). Type A LA may result from severe heart failure, sepsis, or cardiopulmonary arrest; type B can be caused by renal and hepatic failure, diabetes mellitus (DM), or drugs and toxins, including metformin, valproate, and anti-retroviral agents.[3,4] It has been reported that cardiogenic or hypovolaemic shock, severe heart failure, trauma, and sepsis are the most common causes of LA.[5]
Lactate accumulation may be caused by increased production (i.e., increase glycolysis caused by hypoperfusion, hypoxaemia), decreased clearance (impaired hepatic metabolism or renal excretion), or a combination of both.[6] The exact pathophysiology of elevated lactate is likely to be the result of more than 1 condition. Many studies have shown that high lactate levels are associated with substantially increased mortality.[2,7,8] The mortality rate of LA has been reported to be between 50% and 83%.[9–11]
DM has been also considered as one of the causes of LA.[2] The possible explanations include LA arising in patients with diabetic ketoacidosis, which is likely to be due to hypovolaemia[2]; or reduced activity of pyruvate dehydrogenase, which may cause increased lactate levels in patients with DM independent of ketoacidosis.[12] In addition, diabetic patients with micro- or macrovascular disease are at an increased risk of LA, possibly due to the associated systemic hypoxia.[12] Furthermore, metformin, which is the first choice for the pharmacological treatment of type 2 DM (T2DM) in Australia[13] and many other countries,[14,15] has also been reported to be associated with LA. However, it has been suggested that the development of LA in metformin users is most likely due to the presence of concomitant risk factors,[16] rather than metformin alone. A causal link between metformin and LA is yet to be scientifically established.
Given this background, the principal objective of this study was to retrospectively review a series of cases of LA in patients with T2DM and examine the relationship with the use of metformin. More generally, the study investigated the profiles of patients diagnosed with LA and clinical variables associated with in-hospital mortality.
2. Methods
This retrospective audit included patients with a diagnosis of acidosis and who were admitted to the Royal Hobart Hospital (RHH), Tasmania between January 1, 2010, and December 31, 2013. Patients were included in the study if they were admitted for at least an overnight stay, aged 18 years and above, and noted to have acidosis (ICD10 E87.2) either at the time of admission or during their hospital stay. Overall, 476 patients with acidosis during the study period were screened for inclusion.
LA cases were identified as per documentation in the medical record and from the pathology results (lactate level >5 mmol/L and a pH <7.35 from the same sample). For the purpose of this study, the maximum lactate value in each LA case was documented, and the pH value shown in the same test was reported. The LA cases associated with the usage of metformin were reviewed separately.
Other data extracted from patients’ medical records included reason for admission, demographics, medical conditions (both chronic and acute), medications, and relevant pathology results [e.g., lactate, pH, bicarbonate, pao2, paco2, estimated glomerular filtration rate (eGFR), serum creatinine (SCr), albumin, total bilirubin, alanine aminotransferase (ALT), alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT)].
For the purpose of this study, liver disease was defined either by documentation in the patient's medical history or by the presence of abnormal liver function tests (LFTs), defined as hypoalbuminemia and abnormal serum levels of at least 2 of the following: total bilirubin, ALT, ALP, and GGT. Acute kidney injury (AKI) was documented if noted in the patient's record during hospitalization, or strongly suspected based on at least 2 increased SCr values.
All medicines potentially implicated in drug-induced LA were identified: metformin, isoniazid, linezolid, theophylline, valproate, spironolactone, beta-agonists, and nucleoside reverse transcriptase inhibitors.[3,4]
The primary endpoint was the relationship between metformin use and LA. Secondarily, we examined determinants of mortality in LA. The data were summarized and analyzed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY). Descriptive statistics were used to describe the data. Chi-square or Fisher exact tests were performed for the categorical variables. Independent t tests were performed for comparing the continuous variables. Spearman tests were used to explore the possible correlation between age, lactate, pH, bicarbonate, and eGFR. Backward logistic regression was used to identify the independent risk factors for in-hospital mortality in patients with LA. Variables whose probability (P) values were ≤0.10 in the univariate analysis were entered into the final logistic regression model. A P value of <0.05 was considered statistically significant. The study was approved by the Tasmania Health and Medical Human Research Ethics Committee (Reference number: H0014090).
3. Results
A total of 139 patients who met the definition of LA were included in the final analysis. Of these (Table 1), the mean age (SD) was 62 ± 18 years (range of 50–77 years) and 44.6% were female. The mean pH (SD) was 7.14 ± 0.15, with a mean (SD) lactate level of 10.1 ± 4.8 mmol/L. Spearman tests revealed that an increased lactate level was correlated with decreased pH (P < 0.01, r = −0.43) and decreased bicarbonate (P < 0.01, r = −0.58).
Table 1.
Number of patients with lactic acidosis.
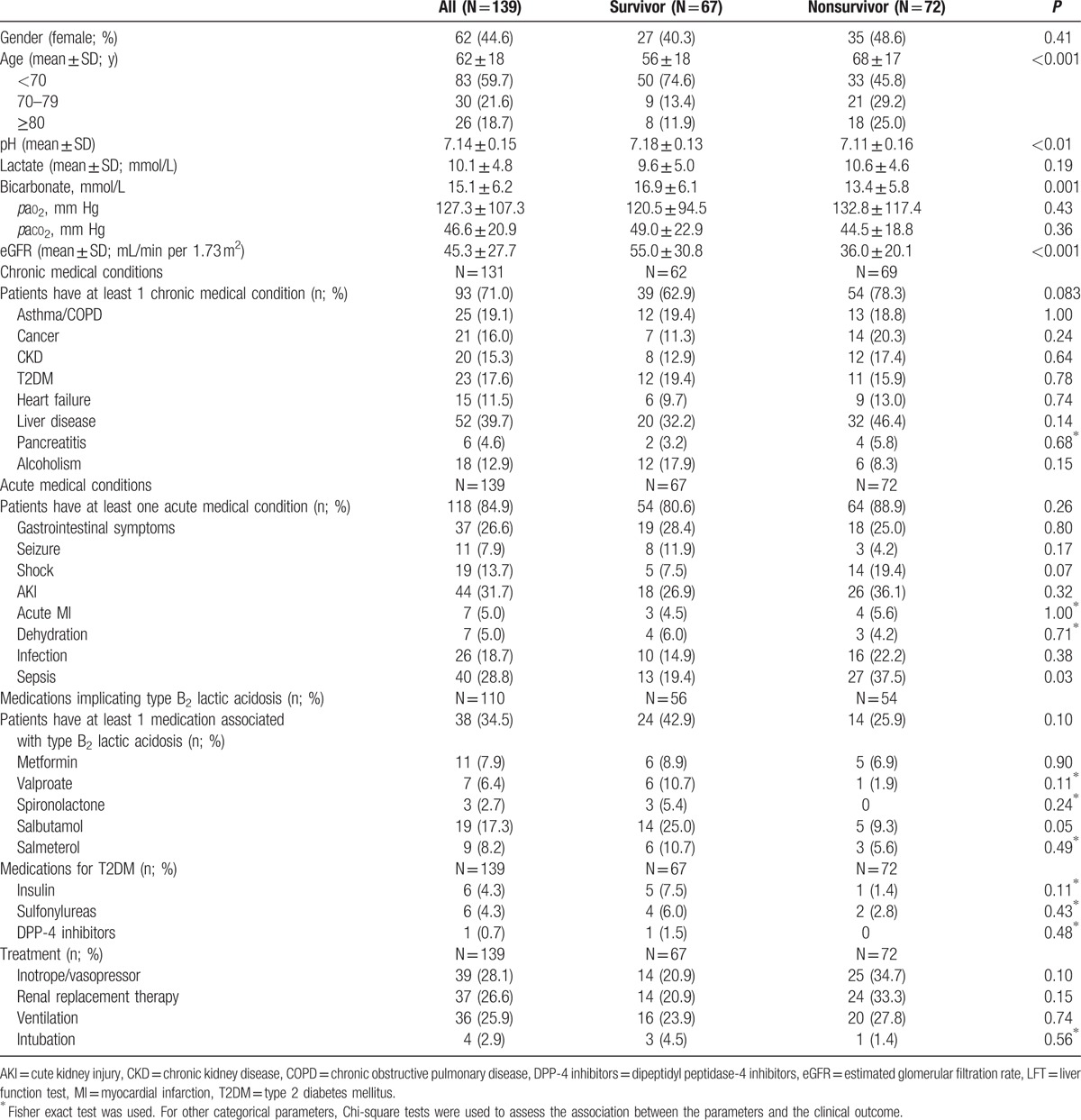
The most common reasons for admission were “diseases of the circulatory system” (n = 36, 25.9%) and “diseases of the digestive system” (n = 20, 14.4%). The most common chronic medical condition associated with LA (131 patients with medical history documented) was liver disease (n = 52, 39.7%), followed by asthma/chronic obstructive pulmonary disease (n = 25, 19.1%). Of the 139 patients, 84.9% (n = 118) had at least 1 acute medical condition associated with LA, with the most common being AKI (n = 44, 31.7%), followed by sepsis (n = 40, 28.8%).
More than half (n = 72, 51.8%) of the patients who experienced LA died during hospitalization. Compared with survivors, the patients who died were much older (P < 0.001, Table 1), with over half of them older than 70 years. Univariate analysis showed that age, pH, bicarbonate, eGFR, and sepsis were all significant factors associated with in-hospital mortality (P ≤ 0.10). Multivariate logistic regression revealed 2 significant independent predictors for in-hospital mortality: aging increased the risk of mortality by 1.04 times for each additional year of age [95% confidence interval (95% CI) 1.01–1.06, P = 0.003], and a lower pH increased the risk of mortality by 25 times with each unit decrease in pH (95% CI 0.002–0.62, P = 0.02).
Of the 131 patients with a medical history documented, 23 had T2DM (6 patients had infection). Over 30% of patients with LA (110 patients with medications documented) were receiving medications associated with type B2 LA. Approximately half (n = 11) of the patients with T2DM were receiving metformin (8 patients were receiving metformin monotherapy; Table 2). There was no significant diffidence in either pH (7.13 ± 0.017 vs 7.15 ± 0.11, P = 0.79) or lactate (10.2 ± 6.9 vs 9.3 ± 3.5 mmol/L, P = 0.67) between metformin users and nonusers, respectively.
Table 2.
Individual information of metformin users with lactic acidosis.
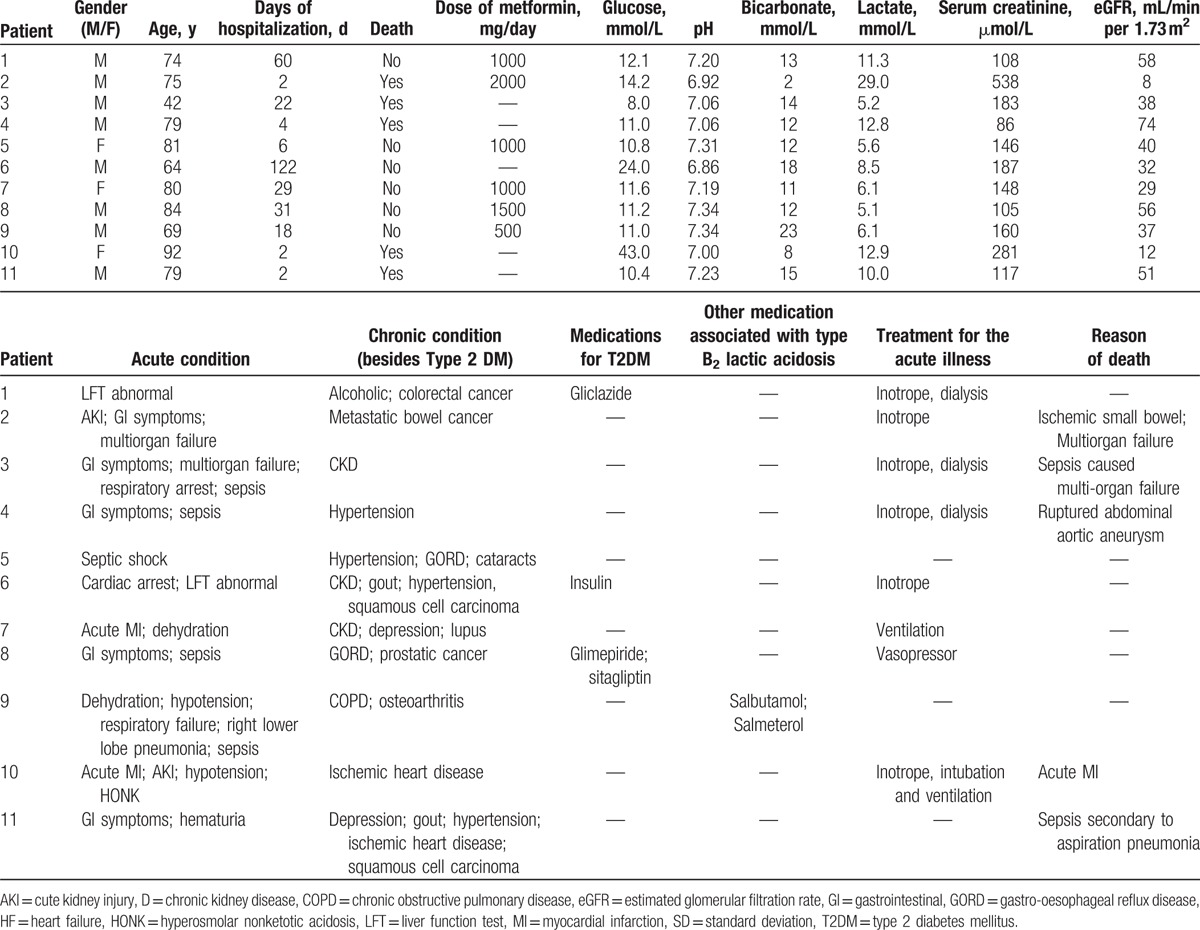
In patients receiving metformin, there were no patients with deliberate overdose, and metformin levels were not reported. Of the 11 metformin-treated patients (mean age of 74 ± 13 years), all patients had at least 1 medical condition (either chronic or acute) associated with an increased risk of LA. However, metformin was documented as the primary reason for the development of LA in 4 patients (patients 2, 5, 7, and 9 in Table 2). In all the other patients, sepsis was documented as the most common reason for LA. Of 11 metformin-treated patients, 5 of them died (45.5%) in the hospital, with 4 of these aged 75 years or older, while in the nonmetformin-treated patients, 6 of them (50%) did not survive. Among the patients who survived, only 1 patient had a lactate level >10 mmol/L (11.3 mmol/L). Metformin was reintroduced to all the survivors at discharge.
4. Discussion
LA was shown to result from various medical conditions, predisposing factors, and medications. Despite appropriate management, the in-hospital mortality was high (approximately 50%). The most significant risk factors for in-hospital mortality were older age and lower pH.
The in-hospital mortality due to LA was comparable to that previously reported. The study by Scale and Harvey reported an in-hospital mortality rate of 54%, with an inclusion of a pH ≤7.2, which was lower than that used in our study (pH < 7.35).[12] Also, consistent with their findings, this present study found no significant difference in lactate levels between patients who died and survived. In both studies, most cases of LA resulting in-hospital mortality were complicated by other medical conditions, such as sepsis and AKI. AKI was reported in more than 30% of the cases and was the most common acute condition associated with LA in our study. In our study, compared with survivors, the patients who died had a higher rate of sepsis (P = 0.03), which has been identified as a common clinical condition associated with an increased mortality in LA patients.[7] Previous studies have demonstrated that mortality of LA cases is increased in patients with multiple comorbidities.[2,8]
A total of 23 patients with LA in our study were diabetic. DM, as well as metformin, is considered to be one of the causes of type B LA, but to date, the exact mechanism of LA has not been elucidated. A study reported similar rates of LA in T2DM patients with and without metformin, and the authors suggested that LA in metformin users was likely related to the underlying medical conditions rather than the use of metformin alone.[17] Furthermore, sulfonylureas have been suspected of LA with the incidence of LA approximately 4.8 cases per 100,000 person-years compared with 3.3 cases per 100,000 person-years among users of metformin.[18] However, the incidence of LA in T2DM patients receiving other anti-diabetic medications is not yet well established.
In our study, 11 patients were receiving metformin either as monotherapy or in combination with other antidiabetic medications. Five patients treated with metformin (45.5%) died, which was higher than a previous study conducted in Australia.[19] That study retrospectively evaluated metformin-associated LA (MALA) cases in an intensive care unit over a 5-year period, including patients with lactate levels >2.0 mmol/L and pH <7.30. A total of 17 patients were diagnosed of MALA with an overall mortality rate of 29% (N = 5). The severity of LA in our study may be different compared with that study, as we only included cases with a lactate level >5.0 mmol/L. Furthermore, our patients receiving metformin were older (74 ± 13 years) than the study conducted in Adelaide (65 ± 10 years). Previous studies have reported that older age was associated with higher mortality in cases of MALA.[12,20]
The safe use of metformin in patients with other chronic risk factors for developing LA is still under debate, especially in patients with stage 3 to 5 CKD. Several studies have recently reported that metformin is a relatively safe option, including in patients with contraindications to its use, such as kidney disease.[21,22] Available data support the “cautious expansion” of metformin use in T2DM patients with mild to moderate renal impairment.[23,24] However, a more careful approach is to be considered in patients who are at risk of abrupt worsening of renal function, especially in patients with CKD stage 3 to 4, who may have serious clinical conditions predisposing to AKI.[25]
Furthermore, it is important to note that to date, no consistent link between LA and the use of metformin has been found.[12,19,26–28] We were not able to identify the clear contribution of metformin due to the other complications associated with LA in each of our cases; besides, the plasma metformin concentration was not measured in the hospital. Instead of “metformin-associated lactic acidosis,” a term “mixed lactic acidosis in metformin-treated patients” has been used.[29] This may be more appropriate to describe LA in metformin users (without metformin concentration measurement) who have other risk factors associated with LA. To further clarify the safety of metformin in patients with contraindications, a prospective study with control groups may be required, including a systematic collection of contraindications with the occurrence of LA, but this is unlikely to occur because of ethical concerns.
This study has some limitations. The retrospective study design may have resulted in missing or incomplete data. Due to the inconsistent documentation of cause of death in the hospital, and the association with multiple conditions of mortality in some patients, it was not always possible to summarize and report the reason for in-hospital mortality. We could not conduct any further investigation in the fatal cases to confirm the relationship with metformin use. Of 11 patients treated with metformin, the dosages were not documented in 5 patients.
5. Conclusion
LA was associated with high in-hospital mortality, with older age and lower pH as the significant risk factors for mortality. Although LA was found in patients receiving metformin, similar numbers of LA were reported in T2DM patients treated with metformin or those nontreated, and the mortality was similar in these 2 groups. All metformin-treated patients had other underlying medical conditions associated with the developing LA. The risk of LA in patients treated with metformin might be overemphasized, and this drug could be considered to be prescribed for more patients.
Footnotes
Abbreviations: AKI = acute kidney injury, ALP = alkaline phosphatase, ALT = alanine aminotransferase, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, DM = diabetes mellitus, DPP-4 inhibitors = dipeptidyl peptidase-4 inhibitors, eGFR = estimated glomerular filtration rate, GGT = gamma-glutamyl transferase, GI = gastrointestinal, GORD = gastro-oesophageal reflux disease, HF = heart failure, HONK = hyperosmolar nonketotic acidosis, LA = lactic acidosis, LFT = liver function test, MI = myocardial infarction, RHH = Royal Hobart Hospital, SCr = serum creatinine, SD = standard deviation, T2DM = type 2 diabetes mellitus.
The authors have no conflicts of interest.
References
- 1.Lalau JD. Lactic Acidosis in Diabetes. Emergencies in Diabetes: Diagnosis Management and Prevention. West Sussex, England:John Wiley & Sons; 2004. [Google Scholar]
- 2.Kraut JA, Madias NE. Lactic acidosis. N Engl J Med 2014; 371:2309–2319. [DOI] [PubMed] [Google Scholar]
- 3.Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit Care Med 1992; 20:80–93. [DOI] [PubMed] [Google Scholar]
- 4.Cohen RD, Woods HF. Lactic acidosis revisited. Diabetes 1983; 32:181–191. [DOI] [PubMed] [Google Scholar]
- 5.Jung B, Rimmele T, Le Goff C, et al. Severe metabolic or mixed acidemia on intensive care unit admission: incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study. Crit Care 2011; 15:R238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phypers B, Pierce T. Lactate physiology in health and disease. Contin Educ Anaesth Crit Care Pain 2006; 6:128–132. [Google Scholar]
- 7.Andersen LW, Mackenhauer J, Roberts JC, et al. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin Proc 2013; 88:1127–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kruse O, Grunnet N, Barfod C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scand J Trauma Resus 2011; 19:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Corte W, Vuylsteke S, De Waele JJ, et al. Severe lactic acidosis in critically ill patients with acute kidney injury treated with renal replacement therapy. J Crit Care 2014; 29:650–655. [DOI] [PubMed] [Google Scholar]
- 10.Gunnerson KJ, Saul M, He S, et al. Lactate versus non-lactate metabolic acidosis: a retrospective outcome evaluation of critically ill patients. Crit Care 2006; 10:R22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stacpoole PW, Wright EC, Baumgartner TG, et al. Natural history and course of acquired lactic acidosis in adults. DCA-Lactic Acidosis Study Group. Am J Med 1994; 97:47–54. [DOI] [PubMed] [Google Scholar]
- 12.Scale T, Harvey JN. Diabetes, metformin and lactic acidosis. Clin Endocrinol (Oxf) 2011; 74:191–196. [DOI] [PubMed] [Google Scholar]
- 13.General Practice Management of Type 2 Diabetes: 2014–15. Melbourne: The Royal Australian College of General Practitioners and Diabetes Australia. Available at: https://www.diabetesaustralia.com.au/PageFiles/763/UPdated%20GP%20guidelines.pdf Accessed November 10, 2014. [Google Scholar]
- 14.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015 a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015; 38:140–149. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed October 21, 2014.]. Type 2 Diabetes: The Management of Type 2 Diabetes (NICE Clinical Guideline 87). National Institute for Health and Care Excellence [updated July 2014]. Available at: https://www.nice.org.uk/guidance/cg87. [Google Scholar]
- 16.van Berlo-van de Laar IR, Vermeij CG, Doorenbos CJ. Metformin associated lactic acidosis: incidence and clinical correlation with metformin serum concentration measurements. J Clin Pharm Ther 2011; 36:376–382. [DOI] [PubMed] [Google Scholar]
- 17.Brown JB, Pedula K, Barzilay J, et al. Lactic acidosis rates in type 2 diabetes. Diabetes Care 1998; 21:1659–1663. [DOI] [PubMed] [Google Scholar]
- 18.Bodmer M, Meier C, Krahenbuhl S, et al. Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis. Diabetes Care 2008; 31:2086–2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biradar V, Moran JL, Peake SL, et al. Metformin-associated lactic acidosis (MALA): clinical profile and outcomes in patients admitted to the intensive care unit. Crit Care Resusc 2010; 12:191–195. [PubMed] [Google Scholar]
- 20.Kim MJ, Han JY, Shin JY, et al. Metformin-associated lactic acidosis: predisposing factors and outcome. Endocrinol Metab (Seoul) 2015; 30:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang W, Castelino RL, Peterson GM. Metformin usage in type 2 diabetes mellitus: are safety guidelines adhered to? Intern Med J 2014; 44:266–272. [DOI] [PubMed] [Google Scholar]
- 22.Emslie-Smith AM, Boyle DI, Evans JM, et al. Collaboration DM Contraindications to metformin therapy in patients with Type 2 diabetes: a population-based study of adherence to prescribing guidelines. Diabet Med 2001; 18:483–488. [DOI] [PubMed] [Google Scholar]
- 23.Flory JH, Hennessy S. Metformin use reduction in mild to moderate renal impairment: possible inappropriate curbing of use based on food and drug administration contraindications. JAMA Intern Med 2015; 175:458–459. [DOI] [PubMed] [Google Scholar]
- 24.Frid A, Sterner GN, Londahl M, et al. Novel assay of metformin levels in patients with type 2 diabetes and varying levels of renal function: clinical recommendations. Diabetes Care 2010; 33:1291–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moioli A, Maresca B, Manzione A, et al. Metformin associated lactic acidosis (MALA): clinical profiling and management. J Nephrol 2016; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Inzucchi SE, Lipska KJ, Mayo H, et al. Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA 2014; 312:2668–2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scott KA, Martin JH, Inder WJ. Acidosis in the hospital setting: is metformin a common precipitant? Intern Med J 2010; 40:342–346. [DOI] [PubMed] [Google Scholar]
- 28.Renda F, Mura P, Finco G, et al. Metformin-associated lactic acidosis requiring hospitalization. A national 10 year survey and a systematic literature review. Eur Rev Med Pharmacol Sci 2013; 17 (Suppl 1):45–49. [PubMed] [Google Scholar]
- 29.Kajbaf F, Lalau JD. Mortality rate in so-called “metformin-associated lactic acidosis”: a review of the data since the 1960 s. Pharmacoepidem Dr S 2014; 23:1123–1127. [DOI] [PubMed] [Google Scholar]


