Supplemental Digital Content is available in the text
Keywords: minimally invasive breast reconstruction, laparoscopy, latissimus dorsi flap
Abstract
Backgroud:
An important drawback of the traditional technique for harvesting latissimus dorsi (LD) myocutaneous flap is a long, posterior donor-site incision. Current techniques involve endoscopic or robotic harvesting via a combined approach of open and closed surgery, which necessitates an open axillary incision and the use of special retractors. In this paper, we introduce a fully enclosed laparoscopic technique for harvesting LD flap (LDF) using only 3 small trocar ports. This technique eliminates the need for axillary and donor-site incisions and specialized retractors and considerably reduces the incision size.
Methods:
We performed laparoscopic harvesting of LDF with prosthesis implantation for immediate breast reconstruction (IBR) after nipple-sparing mastectomy in 2 patients with malignant breast neoplasm who wished to avoid a long scar on the back.
Results:
IBR using this technique was uneventful in both cases, without any donor-site complications or flap failure. Both patients were satisfied with the esthetic results of the procedure, especially the absence of a visible scar on the back.
Conclusion:
Enclosed laparoscopic harvesting of LDF is simpler and less invasive than the traditional methods. These preliminary results warrant further evaluation in a larger population to validate the benefits of this technique.
1. Introduction
The use of the latissimus dorsi (LD) myocutaneous flap (LDMF) for breast reconstruction was first described by Schneider et al in 1977.[1] This muscle is highly effective for the replacement of the excised volume owing to its reliable and consistent vascularity.[2] However, the process of harvesting LDMF results in a long scar on the back, which is unacceptable to most breast cancer patients.[3]
Therefore, there is definitely a pressing need for minimally invasive techniques for harvesting LD flap (LDF). Lately, endoscopic or laparoscopic techniques of flap transfer for tissue reconstruction have gained widespread popularity. In fact, endoscopic breast reconstruction has been demonstrated to be feasible without any compromise in therapeutic results.[4] Many approaches have been described for the endoscopic or robotic harvesting of LDF for immediate breast reconstruction (IBR) without the long scar on the back.[5–7] However, these approaches involve a combination of open and closed procedures performed under direct or indirect vision, using several retractors. Furthermore, these procedures necessitate an extended open vertical incision in the axilla for the dissection of the LD muscle.
In this paper, we describe and discuss the esthetic outcome of a fully laparoscopic technique that is completed as a closed procedure, thereby eliminating the need for open surgery. We present 2 cases of total laparoscopic harvesting of LDF performed using 3 small trocar ports, in combination with prosthesis implantation for IBR after nipple-sparing mastectomy (NSM).
2. Methods
The preoperative surgical designing and anatomical markings are completed with the patient standing. The following borders of the LD muscle are marked: the anterior border, along the posterior axillary line to the iliac crest; the superior border, from the tendinous insertion along tip of the scapula to the posterior border; and the posterior border, along a distance of 3 cm lateral to the spine. Three trocar ports are marked (Fig. 1). The upper trocar is placed in the anterior axillary line parallel to the nipple crossing. A middle trocar port is located 2 cm below the inframammary fold, along the anterior axillary line. The lower trocar port is placed 5 cm superior to the posterior superior iliac spine, along the posterior axillary line. An appropriate distance should be maintained between the trocars to prevent conflict of laparoscopic instruments during the operation. Before the start of the operation, the location of the thoracodorsal pedicle is marked under ultrasound Doppler guidance.
Figure 1.

Preoperative planning. The borders of latissimus dorsi muscle are marked according to the anatomic landmarks, and 3 trocar ports are marked as follows: 1 trocar port (A) is placed in the anterior axillary line parallel to the nipple crossing; another (B) is placed 2 cm below the inframammary fold along the anterior axillary line; and the third (C) is placed 5 cm superior to posterior superior iliac spine along the posterior axillary line.
After NSM, the breast incision is closed temporarily, and the patient's position is changed from supine to prone. The trocars are then placed at the marked points: a zero-degree endoscope is introduced in the upper trocar; the electrocautery apparatus (Hangzhou Kangji Medical Instruments Co., Ltd.), in the middle trocar; and a grasper (Hangzhou Kangji Medical Instruments Co., Ltd.), in lower trocar opening (Fig. 2). CO2 insufflation is applied at a pressure of 10 mm Hg to maintain the patency of the optical cavity.
Figure 2.

Laparoscopic instruments are in place. After trocar placement, a zero-degree endoscope is introduced in the right trocar; an electrocautery apparatus in the middle trocar; and grasper in the left trocar. CO2 is insufflated at a pressure of 10 mm Hg as dissection proceeds.
Dissection of the muscles is initiated along the subcutaneous plane and continued up to their borders. Next, the grasper is used to lift the anterior edge of the LD muscle toward the chest wall, and dissection is continued below the surface of the muscle. To minimize the possibility of postoperative muscle atrophy, subcutaneous fat attached to the muscle should be preserved as much as possible (see Video, Supplemental Video, which shows the laparoscopic technique for LDF harvest). Once dissection is complete in both the superficial and deep planes, an ultrasound knife is used to free the muscle at its inferoposterior border. After the muscle is excised, the flap is harvested and gathered toward the axilla. It is then transferred as a pedicled flap from the axilla and passed onto the NSM space in preparation for a change to the supine position. Since no incision is made in the axilla, it is crucial that the location of the thoracodorsal pedicle be marked by ultrasound Doppler before surgery, to avoid inadvertent injury to the pedicle when the dissection approaches the axilla. Subsequently, all trocars are undocked, and drains are placed through the 3 trocar sites.
3. Case reports and results
3.1. Case 1
The patient was a 40-year-old woman with a single, firm, painless nodule in the upper outer quadrant of left breast who had undergone left breast lumpectomy and was diagnosed with invasive ductal carcinoma. The patient expressed her explicit desire to undergo restoration of the excised breast tissue. Accordingly, we performed laparoscopic harvesting using LDF after NSM and augmentation mammoplasty of bilateral breasts with prosthesis (left, 160 mL; right, 220 mL). The duration of the enclosed laparoscopic harvesting procedure was 161 minutes, and total blood loss was 150 mL.
3.2. Case 2
The patient was a 39-year-old woman with a single, progressive increscent mass in the upper inner quadrant of right breast who had undergone breast lumpectomy and was diagnosed with spindle-type periductal stromal sarcoma of the right breast. She also underwent laparoscopic harvesting of LDF and prosthesis (right, 225 mL) implantation for breast reconstruction after NSM. Enclosed laparoscopic harvesting time was 180 minutes, and total blood loss was 100 mL.
Neither of the patients developed any complications related to the muscle flap such as flap loss, fat necrosis, seroma formation, or thermal injuries of the skin. Neither patient had scarring of the back or scarring in the axillary aspect, unlike other patients who develop significant scars on the back and axilla after LDMF transfer with the traditional method. The 3 ports created for the trocars along the anterior axillary and posterior axillary lines were barely noticeable, and both the patients and the medical staff found that the appearance of the breast in terms of shape, size, and symmetry was satisfactory (Figs. 3 and 4).
Figure 3.

Patient 1. Postoperative view 5 months. (A) and (B) There is little appreciable difference on the back, compared to the other patient with a long donor-site scar who underwent the traditional latissimus dorsi flap harvesting technique for breast reconstruction. (C) and (D) The appearance of the breasts after reconstruction and cosmetic augmentation is better than that before the correction. (E) and (F) Scars of the 3 trocar ports along the anterior axillary line and posterior axillary line are barely noticeable.
Figure 4.
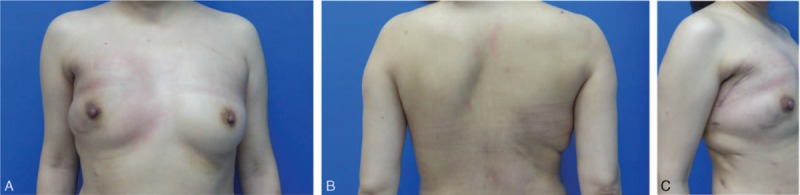
Patient 2. Postoperative view 2 months. The esthetic outcome is acceptable since scars of only 3 trocar ports along the anterior axillary line or posterior axillary line and mastectomy incision are visible.
4. Discussion
Presently, LD muscle is a workhorse flap for breast reconstruction and accounts for 60.8% of all breast reconstruction surgeries performed in Southern China.[2] Several techniques have been described in the past for the endoscopic or robotic harvesting of LDF for IBR, without the need for a long incision on the back. An endoscopic and a video-monitor-assisted technique of harvesting LDF for breast reconstruction was first reported in detail from Japan in 1998.[8] Yang et al[9] reported a technique for LDF transfer via the mastectomy incision and axillary incision under endoscopic guidance. Although both these techniques have the advantage of no scarring on the back, various specific retractors are necessary for the procedure because of the narrow operative view and difficulty in the resection of the distant LD muscle near its paravertebral origin or iliac bone.[9] Missana and Pomel[5] and Pomel et al[10] reported endoscopic harvesting of LDF by using laparoscopic instruments, but their methods necessitate a long incision anterior to the LD performed under direct vision. Selber et al[7] and Chung et al[6] reported techniques for the robotic harvesting of LDF. However, the disadvantages of this approach are that LDF is removed and transferred via an extended axillary incision and the procedure requires various special retractors since it is a combination of both open and closed techniques.
During the last decade, there has been a worldwide increase in the use of acellular dermal matrix (ADM) as an adjunct to implant-based breast reconstruction (IBBR).[11,12] ADM-assisted IBBR helps augment the subpectoral space and create inferolateral implant coverage.[13] However, although it affords a shorter operative time and shorter hospital stay than LDF reconstruction, ADM-assisted IBBR has a higher likelihood of complications than non-ADM breast reconstructions, including IBBR using LD muscle onlay patch.[14,15] In addition, cosmetic outcomes for breast symmetry and shape were higher with LD muscle onlay patch than with ADM.[14] Presently, ADM has not yet been applied in most medical institutions, including our hospital in China, because it is expensive and is not covered by the country's medical insurance.[12,16] We believe that laparoscopic harvesting of LDF procedure is a feasible technique for breast reconstruction, especially in those patients who cannot afford ADM. Nevertheless, long-term evaluation is required to compare the benefits of laparoscopic harvesting of LDF for IBBR and ADM-based reconstruction.
In this paper, we present a novel enclosed laparoscopic technique for LDF harvesting, which offers the following advantages over previous techniques: For the entire harvesting procedure, only 3 small trocar ports are necessary, which greatly minimizes the total size of the incisions. The scars of the trocar ports are barely noticeable after recovery. The entire visual field of operation is clear, and the entire LDF can be seen clearly. The flap can be easily resected in whole or part during the surgery, depending on the individual case. Further, the 3 ports created for the trocars are also used for postoperative drainage, thereby eliminating the need for additional incisions. The flap could be dissected and transferred by a totally laparoscopic approach without an axillary incision or the use of any specialized retractors. Avoiding the axillary incision minimizes the chances of injury to the thoracodorsal pedicle.
The main disadvantage of the enclosed laparoscopic technique for LDF transfer is that it does not include the skin, making the flap volume less than that achieved with the flap from the traditional technique. Moreover, during the procedure, care must be taken when the dissection approaches the axilla, although the location of the thoracodorsal pedicle is marked before the operation under ultrasound Doppler guidance. Finally, a certain level of expertise in laparoscopic surgery is required on the part of the surgeon to ensure the safety of the procedure and shorten the operative time.
In conclusion, we have described a feasible and reproducible technique for enclosed laparoscopic harvesting of LDF. The esthetic outcome with this technique is much better than that with the open technique. This method is especially suitable for young patients, particularly those who do not wish to have scarring of their back. The technique is compatible with both implant-based reconstruction and partial breast reconstruction. Further studies are necessary to validate the feasibility of this technique and determine strategies to improve patient satisfaction and reconstructive outcome. The application of minimally invasive techniques in breast reconstructions has many advantages, and minimally invasive breast reconstruction is expected to be a popular trend in the future.
Supplementary Material
Footnotes
Abbreviations: ADM = acellular dermal matrix, IBBR = implant-based breast reconstruction, IBR = immediate breast reconstruction, LD = latissimus dorsi, LDF = latissimus dorsi flap, LDMF = latissimus dorsi myocutaneous flap, NSM = nipple-sparing mastectomy.
Ethical statement: The study was approved by the Ethical Committee of the Third Military Medical University and the Hospital Clinic Ethics Review Committee. Written informed consent was obtained from the patients involved in the study.
Funding/support: This work was supported by Grants from the National Natural Science Foundation of China (No. 81372813).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- 1.Schneider WJ, Hill HL, Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg 1977; 30:277–281. [DOI] [PubMed] [Google Scholar]
- 2.Jia-Jian C, Nai-Si H, Jing-Yan X, et al. Current status of breast reconstruction in southern China: a 15 year, single institutional experience of 20,551 breast cancer patients. Medicine (Baltimore) 2015; 94:e1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey S, Saint-Cyr M, Zhang K, et al. Breast reconstruction with the latissimus dorsi flap: women's preference for scar location. Plast Reconstr Surg 2010; 126:358–365. [DOI] [PubMed] [Google Scholar]
- 4.Leff DR, Vashisht R, Yongue G, et al. Endoscopic breast surgery: where are we now and what might the future hold for video-assisted breast surgery? Breast Cancer Res Treat 2011; 125:607–625. [DOI] [PubMed] [Google Scholar]
- 5.Missana MC, Pomel C. Endoscopic latissimus dorsi flap harvesting. Am J Surg 2007; 194:164–169. [DOI] [PubMed] [Google Scholar]
- 6.Chung JH, You HJ, Kim HS, et al. A novel technique for robot assisted latissimus dorsi flap harvest. J Plast Reconstr Aesthet Surg 2015; 68:966–972. [DOI] [PubMed] [Google Scholar]
- 7.Selber JC, Baumann DP, Holsinger FC. Robotic latissimus dorsi muscle harvest: a case series. Plast Reconstr Surg 2012; 129:1305–1312. [DOI] [PubMed] [Google Scholar]
- 8.Masuoka T, Fujikawa M, Yamamoto H, et al. Breast reconstruction after mastectomy without additional scarring: application of endoscopic latissimus dorsi muscle harvest. Ann Plast Surg 1998; 40:123–127. [DOI] [PubMed] [Google Scholar]
- 9.Yang CE, Roh TS, Yun IS, et al. Immediate partial breast reconstruction with endoscopic latissimus dorsi muscle flap harvest. Arch Plast Surg 2014; 41:513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pomel C, Missana MC, Atallah D, et al. Endoscopic muscular latissimus dorsi flap harvesting for immediate breast reconstruction after sparing mastectomy. Eur J Surg Oncol 2003; 29:127–131. [DOI] [PubMed] [Google Scholar]
- 11.Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral alloderm slings. Ann Plast Surg 2005; 55:232–239. [DOI] [PubMed] [Google Scholar]
- 12.Vu MM, Kim JY. Current opinions on indications and algorithms for acellular dermal matrix use in primary prosthetic breast reconstruction. Gland Surg 2015; 4:195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Potter S, Browning D, Savović J, et al. Systematic review and critical appraisal of the impact of acellular dermal matrix use on the outcomes of implant-based breast reconstruction. Br J Surg 2015; 102:1010–1025. [DOI] [PubMed] [Google Scholar]
- 14.Lee J, Bae Y. Use of latissimus dorsi muscle onlay patch alternative to acellular dermal matrix in implant-based breast reconstruction. Gland Surg 2015; 4:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ho G, Nguyen TJ, Shahabi A, et al. A systematic review and meta-analysis of complications associated with acellular dermal matrix-assisted breast reconstruction. Ann Plast Surg 2012; 68:346–356. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Chen J, Chen J, et al. Current trends of breast reconstruction after mastectomy for breast cancer patients in China: a survey report. Zhonghua Zhong Liu Za Zhi 2014; 36:851–857. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


