Abstract
Radiographic features of consecutive lumbar spondylolisthesis were retrospectively analyzed in a total of 17 patients treated for this condition at the Third Hospital of Hebei Medical University from June 2005 to March 2012.
To investigate the radiographic features, pelvic compensatory mechanisms, and possible underlying etiologies of consecutive lumbar spondylolisthesis.
To the best of our knowledge, there is no previous report concerning the characteristics of consecutive lumbar spondylolisthesis.
The Taillard index and the lumbar lordosis (LL), pelvic incidence (PI), sacrum slope (SS), and pelvic tilt (PT) were determined on lateral X-ray images, and the angular displacement was analyzed on flexion–extension X-ray images. Correlation between LL and various pelvic parameters and correlation between Taillard index and angular displacement were assessed by Pearson correlation analysis.
A total of 20 cases of isthmic spondylolisthesis and 14 of degenerative spondylolisthesis were retrospectively studied in 17 patients. The Taillard index and the angular displacement in the lower vertebrae were both larger than those in the upper vertebrae. Statistical analysis revealed that LL was correlated with PI and PT, whereas PI was correlated with PT and SS. However, no correlation was identified between Taillard index and angular displacement.
In consecutive lumbar spondylolisthesis, the degree of vertebral slip and the angular displacement of the lower vertebrae were both greater than those of the upper vertebrae, indicating that the compensatory mechanism of the pelvis plays an important role in maintaining sagittal balance.
Keywords: angular displacement, consecutive lumbar spondylolisthesis, pelvic sagittal parameters, Taillard index
1. Introduction
Lumbar spondylolisthesis is a common condition treated by spinal surgery.[1–3] It is usually due to congenital dysplasia, trauma, strain, or other causes of abnormalities in the bony connection between adjacent vertebrae, leading to partial or complete slippage of one vertebrae on adjacent vertebrae.[4,5] It is noteworthy that it rarely causes unilateral pedicle stress fracture. The typical symptoms of this condition are neurological deficits, including low back pain, nerve root irritation, and neural dysfunctions. The most common types of this entity are isthmic and degenerative spondylolisthesis. A variety of surgical fusion techniques, such as anterior interbody fusion, posterior interbody fusion, posterolateral fusion, repair of the pars interarticularis, and reduction and fusion have been applied to stabilize the spine, relieve pain, and improve the patients’ life quality.[6,7]
Spondylolisthesis is most common in middle-aged women, affecting mainly L4–L5.[8–10] Etiologies of spondylolisthesis include bilateral spondylolisthesis, spondylolysis, and interbody chronic dislocation. Radiological investigation is the key component of evaluation of lumbar spondylolisthesis to determine its anatomical abnormalities, etiologies, severity, and possible pathogenic mechanisms to guide the clinical management and assess the prognosis. For this purpose, a number of X-ray, CT, and MRI techniques have been employed to analyze anatomy of vertebrae, lumbar lordosis (LL), and the facet joints associated with the occurrence of slippage.[11–14] In contrast to the abundant radiological data on spondylolisthesis of single vertebral bodies, data for consecutive lumbar spondylolisthesis are absent, although multilevel lumbar spondylolisthesis does occur and accounts for up to 11% of spondylolisthesis. Importantly, multilevel segmental involvement is of considerable significance for the occurrence of cauda equina syndrome.[15]
Herein, we report our results on the radiological features of consecutive spondylolisthesis. We identified a correlation between the forward displacement of the involved vertebrae and pelvic sagittal parameters. Our findings suggest that pelvic compensatory mechanisms play a role in maintaining the overall sagittal spinal and pelvic stability.
2. Materials and methods
2.1. Study subjects
A total of 967 patients were diagnosed with and treated for spondylolisthesis at our hospital from June 2005 to March 2012. Among them, 17 consecutive spondylolisthesis cases (1.75%) were identified in 5 males and 12 females with a median age of 56 years. Out of these 17 patients, 7 had spondylolisthesis involving L3–L4, and 10 had spondylolisthesis involving L4–L5.
The enrollment criteria for these patients were as follows: No spinal fractures, or scoliosis history; no history of spinal surgery; diagnosis of consecutive spondylolisthesis on a lateral lumbar spine X-ray.
2.2. Radiological assessment
The lateral X-ray images for individual patients were retrieved from our Picture Archiving and Communication Systems (PACS). The Taillard index was defined as the relative displacement distance between the involved vertebrae divided by the horizontal length of the upper vertebral body (Fig. 1). The LL was the angle between the L1 endplate and S1 endplate. The pelvic incidence (PI) was denoted as the angle between the vertical line of S1 endplate and the line connecting midpoint of S1 endplate to midpoint of the femoral heads. The sacrum slope (SS) was defined as the angle between the S1 endplate and the horizontal line, while the pelvic tilt (PT) was the angle formed by the vertical line and the line connecting the midpoint of S1 endplate to the midpoint of the femoral heads (Fig. 2). The displacement between the upper and lower intervertebral space was determined on flexion–extension dynamic X-ray radiographs (Fig. 3).
Figure 1.
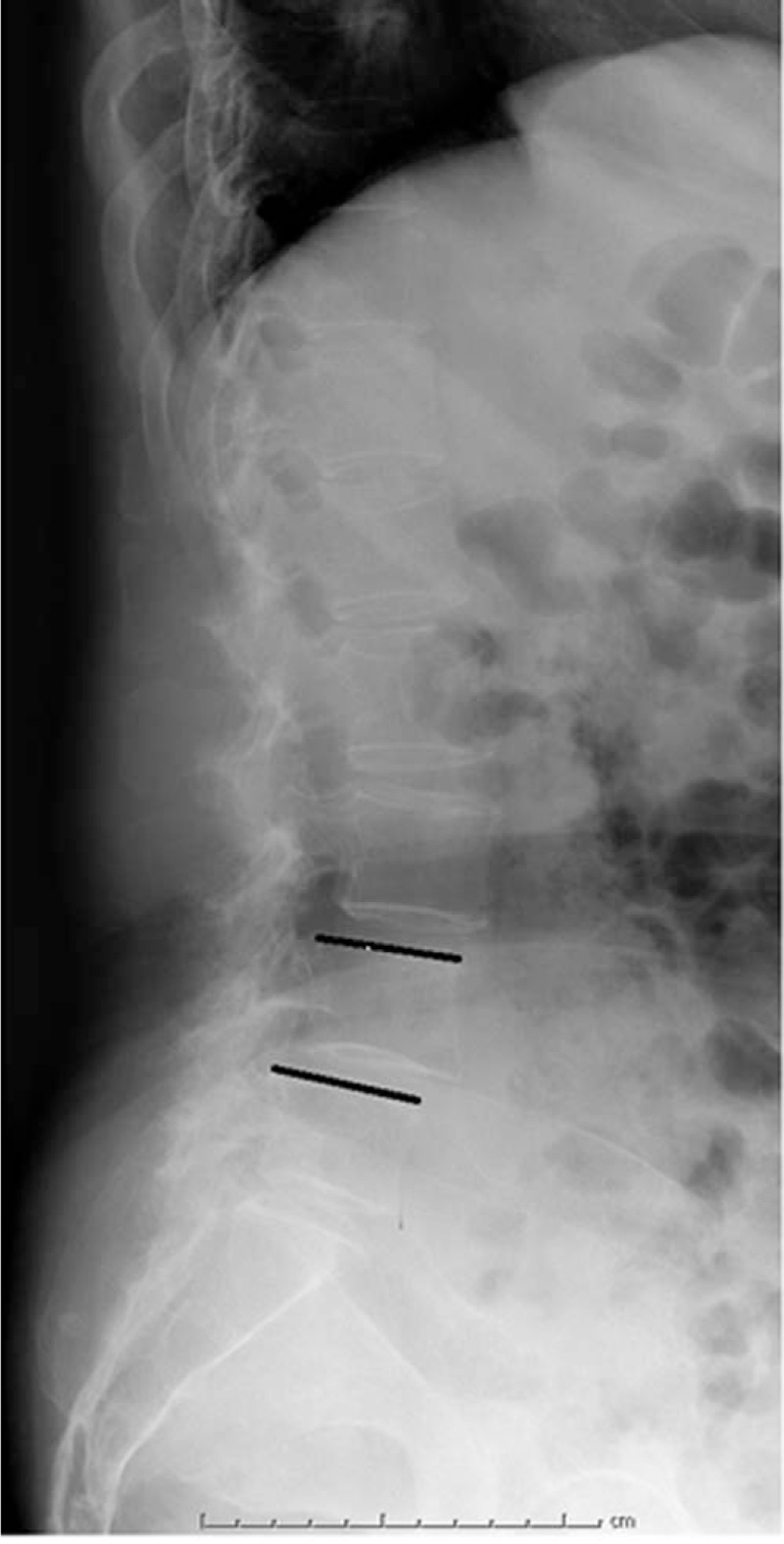
The measurement of Taillard index: the forward displacement distance of upper vertebral body/the length of the upper vertebral body × 100%.
Figure 2.
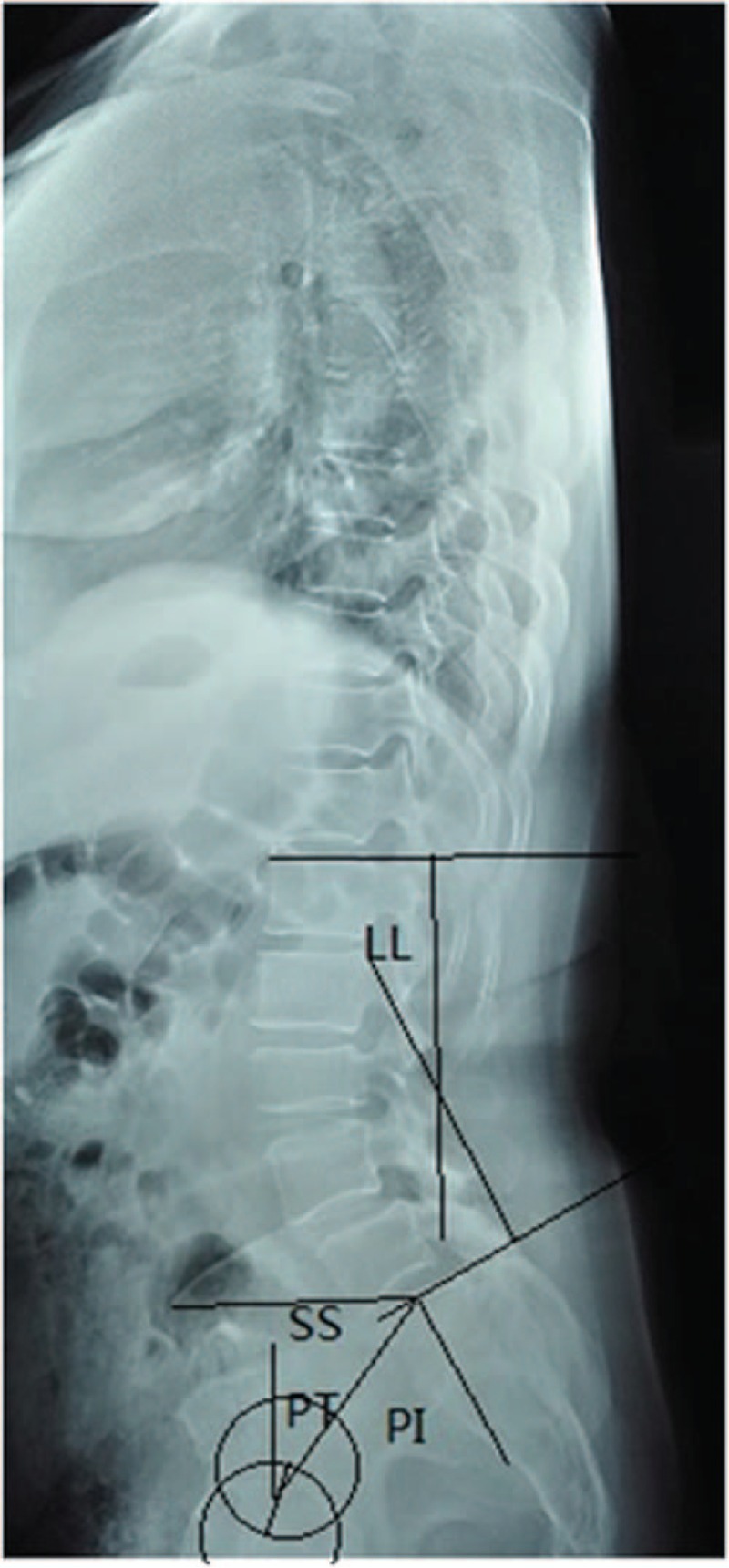
The measurement of the lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), and sacrum slope (SS).
Figure 3.

The measurement of the angular displacement on flexion–extension X-ray. The angular displacement of the upper intervertebral space was calculated as (a1–b1); the angular displacement of lower intervertebral space was determined by calculating (a2–b2).
2.3. Statistical analysis
The data were analyzed with SPSS13.0. Student t test was used to analyze the relative anterior displacement of the vertebrae and the angular displacement of the intervertebral spaces. Pearson correlation analysis was applied to investigate the correlation between LL and pelvic sagittal parameters and the correlation between Taillard index and angular displacements. P < 0.05 was considered statistically significant.
2.4. Ethical review
This study was approved by the Ethical Committee of the Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, China.
3. Results
Twenty isthmic (upper and lower vertebrae) and 14 (upper and lower vertebrae) degenerative consecutive spondylolisthesis were identified in 34 vertebral bodies in 17 patients (Table 1). Among the above mentioned 7 patients with L3–L4 consecutive spondylolisthesis. Out of the 10 patients with consecutive spondylolisthesis, 7 were with isthmic and 3 with degenerative spondylolisthesis (Fig. 1).
Table 1.
The type of lumbar spondylolisthesis.
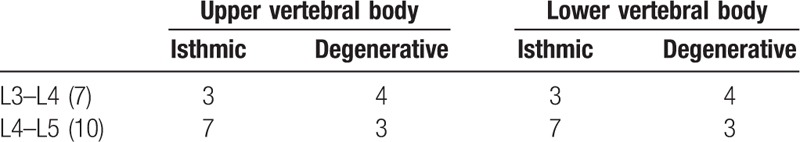
The average Taillard index of the upper vertebrae was 17.6 ± 4.1%, whereas its value for the lower vertebrae was 22.4 ± 4.1% (t = 7.672, P < 0.001). The average angular displacement of the upper vertebrae was 10.8 ± 2.6°, whereas that of the lower vertebrae was 18.6 ± 5.5° (t = 5.251, P < 0.001).
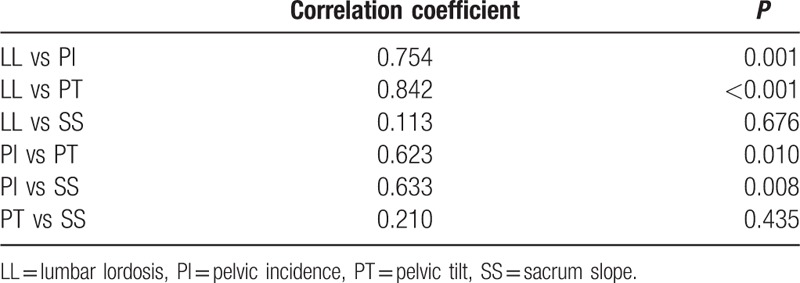
In the 17 patients, the average LL was 58.1 ± 4.3°, the average PI 68.7 ± 4.8°, the average SS 37.2 ± 3.8°, and the average PT 31.6 ± 4.0°. A correlation between LL and PI and PT was identified, while PI was correlated with PT and SS (Table 2). In contrast, no correlation was present between Taillard index and the angular displacement (P > 0.05).
Table 2.
Correlation between LL and the pelvic parameters.
4. Discussion
Spondylolisthesis has a range of causes. For example, isthmus crack spondylolisthesis can be due to a congenital isthmus defect, an acute lumbar trauma leading to an isthmus fracture, stress-related fractures caused by chronic fatigue on the basis of congenital isthmus dysplasia. This condition is commonly detected in the 5th lumbar vertebral body in 30- to 40-year-old adults, as males and females are affected approximately equally. On the other hand, degenerative spondylolisthesis is usually secondary to intervertebral disc degeneration and commonly affects L4–L5 in 50- to 60-year-old women.[4,5,10] Although the diverse causative factors usually lead to single-level spondylolisthesis, we found that consecutive spondylolisthesis is not a rare condition, especially in individuals performing long-term heavy physical labor, such as the subjects enrolled in the present study. We also discovered that pelvic compensation mechanisms play a key role in maintaining the overall sagittal spinal and pelvic stability in this condition. To the best of our knowledge, this is the first radiographic report regarding the biomechanical features of consecutive spondylolisthesis.
Due to its distinct anatomical nature, isthmic spondylolisthesis is considered to be inherently more instable than degenerative spondylolisthesis, a fact reflected by the difference in the angular displacement existing between these 2 types.[15–17] In the present study, identical types of spondylolisthesis in the 2 levels of vertebrae were present in each individual. Therefore, we believe that the effects exerted by the type of spondylolisthesis on angle displacement were minimal in the studied patients.
Interbody gravity force is transmitted and divided into a compression force perpendicular to the shift force that is parallel to the vertebral endplates.[18] In general, lower vertebral bodies bear greater shearing forces with respect to the upper vertebrae, which can accelerate intervertebral degeneration in the disc and facet joints. Consequently, from an anatomical standpoint, the range of movement in the discs that are closer to the lumbosacral region is greater than that in those located away from the lumbosacral region. In line with this mechanism, we found that the angular displacement in the lower vertebral bodies was much more prominent than that in the upper vertebrae in the clinical setting of consecutive spondylolisthesis.
It is worth noting that the antishearing force mechanisms are compromised in lumbar spondylolisthesis.[19–21] To compensate for this defect, a series of compensatory changes are realized in the spine–pelvis sequence to adapt and maintain a stable standing position.[22–24] These adaptive changes are usually reflected by the alteration of spine–pelvis sagittal parameters, such as PI. A number of studies have shown that the extent of increase of PI values in patients with single-level lumbar spondylolisthesis is positively correlated with the severity of displacement of the involved vertebrae.[21,24] Barrey et al[25] has further suggested that PI value is to some extent predictive for displacement of affected vertebrae in 1-level spondylolisthesis. We calculated the PI values in 2-level spondylolisthesis and found that the average PI value in consecutive spondylolisthesis was higher than the reported ones in single-level segment spondylolisthesis (68.7° vs 66.3°),[26] and not surprisingly either, higher than that in healthy individuals.[26,27] We postulated that the high PI values in consecutive spondylolisthesis might be a risk factor for displacement of the affected vertebrae. Nevertheless, to evaluate the biomechanical relevance of an increased PI value in spondylolisthesis requires further prospective studies.
Berthonnaud et al[28] proposed the hinged concept of connection from head to pelvis. Any change in orientation within an anatomical spine segment will cause adaptive changes in adjacent segments in order to maintain the stability of the body. For example, Vialle et al[29] have reported that SS values in single-vertebral lumbar spondylolisthesis gradually increase along with the degree of displacement in spondylolisthesis grade I–III, but decrease in grades IV–V. Although our results clearly demonstrated that consecutive spondylolisthesis resulted in a modification of pelvic parameters, our data indicated that the values of SS (37.2°) and PT (31.6°) in patients with consecutive spondylolisthesis were higher than those observed in the healthy population (PT = 25.1° and SS = 30.7°)[29–31] in the same age group. In the present study, all the Taillard indexes were below 50%, classifying the grade of spondylolisthesis as I or II. We hypothesize, that the compensatory mechanisms in the spine–pelvis sequence in 2-segment spondylolisthesis might be different from that in 1-level spondylolisthesis. Another set of data supporting this notion was the failure of identification of the existence of a significant correlation between PT and SS, which was compatible with the reported finding indicating that PI = SS + PT, and there are opposite trend shifts of PT and SS in spondylolisthesis.[32–34] This discrepancy could be due to two reasons. First, consecutive spondylolisthesis may cause a distinct pelvic–spine compensation which leads to a discordant change in PT and SS. Second, the small sample size and selection bias in the present study might have led to the occurrence of this discrepancy.
As a limitation of the current investigation, we have to point out that the data collected in the present study are derived from X-ray images only. Since whole-spine imaging was not employed, we were unable to conduct an analysis of the whole-spine sequence.
In summary, our study showed that in the spondylolisthesis of 2 adjacent lumbar segments both the degree of the vertebral slip and the angular displacement of the lower vertebrae were greater, than those of the upper vertebrae, indicating that the compensatory mechanism of the pelvis plays an important role in maintaining the sagittal balance.
Footnotes
Abbreviations: LL = lumbar lordosis, PACS = Picture Archiving and Communication Systems, PI = pelvic incidence, PT = pelvic tilt, SS = sacrum slope.
YS and HW contributed equally to this work.
Funding: This research was funded by the Hebei Medical Science Research Key Project, instructional topics (20160600).
The authors have no conflicts of interest to disclose.
References
- 1.Raastad J, Reiman M, Coeytaux R, et al. The association between lumbar spine radiographic features and low back pain: a systematic review and meta-analysis. Semin Arthritis Rheum 2015; 44:571–585. [DOI] [PubMed] [Google Scholar]
- 2.Nakayama T, Ehara S. Spondylolytic spondylolisthesis: various imaging features and natural courses. Jpn J Radiol 2015; 33:3–12. [DOI] [PubMed] [Google Scholar]
- 3.Brown MD, Lockwood JM. Degenerative spondylolisthesis. Instr Course Lect 1983; 32:162–169. [PubMed] [Google Scholar]
- 4.Butt S, Saifuddin A. The imaging of lumbar spondylolisthesis. Clin Radiol 2005; 60:533–546. [DOI] [PubMed] [Google Scholar]
- 5.Herkowitz HN. Spine update. Degenerative lumbar spondylolisthesis. Spine 1995; 20:1084–1090. [DOI] [PubMed] [Google Scholar]
- 6.Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. J Am Acad Orthop Surg 2014; 22:203–213. [DOI] [PubMed] [Google Scholar]
- 7.Clark JC, Jasmer G, Marciano FF, et al. Minimally invasive transforaminal lumbar interbody fusions and fluoroscopy: a low-dose protocol to minimize ionizing radiation. Neurosurg Focus 2013; 35:E8. [DOI] [PubMed] [Google Scholar]
- 8.Gille O, Challier V, Parent H, et al. Degenerative lumbar spondylolisthesis: cohort of 670 patients, and proposal of a new classification. Orthop Traumatol Surg Res 2014; 100 (6 suppl):S311–S315. [DOI] [PubMed] [Google Scholar]
- 9.DeWald CJ, Vartabedian JE, Rodts MF, et al. Evaluation and management of high-grade spondylolisthesis in adults. Spine 2005; 30 (6 suppl):S49–S59. [DOI] [PubMed] [Google Scholar]
- 10.Kornblum MB, Fischgrund JS, Herkowitz HN, et al. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine 2004; 29:726–733.discussion 733–734. [DOI] [PubMed] [Google Scholar]
- 11.Sato J, Ohtori S, Orita S, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 2015. [DOI] [PubMed] [Google Scholar]
- 12.Schmid R, Reinhold M, Blauth M. Lumbosacral dislocation: a review of the literature and current aspects of management. Injury 2010; 41:321–328. [DOI] [PubMed] [Google Scholar]
- 13.Schinnerer KA, Katz LD, Grauer JN. MR findings of exaggerated fluid in facet joints predicts instability. J Spinal Disord Tech 2008; 21:468–472. [DOI] [PubMed] [Google Scholar]
- 14.Krupski W, Majcher P. Radiological diagnostic of lumbar spondylolysis. Ortop Traumatol Rehabil 2004; 6:809–818. [PubMed] [Google Scholar]
- 15.Omidi-Kashani F, Hasankhani EG, Rahimi MD, et al. Comparison of functional outcomes following surgical decompression and posterolateral instrumented fusion in single level low grade lumbar degenerative versus isthmic spondylolisthesis. Clin Orthop Surg 2014; 6:185–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okuda S, Oda T, Yamasaki R, et al. Posterior lumbar interbody fusion with total facetectomy for low-dysplastic isthmic spondylolisthesis: effects of slip reduction on surgical outcomes: clinical article. J Neurosurg Spine 2014; 21:171–178. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Zhou Y, Zhang ZF, et al. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J 2010; 19:1780–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ye YP, Chen D, Xu H. The comparison of instrumented and non-instrumented fusion in the treatment of lumbar spondylolisthesis: a meta-analysis. Eur Spine J 2014; 23:1918–1926. [DOI] [PubMed] [Google Scholar]
- 19.Matsukawa K, Yato Y, Imabayashi H, et al. Biomechanical evaluation of lumbar pedicle screws in spondylolytic vertebrae: comparison of fixation strength between the traditional trajectory and a cortical bone trajectory. J Neurosurg Spine 2016; 24:1–6. [DOI] [PubMed] [Google Scholar]
- 20.Bjarke Christensen F, Stender Hansen E, Laursen M, et al. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with a 5-year follow-up. Spine 2002; 27:1269–1277. [DOI] [PubMed] [Google Scholar]
- 21.Hresko MT, Labelle H, Roussouly P, et al. Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine 2007; 32:2208–2213. [DOI] [PubMed] [Google Scholar]
- 22.Zencica P, Chaloupka R, Hladikova J, et al. [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. Acta Chir Orthop Traumatol Cech 2010; 77:124–130. [PubMed] [Google Scholar]
- 23.Axelsson P, Johnsson R, Stromqvist B. Is there increased intervertebral mobility in isthmic adult spondylolisthesis? A matched comparative study using roentgen stereophotogrammetry. Spine 2000; 25:1701–1703. [DOI] [PubMed] [Google Scholar]
- 24.Lim JK, Kim SM. Difference of sagittal spinopelvic alignments between degenerative spondylolisthesis and isthmic spondylolisthesis. J Korean Neurosurg Soc 2013; 53:96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barrey C, Jund J, Noseda O, et al. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 2007; 16:1459–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajnics P, Templier A, Skalli W, et al. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech 2002; 15:24–30. [DOI] [PubMed] [Google Scholar]
- 27.Funao H, Tsuji T, Hosogane N, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J 2012; 21:2181–2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berthonnaud E, Dimnet J, Roussouly P, et al. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 2005; 18:40–47. [DOI] [PubMed] [Google Scholar]
- 29.Vialle R, Ilharreborde B, Dauzac C, et al. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J 2007; 16:1641–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vialle R, Ilharreborde B, Dauzac C, et al. Intra and inter-observer reliability of determining degree of pelvic incidence in high-grade spondylolisthesis using a computer assisted method. Eur Spine J 2006; 15:1449–1453. [DOI] [PubMed] [Google Scholar]
- 31.Morel E, Ilharreborde B, Lenoir T, et al. [Sagittal balance of the spine and degenerative spondylolisthesis]. Rev Chir Orthop Reparatrice Appar Mot 2005; 91:615–626. [DOI] [PubMed] [Google Scholar]
- 32.Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J 2011; 20 (suppl 5):641–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaleat-Valayer E, Mac-Thiong JM, Paquet J, et al. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J 2011; 20 (suppl 5):634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mac-Thiong JM, Roussouly P, Berthonnaud E, et al. Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine 2010; 35:E1193–E1198. [DOI] [PubMed] [Google Scholar]


