Abstract
Objective
The purposes of this paper are to describe the internal consistency reliability and construct validity of the PAM-13 for hospitalized cardiology and oncology patients and to examine the predictors of low patient activation in the same population.
Methods
We evaluated the internal consistency reliability of the PAM-13 in the inpatient setting. Construct validity of the PAM-13 was then assessed using two approaches: expected known-groups differences between patients with planned and unplanned admissions PAM-13 levels and convergence of PAM-13 levels with other measures.
Results
The PAM demonstrated adequate internal consistency overall (Cronbach α = 0.81). Patients with unplanned admissions were more likely to have low activation than patients with planned admissions (adjusted OR = 5.7, p = 0.008). The PAM-13 was modestly correlated (p < 0.001) with each of the PROMIS Global Health components used in this study (global, physical and mental health).
Conclusion
This study demonstrates the PAM-13 is a reliable and valid measure for use in the inpatient hospital setting and that type of admission (planned versus unplanned) is an important predictor of patient activation.
Practice Implications
By measuring patient activation with the PAM-13, clinicians and researchers can provide tailored communication and care strategies to meet patient’s needs.
Keywords: patient engagement, patient activation, validation, known-group analysis, inpatient, clinical informatics
1. INTRODUCTION
The concept of “patient engagement” has become increasingly important in recent years [1]. Patient engagement is a construct that includes self-efficacy, behavior, and knowledge, and has been shown to predict a variety of health behaviors [2]. Engaging patients in their care is the focus of many public- and private-sector initiatives and programs [3–5]. There is no single definition of patient engagement, nor is there a universally agreed-upon tool for measuring this concept. To date, the most frequently used instrument for measuring patient engagement is the Patient Activation Measure (PAM) [6–9].
The PAM-13 is a 13-item self-reported measure designed to assess patients’ knowledge, skills and confidence in managing their health. The PAM-13 also describes the extent to which patients are informed and involved in their healthcare [6]. The PAM-13 has been validated in multiple outpatient populations including multi-morbid older adults and multiple sclerosis patients, and in relation to employee health characteristics [10–12]. It has strong psychometric properties, with high internal consistency and construct validity [10–12]. Recent studies involving the PAM have found that higher patient activation levels were correlated with improved health outcomes over time including better clinical indicators (e.g., not being obese, having high-density lipoprotein and triglycerides in normal ranges), more healthy behaviors, better self-management, greater use of preventive screening tests, and lower use of costly healthcare services [13,14].
While the PAM has become a widely used tool in outpatient care settings, its applicability to patients in the hospital is not well established [15]. Validating the PAM-13 in the inpatient setting is important as there are over 35 million hospital admissions each year [16] and interventions to impact patient engagement in the hospital are becoming more commonplace [8,17–19]. The purposes of this paper are 1) to describe the psychometric properties (internal consistency reliability and construct validity) of the PAM-13 for hospitalized cardiology and oncology patients with planned and unplanned admissions; and 2) conduct an exploratory analysis to examine the predictors of low activation in the same population.
2. METHODS
2.1 Study design
We first evaluated the internal consistency reliability of the PAM-13 in the inpatient setting. The construct validity of the PAM-13 was then assessed using two approaches: expected known-groups differences of PAM-13 levels and convergence of PAM-13 levels with other measures.
The purpose of validation using known-group differences was to systematically evaluate whether the PAM-13 instrument would discriminate between two known groups (unplanned admissions versus planned admissions) expected to differ on the constructs that the instrument is intended to measure [20–22]. These groups were chosen based on the hypothesis that patients with a planned hospitalization would have a higher PAM level (reflecting higher activation) than patients with an unplanned admission. The rationale behind this assumption was that patients who have planned admissions are more likely to be actively managing their healthcare and have been able to schedule the procedures and treatments for their care ahead of their admission. We believed these patients would be different than those admitted through the emergency department with an unplanned admission for an emergent problem. Additionally, we hypothesized that this difference would be apparent among both cardiology and oncology patients.
We examined convergent validity by correlating the PAM-13 levels with quality of life measures, specifically, the Patient Reported Outcomes Measurement Information System (PROMIS) Global Health short form scores [23]. We conjectured that participants with higher activation levels would also have higher mental and physical quality of life scores. Our hypothesis was that these quality of life measures would be positively correlated with the PAM-13 level. This hypothesis was based on prior findings of modest correlation between the PAM-13 and a multiple sclerosis quality of life measure (r= 0.42) [10].
We also conducted an exploratory analysis to examine predictors of low activation according to PAM-13 levels and scores. We tested for differences by age, education, health literacy and primary clinical service lines (oncology and cardiology) based on prior literature [7,10,11,24]. We then compared the PAM-13 levels found in this inpatient study to those previously reported in other settings.
2.2 Subjects
We performed the evaluation of known-group differences based on data collected from 100 participants continuously recruited from cardiology and oncology units at a large, urban, academic medical center. This sample size was chosen based on previous literature regarding validation of measures [25]. Criteria for inclusion were 18 years or older and English speaking. Exclusion criteria were inability to perform the interview in English, and severe cognitive or psychiatric impairment. Participants were compensated $10 for their time, typically around 15 minutes. Participants provided written informed consent, and were instructed that their participation was completely voluntary, there were no right or wrong answers, and they were free to skip any questions if they did not feel comfortable answering them. Additionally, they were informed that participation would have no bearing on their clinical care. These steps were taken to ensure the survey was administered without undue influence from the investigators. The research protocol and written informed consent form describing the study and compensation were approved by the medical center’s Institutional Review Board.
In total, 50 cardiology participants (25 planned and 25 unplanned admissions) and 50 oncology participants (25 planned and 25 unplanned admissions) were recruited from July to October 2015. On the cardiology service, recruitment for planned admissions was conducted among those patients with a known disease (e.g., aortic stenosis) undergoing a planned heart valve repair or replacement (e.g., a transcatheter aortic valve replacement). Unplanned cardiology participants came through the hospital’s emergency department and were diagnosed with ST-segment elevation myocardial infarction, non-ST segment elevation myocardial infarction, or acute coronary syndrome. On the oncology unit, the planned-admission participants came in for chemotherapy or another planned treatment. Unplanned oncology participants came through the hospital’s emergency department and were admitted with diagnoses such as fever and respiratory failure.
2.3 Data Collection
Each participant’s admission status of planned versus unplanned was collected by reviewing the electronic health record (EHR). Data were collected by surveying each participant and storing the results in a secure database. Participants elected whether to be asked the questions orally by the research coordinator, or to respond directly to the survey using a tablet computer provided to them by the research coordinator.
2.4 Measures
2.4.1 Sample characteristics
Sample characteristics were collected through a demographic form completed at enrollment. These questions included information on age, gender, race, ethnicity, education level, and technology use. Technology-use questions asked about the patient’s experience using the internet (“Do you access the internet?”; yes or no), what devices they used to access the internet (“How do you access the internet (select all that apply)”; desktop, laptop, smartphone, tablet, other), and how much they used the internet on a daily basis (“Typically, how much do you use the internet on a given day?”; less than 30 minutes, 1-2 hours, 3-4 hours, 5 or more hours). Income was measured with the question, “Financially, would you say you are… comfortable; have enough to make ends meet; or do not have enough to make ends meet?” as traditional questions using numerical income scales have been fraught with a wide range of bias [26] and random error [27].
2.4.2 Patient activation
Patient activation, was measured using the PAM-13. The responses to each of the 13 items range from 1 (strongly disagree) to 4 (strongly agree). Scores were calculated by summing the responses, weighted to a scale of 0 to 100, and then converting the score to a PAM level (1-4) using the PAM scoring spreadsheet. The four PAM levels are 1) Disengaged and overwhelmed (indicated by a score of 0.0-47.0) 2) Becoming aware, but still struggling (47.1-55.1), 3) Taking action (55.2-72.4), and 4) Maintaining behaviors and pushing further (72.5-100).
2.4.3 Quality of life
Quality of life was measured using the 10-item Patient Reported Outcomes Measurement Information System (PROMIS) Global Health short form questionnaire [28]. PROMIS was developed to provide instruments that allow for the efficient, flexible, and precise measurement of patient-reported outcomes [23]. The Global Health short form includes mental and physical health components as well as a single item on general health status, “In general would you say your health is…”. Participants respond to each item using a 5-item Likert-type scale. Previous tests of construct validity for the PAM have shown strong associations with other functional status (SF-36[29] and SF-12[30]) measures. We chose to use the PROMIS questionnaires because they are freely available and capture the same information as legacy measures with fewer items [23,31].
2.4.4 Health Literacy
Study participants answered three health literacy questions developed by Chew et al. [32]. These questions facilitate the identification of patients with “inadequate health literacy.” Each question has differing sensitivity and specificity based on the cutoff selected by the researchers. Cutoffs were selected to optimize the sensitivity and specificity tradeoff based on the findings of Chew and colleagues [32].
2.5 Statistical Analysis
Baseline characteristics of participants in the planned and unplanned admission groups were compared using two-sample t-tests for continuous variables and chi-squared tests for categorical variables.
Internal consistency (reliability) of the PAM was assessed using Cronbach’s alpha. An alpha of at least 0.80 was considered evidence of good internal consistency.
Construct validity was evaluated through a known-group differences analysis of the PAM levels between planned and unplanned admissions. PAM levels were dichotomized into ‘low activation’ (PAM levels 1 and 2), and ‘high activation’ (PAM levels 3 and 4). The known groups were then analyzed using a chi-square test. Logistic regression was used to determine the odds ratio of having low activation between the known groups (unplanned versus planned admissions). We conducted forward and backward step-wise selection using all collected variables (with entry and removal criterion of p = 0.2) to identify those variables associated with low activation. Collinearity between related variables was analyzed, with small correlations (r < 0.3) found between variables included in the model.
To analyze differences across service lines (cardiology versus oncology), the median PAM-13 levels between unplanned versus planned admissions were compared using Wilcoxon rank-sum tests, and the proportions of ‘low activation’ were compared using chi-squared tests. In addition, we also compared average PAM-13 scores (0-100) between services lines and admission type again using a Wilcoxon rank-sum test.
Convergent validity was assessed by correlating the PAM-13 with the PROMIS Global Health short form measures. A Spearman rank correlation between each of the PROMIS Global Health measures and the four PAM-13 levels was calculated. This correlation was also completed using the continuous PAM-13 scores. We also conducted an ANOVA to determine the strength of the association between the PROMIS scores and activation level.
Predictors of low activation and PAM-13 scores were analyzed through chi-square tests for categorical variables and ANOVA for continuous variables. All baseline demographic data was included in the analysis.
PAM levels from the inpatient setting were compared with four published studies in other settings [10,24,33,34] using Wilcoxon rank-sum tests. The four studies that were selected reported sample size and the distribution of participants across the four PAM-13 levels.
Analyses were completed using STATA version 14 [35] and R version 3.0.2 [36].
3. RESULTS
Participant characteristics are described in Table 1. The average age in our cohort was 64 years, (range = 22-102). The majority of the participants were male (65%), 13% were black, 9% were Asian, 9% reported their race as “other” or were multi-racial, and 16% were Hispanic/Latino. Almost one-fifth (18%) of the participants reported their income level as “not having enough money to make ends meet”.
Table 1.
Baseline demographics and analysis of predictors of low activation
| Variable |
Overall n=100 |
Low Activation n=40 |
High Activation n=60 |
p-value |
|---|---|---|---|---|
| Age | 64.1 (1.69) | 65.7 (16.0) | 63.1 (17.6) | 0.447 |
| Gender, Female | 35 (35%) | 12 (30%) | 23 (38%) | 0.392 |
| Service | 0.221 | |||
| Cardiology | 50 (50%) | 23 (57.5%) | 27 (45%) | |
| Oncology | 50 (50%) | 17 (42.5%) | 33 (55%) | |
| Country of Origin* | 0.530 | |||
| Dominican Republic or Puerto Rico | 7 (7%) | 3 (7.5%) | 3 (5%) | |
| United States | 72 (72%) | 27 (67.5%) | 45 (75%) | |
| Other | 20 (20%) | 10 (22%) | 11 (18.3%) | |
| Education | 0.832 | |||
| Some high school or less | 11 (11%) | 5 (12.5%) | 6 (10%) | |
| High School, some college, or Associate’s degree |
51 (51%) | 19 (47.5%) | 32 (53.3%) | |
| College or more | 38 (38%) | 16 (40%) | 22 (36.7%) | |
| Race | 0.769 | |||
| Asian or Pacific Islander | 9 (9%) | 5 (12.5%) | 4 (6.67%) | |
| Black or African American | 13 (13%) | 5 (12.5%) | 8 (13.3%) | |
| Other, multi-race, or prefer not to answer |
14 (14%) | 6 (15%) | 8 (13.3%) | |
| White | 64 (64%) | 24 (60%) | 40 (66.7%) | |
| Ethnicity | ||||
| Hispanic, Latino or Spanish Origin | 16 (16%) | 6 (15%) | 10 (16.7%) | 0.215 |
| Income | 0.948 | |||
| Comfortable | 50 (50%) | 21 (52.5%) | 29 (49.2%) | |
| Have enough to make ends meet | 31 (31%) | 12 (30%) | 19 (32.2%) | |
| Do not have enough to make ends meet | 18 (18%) | 7 (17.5%) | 11 (18.6%) | |
| Participants with Inadequate Health Literacy |
||||
| 1. How confident are you filling out medical forms by yourself? |
38 (38%) | 18 (45%) | 20 (33.3%) | 0.239 |
| 2. How often do you have problems learning about your medical condition because of difficulty understanding written information? |
14 (14%) | 8 (20%) | 6 (10%) | 0.158 |
| 3. How often do you have someone help you when you read hospital materials? |
30 (30%) | 15 (37.5%) | 15 (25%) | 0.181 |
| Technology Use | ||||
| Yes, I use the internet | 68 (68%) | 26 (65%) | 42 (70%) | 0.600 |
| Length of daily internet use (of internet users) |
0.433 | |||
| Less than 30 minutes | 27 (39.7%) | 11 (27.5%) | 16 (26.7%) | |
| 1-2 hours a day | 17 (25%) | 9 (22.5%) | 8 (13.3%) | |
| 3-4 hours a day | 14 (20.6%) | 4 (10%) | 10 (16.7%) | |
| 5 or more hours a day | 10 (14.7%) | 2 (5%) | 8 (13.3%) | |
| Use IT to look up health information | ||||
| Yes | 57 (57%) | 22 (55%) | 35 (58.3%) | 0.742 |
| Family member looks up health information online |
63 (63%) | 28 (70%) | 35 (58.3%) | 0.236 |
| Device use (of those who use the internet) |
||||
| Desktop | 38 (56%) | 13 (32.5%) | 25 (41.7%) | 0.355 |
| Laptop | 32 (47%) | 15 (37.5%) | 17 (28.3%) | 0.336 |
| Smartphone | 33 (49%) | 12 (30%) | 21 (35%) | 0.602 |
| Tablet | 21 (31%) | 4 (10%) | 17 (28.3%) | 0.027 |
Abbreviations: SD: standard deviation, n: number
For continuous variables, mean (SD) were reported, and p-values were calculated using two sample t-tests. For categorical variables, n (%) were reported, and p-values were calculated using chi-squared tests.
Percentages do not add to 100% as not all participants provided a response.
3.1 Psychometric results (Reliability, construct and convergent validity)
The PAM demonstrated adequate internal consistency overall (Cronbach α = 0.81).
We found a statistically significant difference in the PAM-13 levels of participants who had planned compared to unplanned admissions. Among participants with unplanned admissions, 56% had low activation compared to 24% of participants with planned admissions (p = 0.001). This difference confirmed our hypothesis that the PAM-13 instrument is able to differentiate between the two known groups. Overall, patients with unplanned admissions were more likely to have low activation compared to patients with planned admissions (unadjusted OR = 4.03, p = 0.001) (Table 2). The difference remained significant after adjustment for baseline covariates (adjusted OR = 5.7, p = 0.008). The final model included age, gender, race, ethnicity, education, income, and use of a tablet computer to access the internet (Table 2).
Table 2.
Logistic regression model of predictors of low activation
| OR | 95% CI | |
|---|---|---|
| Model 1 | ||
| Unplanned/planned | 4.03 | 1.71 – 9.49* |
|
| ||
| Model 2 | ||
| Unplanned/planned | 5.72 | 2.06-15.9* |
| Age | 1.01 | .98-1.05 |
| Race (White versus Non-White) | 1.30 | .44-3.82 |
| Income† (Reference: Comfortable) | 1.29 | .65-2.57 |
| Ethnicity (Not-Latino versus Latino) | 1.43 | .46-4.46 |
| Gender (Male versus Female) | .49 | .18-1.32 |
| Education† (Reference: Some high school or less) | .95 | .45-1.97 |
| Tablet (No tablet use versus tablet use) | 0.33 | .59-1.28 |
statistically significant at p < 0.05
Categories as described in Table 1
There was a higher proportion of participants with low activation in the unplanned admission group. This finding was consistent across both the oncology and cardiology service lines (p = 0. 007, and p = 0. 047, respectively). Both the median (interquartile range) PAM-13 levels and mean (standard deviation) PAM-13 scores were lower in the unplanned admission group (Table 3). There was no statistically significant difference in PAM-13 level between oncology and cardiology service lines.
Table 3.
PAM-13 levels and scores by service and admission type
| Unplanned PAM-13 Level* |
Planned PAM-13 Level* |
p-value | Unplanned PAM-13 Score† |
Planned PAM-13 Score† |
p-value | |
|---|---|---|---|---|---|---|
|
Overall
(n=100) |
2 (2-3) | 3 (3-4) | 0.001 | 57.0 (12.6) | 66.2 (13.4) | 0.002 |
|
| ||||||
|
Cardiology
(n=50) |
2 (2-3) | 3 (2-4) | 0.032 | 57.0 (12.0) | 65.9 (14.7) | 0.021 |
|
Oncology
(n=50) |
2 (2-3) | 3 (3-4) | 0.012 | 57.1 (13.4) | 66.5 (12.2) | 0.005 |
| 0.221‡ | 0.888‡ | |||||
Median (IQR) are reported, p-values were calculated using Wilcoxon-rank sum tests.
Mean (SD) are reported, p-values were calculated using Wilcoxon-rank sum tests.
Difference between cardiology/oncology overall
The PAM-13 was modestly correlated (p < 0.001) with each of the three PROMIS Global Health components used in this study (global, physical and mental health) (Table 4). Analysis of correlations using the PAM-13 scores (instead of levels) were consistent. The results of the ANOVA comparing PROMIS global, physical and mental quality of life measures across participants with low and high activation demonstrated that lower scores on PROMIS measures were associated with low activation (Table 5).
Table 4.
Correlations between PAM and PROMIS measures
| n = 96 |
PAM Level r (p-value) |
PROMIS Global
Health |
PROMIS
Physical Health |
PROMIS Mental
Health |
|---|---|---|---|---|
| PAM Level | --- | |||
|
PROMIS Global
Health |
0.4003 (0.0001) | --- | ||
|
PROMIS Physical
Health * |
0.396 (0.0001) | 0.660 (<0.0001) | --- | |
|
PROMIS Mental
Health * |
0.447 (<0.0001) | 0.4307 (<0.0001) | 0.437 (<0.0001) | --- |
Correlations and p-values were calculated using a Spearman Rank correlation.
Measures were converted into T-scores prior to analysis
Table 5.
Associations between PROMIS measures and PAM levels
| PROMIS measures | Low-PAM | High-PAM | p-value |
|---|---|---|---|
| Global health question† | 2.05 (0.75) | 2.66 (1.04) | 0.0019 |
| Physical health* | 37.6 (8.42) | 42.98 (8.84) | 0.0033 |
| Mental health* | 41.5 (6.54) | 46.1 (6.11) | 0.0006 |
Mean (SD) were reported, and p-values were calculated using one-way ANOVA.
Failed Bartlett’s test for homoscedasticity, unequal variances across groups
PROMIS measures are reported as T-scores
3.2 Identifying predictors of low activation
Differences across demographic variables between participants with low and high activation are described in Table 1. There was a difference between the proportion of patients who had low and high activation by the use of a tablet computer to access the internet (p = 0.027), however it was no longer significant when included in the stepwise logistic regression model. When using the continuous PAM-13 scores, statistically significant differences were found using logistic regression by use of a tablet computer (OR = 1.04, 95% CI = 1.00 – 1.07, p = 0.043) and a significant difference was found using a linear regression model by the mean number of participants with inadequate health literacy (based on the health literacy question, “How often do you have problems learning about your medical condition because of difficulty understanding written information?”) (β = −0.005, 95% CI = −0.010 – −0.0002,_p = 0.043) were found.
3.3 Comparison to outpatient studies
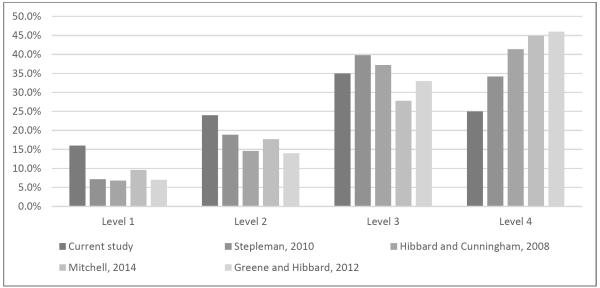
The PAM-13 levels of our patient population were significantly lower than the PAM-13 levels of the four other PAM-related studies we included (Figure 1, Table 6). The four studies included three studies in the outpatient setting (a study in a multiple sclerosis clinic in the southeastern U.S.[10], a national survey [24], and a study in primary care clinics in Minnesota [34]), and one inpatient study of cardiac patients in Boston [33]. Sample sizes ranged from 196 to over 25,000.
Figure 1.
PAM-13 levels across studies
Table 6.
Comparison of outpatient PAM-13 levels to our inpatient PAM-13 levels
| Individual Studies | Sample Size | PAM-13 level Mean (SD) |
p-value* |
|---|---|---|---|
|
| |||
| Stepleman, 2010 | 196 | 3.01 (0.91) | 0.005 |
| Hibbard and Cunningham, 2008 | 17,800 | 3.13 (0.90) | <0.0001 |
| Mitchell, 2014 | 695 | 3.08 (1.00) | <0.0001 |
| Greene and Hibbard, 2012 | 25,047 | 3.18 (0.92) | <0.0001 |
p-value of comparison of each study with our PAM-13 levels based on Wilcoxon rank-sum test.
The mean (SD) of this inpatient PAM study was 2.69 (1.02).
4. DISCUSSION AND CONCLUSION
4.1 Discussion
This study provides evidence for the internal consistency reliability and the construct validity of the PAM-13 instrument for use in the inpatient setting. The study also confirms that type of admission is important to consider when analyzing PAM levels. There was a significant difference in PAM levels between hospitalized patients with unplanned compared to planned admissions, no differences in the PAM levels between cardiology and oncology service lines, and specific demographic variables were not predictive of low activation.
Our results complement the findings from a recent study by Schmaderer et al. [15] that documented the psychometric properties of the PAM for use in hospitalized multimorbid patients. Our results build on the Schmaderer study by demonstrating the importance of admission type in predicting low patient activation. These results are important for other researchers who are using the PAM-13 to measure patient activation in inpatient randomized controlled trials [8,17].
A study conducted by Hibbard and Cunningham,[24] suggested that patients with cancer had a slightly higher average PAM score than patients with hypertension (65.8 versus 63.5). Our study results did not identify a statistically significant difference in PAM scores between patients on our cardiology versus oncology services (61.5 versus 61.8, respectively). In contrast to our study, which was conducted in an urban, inpatient, academic setting, Hibbard and Cunningham performed a nationwide survey, with a sample size of over 17,800 participants in the outpatient setting.
Our study found a modest correlation between PAM-13 levels and quality of life (measured with the PROMIS Global Health short form), further supporting the validity of the PAM-13. The PROMIS mental health measure had the strongest correlation with activation, which was consistent with other studies that have analyzed the relationship between PAM levels and quality of life measures [10].
In the univariate analysis we found only one significant predictor of low activation we measured, not using a tablet computer to access the internet. The other demographic variables included in the final model were not significant predictors of low activation. This may be due to the small sample size and the study being underpowered to determine differences by demographics variables. One of the three questions used to identify patients with inadequate health literacy was found to be correlated with the PAM-13 scores, however we did not find it to be a predictor of low activation using the categorical PAM-13 levels. This could be due to the decrease in power using the categorical variable. However, the relationship between PAM scores and literacy is so small to not be clinically relevant. As such, we would not recommend using health literacy as a proxy measure of patient activation. Additional research by Hibbard et al.,[37] also indicates that activation is not simply a marker for socioeconomic status. These are important findings as they suggest that if someone is economically or socially disadvantaged it is not necessarily an indicator that they have low activation.
This study assessed differences between the PAM-13 levels of our hospitalized patients versus those from the literature. We found the PAM-13 levels of our hospitalized patients to be significantly lower than those in the four other studies we analyzed. One difference between our study and the others is that patients in our study were older (average age of 64.1), whereas average ages reported in the other studies ranged from 46 to 50. Our results may suggest that there could be a change in PAM levels when patients enter the hospital. Being a hospitalized patient has been called one of the most “dis-empowering situations one can experience in modern society,” [38] and this change in environment could contribute to decreasing patients’ PAM levels. Upon hospitalization, measures should be taken to address patient-specific activation during that time period.
Use of the PAM-13 in the inpatient setting could allow for a more customized approach to tailoring interventions, preparing appropriate education, and follow-up after discharge. Knowing the activation level of a patient in the hospital could support clinicians’ efforts to tailor their communication and educational materials, facilitate more productive interaction and potentially increase the patient’s knowledge and self-efficacy. For example, knowing that a patient has lower activation and needs a more thorough explanation of a medication schedule would allow for the clinician to prioritize spending that extra time with the patient while they are in the hospital. Also, knowing that a patient’s activation level may decrease upon being admitted to the hospital may help clinicians tailor communication with patients. Improved patient-provider interaction could enable patients to have a more seamless discharge process and could help to reduce future admissions.
4.1.1 Limitations
Strengths of this study are that it was conducted in a large, urban, academic medical center with a diverse population. While we did not include non-English speaking patients in our study, 16% our participants identified as Hispanic/Latino. Validation of the PAM-13 among a diverse population of hospitalized patients contributes to the generalizability of the study findings.
Additionally, this study was conducted at a single site. While the PAM-13 was valid in this setting, there is the potential that these results may not be broadly generalizable to other inpatient settings. Due to the small sample size, our analysis of predictors of low activation may have been underpowered to detect differences by all the demographic variables collected in the study.
4.1.2 Future research
Future steps for research include validating the Spanish version of the PAM in the inpatient setting and identifying interventions that are successful for improving activation for patients with low PAM scores.
4.2 Conclusion
This study demonstrates that the PAM-13 is a reliable and valid measure to be used in the inpatient setting. It has also shown that knowing the admission type is an important predictor of patient activation. Understanding a patient’s level of activation is important for being able to optimize inpatient communication. By measuring patient activation with the PAM-13, clinicians and researchers can more accurately understand their patients and provide tailored communication and care strategies to meet patients’ needs.
4.3 Practice Implications
By showing that the PAM is a reliable and valid measure of patient activation in the inpatient setting, we believe that its use in the hospital can facilitate patient-provider communication and allow for the tailoring of care to a patient’s specific activation level. This improved interaction could facilitate the improvement of patients’ clinical outcomes, including reducing readmissions and improving patients’ self-management of their own health.
Highlights.
The PAM has is a reliable and valid measure for use in the inpatient setting
Type of admission is an important predictor of patient activation
Measuring patient activation can allow for tailored care strategies in the hospital
ACKNOWLEDGMENTS
None
FUNDING
This study was funded by the Agency for Healthcare Research and Quality [R01-HS021816]. The authors gratefully acknowledge funding for Dr. Ruth Masterson Creber by the National Institute of Nursing Research (NINR) of the National Institutes of Health (NIH) under Award Number, K99NR016275, “mHealth for Heart Failure Symptom Monitoring.” Her post-doctoral funding was also funded by NIH/NINR (T32NR007969) at Columbia University School of Nursing. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors also gratefully acknowledge doctoral funding for Jennifer Prey by the National Library of Medicine [T15LM007079] through Columbia University Department of Biomedical Informatics.
Appendix A. Baseline socio-demographic and lifestyle characteristics of PAM validation participants by admission type (planned versus unplanned)
| Variable | Overall N=100 |
Unplanned N=50 |
Planned N=50 |
p-value |
|---|---|---|---|---|
| Age | 64.1 (1.69) | 59.8 (2.34) | 68.4 (2.3) | 0.010 |
| Gender, Female | 35 (35%) | 20 (40%) | 15 (30%) | 0.295 |
| Country of Origin | 0.226 | |||
| Dominican Republic or Puerto Rico | 7 (7%) | 3 (6%) | 4 (8%) | |
| United States | 72 (72%) | 33 (67%) | 39 (78%) | |
| Other | 20 (20%) | 14 (28%) | 7 (14%) | |
| Education | 0.534 | |||
| Some high school or less | 11 (11%) | 5 (10%) | 6 (12%) | |
| High School/some college | 46 (46%) | 26 (52%) | 20 (40%) | |
| College/Associate’s degree | 24 (24%) | 12 (24%) | 12 (24%) | |
| Master’s/Doctoral degree | 19 (19%) | 7 (14%) | 12 (24%) | |
| Race | 0.032 | |||
| Asian or Pacific Islander | 9 (9%) | 6 (12%) | 3 (6%) | |
| Black or African American | 13 (13%) | 10 (20%) | 3 (6%) | |
| Other or multi-race | 9 (9%) | 7 (10%) | 5 (8%) | |
| White | 64 (64%) | 23 (50%) | 38 (78%) | |
| Prefer not to answer | 5 (5%) | 4 (8%) | 1 (2%) | |
| Ethnicity | ||||
| Hispanic, Latino or Spanish Origin | 16 (16%) | 10 (20%) | 6 (12%) | 0.275 |
| Income | 0.014 | |||
| Comfortable | 50 (50%) | 18 (36%) | 32 (64%) | |
| Have enough to make ends meet | 31 (31%) | 20 (40%) | 11 (22%) | |
| Do not have enough to make ends meet | 18 (18%) | 12 (24%) | 6 (12%) | |
| Participants with Inadequate Health Literacy |
||||
| 1. How confident are you filling out medical forms by yourself? |
38 (38%) | 19 (38%) | 19 (38%) | 1.00 |
| 2. How often do you have problems learning about your medical condition because of difficulty understanding written information? |
14 (14%) | 9 (18%) | 5 (10%) | 0.249 |
| 3. How often do you have someone help you when you read hospital materials? |
30 (30%) | 15 (30%) | 15 (30%) | 1.00 |
| Technology Use | ||||
| Yes, I use the internet | 68 (68%) | 35 (70%) | 33(66%) | 0.668 |
| Length of daily internet use (of internet users) |
0.333 | |||
| Less than 30 minutes | 27 (39.7%) | 11 (31.4%) | 16 (48.5%) | |
| 1-2 hours a day | 17 (25%) | 10 (28.6%) | 7 (21.2%) | |
| 3-4 hours a day | 14 (20.6%) | 9 (25.7%) | 5 (15.2%) | |
| 5 or more hours a day | 10 (14.7%) | 5 (14.3%) | 5 (15.2%) | |
| Use IT to look up health information | ||||
| Yes | 57 (57%) | 31 (62%) | 26 (52%) | 0.313 |
| Family member looks up health information online |
63 (63%) | 30 (60%) | 33 (66%) | 0.534 |
| Device use (of those who use the internet) |
||||
| Desktop | 38 (56%) | 18 (51%) | 20 (61%) | 0.680 |
| Laptop | 32 (47%) | 16 (46%) | 16 (48%) | 0.819 |
| Smartphone | 33 (49%) | 19 (54%) | 14 (42%) | 0.288 |
| Tablet | 21 (31%) | 11 (31%) | 10 (30%) | 0.806 |
Abbreviations: SD: standard deviation, N: number
For continuous variables, mean (SD) were reported, and p-values were calculated using two sample t-tests. For categorical variables, n (%) were reported, and p-values were calculated using chi-squared tests.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COMPETING INTERESTS
None
REFERENCES
- [1].Dentzer S. Rx For The “Blockbuster Drug” Of Patient Engagement. Health Aff. (Millwood) 2013;32:202–202. doi: 10.1377/hlthaff.2013.0037. [DOI] [PubMed] [Google Scholar]
- [2].Hibbard JH, Mahoney ER, Stock R, Tusler M. Do Increases in Patient Activation Result in Improved Self-Management Behaviors? Health Serv. Res. 2007;42:1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. [accessed October 5, 2012];Meaningful Use | Policy Researchers & Implementers | HealthIT.gov. 2012 http://www.healthit.gov/policy-researchers-implementers/meaningful-use.
- [4].Delbanco T, Berwick DM, Boufford JI, Edgman-Levitan, Ollenschläger G, Plamping D, Rockefeller RG. Healthcare in a land called PeoplePower: nothing about me without me. Health Expect. 2001;4:144–150. doi: 10.1046/j.1369-6513.2001.00145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. [accessed September 23, 2014];Speak Up Initiatives, Jt. Comm. 2002 http://www.jointcommission.org/speakup.aspx.
- [6].Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Creber R. Masterson, Prey J, Ryan B, Alarcon I, Qian M, Bakken S, Feiner S, Hripcsak G, Polubriaginof F, Restaino S, Schnall R, Strong P, Vawdrey D. Engaging hospitalized patients in clinical care: Study protocol for a pragmatic randomized controlled trial. Contemp. Clin. Trials. 2016;47:165–171. doi: 10.1016/j.cct.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Toscos T, Daley C, Heral L, Doshi R, Chen Y-C, Eckert GJ, Plant RL, Mirro MJ. Impact of electronic personal health record use on engagement and intermediate health outcomes among cardiac patients: a quasi-experimental study. J. Am. Med. Inform. Assoc. 2016;23:119–128. doi: 10.1093/jamia/ocv164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Stepleman L, Rutter MC, Hibbard J, Johns L, Wright D, Hughes M. Validation of the patient activation measure in a multiple sclerosis clinic sample and implications for care. Disabil Rehabil. 2010;32:1558–67. doi: 10.3109/09638280903567885. [DOI] [PubMed] [Google Scholar]
- [11].Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring self-management of patients’ and employees’ health: further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009;77:116–22. doi: 10.1016/j.pec.2009.02.018. [DOI] [PubMed] [Google Scholar]
- [12].Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L, Wegener ST. Psychometric Properties of the Patient Activation Measure among Multimorbid Older Adults. Health Serv. Res. 2011;46:457–478. doi: 10.1111/j.1475-6773.2010.01210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When Patient Activation Levels Change, Health Outcomes And Costs Change, Too. Health Aff. (Millwood) 2015;34:431–437. doi: 10.1377/hlthaff.2014.0452. [DOI] [PubMed] [Google Scholar]
- [14].Hibbard JH, Greene J, Shi Y, Mittler J, Scanlon D. Taking the Long View How Well Do Patient Activation Scores Predict Outcomes Four Years Later? Med. Care Res. Rev. 2015 doi: 10.1177/1077558715573871. 1077558715573871. [DOI] [PubMed] [Google Scholar]
- [15].Schmaderer M. Psychometric Properties of the Patient Activation Measure in Multimorbid Hospitalized Patients. J. Nurs. Meas. 2015;23:128–141. doi: 10.1891/1061-3749.23.3.E128. [DOI] [PubMed] [Google Scholar]
- [16].Centers for Disease Control and Prevention . FastStats. Centers for Disease Control and Prevention; [accessed October 22, 2015]. 2010. http://www.cdc.gov/nchs/fastats/hospital.htm. [Google Scholar]
- [17].O’Leary KJ, Lohman ME, Culver E, Killarney A, Smith GR, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J. Am. Med. Inform. Assoc. 2015 doi: 10.1093/jamia/ocv058. ocv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Dalal AK, Dykes PC, Collins S, Lehmann LS, Ohashi K, Rozenblum R, Stade D, McNally K, Morrison CR, Ravindran S, Mlaver E, Hanna J, Chang F, Kandala R, Getty G, Bates DW. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J. Am. Med. Inform. Assoc. 2015 doi: 10.1093/jamia/ocv093. ocv093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: A pilot study to improve inpatient engagement. J. Hosp. Med. 2014 doi: 10.1002/jhm.2169. n/a–n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Netemeyer RG, Bearden WO, Sharma S. Scaling procedures: Issues and applications. Sage; 2003. [Google Scholar]
- [21].Portney LG. Foundations of clinical research : applications to practice. 3rd ed Pearson/Prentice Hall; Upper Saddle River, N.J.: 2009. [Google Scholar]
- [22].Davidson M. Encycl. Qual. Life Well- Res. Springer; 2014. Known-Groups Validity; pp. 3481–3482. [Google Scholar]
- [23].Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, DeVellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai J-S, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter. Res Briefs. 2008;8:1–9. [PubMed] [Google Scholar]
- [25].Strickland OL. Using Factor Analysis for Validity Assessment: Practical Considerations. J. Nurs. Meas. 2003;11:203–205. doi: 10.1891/jnum.11.3.203.61274. [DOI] [PubMed] [Google Scholar]
- [26].Horowitz JL, Manski CF. Identification and Robustness with Contaminated and Corrupted Data. Econometrica. 1995;63:281–302. doi: 10.2307/2951627. [DOI] [Google Scholar]
- [27].Moore JC, Stinson LL, Welniak EJ. Income measurement error in surveys: A review. J. Off. Stat.-Stockh.- 2000;16:331–362. [Google Scholar]
- [28].Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual. Life Res. 2009;18:873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Brazier J-11, Harper R, Jones N, O’cathain A, Thomas K, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Bmj. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J. Clin. Epidemiol. 1998;51:1171–1178. doi: 10.1016/s0895-4356(98)00109-7. others. [DOI] [PubMed] [Google Scholar]
- [31].Fries JF, Bruce B, Cella D. The promise of PROMIS: using item response theory to improve assessment of patient-reported outcomes. Clin. Exp. Rheumatol. 2005;23:S53. [PubMed] [Google Scholar]
- [32].Chew L, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Health Lond. Engl. 1997. 2004;11:12. [PubMed] [Google Scholar]
- [33].Mitchell SE, Gardiner PM, Sadikova E, Martin JM, Jack BW, Hibbard JH, Paasche-Orlow MK. Patient Activation and 30-Day Post-Discharge Hospital Utilization. J. Gen. Intern. Med. 2014;29:349–355. doi: 10.1007/s11606-013-2647-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27:520–6. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].StataCorp . Stata Statistical Software: Release 14. StataCorp LP; College Station, TX: 2015. [Google Scholar]
- [36].R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. http://www.R-project.org/ [Google Scholar]
- [37].Hibbard JH, Greene J, Becker ER, Roblin D, Painter MW, Perez DJ, Burbank-Schmitt E, Tusler M. Racial/Ethnic Disparities And Consumer Activation In Health. Health Aff. (Millwood) 2008;27:1442–1453. doi: 10.1377/hlthaff.27.5.1442. [DOI] [PubMed] [Google Scholar]
- [38].Bickmore TW, Pfeifer LM, Jack BW. Taking the time to care. SIGCHI Conf. Hum. Factors Comput. Syst.; ACM Press; 2009. p. 1265. [DOI] [Google Scholar]