Supplemental Digital Content is available in the text
Keywords: China, cohort study, diabetes, fasting glucose, impaired fasting glucose, incidence, obesity
Abstract
The worldwide prevalence and incidence of diabetes and obesity are increasing in pandemic proportions. This is particularly relevant for China, where an extremely large population is growing, aging, and urbanizing. We thus conducted a prospective study to examine the prevalence and incidence of impaired fasting glucose (IFG) and diabetes, the rate at which fasting blood glucose rises, and the major modifiable risk factors associated with these outcomes in a large Chinese population from the Kailuan prospective study.
A prospective cohort included 100,279 Chinese participants, aged 18 years or more, who had available information on fasting blood glucose concentrations at the start of the study (2006). Examination surveys were conducted every 2 years in 2008 and 2010. For the analyses of incident diabetes, we included 76,869 participants who were free of diabetes, cardiovascular disease, and cancer at the baseline and participants in the 2008 and/or 2010 follow-up. Diabetes was defined by a fasting blood glucose concentration ≥7 mmol/L, self-reported history, or active treatment with insulin or any oral hypoglycemic agent. IFG was defined by a fasting blood glucose concentration between 5.6 and 6.9 mmol/L.
During the 4-year study, the prevalence of diabetes and IFG rose from 6.6% to 7.7%, and 17.3% to 22.6%, respectively. There were 17,811 incident cases of IFG and 4867 incident cases of diabetes. The age-standardized incident rate of IFG and diabetes were 62.6/1000 person-years (51.2/1000 person-years in women and 73.8/1000 person-years in men) and 10.0/1000 person-years (7.8/1000 person-years in women and 12.1/1000 person-years in men), respectively. We observed steady increases in fasting blood glucose with body anthropometrics and in every defined category of body mass index, including in those traditionally considered to be well within the “normal” range.
In this large longitudinal study of Chinese adults, we observed a high prevalence and incidence of IFG and diabetes over 4 years of follow-up. Our findings are alarming for Chinese public health since steady rises in fasting blood glucose were seen across all permutations of body habitus, even apparently very lean individuals.
1. Introduction
The worldwide prevalence and incidence of chronic noncommunicable diseases, particularly diabetes and obesity, are increasing in pandemic proportions.[1] South and southeast Asian countries are predicted to represent a disproportionately large burden of the global incidence of diabetes. This is particularly relevant for China, where an extremely large population is growing, aging, and urbanizing. The epidemiologic forecast predicts that the prevalence of diabetes in China will double between 2000 and 2030.[1,2] Perhaps more alarming is the fact that the prevalence of prediabetes cases is expected to be several fold higher than the number of diabetes cases, thereby dramatically magnifying the pool of at-risk individuals.[3]
The ramifications of uncontrolled increases in adiposity and consequent increases in the incidence of impaired fasting glucose (IFG) and diabetes in China are expected to be disastrous: higher body mass index (BMI) and impaired glycemic control contribute to micro- and macrovascular complications[4] and predict mortality.[5,6] Addressing the epidemic of diabetes and diabetes-associated complications has been identified as a public policy priority for China to reduce death, disability, and improve quality of life measures.[7] A failure to address these outcomes may have immeasurable effects on China's domestic economy, and global economies, by influencing human health and healthcare allocations.
Fortunately, interventions to modify risk factors that result in impaired glycemic control and diabetes have shown the potential for success by mitigating the incidence of diabetes in the United States[8] and in China.[9] In order for large-scale public health initiatives in China to better identify populations at risk for developing IFG and diabetes, and institute measures to halt their progression, an improved understanding of the incidence of IFG and diabetes as well as the associated modifiable risk factors is needed. In particular, since progressive increases in fasting blood glucose can predict impending IFG and diabetes, identifying factors that contribute to rising blood glucose over time may help target interventions. With Chinese public health policies in mind, we aimed to identify the prevalence and incidence of IFG and diabetes, the rate at which fasting blood glucose rises, and the major modifiable risk factors associated with these outcomes in a large Chinese population from the Kailuan prospective study.
2. Materials and methods
2.1. Study design and population
The Kailuan study is a prospective cohort study based in the Kailuan community (a large population of employees of the Kailuan coal mining company), in the city of Tangshan, a large modern city southeast of Beijing.[10,11] From June 2006 to October 2007, all 155,418 employees aged 18 years or more (including the retired) of the Kailuan Company were invited to participate. A total of 101,510 participants (81,110 men and 20,400 women, aged 18–98 years) agreed to participate and were enrolled after written informed consent was obtained. There were no major demographic differences between those who agreed to participate in the study and those who declined to participate, except for a small variation in sex distribution, as previously described.[11]
Our present study includes data and longitudinal follow-up of these participants over 4 years (2006–2010), where surveys were conducted every 2 years (2006, 2008, and 2010). The main analytic aims of this report include determination of the prevalence and incidence of diabetes in participants across the 4-year period, determination of the prevalence and incidence of IFG during the 4-year period, and identifying modifiable variables that may contribute to incident diabetes and IFG in this population.
2.2. Ethical review
The study was approved by the Ethics Committee of the Kailuan General Hospital and Brigham and Women's Hospital in Boston.
2.3. Assessment of the prevalence and incidence of IFG and diabetes
For IFG and diabetes prevalence calculations, we included the 100,279 participants who had available information on fasting blood glucose concentrations. To calculate the true incident diabetes rate, we excluded participants who had diabetes (n = 9486) and those who did not participate in the 2008 or 2010 surveys (n = 13,228). Participants who did not follow-up on subsequent exams were older and more likely to be women and had lower educational level and higher prevalence of hypertension and family history of diabetes (eTable 1). Because of the risk that a prior diagnosis of, or active treatment for, cancer and cardiovascular disease (CVD) could influence current glycemic control, we further excluded individuals with a history of cancer and CVD (n = 693) to establish a study population of 60,189 men and 16,680 women (n = 76,869) for the analyses of incident diabetes. Diabetes was defined by a self-reported history, active treatment with insulin or any oral hypoglycemic agent, or a fasting blood glucose concentration ≥7.0 mmol/L. To calculate the true incidence of IFG, we further excluded 18,055 participants who had IFG at baseline in 2006, leaving 58,814 participants (44,904 men and 13,910 women) for the incident IFG analyses. IFG was defined by a fasting blood glucose concentration between 5.6 and 6.9 mmol/L. Participant inclusion is detailed in eFigure 1.
2.4. Blood sampling
Fasting blood samples were collected at baseline in 2006 and again in 2008 and 2010 from the antecubital vein after an 8- to 12-hour overnight fast in vacuum tubes containing ethylene diamine tetraacetic acid. Fasting blood glucose concentrations in each survey were measured with the hexokinase/glucose-6-phosphate dehydrogenase method. The same assay was used on all participants at baseline in 2006 and at each follow-up examination in 2008 and 2010. The coefficient of variation using blind quality control specimens was <2.0%.
2.5. Assessment of potential exposures and covariates
Weight and height were measured by trained field workers during the interview, and BMI was calculated as weight (kg)/height (m2). Waist circumference (WC) was measured with a nonstretchable tape held at the level of the naval while standing without clothing. We measured hip circumference at the level of the maximal protrusion of the gluteal muscles (hips). The position was verified by passing the tape measure above and below the observed maximum. Waist-to-hip ratio (WHR) was calculated as WC (cm)/hip (cm).
Systolic blood pressure (SBP) and diastolic blood pressure were measured twice from the seated position using a mercury sphygmomanometer. The average of the 2 readings was used for the analyses. Information on potential confounders, such as age; sex; educational level; average income of each family member; and family history of diabetes, smoking, alcohol intake, physical activity, and work environment was collected via questionnaires in 2006 and updated every 2 years, as detailed in online text.
Information on smoking, alcohol intake, physical activity, and work environment was collected using questionnaires. Physical activity was evaluated from responses to questions regarding the frequency of physical activity (20+ minutes per time) during leisure time, with the possible responses including never, sometimes, and 4+ times per week. Smoking status was classified using self-reported information as “never”, “past, 1–19 cigarettes/d”, “past, 20+ cigarettes/d”, “current, 1–19 cigarettes/d”, or “current, 20+ cigarettes/d”. Alcohol intake was classified using self-reported frequency as “never”, “past”, “current, <1 time/d”, or “current, 1+ times/d”. The possible responses for work environment included “working on the ground”, “working underground without exposure to dust”, or “working underground with exposure to dust”, where the latter 2 choices reflect that minority of the population that was actively involved in underground coal mining–related work and may or may not have had direct inhalational or contact exposures that could be of potential relevance.
2.6. Statistical analyses
To compare our study and population with previous publications focused on the prevalence of diabetes in China, we calculated the standardized prevalence and incidence, which were weighted according to age distribution of the Chinese adult population aged 18 years or more, based on 2010 China population census data.[12] The prevalence of IFG and diabetes at each follow-up survey (2006, 2008, and 2010) was calculated as the cross-section of the number of cases divided by the total population in that year. Incident IFG and diabetes were defined at the first development of a fasting blood glucose value fulfilling this diagnosis. Person-year was calculated from the date the 2006 interview was conducted to the date of that either IFG or diabetes occurred (depending on the analysis in question), date of death, or the date of participating in the last interview in this analysis, whichever came first. Because there was no evidence of nonproportional hazards for major exposures, we used Cox proportional hazard models to assess the hazard ratio (HR) of IFG and diabetes during follow-up, according to baseline obesity (as assessed by BMI, WC, and WHR) status, adjusting for age, gender, educational level, family history of diabetes, physical activity, smoking status, alcohol intake, work environment, hypertension, and fasting blood glucose concentration. For those with missing information on 1 covariate, we used a “missing value indicator” in the analyses. The time scale for the left-truncated survival model was age (months), which was additionally stratified by calendar time in 2-year groups.
The relationship between obesity indices and repeated measures of rate of change in fasting glucose over the 4-year period was analyzed using a generalized estimating equation procedure in Statistical Analysis System (SAS). Different covariance models were compared based on quasilikelihood under the independence model criterion. The interaction term of BMI/WC with time was tested to determine effects of these obesity indices on the change in fasting glucose over time.
Because approximately 1/3 of the study participants worked underground in the coal mines, we also conducted a sensitivity analysis after excluding these participants (n = 23,836).
3. Results
3.1. Population characteristics
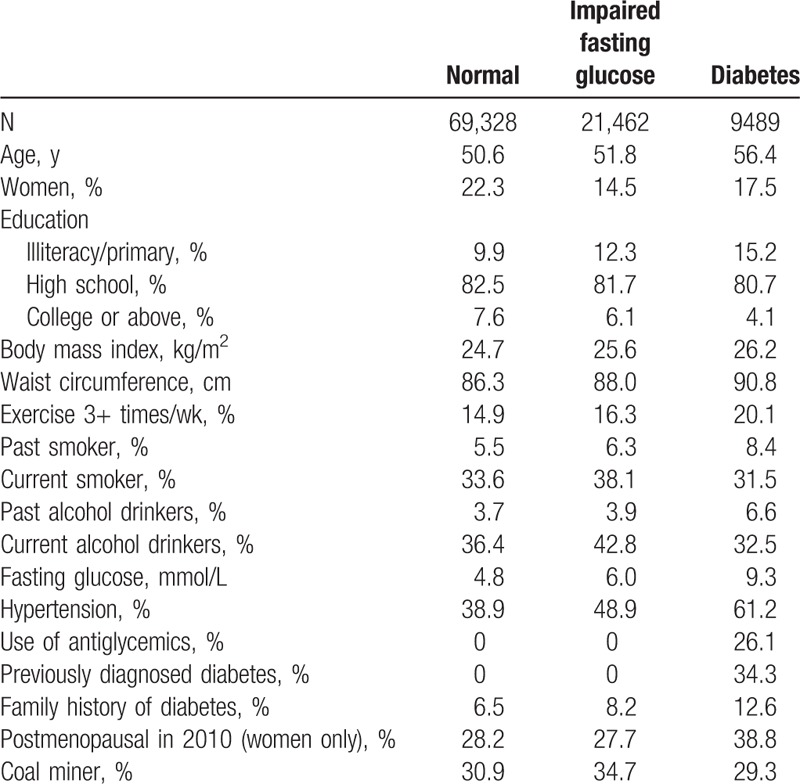
Individuals with diabetes or IFG, compared to those with normal fasting blood glucose, were more likely to have lower education, obesity, hypertension, and family history of diabetes (Table 1). Individuals with diabetes also tended to adopt a healthier lifestyle, such as frequent exercise and not smoking/alcohol drinking, although they were more likely to be past smokers and alcohol drinkers. Among individuals with diabetes at baseline, 34% were previously diagnosed and 26% were using antiglycemic medications.
Table 1.
Basic characteristics of participants of the Kailuan study, according to diabetes status in 2006.
3.2. Prevalence of IFG and diabetes
The age-standardized prevalence of IFG was 17.3% in 2006, 20.7% in 2008, and 22.6% in 2010, whereas the prevalence of diabetes was 6.6% in 2006, 7.6% in 2008, and 7.7% in 2010. The sex-specific prevalence of IFG and diabetes at baseline in 2006 and in subsequent surveys in 2008 and 2010 are shown in eFigure 2.
3.3. Incidence of IFG and diabetes
Between 2006 and 2010, we documented 17,811 incident cases of IFG and 4867 incident cases of diabetes. The age-standardized incident rate of IFG was 62.6/1000 person-years (51.2/1000 person-years in women and 73.8/1000 person-years in men; P difference for genders <0.001) and 26.3/1000 person-years when the World Health Organization (WHO) criteria was used.[13] The age-standardized incident rate of diabetes was 10.0/1000 person-years (7.8/1000 person-years in women and 12.1/1000 person-years in men; P difference for genders <0.001). The incident rates of IFG and diabetes increased with older age, and the gender differences disappeared among those aged 60 years or more (P > 0.10) (Fig. 1). Incident rates of IFG and diabetes by age and BMI categories are displayed in eTable 2. When we further included those with cancer and CVD, the incident rate increased to 75.6/1000 person-years for IFG and 13.9/1000 person-years for diabetes.
Figure 1.
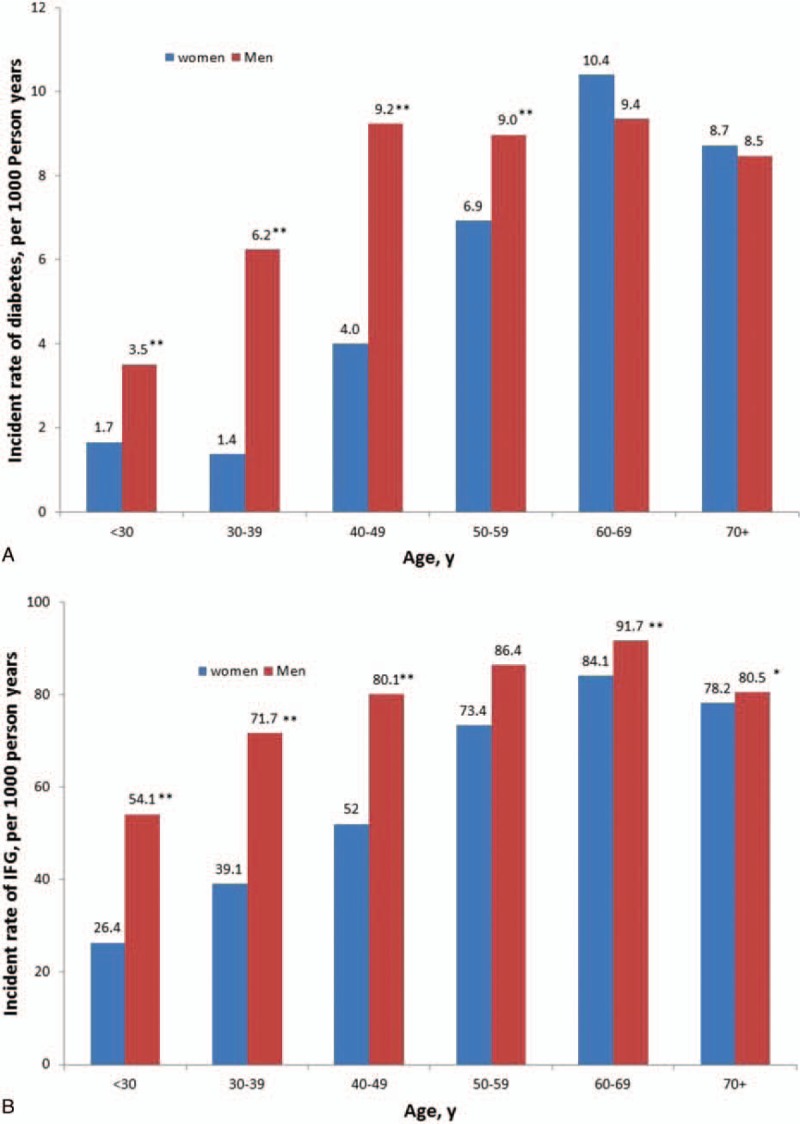
Incident rate (per 1000 person-year) of diabetes (panel A) and impaired fasting glucose (panel B) according to gender and baseline age in 2006. ∗P < 0.05, ∗∗P < 0.001, relative to women.
3.4. Major modifiable risk factors and the rate of change in fasting blood glucose
Because we observed significant interactions between gender and obesity indices (P interaction <0.001 for all), we presented results for men and women separately. Adiposity, as assessed by BMI, WC, and WHR, was associated with an increased risk of developing diabetes and IFG (Table 2 ) during 4-year prospective follow-up in both genders. Incident diabetes was also significantly predicted by physical inactivity, smoking, alcohol consumption, higher SBP, higher fasting blood glucose and triglycerides, and working underground with dust exposure (eTable 3).
Table 2.
Relative risk and 95% confidence intervals of diabetes and impaired fasting glucose according to obesity status in men and women in the Kailuan cohort.
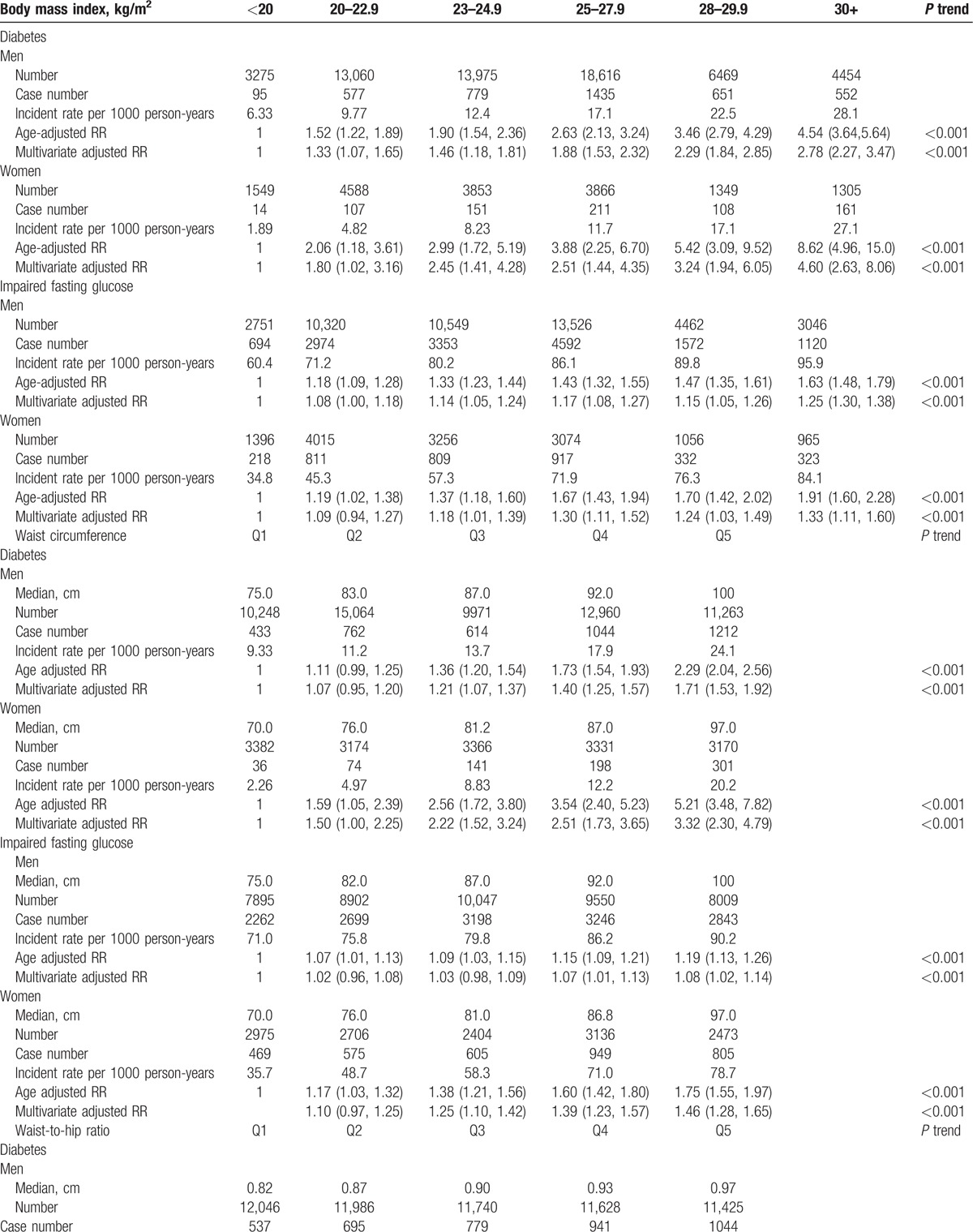
Table 2(Continious).
Relative risk and 95% confidence intervals of diabetes and impaired fasting glucose according to obesity status in men and women in the Kailuan cohort.
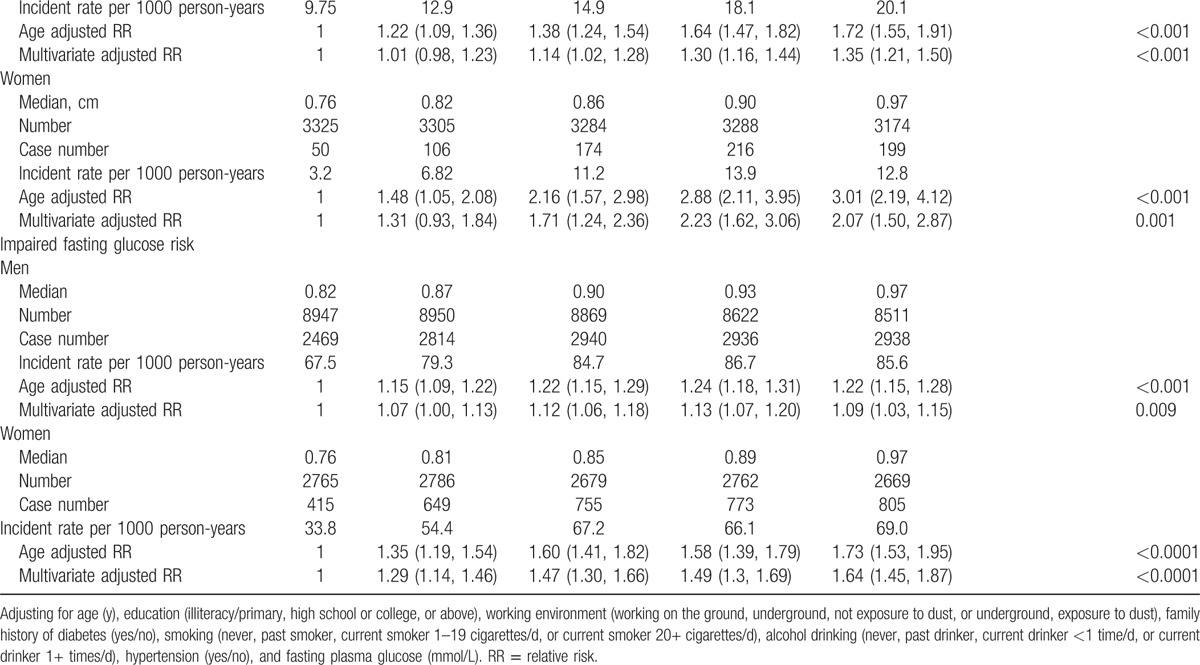
To better appreciate how body habitus contributes to the incidence of IFG and diabetes, we categorized BMI to approximately represent notable WHO cutoffs for Asian and non-Asian populations.[14] Although higher BMI was associated with faster increases in blood glucose concentrations (P < 0.0001 in both men and women), we observed steady increases in fasting blood glucose concentrations across each BMI category, including those traditionally considered to be well within the “normal” range (with BMI < 23 kg/m2) (Fig. 2). We further examined the prediction of IFG and diabetes as a function of body habitus as represented by BMI and WC and once again observed that even those with traditionally “normal” BMI and WC in non-Chinese populations displayed a significantly higher risk of developing IFG or diabetes with higher BMI and WC (Fig. 3, panels A–D). We observed similar patterns for the associations between BMI/WC and annual increase in fasting blood glucose over 4 years of follow-up in both men and women (eFigure 3).
Figure 2.
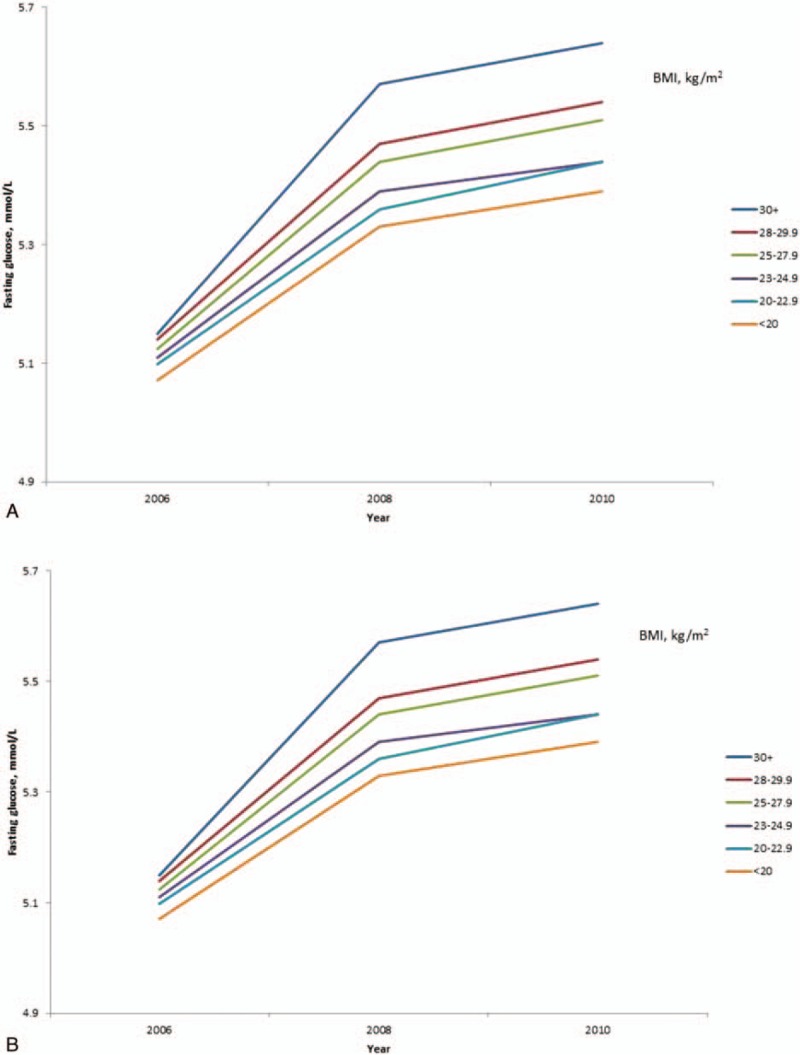
Change in fasting blood glucose concentrations between surveys according to baseline body mass index (BMI) among men (panel A) and women (panel B) without diabetes at the baseline. The interaction term of BMI with time was significant (P < 0.0001) for both men and women, suggesting that higher BMI was associated with a significantly faster increase in glucose over time.
Figure 3.
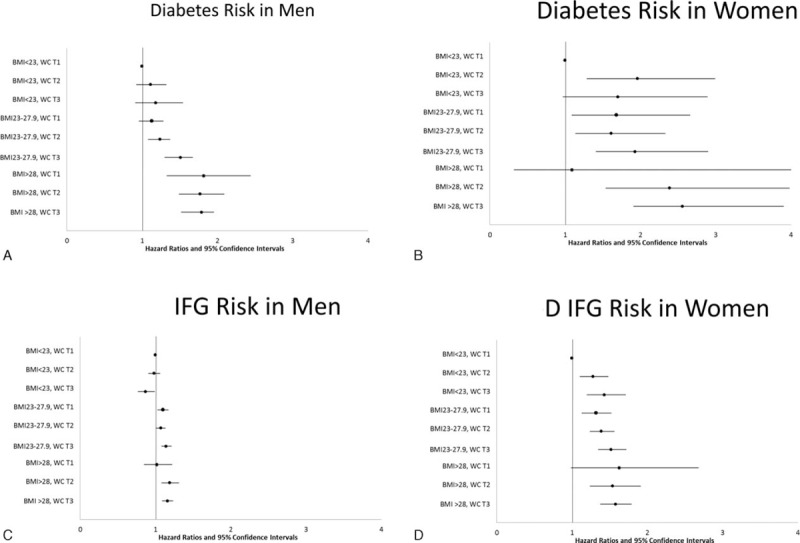
Hazard ratio of diabetes (panel A: men and B: women) and impaired fasting glucose (panel C: men and D: women) according to the joint classification of body mass index and waist circumference in men and women, adjusting for age (y), education (illiteracy/primary, high school or college, or above), working environment (working on the ground, underground, not exposure to dust, or underground, exposure to dust), family history of diabetes (yes/no), smoking (never, past smoker, current smoker 1–19 cigarettes/d, or current smoker 20+ cigarettes/d), alcohol drinking (never, past drinker, current drinker <1 time/d, or current drinker 1+ times/d), hypertension (yes/no), and fasting plasma glucose (mmol/L).
3.5. Sensitivity analyses to evaluate the influence of coal mining status
To evaluate whether our aforementioned findings could have been disproportionately confounded by those participants who worked underground in coal mines, we conducted sensitivity analyses after excluding all coal miners and observed similar results (eTable 4).
4. Discussion
As urbanization, population growth, and accompanying lifestyle changes continue in China, the incidence of prediabetes and diabetes is rapidly rising.[1] To our knowledge, our study represents the largest longitudinal study focused on assessing the prospective incidence of prediabetes and diabetes in China and highlights the steady rise in fasting blood glucose with time that is associated with modifiable risk factors such as body habitus.[7,15] Compared with the only prospective study of diabetes conducted in China in the 1980s,[16] our study findings indicate that the incident rate of diabetes has increased greatly during the past 3 decades. In 1993, Hu et al[16] described the age-standardized incident rate of diabetes in 36,471 men and women living in a northeastern Chinese city of 1.3/1000 person-years during 4 years of follow-up (1986–1990). Of note, in this study, diabetes was defined by a fasting plasma glucose concentration of greater than 7.77 mmol/L, and the incidence rate was age-standardized according to the 1982 population census data of China. If we were to have employed the same definition of diabetes in our present study, the incident rate of diabetes in the Kailuan cohort from 2006 to 2010 would be approximately 4.6/1000 person-years, still substantially higher than that reported from 1986 to 1990. More recently, smaller and shorter prospective studies reported similar incidence rates.[15,17] Our findings highlight the epidemic rise of impaired glycemic control and diabetes in China, underscoring the prior concerns by researchers and regulatory agencies.[1,2,7]
The interpretation and implications of our findings are best realized in the context of the 2 largest cross-sectional studies reporting on diabetes in China. Using a modality of tests to identify prevalent diabetes, including fasting blood glucose, oral glucose-tolerance tests, and fasting 2-hour glucose levels, Yang et al[18] reported that the prevalence of diabetes was 9.7% (10.6% in men and 8.8% in women), and prevalence of prediabetes was 15.5% (16.1% in men and 14.9% in women) in 2007 based on a sample of 46,239 nationally representative adults. In contrast to Yang et al, Xu et al[19] examined the prevalence of diabetes in China in 2010, using fasting blood glucose, hemoglobin-A1c, and an oral glucose tolerance test to characterize glycemic control. They noted a prevalence of diabetes of 11.6% (12.1% in men and 11.0% in women) and prevalence of prediabetes of 50.1% (52.1% in men and 48.1% in women). The very large disparity in the prevalence estimates from these 2 studies may be explained by the fact that the latter incorporated hemoglobin-A1c values for the diagnosis of diabetes as per the 2010 American Diabetes Association (ADA) guidelines,[20] and/or that the prevalence of abnormal glycemic control markedly increased in the 3 years that separated these studies.
In comparison to the aforementioned reports, our findings from the prospective Kailuan study are noteworthy. The Kailuan study represents only the population from the city of Tangshan who were employees of the Kailuan company. At first glance, this restriction may indicate a non-nationally representative sample, however, focusing on such a geographically confined and controlled population permitted this very large and ongoing prospective study with recurring health surveys that assess outcome measures over time. In this regard, our study represents a much larger sample size, and uniquely assesses the incidence of prediabetes and diabetes in the context of modifiable risk factors over time that could serve as targets for Chinese public health efforts. We observed a prevalence of diabetes and IFG that rose from 6.6% to 7.7%, and 17.3% to 22.6%, respectively, between 2006 and 2010. Although we only used ADA and WHO guidelines for fasting blood glucose to assess IFG and diabetes, and not a glucose tolerance test, this classification has been shown to parallel the use of hemoglobin-A1c for the identification of individuals at risk for developing adverse sequelae.[21] It is very likely that we may have observed higher incidence rates using the oral glucose tolerance test, since it is known to be more sensitive and specific in detecting impaired glucose tolerance.
Not surprisingly, both men and women exhibited increased incident rates of prediabetes and diabetes as a function of higher body adiposity, irrespective of age. An alarming and noteworthy finding was that even individuals traditionally considered to be “thin” or “non-overweight” exhibited steady increases in fasting blood glucose over time. This was evident even in those individuals in BMI categories of <20 kg/m2 or <23 kg/m2. While it has been recognized that Asian populations are prone to insulin-resistant states at much lower BMI categories than Caucasian counterparts,[22] another factor contributing to this phenomenon may be the distribution of body fat rather than overall BMI. Our analyses suggest that even within low BMI categories, higher WC predicted higher fasting blood glucose and increased the HR for incident IFG and diabetes. This may account for the higher incidence of diabetes in our study population when compared to the United States, which has a higher mean BMI than the Kailuan cohort (approximately 29 kg/m2 in contrast to 25 kg/m2).[23] In 2010, the Center for Disease Control estimated the incidence of diabetes to be 5.5, 15.6, and 13.1 cases per 1000 population in men aged 18 to 44, 45 to 64, and 65 to 79 years, respectively.[24] In women, these estimates were 3.8, 11.5, and 11.9 cases per 1000 population in the same age categories.[24] In contrast, incident diabetes rates in the Kailuan cohort were 10.4, 17.5, and 17.9 cases per 1000 population in men aged 18 to 44, 45 to 64, and 65+ years, and 3.6, 13.1, and 19.5 cases per 1000 population in women of the same age groups.
Diabetes and prediabetes contribute to morbidity, mortality, and healthcare costs. Public health policies that target the early identification and prevention of prediabetes and diabetes may mitigate the individual health and societal burdens associated with these diseases. Like other studies before us,[18,19] we observed a very high prevalence and incidence of diabetes and prediabetes in the Kailuan cohort. Unlike prior investigations, however, we report a disturbingly high incidence of both of these conditions, that is clearly rapidly rising compared to prior surveys in China,[16] in a very large cohort followed over 4 years that appears to be similar irrespective of age or gender. We believe that analysis of the major modifiable risk factors that could contribute to this high incidence could help guide public health decisions to reduce the trajectory of these unfavorable trends. Encouraging weight loss is certainly a widely accepted intervention to lower blood glucose and ultimately reduce the incidence of diabetes,[8] but this may not be the most optimal intervention in Chinese individuals within the very low BMI categories who continue to demonstrate a notable risk for developing glucose intolerance. Furthermore, BMI alone may not account for body fat distribution; WC may be a particularly important barometer of incident risk, especially in those individuals with low BMI. Optimizing WC and BMI will likely require policies to educate the public on healthy eating and improved physical fitness. Other factors such as smoking cessation, physical inactivity, hypertension, and avoidance of dust and environmental exposures are also likely to mitigate the incident risk of prediabetes and diabetes.
Our study has several limitations. All participants were from the Kailuan community. However, our findings are likely generalizable because similar incident rates were reported in recent Chinese studies.[15,17] Further, we did not collect information on random plasma glucose level and oral glucose tolerance test results, and we may underestimate the prevalence/incidence rates.
In summary, we observed a high prevalence and incidence of IFG and diabetes in a large cohort of Chinese adults. These results are considered as alarming for Chinese public health since steady rises in fasting blood glucose were seen across all permutations of body habitus, even apparently very lean individuals. Whether public policy to address physical inactivity, weight reduction, or body habitus can alter the trajectory of these ominous findings warrants investigation.
Supplementary Material
Footnotes
Abbreviations: ADA = American Diabetes Association, BMI = body mass index, CVD = cardiovascular disease, HR = hazard ratio, IFG = impaired fasting glucose, SBP = systolic blood pressure, WC = waist circumference, WHO = World Health Organization, WHR = waist-to-hip ratio.
AV and LC have contributed equally to the article.
Author contributions: All the authors who are named below gave the permission to be named; Drs XG and SW had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: AV, LC, SW, and XG. Acquisition of data: AV, LC, LS, BL, SC, XL, XL, FBH, SW, and XG. Analysis and interpretation of data: AV, LC, BL, FBH, SW, and XG. Drafting of the manuscript: AV, LC, BL, and XG. Critical revision of the manuscript for important intellectual content: AV, LC, LS, BL, SC, XL, XL, XX, FBH, SW, and XG. Statistical analysis: BL and XG. Obtained funding: AV and SW. Administrative, technical, or material support: LC, LS, SC, XL, XL, and SW. Study supervision: SW and XG. Drs AV and LC contributed equally to this work and are co–first authors. Drs XG and SW contributed equally to this work and are co–senior authors.
Funding/support: This work is supported by the National Institutes of Diabetes and Digestive and Kidney Disease of the National Institutes of Health under award number R01 DK107407; by grant 2015085 from the Doris Duke Charitable Foundation; and by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number K23HL111771.
Role of the sponsor: The funding agencies had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript or decision to submit for publication.
All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest and none were reported.
Supplemental Digital Content is available for this article.
References
- 1.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. N Engl J Med 2007; 356:213–215. [DOI] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27:1047–1053. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services, CDC, U.S. Department of Health and Human Services, CDC National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. 2011; http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdfhttp://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf (accessed Sep 1st, 2015). [Google Scholar]
- 4.He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med 2005; 353:1124–1134. [DOI] [PubMed] [Google Scholar]
- 5.Wen CP, Cheng TY, Tsai SP, et al. Increased mortality risks of pre-diabetes (impaired fasting glucose) in Taiwan. Diabetes Care 2005; 28:2756–2761. [DOI] [PubMed] [Google Scholar]
- 6.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011; 364:719–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2013; 381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997; 20:537–544. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Q, Zhou Y, Gao X, et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 2013; 44:2451–2456. [DOI] [PubMed] [Google Scholar]
- 11.Wu S, Huang Z, Yang X, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes 2012; 5:487–493. [DOI] [PubMed] [Google Scholar]
- 12.Population Census Office under the State Council Tabulation on the 2010 Population Census of People's Republic of China. Beijing:China Statistics Press; 2013. [Google Scholar]
- 13.World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation 2006. [Google Scholar]
- 14.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363:157–163. [DOI] [PubMed] [Google Scholar]
- 15.Shang X, Li J, Tao Q, et al. educational level, obesity and incidence of diabetes among Chinese adult men and women aged 18–59 years old: an 11-year follow-up study. PLoS One 2013; 8:e66479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu YH, Li GW, Pan XR. [Incidence of NIDDM in Daqing and forecasting of NIDDM in China in 21st century]. Zhonghua Nei Ke Za Zhi 1993; 32:173–175. [PubMed] [Google Scholar]
- 17.Sun L, Zong G, Pan A, et al. Elevated plasma ferritin is associated with increased incidence of type 2 diabetes in middle-aged and elderly Chinese adults. J Nutr 2013; 143:1459–1465. [DOI] [PubMed] [Google Scholar]
- 18.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362:1090–1101. [DOI] [PubMed] [Google Scholar]
- 19.Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013; 310:948–959. [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33 (suppl 1):S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inzucchi SE. Diagnosis of diabetes. N Engl J Med 2013; 368:193. [DOI] [PubMed] [Google Scholar]
- 22.Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363:157–163. [DOI] [PubMed] [Google Scholar]
- 23.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012; 307:491–497. [DOI] [PubMed] [Google Scholar]
- 24.CDC Diabetes Data & Trends. 2013; http://www.cdc.gov/diabetes/statistics/incidence/fig3.htmhttp://www.cdc.gov/diabetes/statistics/incidence/fig3.htm. 2013 (Oct 8) (accessed Sep 1st, 2015). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


