Abstract
Nonalcoholic fatty liver disease (NAFLD) and occupational stress have been recognized as major public health concerns. We aimed to explore whether occupational stress was associated with NAFLD in a police population.
A total of 6559 male police officers were recruited for this prospective study in April 2007. Among them, 2367 eligible subjects participated in follow-up from 2008 to 2011. NAFLD was diagnosed based on standard criteria. Occupational stress was evaluated by Occupational Stress Inventory-Revised scores.
The incidence of NAFLD was 31.2% in the entire police. After adjusting for traditional risk factors, moderate occupational stress (MOS), high occupational stress (HOS), and high personal strain (HPS) were risk factors (MOS: hazard ratio [HR] = 1.237, 95% confidence interval [CI] = 1.049–1.460; HOS: HR = 1.727, 95% CI = 1.405–2.124; HPS: HR = 3.602, 95% CI = 1.912–6.787); and low occupational stress (LOS) and low personal strain (LPS) were protective factors (LOS: HR = 0.366, 95% CI = 0.173–0.776; LPS: HR = 0.490, 95% CI = 0.262–0.919) for NAFLD in the entire police cohort. HOS and HPS remained robust among traffic police.
HOS and HPS were independent predictors for the development of NAFLD in a Chinese police population. Additional future prospective investigations are warranted to validate our findings.
Keywords: cohort study, nonalcoholic fatty liver disease, occupational stress, police officers
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) has been a major public health issue and gained increasing attention in both clinical studies and as a research-focus due to its potential effects on individual health over the past several years.[1] The prevalence of NAFLD, in the Chinese general population, is reported to be 20% (6.3–27.0%), which is increasing with a rapid increase in obesity and other metabolic syndromes (MetS).[2–4]
As far as we know, NAFLD, which is characterized by an increased accumulation of fat in the liver without excessive alcohol consumption, represents a wide spectrum of diseases ranging from simple steatosis to nonalcoholic steatohepatitis (NASH) or cirrhosis.[2] Several large population studies have reported that NAFLD is closely associated with increased rates of mood disorders and stress.[5,6] The lifetime prevalence of major depressive disorder and generalized anxiety disorder were higher in patients with NASH than in control subjects (63.8% vs 33.3%) after matching for covariates.[6] Moreover, occupational stress is becoming a major working-mental health issue that could lead to less cooperation, low productivity, regular absenteeism, and poor quality of life.[7] Previous studies indicate that policing is one of the most stressful occupations, and high work stress is associated with MetS in police officers.[8,9] However, little is known about the relationship between occupational stress and NAFLD, especially in Chinese police officers, who play a pivotal role in modern society and have relatively high stress due to exposure to potential violence and life-threatening events in the daily workplaces.[9]
Current estimates suggest that occupational stress can be evaluated using various questionnaires.[10] The Occupational Stress Inventory-Revised (OSI-R) questionnaire, which is confirmed to have a good reliability and validity in different occupational populations, has been widely used to assess the degree of occupational stress, and to analyze the relationship between occupational stress and healthy disorders.[11] Thus, our study was established to examine the relationship between occupational stress based on OSI-R scores and the incidence of NAFLD in a police cohort in Tianjin, China.
2. Methods
2.1. Study population
All the subjects in our study were recruited in April 2007 at the Medical Center of Police Hospital in Tianjin, China, where medical examinations are provided to both working and retired policemen every year.[9,11] A total of 6559 male police officers (aged 20–60 years) participated in the study; they received free health examinations, and completed the OSI-R questionnaire and interviewer-administered questionnaires. Among them, 4192 participants were excluded based on the following criteria: 408 did not complete the OSI-R and self-designed questionnaires at baseline; 295 had missing ultrasound scanning data; 981 had a history of or concurrent alcohol abuse (more than 30 g/d for males)[12]; 362 were using steatohepatitis medication; 2146 had been diagnosed with NAFLD, chronic hepatitis B or C, autoimmune hepatitis or other liver diseases at the beginning of the study. Ultimately, the other 2367 subjects agreed to be followed up with dynamic observations each year from 2008 to 2011 (see Fig. 1 for a subject flowchart).
Figure 1.
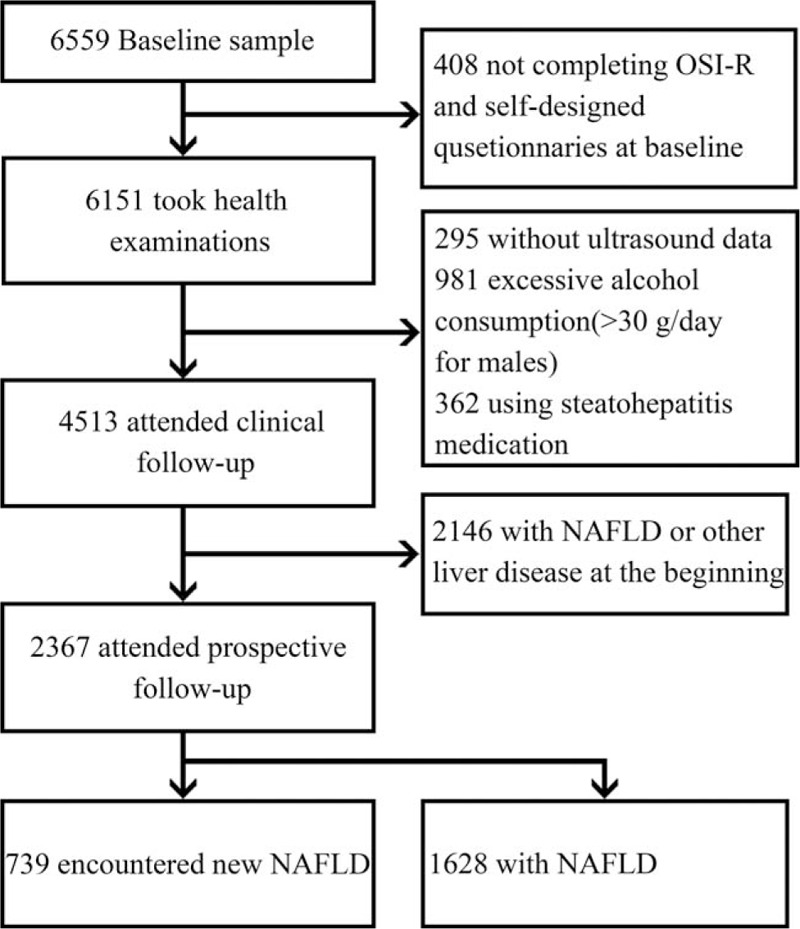
Flow chart of the study population.
This survey protocol was approved by the ethics committee of Tianjin Medical University (Tianjin, China) and the Tianjin Public Health Bureau (Tianjin, China). We received written consent from all the participants at baseline.
2.2. Clinical and laboratory assays
All the subjects underwent clinical and laboratory assays that included anthropometric measurements, abdominal ultrasonographic scanning, and biochemical measurements.
The anthropometric measurements included height, weight, waist circumference, hip circumference, and blood pressure (BP). BP was measured 3 times with an Electronic Sphygmomanometer (XW-200, made in Shenzhen, China) after 5 min of rest, and we calculated the average.[9] Ultrasonic scanning was performed in all the participants by an experienced radiologist in a double-blinded fashion. Fasting blood samples were obtained via venipuncture by well-trained clinical nurses from 8 am until noon, and were sent to a laboratory in police hospital <60 min after collection.[11] Biochemical values including alanine aminotransferase (ALT), total cholesterol (TC), triglycerides (TG), high- and low-density lipoprotein cholesterol (H/LDL-C), and fasting plasma glucose (FPG) were tested using an Automatic Biochemical Analyzer (TBA-120FR, Toshiba Corp, made in Shanghai, China) with standard laboratory procedures.[9]
2.3. Measurement of occupational stress
Occupational stress was measured with the Chinese version of the OSI-R, which is a self-report questionnaire and a psychometrically validated stress instrument that includes 3 individual scales: the Occupational Roles Questionnaire (ORQ), Personal Strain Questionnaire (PSQ), and Personal Resources Questionnaire (PRQ).[13] To provide individual levels, the OSI-R scores were transformed into standard T scores. Then, we divided our sample into 4 groups according to T scores: low stress and strain (≤40; LOS/LPS), normal stress and strain (40–59; NOS/NPS), moderate stress and strain (60–69; MOS/MPS), and high stress and strain (≥70; HOS/HPS) for ORQ and PSQ; and significant deficits in coping resources (<30; SDCR), moderate lack of coping resources (30–39; MLCR), average coping resources (40–59), and high coping resources (≥60; HCR) for PRQ.[13] In particular, the OSI-R questionnaire used in the present study was confirmed to have good reliability and internal consistency for Chinese policemen (Cronbach alpha: OSI-R = 0.883, ORQ = 0.908, PSQ = 0.934, and PRQ = 0.909).[11]
2.4. Diagnosis of NAFLD
The standard criteria for the diagnosis of NAFLD were based on the ordinance issued by the Fatty Liver Disease Study Group of the Chinese Liver Disease Association[14]: exclusion of other liver diseases, such as alcohol or drug-induced liver diseases, autoimmune or viral hepatitis, metabolic liver disease, and genetic liver disease[1]; laboratory tests: elevated ALT (>29 IU/L)[15]; and abdominal ultrasonic examinations: increased hepatic echogenicity compared with the spleen and kidneys, blurring of liver vasculature, and deep attenuation of ultrasonographic signals through the right hepatic lobe.
2.5. Measurements of covariates
Thorough socioeconomic and demographic variables were collected based on interviewer-administered questionnaires. Those characteristics included age (<45, 45–54, or ≥55), body mass index (BMI; <18.5, 18.5–24.99, 25–29.99, or ≥30),[16] marital status (married or other), educational level (lower than college or college and above), office work, working strength (≤8 or >8 h), smoking status (nonsmoker, current smoker, or former smoker), alcohol status (nondrinker, current drinker, or former drinker), physical exercise (never or seldom, occasionally, often, or every day), and MetS-related factors (central obesity; hypertension; elevated TG; reduced HDL-C, or raised FPG). Among them, BMI was calculated as body weight (in kilograms) divided by the square of body height (in square meters).[16]
MetS was diagnosed using the New International Diabetes Federation worldwide definition.[17] The criteria were central obesity (waist circumference ≥ 90 cm in males) plus at least 2 of the 4 following factors:
Raised BP (systolic BP ≥ 130 or diastolic BP ≥ 85 mm Hg) or reported antihypertensive treatments.
Elevated TG levels (≥1.7 mmol/L) or reported treatments with this abnormalities.
Reduced HDL-C (<1.03 mmol/L in males) or reported treatments with this lipid abnormalities.
Raised FPG (≥5.6 mmol/L) or reported diagnosed diabetes.
2.6. Statistical analysis
Mann–Whitney U test was conducted for continuous variables, and a Chi-squared test for categorical variables, which were reported as means ± standard deviations (SD) or frequencies, to compare the differences between subjects with and without NAFLD. Univariate Cox-proportional hazards regression analysis was performed to identify risk factors related to NAFLD. Cox-proportional hazards regression models were applied to explore predictors for the development of NAFLD before and after adjusting for covariates, such as age, BMI, marital status, office work, working strength, educational level, smoking status, alcohol intake, physical exercise, police assignments, central obesity, raised BP, elevated TG, reduced HDL-C, and raised FPG and MetS. Meanwhile, Kaplan–Meier survival curve and the log-rank test were conducted to compare cumulative survival rate on different police assignments. All the statistical analyses were performed using SPSS 19.0 software (IBM, Chicago, IL). A 2-tailed P < 0.05 was considered statistically significant. For multiple comparisons, the adjusted P value based on Bonferroni method was considered credible for estimating statistically significant.
3. Results
3.1. Baseline characteristics of the cohort population and comparison between NAFLD nononset and new-onset groups
The final study included 2367 subjects with a mean age of 36.65 (SD = 9.37) years. During a 4-year follow-up (median time: 2.61 years, 25th to 75th percentiles: 1.53–3.75 years), 739 participants (31.2%) developed new NAFLD. The prevalence rates (number of new cases) were 9.5% (225) in 2008, 4.8% (113) in 2009, 9.5% (226) in 2010, and 7.4% (175) in 2011.
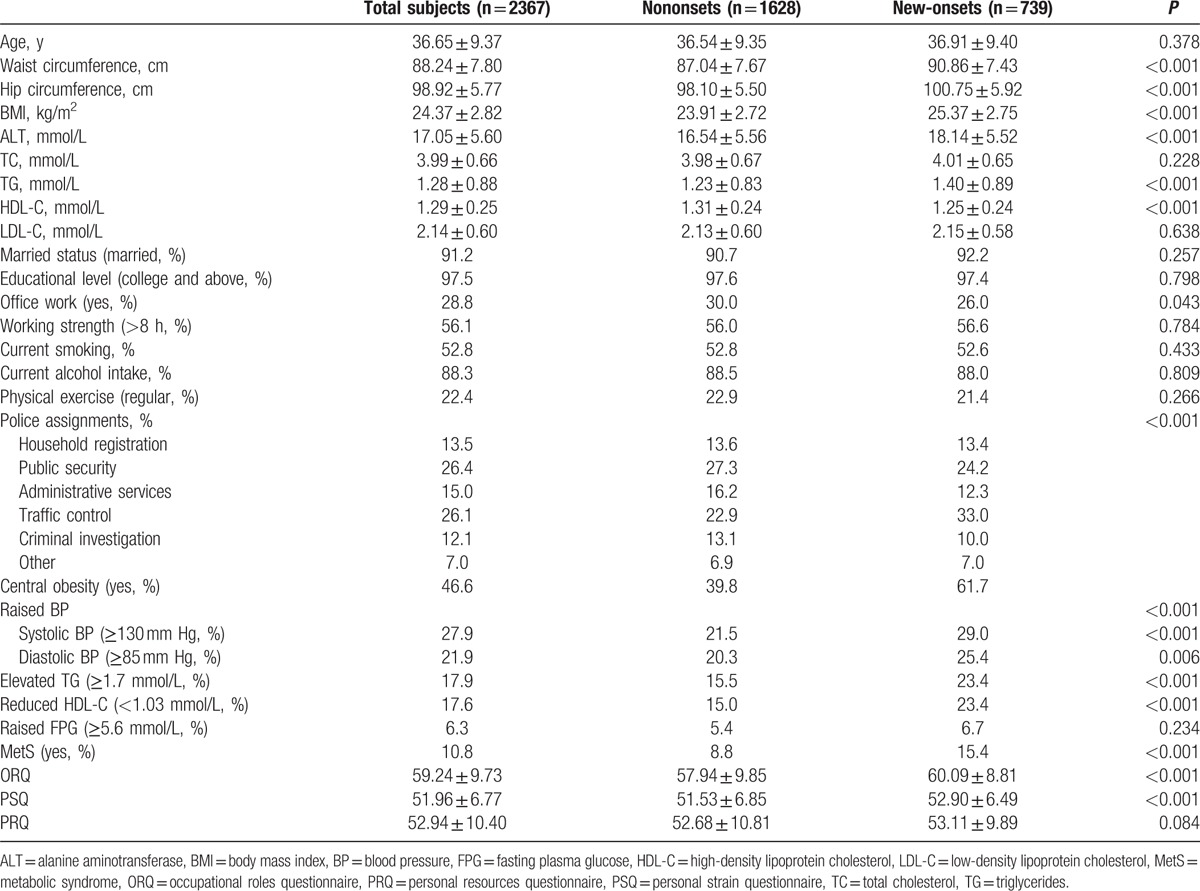
Compared to the nononset subjects, those new-onsets had higher ORQ and PSQ scores; higher waist and hip circumferences; and higher levels of BMI, ALT, TG, and HDL-C. Categorical variables including office work, police assignments, central obesity; hypertension; elevated TG; and reduced HDL-C and MetS were significantly different between the groups, whereas no significant difference was noted in terms of age, TC, LDL-C, marital status, educational level, working strength, current smoking status, current alcohol intake, physical exercise, and raised FPG or PRQ scores (Table 1).
Table 1.
Baseline characteristics of the study population and comparison between nonalcoholic fatty liver disease nononset group and the new-onset group.
3.2. Association between occupational stress and NAFLD in all police officers
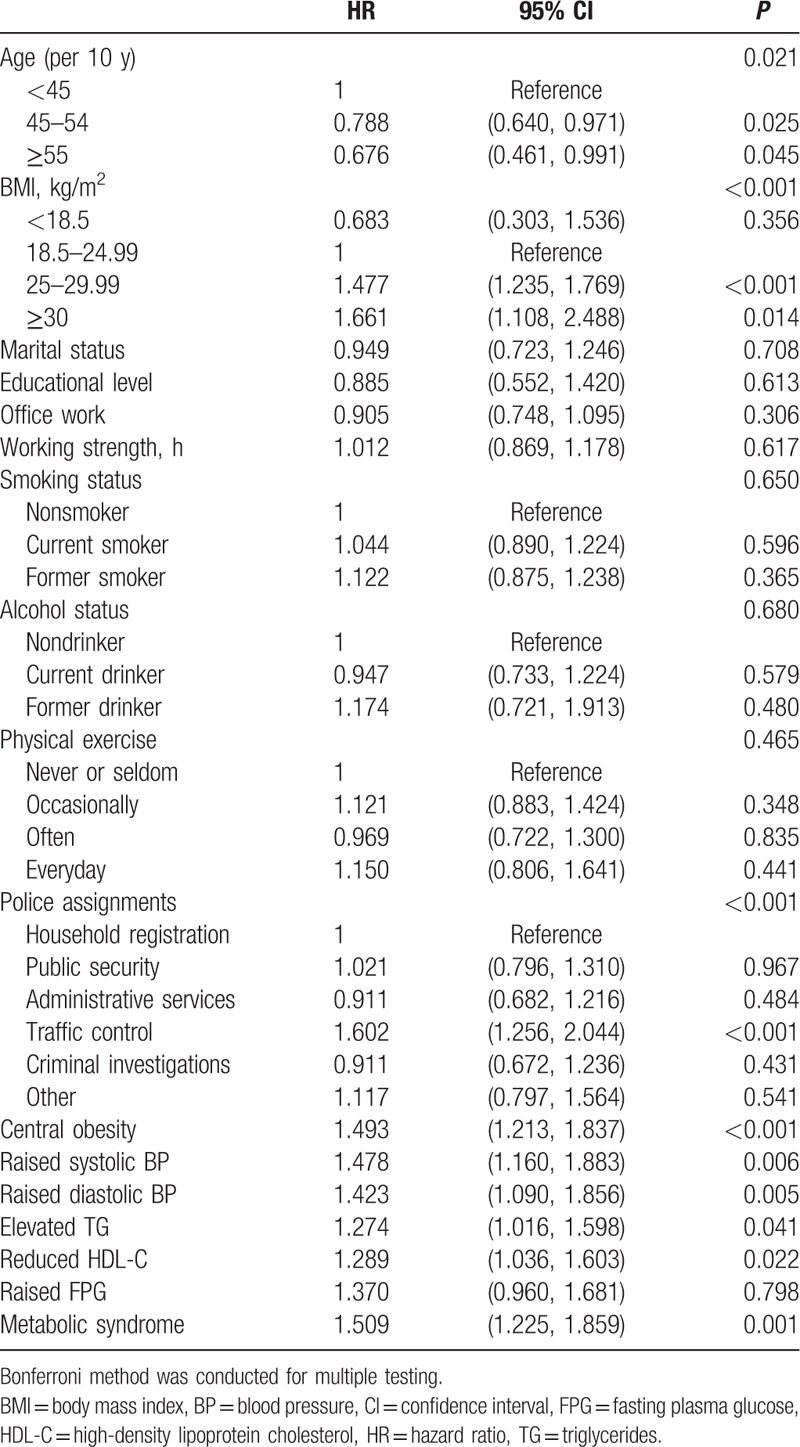
Before adding occupational stress to the model, we primarily found that age, BMI, police assignments, central obesity; hypertension; elevated TG; and reduced HDL-C and MetS were predictive for the occurrence of NAFLD (Table 2).
Table 2.
Cox-regression analyses of traditional risk factors associated with nonalcoholic fatty liver disease.
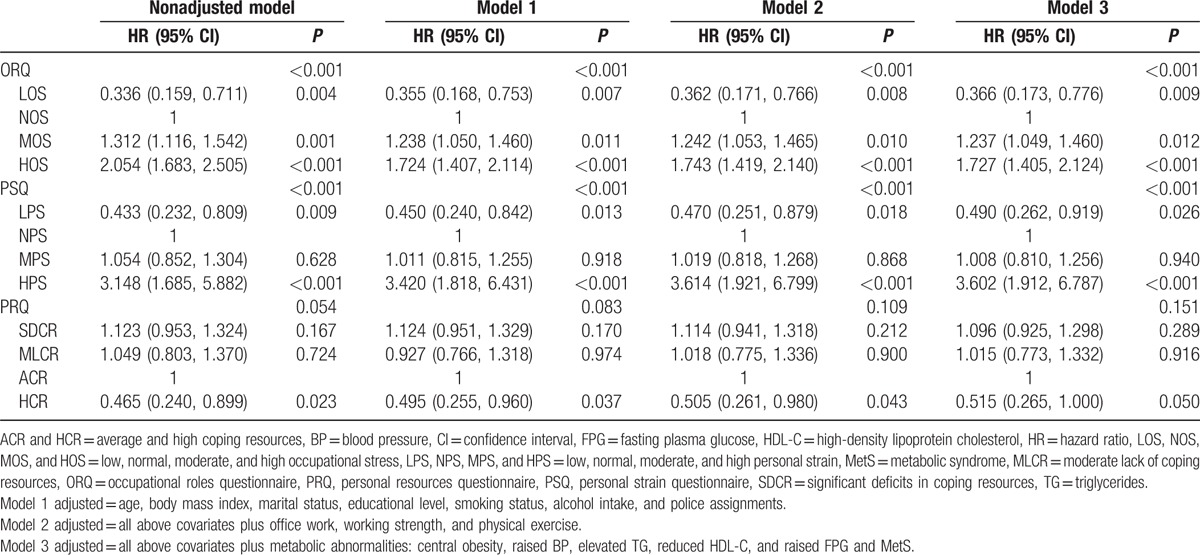
The results of the Cox-proportional hazards regression also indicated that, before and after adjusting for traditional risk factors, MOS, HOS, and HPS were risk factors for NAFLD (MOS: hazard ratio [HR] = 1.237, 95% confidence interval [CI] = 1.049–1.460; HOS: HR = 1.727, 95% CI = 1.405–2.124; HPS: HR = 3.602, 95% CI = 1.912–6.787). In addition, LOS and LPS were protective factors against NAFLD (LOS: HR = 0.366, 95% CI = 0.173–0.776; LPS: HR = 0.490, 95% CI = 0.262–0.919) (Table 3).
Table 3.
Cox-regression analyses of T-scores associated with nonalcoholic fatty liver disease in all police officers.
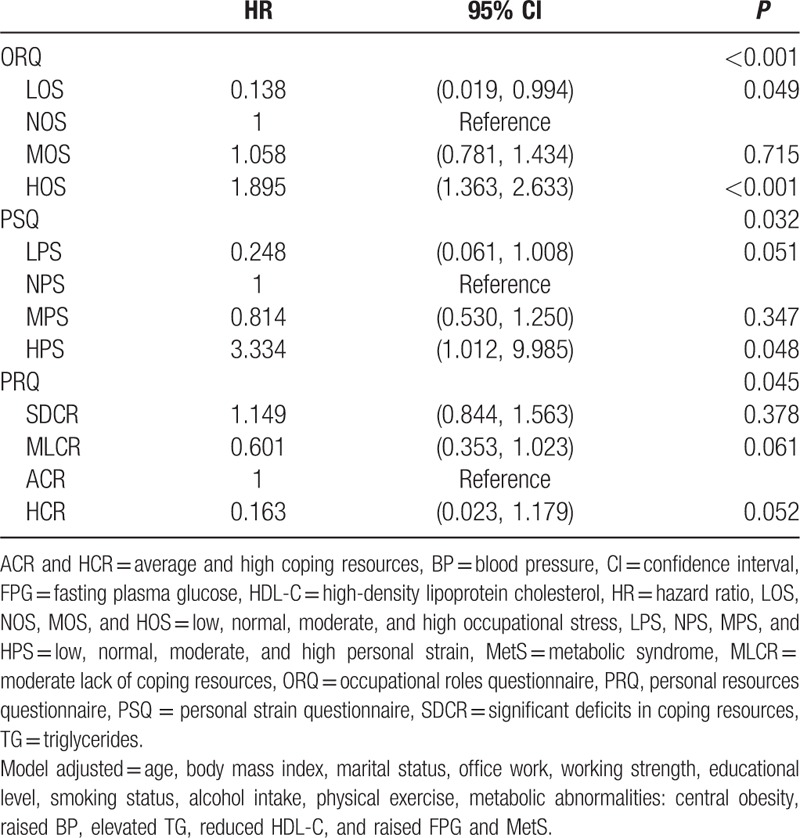
3.3. Association between occupational stress and NAFLD in traffic police officers
Figure 2 indicates that the incidence of NAFLD in traffic police was significantly higher than in other police. After adjusting for traditional risk factors in the subgroup of traffic police, Table 4 shows that HOS and HPS were still risk factors (HOS: HR = 1.895, 95% CI = 1.363–2.633; HPS: HR = 3.334, 95% CI = 1.012–9.985) and LOS was still a protective factor (with lower HR: 0.138) for NAFLD. We also observed that MLCR (HR = 0.601) and HCR (HR = 0.163), which were not significant in the overall police, trend to be protective factors in the traffic police officers.
Figure 2.
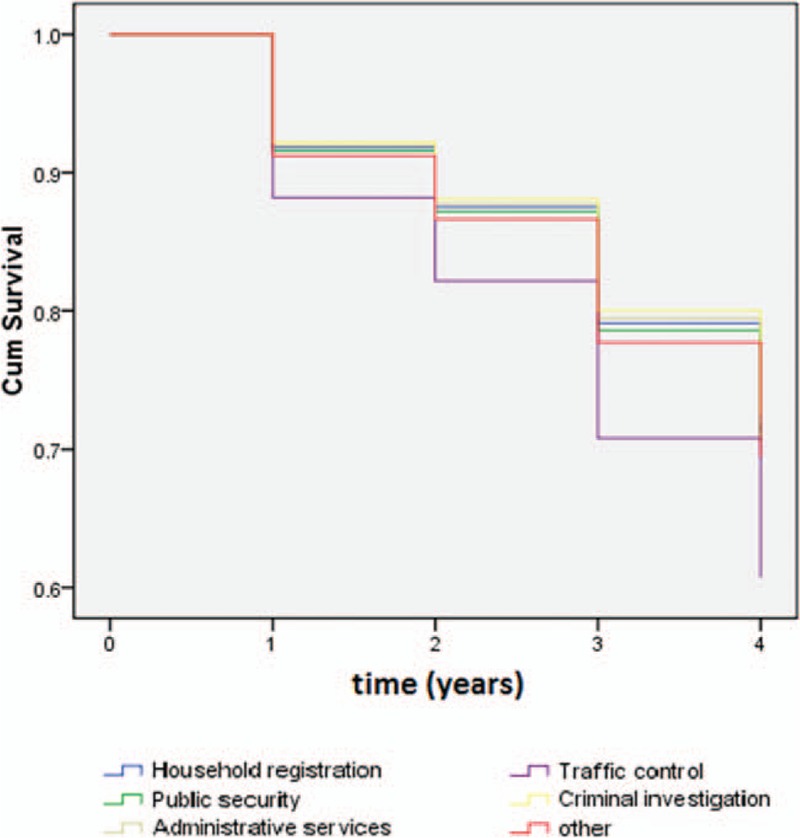
Kaplan–Meier survival curves for different police populations.
Table 4.
Cox-regression analyses of T-scores associated with nonalcoholic fatty liver disease among traffic officers.
4. Discussion
To the best of our knowledge, NAFLD has been considered to be a main cause of chronic liver disease in both developed and developing countries, affected about 30% of the general population.[1,3] In the developed countries, like North America, Japan, Northern and Southern Europe, South America, Australia, and the Middle East, the prevalence of NAFLD varies from 20% to 46%.[18] Partly because of different dietary habits and body composition differences in fat and muscle, the prevalence of NAFLD in the Asian countries is 20% in China; 27% in Hong Kong; and ranges from 15% to 45% in South Asia, South-East Asia, Korea, and Taiwan.[1] In our present study, approximately one-third (31.2%) of the participants developed new NAFLD during the follow-up. HOS and HPS were independent predictors for the development of NAFLD in a Chinese police population. However, given that NAFLD is often asymptomatic,[1] limited studies have investigated the association between NAFLD and occupational stress.
Although several published studies have reported that depression and anxiety is associated with NAFLD, controversy remains about the relationship between depression and NAFLD. On one hand, a 2011 study with a small sample size demonstrated no clear relationship between NAFLD and depression.[19] Lee et al[20] found that depression did not independently influence the incidence of NAFLD at the population level after controlling for covariates. On the other hand, a case–control study demonstrated that depression and anxiety could impact the severity and progression of NASH.[6] Similarly, a population-based study showed a higher rate of depression in patients with NAFLD (27.2%) than in patients with chronic hepatitis B (3.7%).[5] At the same time, compared to both a healthy population and patients with hepatitis B or C, a lower quality of life was found in patients with NAFLD.[21,22] Another cross-sectional study analyzing 567 adult-NAFLD patients proposed that subclinical (odds ratio [OR] = 2.1, 95% CI = 1.0–4.4) and clinical (OR = 3.6, 95% CI = 1.4–8.8) depression were associated with a significantly higher degree of hepatocyte ballooning.[23] In addition, a meta-analysis based on 166,631 individuals and a mean 9.5 years of follow-up, found a noticeable relationship between high psychological distress and liver disease mortality (HR = 2.59), especially in the subgroup of subjects with NAFLD.[24] There is also growing evidence that children and adolescents with NAFLD have a higher rate of psychological distress compared with healthy or obese controls.[25,26] Furthermore, in the present research, occupational stress was demonstrated to be a risk factor for NAFLD among Chinese police officers.
Looking at various studies around the world, about 25% to 30% of police officers have a stress-related physical health problem,[27,28] with an explanation that they are exposed to numerous types of risk factors including environmental stress, administrative pressure, rotating shifts, high work load, depression, less sleep, poor nutrition, and less physical activities.[29–31] A few studies have suggested that work stress is associated with higher prevalence of MetS in police officers who belong to a community with more adverse risk factors and higher mortality rates than the general population.[32–34] Hartley et al[27] also found a positive association between job stress and the number of MetS components. And a cohort study demonstrated that occupational stress was an independent predictor of diabetes.[11,35] Additionally, NAFLD is a hepatic manifestation of MetS (i.e., associated with those traditional risk factors).[32,36,37] Thus, we further analyzed the association between occupational stress and NAFLD after adjusted MetS-related factors.
Compounding this issue is the well-known fact that physical activity has been one of the most important protectors against MetS and cancers worldwidely,[38–40] as well as a dose–dependent relationship between exercise and quality of life improvements.[41–43] In one study, Franke and Anderson[44] reported that exercise could reduce cardiovascular disease risk via modifying major risk factors in a law enforcement office population (>48 years of age). And Heneweer et al[39] suggested that better physical fitness can be helpful for the prevention of low back pain. In another study, Pollock et al[45] showed that middle-aged police officers have lower levels of physical fitness and higher disease risk than younger police officers (<30 years old). Meanwhile, a 15-year cohort study has proved that physical activity in the early adulthood can predict the physical fitness of middle-aged police,[46] along with that police officers usually display high job-related physical activity levels and can complete all police tasks on their daily work.[39,47,48] However, there is a correlation between physical activity levels and police duties, which requiring different demands.[38] Ramey et al[49] also pointed that police officers tend to be less active on their work days than during off-duty hours. While in our current study, regular physical activity levels have no difference between NAFLD nononset and new-onset groups (P = 0.266). The explanation could be that we used self-reported physical activity questionnaires, which could be affected by self-images and have recall bias. Thus, further studies are required to investigate this factor in detail.
Another interesting result of our study was that occupational stress is more related with NAFLD in traffic police population. The rapid economic growth and massive transportation developments in modern China have been accompanied by increases in workloads, urbanization and automobile use, along with severe air pollution, and high traffic noise.[9] Additionally, the Chinese traffic police are a full-time traffic control staff and are exposed to air pollution and traffic noise almost every day.[9,11] Mounting evidence has demonstrated that a heavy workload and high noise and air pollution cannot only damage people's physical and mental health but also mediate the pathogenesis of NAFLD via insulin resistance (IR), inflammation or oxidative stress (OS).[50,51] Thus, we assumed that environmental factors might play a vital role in the association between NAFLD and occupational stress.
The mechanisms by which occupational stress affects NAFLD remain unclear and complex. Several plausible mechanisms have been proposed, including cytokine-related inflammation, activation of the hypothalamic–pituitary–adrenal axis, IR, OS, and several indirect mechanisms.[3,52] First, cytokines such as interleukin-1, interleukin-6, and tumor necrosis factor-α have been postulated to be responsible for the changes in depression in inflammatory patients.[53] These cytokines, which have been demonstrated to be involved in the pathogenesis of NASH,[53,54] can cause depressive symptoms by inducing dysfunctions in brain neurotransmission and a similar “sickness behavior” in a mouse model.[55,56] Second, a growing body of evidence has suggested that depression can continuously activate and overstimulate the hypothalamic–pituitary–adrenal axis to increase cortisol secretion, which is associated with IR in the control of liver fat accumulation.[24,51] Guevara et al[57] also discovered that measurable changes in brain density were related to liver disease. Furthermore, some reports have revealed that depression and anxiety are potentially connected to IR,[7,51] and higher OS markers were found in a group of patients with depression versus control subjects.[58] Third, according to the “multiple-hit” theory, IR and OS are involved in the process of NAFLD,[24] both of which can lead to greater accumulation of hepatic TG and disorders of lipid metabolism.[59] Another mechanism may involve a battery of unhealthy behaviors, such as excessive drinking, cigarette smoking, and overeating, which can be brought by occupational stress.[60] Subsequently, in parallel to these behaviors, serum leptin levels decrease and triglyceride levels increase, resulting in a high prevalence of NAFLD or other MetS.[60]
4.1. Limitations
It is notable that our study examined whether occupational distress was correlated with NAFLD in a police population after adjusting for baseline demographic and socioeconomic variables, which could have clinical and therapeutic implications as well as provide further information to investigators about the underlying mechanisms.
However, there are several limitations of our research. First, the scale that was used in our study might be a crude measure, although has been validated for evaluating occupational stress.[10] Additionally, we recorded OSI-R scores via questionnaires at baseline only, with no reassessments during the follow-up years. Second, considering the large sample size of our study, we utilized blood tests (based on ALT) and ultrasonography as screening tools, which were relatively sensitive, low cost, and widely available to all subjects.[61] However, the sensitivity was lower than that of liver biopsy, which is the “gold standard” for diagnosis of NAFLD.[61] Third, NAFLD had appeared to be associated with air pollution and traffic noise.[62] However, we did not obtain comprehensive nutrition and environmental monitoring data, regarding the nutritional status, air pollution status, and traffic noise levels, encountered by police officers. Thus, it is difficult to confirm the precise influence of nutrition and environmental factors on NAFLD and occupational stress. Lastly, the number of female police officers in our study is relatively small (n = 501) versus male officers (n = 6559) and the incidence of NAFLD in policewomen is also relatively low (5.6%), so we just analyzed and compared male data in the end. Thus, we could not provide valuable conclusions about the female police population. In view of these limitations, more clinical and epidemiological studies are required to enrich and confirm our findings.
In summary, this cohort study reveal that HOS and HPS are independent predictors of NAFLD in a Chinese police population, especially among traffic control police. Systematic investigations using more accurate and noninvasive imaging techniques are warranted to confirm our conclusions and to contribute to the development of more suitable treatments and psychological interventions for NAFLD and occupational stress, consequently elucidating the need for regular screening, healthy lifestyle modifications, and stress monitoring among occupational populations.
Acknowledgments
The authors thank all of the physicians and nurses at the Tianjin Medical Center of Police Hospital for their cooperation and data collection support. The authors also acknowledge the efforts of prior investigators in this area of research.
Footnotes
Abbreviations: ALT = alanine aminotransferase, BMI = body mass index, BP = blood pressure, CI = confidence interval, FPG = fasting plasma glucose, HCR = high coping resources, HDL-C = high-density lipoprotein cholesterol, HR = hazard ratio, IR = insulin resistance, LDL-C = low-density lipoprotein cholesterol, LOS, NOS, MOS, and HOS = low, normal, moderate, and high occupational stress, LPS, NPS, MPS, and HPS = low, normal, moderate, and high personal strain, MetS = metabolic syndrome, MLCR = moderate lack of coping resources, NAFLD = nonalcoholic fatty liver disease, NASH = nonalcoholic steatohepatitis, ORQ = occupational roles questionnaire, OS = oxidative stress, OSI-R = Occupational Stress Inventory-Revised, PRQ = personal resources questionnaire, PSQ = personal strain questionnaire, SD = standard deviation, SDCR = significant deficits in coping resources, TC = total cholesterol, TG = triglycerides.
CL and J-JX contributed equally to this work.
This study was supported by grant 08ZCGYSF01500 and 10ZCKFSF00600 from the Tianjin Municipal Science and Technology Commission.
The authors have no conflicts of interest to disclose.
References
- 1.Farrell GC, Wong VW, Chitturi S. NAFLD in Asia—as common and important as in the West. Nat Rev Gastroenterol Hepatol 2013; 10:307–318. [DOI] [PubMed] [Google Scholar]
- 2.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol 2013; 10:330–344. [DOI] [PubMed] [Google Scholar]
- 3.Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis 2008; 28:339–350. [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Xue J, Chen P, et al. Prevalence of nonalcoholic fatty liver disease in mainland of China: a meta-analysis of published studies. J Gastroenterol Hepatol 2014; 29:42–51. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein AA, Kallman Price J, Stepanova M, et al. Depression in patients with nonalcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics 2011; 52:127–132. [DOI] [PubMed] [Google Scholar]
- 6.Elwing JE, Lustman PJ, Wang HL, et al. Depression, anxiety, and nonalcoholic steatohepatitis. Psychosom Med 2006; 68:563–569. [DOI] [PubMed] [Google Scholar]
- 7.Chandola T, Britton A, Brunner E, et al. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J 2008; 29:640–648. [DOI] [PubMed] [Google Scholar]
- 8.Garbarino S, Magnavita N. Work stress and metabolic syndrome in police officers. A prospective study. PLoS ONE 2015; 10:e0144318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X, Leng L, Yu H, et al. Psychological distress and dyslipidemia in Chinese police officers: a 4-year follow-up study in Tianjin, China. J Occup Environ Med 2015; 57:400–405. [DOI] [PubMed] [Google Scholar]
- 10.Yang X, Ge C, Hu B, et al. Relationship between quality of life and occupational stress among teachers. Public Health 2009; 123:750–755. [DOI] [PubMed] [Google Scholar]
- 11.Yu H, Liu JC, Fan YJ, et al. Association between occupational stressors and type 2 diabetes among Chinese police officers: a 4-year follow-up study in Tianjin, China. Int Arch Occup Environ Health 2015; 89:277–288. [DOI] [PubMed] [Google Scholar]
- 12.Lin YC, Chou SC, Huang PT, et al. Risk factors and predictors of non-alcoholic fatty liver disease in Taiwan. Ann Hepatol 2011; 10:125–132. [PubMed] [Google Scholar]
- 13.Osipow SH. A Manual for the Occupational Stress Inventory Revised Edition (Professional Manual). Lutz, FL:Psychological Assessment Resources, Inc; 1998. [Google Scholar]
- 14.Zeng MD, Fan JG, Lu LG, et al. Guidelines for the diagnosis and treatment of nonalcoholic fatty liver diseases. J Dig Dis 2008; 9:108–112. [DOI] [PubMed] [Google Scholar]
- 15.Ruhl CE, Everhart JE. Upper limits of normal for alanine aminotransferase activity in the United States population. Hepatology (Baltimore, MD) 2012; 55:447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akram DS, Astrup AV, Atinmo T, et al. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894:i–xii. [PubMed] [Google Scholar]
- 17.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabetic Med 2006; 23:469–480. [DOI] [PubMed] [Google Scholar]
- 18.Ross AB, Godin JP, Minehira K, et al. Increasing whole grain intake as part of prevention and treatment of nonalcoholic fatty liver disease. Int J Endocrinol 2013; 2013:585876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Surdea-Blaga T, Dumitrascu DL. Depression and anxiety in nonalcoholic steatohepatitis: is there any association? Rom J Intern Med 2011; 49:273–280. [PubMed] [Google Scholar]
- 20.Lee K, Otgonsuren M, Younoszai Z, et al. Association of chronic liver disease with depression: a population-based study. Psychosomatics 2013; 54:52–59. [DOI] [PubMed] [Google Scholar]
- 21.David K, Kowdley KV, Unalp A, et al. Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology (Baltimore, MD) 2009; 49:1904–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dan AA, Kallman JB, Wheeler A, et al. Health-related quality of life in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2007; 26:815–820. [DOI] [PubMed] [Google Scholar]
- 23.Youssef NA, Abdelmalek MF, Binks M, et al. Associations of depression, anxiety and antidepressants with histological severity of nonalcoholic fatty liver disease. Liver Int 2013; 33:1062–1070. [DOI] [PubMed] [Google Scholar]
- 24.Russ TC, Kivimaki M, Morling JR, et al. Association between psychological distress and liver disease mortality: a meta-analysis of individual study participants. Gastroenterology 2015; 148:958–966. [DOI] [PubMed] [Google Scholar]
- 25.Kerkar N, D’Urso C, Van Nostrand K, et al. Psychosocial outcomes for children with nonalcoholic fatty liver disease over time and compared with obese controls. J Pediatr Gastroenterol Nutr 2013; 56:77–82. [DOI] [PubMed] [Google Scholar]
- 26.Berardis S, Sokal E. Pediatric non-alcoholic fatty liver disease: an increasing public health issue. Eur J Pediatr 2014; 173:131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hartley TA, Burchfiel CM, Fekedulegn D, et al. Associations between police officer stress and the metabolic syndrome. Int J Emerg Ment Health 2011; 13:243–256. [PMC free article] [PubMed] [Google Scholar]
- 28.Violanti JM. Introduction to special issue: stress and health in law enforcement. Int J Emerg Ment Health 2011; 13:209–210. [PubMed] [Google Scholar]
- 29.Violanti JM, Fekedulegn D, Hartley TA, et al. Life expectancy in police officers: a comparison with the U.S. general population. Int J Emerg Ment Health 2013; 15:217–228. [PMC free article] [PubMed] [Google Scholar]
- 30.Kales SN, Tsismenakis AJ, Zhang C, et al. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens 2009; 22:11–20. [DOI] [PubMed] [Google Scholar]
- 31.Amine EK, Baba NH, Belhadj M, et al. Diet, nutrition and the prevention of chronic diseases. Report of a Joint WHO/FAO Expert Consultation. World Health Organ Tech Rep Ser 2003; 916:i–viii. [PubMed] [Google Scholar]
- 32.Hartley TA, Knox SS, Fekedulegn D, et al. Association between depressive symptoms and metabolic syndrome in police officers: results from two cross-sectional studies. J Environ Public Health 2012; 2012:861219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tharkar S, Kumpatla S, Muthukumaran P, et al. High prevalence of metabolic syndrome and cardiovascular risk among police personnel compared to general population in India. J Assoc Physicians India 2008; 56:845–849. [PubMed] [Google Scholar]
- 34.Aguilar M, Bhuket T, Torres S, et al. Prevalence of the metabolic syndrome in the United States, 2003–2012. Jama 2015; 313:1973–1974. [DOI] [PubMed] [Google Scholar]
- 35.Violanti JM, Fekedulegn D, Andrew ME, et al. Adiposity in policing: mental health consequences. Int J Emerg Mental Health 2011; 13:257–266. [PubMed] [Google Scholar]
- 36.Thayyil J, Jayakrishnan TT, Raja M, et al. Metabolic syndrome and other cardiovascular risk factors among police officers. N Am J Med Sci 2012; 4:630–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sperling LS, Mechanick JI, Neeland IJ, et al. The cardio-metabolic health alliance: working toward a new care model for the metabolic syndrome. J Am Coll Cardiol 2015; 66:1050–1067. [DOI] [PubMed] [Google Scholar]
- 38.Leischik R, Foshag P, Strauss M, et al. Aerobic capacity, physical activity and metabolic risk factors in firefighters compared with police officers and sedentary clerks. PLoS ONE 2015; 10:e0133113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heneweer H, Picavet HS, Staes F, et al. Physical fitness, rather than self-reported physical activities, is more strongly associated with low back pain: evidence from a working population. Eur Spine J 2012; 21:1265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leischik R, Foshag P, Strauss M, et al. Physical activity, cardiorespiratory fitness and carotid intima thickness: sedentary occupation as risk factor for atherosclerosis and obesity. Eur Rev Med Pharmacol Sci 2015; 19:3157–3168. [PubMed] [Google Scholar]
- 41.Pereira MJ, Coombes BK, Comans TA, et al. The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: a systematic review. Occup Environ Med 2015; 72:401–412. [DOI] [PubMed] [Google Scholar]
- 42.Leischik R, Dworrak B, Strauss M, et al. Plasticity of health. Ger J Med 2016; 1:1–17. [Google Scholar]
- 43.Edwardson CL, Gorely T, Davies MJ, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS ONE 2012; 7:e34916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Franke WD, Anderson DF. Relationship between physical activity and risk factors for cardiovascular disease among law enforcement officers. J Occup Med 1994; 36:1127–1132. [DOI] [PubMed] [Google Scholar]
- 45.Pollock ML, Gettman LR, Meyer BU. Analysis of physical fitness and coronary heart disease risk of Dallas area police officers. J Occup Med 1978; 20:393–398. [PubMed] [Google Scholar]
- 46.Sorensen L, Smolander J, Louhevaara V, et al. Physical activity, fitness and body composition of Finnish police officers: a 15-year follow-up study. Occup Med (Oxf, Engl) 2000; 50:3–10. [DOI] [PubMed] [Google Scholar]
- 47.Spitler DL, Jones G, Hawkins J, et al. Body composition and physiological characteristics of law enforcement officers. Br J Sports Med 1987; 21:154–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soroka A, Sawicki B. Physical activity levels as a quantifier in police officers and cadets. Int J Occup Med Environ Health 2014; 27:498–505. [DOI] [PubMed] [Google Scholar]
- 49.Ramey SL, Perkhounkova Y, Moon M, et al. Physical activity in police beyond self-report. J Occup Environ Med 2014; 56:338–343. [DOI] [PubMed] [Google Scholar]
- 50.Prasad SB, Vidyullatha P, Vani GT, et al. Association of gene polymorphism in detoxification enzymes and urinary 8-OHdG levels in traffic policemen exposed to vehicular exhaust. Inhal Toxicol 2013; 25:1–8. [DOI] [PubMed] [Google Scholar]
- 51.Tilg H, Moschen AR. Insulin resistance, inflammation, and non-alcoholic fatty liver disease. Trends Endocrinol Metab 2008; 19:371–379. [DOI] [PubMed] [Google Scholar]
- 52.Zelber-Sagi S, Toker S, Armon G, et al. Elevated alanine aminotransferase independently predicts new onset of depression in employees undergoing health screening examinations. Psychol Med 2013; 43:2603–2613. [DOI] [PubMed] [Google Scholar]
- 53.Wu CL, Zhao SP, Yu BL. Intracellular role of exchangeable apolipoproteins in energy homeostasis, obesity and non-alcoholic fatty liver disease. Biol Rev Camb Philos Soc 2015; 90:367–376. [DOI] [PubMed] [Google Scholar]
- 54.Mann JP, De Vito R, Mosca A, et al. Portal inflammation is independently associated with fibrosis and metabolic syndrome in paediatric non-alcoholic fatty liver disease. Hepatology (Baltimore, MD) 2015; 63:745–753. [DOI] [PubMed] [Google Scholar]
- 55.Dantzer R, O’Connor JC, Lawson MA, et al. Inflammation-associated depression: from serotonin to kynurenine. Psychoneuroendocrinology 2011; 36:426–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Milaneschi Y, Corsi AM, Penninx BW, et al. Interleukin-1 receptor antagonist and incident depressive symptoms over 6 years in older persons: the InCHIANTI study. Biol Psychiatry 2009; 65:973–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guevara M, Baccaro ME, Gomez-Anson B, et al. Cerebral magnetic resonance imaging reveals marked abnormalities of brain tissue density in patients with cirrhosis without overt hepatic encephalopathy. J Hepatol 2011; 55:564–573. [DOI] [PubMed] [Google Scholar]
- 58.Ozcan ME, Gulec M, Ozerol E, et al. Antioxidant enzyme activities and oxidative stress in affective disorders. Int Clin Psychopharmacol 2004; 19:89–95. [DOI] [PubMed] [Google Scholar]
- 59.Hotamisligil GS. Inflammation and metabolic disorders. Nature 2006; 444:860–867. [DOI] [PubMed] [Google Scholar]
- 60.Patten SB, Williams JV, Lavorato DH, et al. A longitudinal community study of major depression and physical activity. Gen Hosp Psychiatry 2009; 31:571–575. [DOI] [PubMed] [Google Scholar]
- 61.Shannon A, Alkhouri N, Carter-Kent C, et al. Ultrasonographic quantitative estimation of hepatic steatosis in children with NAFLD. J Pediatr Gastroenterol Nutr 2011; 53:190–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sorensen M, Andersen ZJ, Nordsborg RB, et al. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ Health Perspect 2013; 121:217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]


