Abstract
Background
For blunt trauma patients who have failed the NEXUS low-risk criteria, the adequacy of CT as the definitive imaging modality for clearance remains controversial. The purpose of this study was to prospectively evaluate the accuracy of CT for the detection of clinically significant C-spine injury.
Methods
Prospective multicenter observational study (09/2013-03/2015), at 18 North American Trauma Centers. All adult (≥18yo) blunt trauma patients underwent a structured clinical examination. NEXUS failures underwent a CT of the C-spine with clinical follow up to discharge. The primary outcome measure was sensitivity and specificity of CT for clinically significant injuries requiring surgical stabilization, halo or cervical-thoracic orthotic (CTO) placement using the gold standard of final diagnosis at the time of discharge, incorporating all imaging and operative findings.
Results
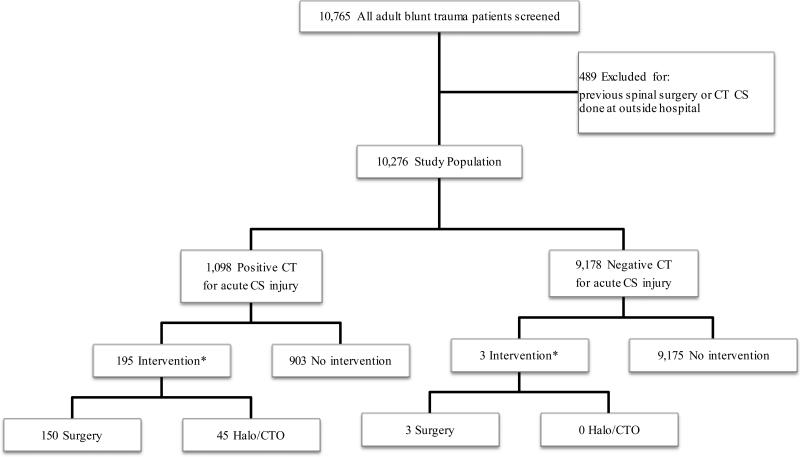
10,765 patients met inclusion criteria, 489 (4.5%) were excluded (previous spinal instrumentation or outside hospital transfer). 10,276 patients [4,660 (45.3%) unevaluable/distracting injuries, 5,040 (49.0%) midline C-spine tenderness, 576 (5.6%) neurologic symptoms] were prospectively enrolled: mean age 48.1yo (range 18-110), SBP 138 (SD 26), median GCS 15 (IQR 14,15), ISS 9 (IQR 4,16). Overall, 198 (1.9%) had a clinically significant C-spine injury requiring surgery [153 (1.5%)] or halo [25 (0.2%)] or CTO [20 (0.2%)]. The sensitivity and specificity for clinically significant injury was 98.5% and 91.0% with a NPV of 99.97%. There were 3 (0.03%) false negative CT scans that missed a clinically significant injury, all had a focal neurologic abnormality on their index clinical examination consistent with central cord syndrome and 2 of 3 had severe degenerative disease.
Conclusions
For patients requiring acute imaging for their C-spine after blunt trauma, CT was effective for ruling out clinically significant injury with a sensitivity of 98.5%. For patients with an abnormal neurologic exam as the trigger for imaging, there is a small but clinically significant incidence of a missed injury and further imaging with MRI is warranted.
Level of Evidence
Level II, Diagnostic Tests or Criteria
Keywords: cervical spine, cervical collar, blunt trauma, clearance
Background
After all immediately life-threatening injuries have been addressed, clearance of the cervical spine remains one of the most critical subsequent steps in the systematic evaluation of the multisystem blunt trauma patient. While all trauma patients are at risk of injury, the actual incidence is only 1-3%(1) with the number that are unstable requiring intervention being even smaller. However, because missing a clinically significant injury in a patient that arrives neurologically intact can lead to a subsequent injury, delineating the optimal mechanism for clearance remains an important research goal. Due to time and cost constraints as well as the radiation burden, screening imaging cannot be performed in all patients. Therefore to develop a safe and accurate process for clearance of the cervical spine (C-spine), two questions must be addressed: 1. Which patients require screening and 2. What is the optimal diagnostic modality for this screening.
For the first question, in patients that are awake, alert and evaluable with no distracting injuries, and neurologically normal with no midline C-spine tenderness, the collar can be cleared clinically using the National Emergency X-Radiography Utilization Study (NEXUS) decision making rule(2). For those that fail to meet this standard however, imaging is required and Computed Tomography (CT) is utilized as the next step in radiographic clearance. The sensitivity of CT is superior to that of plain films rendering the latter of minimal benefit in the acute diagnostic evaluation of the blunt trauma patient at risk of injury(3-5). For those that have a CT that is both adequate and negative, the added value of obtaining an MRI remains poorly defined and is the crux of the second question. The contemporary evidence base is weak because of the small patient numbers and primarily retrospective design of many of the studies that are currently being used to drive practice(6-14). In 2015, the Eastern Association for the Surgery of Trauma published a comprehensive systematic review(7, 11, 12, 14-22) and practice management guidelines specifically for the obtunded adult blunt trauma patient(23). In summarizing five studies with a total of 1,017 patients meeting their entry criteria, the summary conclusion was that they would “conditionally recommend cervical collar removal after a negative high quality C-spine CT scan result alone”. This was based on the high negative predictive value (NPV) of CT for excluding unstable fractures, as well as the high cost and real risk associated with transport to MRI, with the potential for unnecessary treatments being rendered for questionable findings. For patients who require imaging because of persistent midline tenderness or neurologic deficits and have a negative CT, less data is available. In a recent prospective, single center observational study, 830 patients with tenderness or focal neurologic deficit were evaluated with CT, which was found to have a sensitivity and specificity of 100% for clinically significant injuries(24).
While the data to date is consistent, the absence of a large scale multicenter dataset examining this clinical issue has made the development of a universally acceptable protocol for C-spine clearance a challenge. To this end, a prospective multicenter trial was designed and conducted through the Multi-Institutional Trials group of the Western Trauma Association. The purpose of this study was to prospectively evaluate the sensitivity and specificity of CT Scan for the detection of clinically significant C-spine injury.
Methods
This is a prospective multicenter observational trial performed at 18 Level I and II trauma centers in North America through the Western Trauma Association Multi-institutional Trials group. The study was designed to evaluate the diagnostic Sensitivity, Specificity, Negative and Positive Predictive Value (NPV and PPV) of CT Scan for the detection of clinically significant C-spine injury after blunt trauma. After independent IRB approval at each of the study sites, a convenience sampling of blunt trauma patients (09/2013-03/2015), 18 years and older were prospectively screened for enrollment at the time of their initial trauma evaluation. Patients were screened utilizing a standardized clinical examination. Those patients failing the NEXUS(2) low risk criteria underwent a CT Scan of the C-spine and were prospectively followed to discharge. Any patients who were transferred from an outside facility, had a history of spinal instrumentation or who did not undergo diagnostic imaging with CT Scan of their C-spine were excluded from the final analysis. All patients underwent multidetector helical CT (MDCT,≥64 channel) at the 18 participating centers. Patients with cervical spine imaging from outside hospitals were excluded. This was a convenience sampling. The patients who were not included in this study made up a small percentage of the total however further information on these patients were not obtained.
This was a pragmatic observational study and all patient care decisions were made by the treating surgical team without reference to the study protocol. Likewise any additional imaging including the use of MRI was at the discretion of the treating clinician based on individual provider preference and local institutional protocols. The history and physical examination was performed by a senior resident or faculty member using a structured form and included injury demographics, associated injuries, all imaging performed for the C-spine and treatments rendered. All imaging was interpreted by an attending radiologist blinded to the study case report form contents and the final attending radiologist read was utilized for the analysis. The physical examination consisted of the NEXUS criteria including the patient's ability to cooperate with the assessment (awake and alert, not intoxicated, no painful distracting injuries) as well as for those who were evaluable, the presence or absence of midline C-spine tenderness and the results of the neurological examination.
The primary outcome measure assessed in this study was the presence of a clinically significant C-spine fracture. For a fracture to be clinically significant, an abnormal or equivocal finding observed on either CT or MRI consistent with acute traumatic injury was necessary, along with one of three active interventions: surgical stabilization, Halo Orthotic placement or use of a Cervical-Thoracic Orthotic (CTO).
A power analysis was performed assuming a conservative estimated incidence of clinically significant C-spine injury of 2% derived from the largest prospective study cohort to date(24). The sample size needed to achieve statistical significance at the 5% level, 2-tailed, with β value of 0.20 was 5,350 to detect 107 patients with a clinically significant injury. Categorical values were compared using the Fisher exact test or Pearson χ2 test, as appropriate. Continuous variables were compared using an unpaired, 2-tailed t-test. All analysis was performed using SPSS Mac version 23.0 (IBM Corp., Armonk, NY). Descriptive statistics were used to characterize the study population. Mean with SD or Range, or Median with IQR were used to characterize age, ISS, SBP, HR, and GCS. Using a gold standard of the final diagnosis at the time of discharge, which included the results of all imaging and operative findings as the criterion standard, sensitivity, specificity, NPV and PPV for CT Scan in the diagnosis of clinically significant C-spine injury were calculated.
Results
During the study period, 35,538 blunt trauma patients 18 years or older presented to the 18 study sites with 10,765 screened patients meeting the entry criteria. Of these, 489 (4.5%) were excluded (470 previous spinal surgery, 17 outside hospital transfer, two both) resulting in 10,276 patients enrolled in the study protocol. Of the remaining 10,276 patients, 4,660 (45.3%) were unevaluable or with distracting injuries precluding evaluation, 5,040 (49%) had midline C-spine tenderness and 576 (5.6%) had neurologic symptoms as their primary reason for inability to clear the C-spine clinically. The study population was predominantly male (66.7%) with a mean age of 48.1 years (Range: 18-110) and Median ISS 9 (4-16). The most common mechanism of injury was a motor vehicle collision (30.0%) followed by ground level fall (20.9%) and fall from height (11.9%) (Table 1). Overall, 950 (9.2%) patients had MRI, and the Median length of stay was 2 (1-6) days. The in-hospital mortality was 3.1%, none directly attributable to the C-spine injury (Table 2).
Table 1.
Characteristics of Blunt Trauma CS patients (n=10,276)
| Total |
CS Injuries (Sx or Halo or CTO) |
No CS injury |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | n=10,276 | n=198 | n=10,078 | p | ||||||
| Age, Mean [Range], years | 48.1 | [18-110] | 51.1 | [18,92] | 48.1 | [18,110] | 0.138 | |||
| Male Gender, No.(%) | 6,858 | (66.7%) | 146 | (73.7%) | 6,712 | (66.6%) | 0.036 | |||
| Blunt Mechanism, No.(%) | 0.005 | |||||||||
| MVC | 3,085 | (30.0%) | 67 | (33.8%) | 3,018 | (29.9%) | 0.280 | |||
| GLF | 2,149 | (20.9%) | 41 | (20.7%) | 2,108 | (20.9%) | 0.998 | |||
| Fall from height | 1,221 | (11.9%) | 32 | (16.2%) | 1,189 | (11.8%) | 0.080 | |||
| Other | 1,052 | (10.2%) | 27 | (13.6%) | 1,025 | (10.2%) | 0.144 | |||
| AVP | 925 | (9.0%) | 11 | (5.6%) | 914 | (9.1%) | 0.111 | |||
| Assault | 718 | (7.0%) | 2 | (1.0%) | 716 | (7.1%) | 0.001 | |||
| MCC | 713 | (6.9%) | 13 | (6.6%) | 700 | (6.9%) | 0.939 | |||
| BVA | 387 | (3.8%) | 5 | (2.5%) | 382 | (3.8%) | 0.457 | |||
| ISS, Median [IQR] | 9 | [4-16] | 17 | [10-25] | 9 | [4-16] | <0.0001 | |||
| Admission GCS, Median [IQR] | 15 | [14-15] | 15 | [14-15] | 15 | [14-15] | 0.426 | |||
| Admission SBP, Mean ± SD | 138 | ± | 26 | 133 | ± | 31 | 138 | ± | 25 | 0.006 |
| Admission HR, Mean ± SD | 90 | ± | 20 | 84 | ± | 23 | 90 | ± | 20 | <0.001 |
| Neurologic Exam, No.(%) | ||||||||||
| Unevaluable | 4,660 | (45.3%) | 71.0 | (35.9%) | 4,589 | (45.5%) | 0.008 | |||
| TBI | 375 | (3.6%) | 6.0 | (3.0%) | 369 | (3.7%) | 0.781 | |||
| Distracting Injury | 438 | (4.3%) | 5.0 | (2.5%) | 433 | (4.3%) | 0.296 | |||
| Intoxicated/Intubated | 1,171 | (11.4%) | 17.0 | (8.6%) | 1,154 | (11.5%) | 0.253 | |||
| Combination | 2,676 | (26.0%) | 43.0 | (21.7%) | 2,633 | (26.1%) | 0.187 | |||
| Evaluable | 5,616 | (54.7%) | 127 | (64.1%) | 5,489 | (54.5%) | 0.001 | |||
| Evaluable + no deficit | 5,040 | (49.0%) | 60 | (30.3%) | 4,980 | (49.4%) | <.0001 | |||
| Evaluable + motor deficit | 243 | (2.4%) | 18 | (9.1%) | 225 | (2.2%) | <.0001 | |||
| Evaluable + sensory deficit | 182 | (1.8%) | 17 | (8.6%) | 165 | (1.6%) | <.0001 | |||
| Evaluable + motor/sensory deficit | 151 | (1.5%) | 32 | (16.2%) | 119 | (1.2%) | <.0001 | |||
| Type of Imaging, No.(%) | ||||||||||
| CT | 10,276 | (100.0%) | 198 | (100.0%) | 10,078 | (100.0%) | 1.000 | |||
| MRI | 950 | (9.2%) | 126 | (63.6%) | 824 | (8.2%) | <0.0001 | |||
| Plain X-Ray | 144 | (1.4%) | 28 | (14.1%) | 116 | (1.2%) | <0.0001 | |||
| Flex-Ex CS X-Ray | 43 | (0.4%) | 2 | (1.0%) | 41 | (0.4%) | 0.474 | |||
Abbreviations: CS- C-spine, Sx- Surgery, CTO- Cervical Thoracic Orthotic, MVC- Motor Vehicle Collision, GLF- Ground Level Fall, AVP- Automobile Versus Pedestrian, MCC- Motorcycle Collision, BVA- Bicycle Versus Automobile, TBI- Traumatic Brain Injury, ISS- Injury Severity Score, IQR- Interquartile Range, GCS- Glasgow Coma Scale, SBP- Systolic Blood Pressure, SD- Standard Deviation, HR- Heart Rate, CT- Computed Tomography, MRI- Magnetic Resonance Imaging
Table 2.
Interventions and Outcomes of Blunt Trauma CS patients (n=10,276)
| Total |
CS Injuries (Sx, Halo or CTO) |
No CS injury |
|||||
|---|---|---|---|---|---|---|---|
| Variables | n=10,276 | n=198 | n=10,078 | p | |||
| Final Neurologic Diagnosis, No.(%) | |||||||
| CS Injury (all) | 1,096 | (10.7%) | 198 | (100.0%) | 898 | (8.9%) | NA |
| CS Injury (CTO, Halo or Sx) | 198 | (1.9%) | 198 | (100.0%) | 0 | (0.0%) | NA |
| CS Injury (Halo or Sx) | 178 | (1.7%) | 178 | (89.9%) | 0 | (0.0%) | NA |
| Treatment, No.(%) | |||||||
| None | 7,774 | (75.7%) | 0 | (0.0%) | 7,774 | (77.1%) | NA |
| Soft collar | 193 | (1.9%) | 0 | (0.0%) | 193 | (1.9%) | NA |
| Hard collar | 2,063 | (20.1%) | 0 | (0.0%) | 2,063 | (20.5%) | NA |
| CTO | 20 | (0.2%) | 20 | (10.1%) | 0 | (0.0%) | NA |
| Halo | 25 | (0.2%) | 25 | (12.6%) | 0 | (0.0%) | NA |
| Sx | 153 | (1.5%) | 153 | (77.3%) | 0 | (0.0%) | NA |
| Other | 48 | (0.5%) | 0 | (0.0%) | 48 | (0.5%) | NA |
| Discharge GCS, Median [IQR] | 15 | [15-15] | 15 | [15-15] | 15 | [15-15] | <0.0001 |
| Discharge Disposition, No.(%) | |||||||
| Home | 7,258 | (72.0%) | 70 | (36.3%) | 7,188 | (72.7%) | <0.0001 |
| Skilled Nursing Facility | 928 | (9.2%) | 25 | (13.0%) | 903 | (9.1%) | 0.139 |
| Rehabilitation | 777 | (7.7%) | 67 | (34.7%) | 710 | (7.2%) | <0.0001 |
| Other | 409 | (4.1%) | 9 | (4.7%) | 400 | (4.0%) | 0.860 |
| Outside Hospital | 361 | (3.6%) | 13 | (6.7%) | 348 | (3.5%) | 0.029 |
| Expired | 311 | (3.1%) | 9 | (4.7%) | 302 | (3.1%) | 0.284 |
| Jail | 39 | (0.4%) | 0 | (0.0%) | 39 | (0.4%) | 0.773 |
| Hospital LOS, Median [IQR] | 2 | [1-6] | 8 | [4.4-18.0] | 2 | [1.0-6.0] | <0.0001 |
| ICU LOS, Median [IQR] | 0 | [0-1.4] | 3 | [1.0-8.0] | 0 | [0-1.1] | <0.0001 |
| In-Hospital Mortality, No.(%) | 311 | (3.1%) | 9 | (4.7%) | 302 | (3.1%) | 0.284 |
Abbreviations: CS- C-spine, Sx- Surgery, CTO- Cervical Thoracic Orthotic, GCS- Glasgow Coma Scale, IQR- Interquartile Range, ICU- Intensive Care Unit, LOS- Length Of Stay
Of the 10,276 patients who failed the NEXUS low risk criteria and required CT scan clearance, 1,096 (10.7%) were diagnosed with an injury. Of these, 198 (1.9%) met the definition of clinically significant requiring intervention. Surgery was required for 153 (1.5%), a Halo orthotic was placed in 25 (0.2%), and a CTO was required for 20 (0.2%) (Table 2). All but three (1.5%) of these injuries were diagnosed on the initial CT Scan, the remainder were diagnosed on MRI. These three patients with a nondiagnostic CT all had an index neurologic exam on presentation consistent with central cord syndrome. In addition, two had cervical degenerative disease on CT. All three underwent surgical stabilization (Table 3).
Table 3.
Characteristics of Patients with Clinically Significant Missed Injuries
| Patient | Age | Gender | Mechanism | Treatment | CT | MRI | Final Diagnosis |
|---|---|---|---|---|---|---|---|
| 1 | 79 | male | auto vs. ped | C5-6 ACDF | degenerative disease | C6 cord contusion | central cord syndrome |
| 2 | 58 | male | ground level fall | C4-5 ACDF | degenerative disease | C4-5 disk herniation | central cord syndrome |
| 3 | 36 | male | fall from height | Anterior cervical microdiskectomy C4-5 arthrodesis | normal | C4/5 cord contusion | central cord syndrome |
Abbreviations: ACDF- Anterior cervical discectomy and fusion
Injuries requiring surgery included fractures (83.3%), subluxation or dislocation (18.7%), stenosis (13.1%), ligamentous injury (13.1%), disc injury (4.0%) and epidural hematoma (4.0%). Surgical interventions included fusion, fixation or arthrodesis (88.4%) and decompression, laminectomy or corpectomy (19.4%). The level of injury for those requiring operative intervention in decreasing frequency were C6 (54.2%), C5 (35.3%), C7 (34.6%), C4 (30.7%), C2 (26.1%), C1 (10.5%) and C3 (7.8%). Injuries requiring Halo orthotic placement involved C2 (88%), C1 (36%), C5 (16%), C6 (12%), C3 (12%), C4 (12%) and C7 (8%). Injuries requiring CTO were at C7 (45%), C6 (40%), C2 (20%), C3 (15%), C1 (10%), C4 (5%) and C5 (5%) (Table 4).
Table 4.
Clinically Significant Injury Distribution by Location
| Fisher's Exact Test P-Value | |||||||
|---|---|---|---|---|---|---|---|
| Level | All | Surgery | Halo | CTO | Sx vs Halo | Halo vs CTO | Sx vs CTO |
| C1 | 27 (13.6%) | 16 (10.5%) | 9 (36%) | 2 (10%) | 0.0024 | 0.0791 | 1.0000 |
| C2 | 66 (33.3%) | 40 (26.1%) | 22 (88%) | 4 (20%) | 0.0001 | 0.0001 | 0.7853 |
| C3 | 18 (9.1%) | 12 (7.8%) | 3 (12%) | 3 (15%) | 0.4466 | 1.0000 | 0.3874 |
| C4 | 51 (25.8%) | 47 (30.7%) | 3 (12%) | 1 (5%) | 0.0578 | 0.6174 | 0.0154 |
| C5 | 59 (29.8%) | 54 (35.3%) | 4 (16%) | 1 (5%) | 0.0667 | 0.3624 | 0.0045 |
| C6 | 94 (47.5%) | 83 (54.2%) | 3 (12%) | 8 (40%) | 0.0001 | 0.0409 | 0.2449 |
| C7 | 64 (32.3%) | 53 (34.6%) | 2 (8%) | 9 (45%) | 0.0088 | 0.0059 | 0.4577 |
Surgery- 153 patients, Halo- 25 patients, CTO- 20 patients
Abbreviation: CTO- Cervical Thoracic Orthosis
Overall, 2,063 (20.1%) patients were treated with a “hard” collar (Table 2). The discharge instructions ranged from wearing the collar for comfort to wearing the collar at all times. Of these, 1438 (69.7%) had normal imaging and did not have a C-spine diagnosis at the time of discharge. For the remaining 625 patients with a finding on CT or MRI, 31 had a negative CT with a positive MRI. The MRI findings for 29 (93.5%) of these patients consisted of equivocal findings or edema, “sprains” or “strains”. Two patients had a finding other than those described above. One patient was a 55-year old male who was a restrained rear seat MVC passenger who presented with C-spine and lower back tenderness and decreased right anterior thigh sensation. He had a normal CT of the C-spine with a concurrent distraction fracture involving the anterior cortical margin of the T9 vertebral body without subluxation and degenerative changes visible in the L-spine. On the MRI, there was widening of the anterior disc space at the C6-7 level and edema consistent with a possible injury to the anterior ligament. He was treated with a Semi-rigid collar which was successfully removed at 6 weeks with no residual neurological issues. The second patient was a 48-year old female who presented after a MVC with C-spine tenderness and a normal neurologic exam. The CT was negative however the MRI was equivocal for injury, demonstrating a possible non-displaced fracture involving the left inferior articular facet of C5. A semi-rigid collar was prescribed for when the patient was out of bed. Both injuries were considered to be stable injuries by the neurosurgery service caring for the patient.
Comparison of CT with the criterion standard of final diagnosis at the time of discharge demonstrated a sensitivity of 98.5% and specificity of 91.0% for clinically significant injuries. The PPV was 17.8% and NPV was 99.97%. In all patients with a clinically significant C-spine diagnosis, either the CT was positive for injury or there was an abnormal motor exam. No clinically significant injury was missed when CT was combined with the motor exam. Comparison of CT and motor exam with the criterion standard of final diagnosis at time of discharge demonstrated a 100% sensitivity with a NPV of 100% for detecting all clinically significant C-spine injuries.
Discussion
Clearance of the C-spine remains a critical step in the management of the multisystem blunt trauma patient. There are severe consequences if a clinically significant injury is missed, especially in the patient who arrives neurologically intact, with an occult unstable injury. Clinical examination has been demonstrated to be effective at determining who requires imaging, with both the NEXUS low risk criteria and Canadian C-spine Rules(2, 25, 26) documenting high sensitivities and acceptable specificities for the detection of clinically significant injuries. Patients who cannot be cleared by these clinical decision rules require screening imaging. While CT has been accepted as the standard first line diagnostic modality, the adequacy of a normal CT alone has been questioned.
Unfortunately, the literature providing the foundation for our current clinical practice remains less than ideal, with small, predominately retrospective and single center based case series attempting to evaluate the adequacy of CT for clearance. With a retrospective study design, accurate capture of the presenting clinical examination in particular remains a challenge. In 2015 the Eastern Association for the Surgery of Trauma confronted this issue by performing a systematic review of the existing literature(23). They targeted a specific population, those who could not be cleared by the NEXUS low risk criteria due to being obtunded. Their practice management guidelines highlighted the paucity of patients enrolled in the 5 studies that met their inclusion criteria. Despite this limitation, they did conclude that a high quality negative CT could effectively exclude an unstable fracture. They noted that this was due to both the discriminating ability of the CT as well as the downstream effects of additional imaging such as MRI detecting clinically irrelevant injuries that go on to be treated. There is also a real risk to the travel required to obtain this additional imaging. The group emphasized the need for large, protocol-driven, prospective corroborating datasets to support their conclusions. In addition to the obtunded patient, a subset of the evaluable patient cohort may also require screening imaging. These are patients with either residual midline C-spine tenderness or with neurologic deficits. Unfortunately, there is even less data supporting the accuracy of CT screening in this patient population. In a contemporary prospective observational study of 830 patients, for those with tenderness or a neurologic deficit, the sensitivity was again found to be 100% for clinically significant injuries(24).
This is the first large-scale prospective multicenter study to address the adequacy of CT as a screening modality and the findings were consistent with that of the studies previously discussed. For all clinically significant fractures, CT has a high sensitivity with acceptable specificity and is therefore an effective screening modality. For the three patients who had injuries that were missed by CT, all had a neurologic motor deficit consistent with central cord syndrome. If all patients with a negative CT who had a neurologic deficit underwent MRI, the sensitivity for detecting clinically significant injuries would be increased to 100%.
In this study cohort, approximately a fifth of patients were treated with a “hard” collar. This was expressly omitted as a clinically significant outcome measure because of the difficulty in adjudicating the clinical relevance of the diagnoses leading to these collars being prescribed. Highlighting this fact was the wide variability in the instructions given to the patient at discharge ranging from wear for comfort, to when out of bed, to at all times. Perhaps even more important was that fact that more than 2/3 of patients who were prescribed one of these collars had no C-spine injury diagnosis at the time of discharge. Despite the pitfalls of using this as an outcome measure, because of the potential that there may have been a clinically significant injury within this group of patients, all patients with a negative CT but positive MRI resulting in collar prescription were reviewed in detail. This amounted to approximately 1.5% of the study population. The vast majority of these had equivocal findings or a strain or sprain. The two patients who had an MRI with something other than a strain or sprain both had MRI findings that were equivocal, and even if there truly was an injury, they would have been stable and would not have benefited from prolonged immobilization or surgery. While it was not possible to confirm the clinical relevance of the “strains” and “sprains” diagnosed on MRI and treated with a “hard” collar, the possibility remains that some of these were clinically relevant. This remains a limitation of the study. Practically, the prescription of a collar for outpatient use in these patients with midline C-spine tenderness for comfort without a defined injury may be warranted at the discretion of the treating physician.
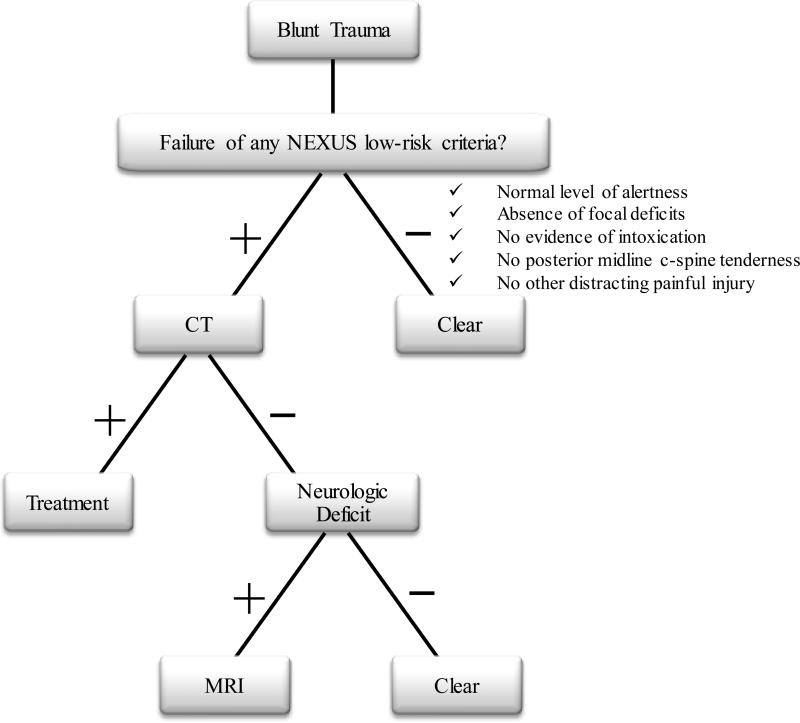
In summary, the primary objective of this study was to evaluate the ability of CT to clear the C-spine. In this large multicenter study, CT was found to be highly sensitive for clinically significant injuries. Based on these results, we would propose the following decision making algorithm (Figure 2). For the patient that arrives into the resuscitation bay after blunt trauma with an uncleared C-spine, the NEXUS low risk criteria should be applied. If negative, the collar should be removed. All other patients should proceed to CT as the initial screening modality. If the CT is adequate and negative, the collar may be removed with a low risk of clinically significant injury. The only exception to this is the patient who arrives with motor or sensory neurologic deficits or without witnessed movement of all extremities. Even if the CT is adequate and negative, MRI may detect a small percentage of patients who have clinically significant injuries.
Figure 2.
Clinical decision rule for cervical spine evaluation after blunt trauma. NEXUS criteria defined in Hoffman et al.2
Figure 1.
Enrolled adult, blunt trauma patients between September 2013 to March 2015. (Abbreviations: CT, computed tomography; CS, C-spine; CTO, cervical thoracic orthotic. * Intervention was defined as surgery, Halo or CTO
Author Contributions
All authors contributed actively to the drafting and critical revision of the manuscript, and each approved the final version being submitted. In addition, the authors contributed to the following: Kenji Inaba, MD -- Concept; Literature Search; Study Design; Data Collection, Analysis and Interpretation. Saskya Byerly, MD -- Literature Search; Study Design; Data Collection, Analysis and Interpretation. Lisa D Bush, MPAS -- Data Collection and Analysis. Matthew J. Martin, MD -- Data Collection, Analysis and Interpretation. David T. Martin, MD -- Data Collection and Interpretation. Kimberly A. Peck, MD -- Data Collection and Interpretation. Galinos Barmparas, MD -- Data Collection and Interpretation. Matthew J Bradley, MD -- Data Collection and Interpretation. Joshua P Hazelton, DO -- Data Collection and Interpretation. Raul Coimbra, MD, PhD – Data Collection and Interpretation. Asad J Choudhry, MBBS -- Data Collection and Interpretation. Carlos V.R. Brown, MD -- Data Collection and Interpretation. Chad G. Ball, MD MSC -- Data Collection and Interpretation. Jill R Cherry-Bukowiec, MD MS -- Data Collection and Interpretation. Clay Cothren Burlew, MD -- Data Collection and Interpretation. Bellal Joseph, MD -- Data Collection and Interpretation. Julie Dunn, MD MS -- Data Collection and Interpretation. Christian T. Minshall, MD PhD -- Data Collection and Interpretation. Matthew M Carrick, MD -- Data Collection and Interpretation. Gina M. Berg, PhD MBA -- Data Collection and Interpretation. Demetrios Demetriades, MD PhD -- Study Design; Data Collection, Analysis and Interpretation. Megan Linnebur, MD -- Study Design; Data Collection. Ranan Mendelsberg, MD -- Data Collection. Moazzam Khan, MD -- Data Collection. Yvonne Hojberg -- Data Collection. Monica D. Wong, MS -- Study Design; Data Collection and Analysis. Jayun Cho, MD -- Data Collection and Analysis. Tom Maxim, BS -- Data Collection. Elizabeth Benjamin, MD PhD -- Data Analysis and Data Interpretation. William B. Long, MD -- Data Interpretation. Martin Schreiber, MD -- Data Interpretation. Samantha J. Underwood, MS -- Data Collection. Casey E. Dunne, MPH -- Data Collection. Eric J Ley, MD -- Data Interpretation. Marissa K. Srour, MD -- Data Collection. Jay Menaker, MD -- Data Interpretation. Thomas M. Scalea, MD -- Data Interpretation. Lisa M Capano-Wehrle, MPH -- Data Collection. Ryan D. DeAngelis, BS -- Data Collection. Aneta S. Pariaszevski, BS -- Data Collection. Allison E Berndtson, MD -- Data Collection. Martin D Zielinski, MD -- Data Interpretation. Amanda L. Klein, MD -- Data Collection. Ammar A Almadani, MD -- Data Collection. Alexandra Sheth, BS -- Data Collection. Kathryn M. Beauchamp, MD -- Data Collection. Mazhar Khalil, MD -- Data Collection. Katherine L. Corey, MPA BSN -- Data Collection. Steve E. Wolf, MD -- Data Interpretation. Barbara A Shaffer, BSN -- Data Collection. Paul B Harrison, MD -- Data Interpretation.
Saskya Byerly, MD -- saskya.byerly@med.usc.edu
Demetrios Demetriades, MD PhD -- demetrios.demetriades@med.usc.edu
Megan Linnebur, MD -- megan.linnebur@med.usc.edu
Ranan Mendelsberg, MD -- ranan.mendelsberg@med.usc.edu
Moazzam Khan, MD -- mkhan00@hotmail.com
Yvonne Hojberg -- eeveehojberg@hotmail.com
Monica D. Wong, MS -- monica.wong@med.usc.edu
Jayun Cho, MD -- jayun.cho@usc.edu
Tom Maxim, BS -- tmaxim@usc.edu
Elizabeth Benjamin, MD PhD -- elizabeth.benjamin@med.usc.edu
Lisa D Bush, MPAS -- lisabush@me.com
Matthew J. Martin, MD -- Traumadoc22@gmail.com
William B. Long, MD -- wlong@lhs.org
David T. Martin, MD -- davethomasmartin@gmail.com
Martin Schreiber, MD -- schreibm@ohsu.edu
Samantha J. Underwood, MS -- underwos@ohsu.edu
Kimberly A. Peck, MD -- peck.kimberly@scrippshealth.org
Casey E. Dunne, MPH -- dunne.casey@scrippshealth.org
Galinos Barmparas, MD -- galinos.barmparas@cshs.org
Eric J Ley, MD -- eric.ley@cshs.org
Marissa K. Srour, MD -- marissasrour@gmail.com
Matthew J Bradley, MD -- mbradley1@umm.edu
Jay Menaker, MD -- jmenaker@umm.edu
Thomas M. Scalea, MD -- tscalea@umm.edu
Joshua P Hazelton, DO -- hazelton-joshua@cooperhealth.edu
Lisa M Capano-Wehrle, MPH -- capano-wehrle-lisa@cooperhealth.edu
Ryan D. DeAngelis, BS -- deangelir2@rowan.edu
Aneta S. Pariaszevski, BS -- pariaszea0@rowan.edu
Raul Coimbra, MD, PhD -- rcoimbra@ucsd.edu
Allison E Berndtson, MD -- aberndtson@ucsd.edu
Asad J Choudhry, MBBS -- choudhry.asad@mayo.edu
Martin D Zielinski, MD -- zielinski.martin@mayo.edu
Carlos V.R. Brown, MD -- cvrbrown@seton.org
Amanda L. Klein, MD -- ALKlein@seton.org
Chad G. Ball, MD MSC -- ball.chad@gmail.com
Ammar A Almadani, MD -- aalmadani69@yahoo.com
Jill R Cherry-Bukowiec, MD MS -- jillcher@med.umich.edu
Alexandra Sheth, BS -- assheth@med.umich.edu
Clay Cothren Burlew, MD -- clay.cothren@dhha.org
Kathryn M. Beauchamp, MD -- Kathryn.Beauchamp@dhha.org
Bellal Joseph, MD -- bjoseph@surgery.arizona.edu
Mazhar Khalil, MD -- mkhalil@surgery.arizona.edu
Julie Dunn, MD MS -- Julie.Dunn@uchealth.org
Katherine L. Corey, MPA BSN -- Katherine.Corey@uchealth.org
Christian T. Minshall, MD PhD -- Christian.minshall@utsouthwestern.edu
Steve E. Wolf, MD -- steven.wolf@utsouthwestern.edu
Matthew M Carrick, MD -- matt.carrick@acutesurgical.com
Barbara A Shaffer, BSN -- Barbara.Shaffer@hcahealthcare.com
Gina M. Berg, PhD MBA -- gberg@kumc.edu
Paul B Harrison, MD -- PHarrison@kansassurgical.com
Footnotes
The WTA C-Spine Study Group members:
Megan Linnebur1, MD, Ranan Mendelsberg1, MD, Moazzam Khan1, MD, Yvonne Hojberg, Monica D. Wong1, MS, Jayun Cho1, MD, Tom Maxim1, BS, Elizabeth Benjamin1, MD, PhD, William B. Long2, MD, Martin Schreiber3, MD, Samantha J. Underwood3, MS, Casey E. Dunne4, MPH, Eric J. Ley5, MD, Marissa K. Srour5, MD, Jay Menaker6, MD, Thomas M. Scalea6, MD, Lisa M. Capano-Wehrle7, MPH, Ryan D. DeAngelis7, BS, Aneta S. Pariaszevski7, BS, Allison E. Berndtson8, MD, Martin D. Zielinski9, MD, Amanda L. Klein10, MD, Ammar A. Almadani11, MD, Alexandra Sheth12, BS, Kathryn M. Beauchamp13, MD, Mazhar Khalil14, MD, Katherine L. Corey15, MPA, BSN, Steve E. Wolf16, MD, Barbara A. Shaffer17, BSN, Paul B Harrison18, MD
Conflict of Interest: None
Funding Disclosures: None
This study was presented at the 46th Western Trauma Association annual meeting February 28-March 4, 2016 in Lake Tahoe, California.
References
- 1.Grossman MD, Reilly PM, Gillett T, Gillett D. National survey of the incidence of cervical spine injury and approach to cervical spine clearance in U.S. trauma centers. J Trauma. 1999;47(4):684–90. doi: 10.1097/00005373-199910000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94–9. doi: 10.1056/NEJM200007133430203. [DOI] [PubMed] [Google Scholar]
- 3.Mathen R, Inaba K, Munera F, Teixeira PG, Rivas L, McKenney M, Lopez P, Ledezma CJ. Prospective evaluation of multislice computed tomography versus plain radiographic cervical spine clearance in trauma patients. J Trauma. 2007;62(6):1427–31. doi: 10.1097/01.ta.0000239813.78603.15. [DOI] [PubMed] [Google Scholar]
- 4.Hennessy D, Widder S, Zygun D, Hurlbert RJ, Burrowes P, Kortbeek JB. Cervical spine clearance in obtunded blunt trauma patients: a prospective study. J Trauma. 2010;68(3):576–82. doi: 10.1097/TA.0b013e3181cf7e55. [DOI] [PubMed] [Google Scholar]
- 5.Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58(5):902–5. doi: 10.1097/01.ta.0000162138.36519.2a. [DOI] [PubMed] [Google Scholar]
- 6.Russin JJ, Attenello FJ, Amar AP, Liu CY, Apuzzo ML, Hsieh PC. Computed tomography for clearance of cervical spine injury in the unevaluable patient. World Neurosurg. 2013;80(3-4):405–13. doi: 10.1016/j.wneu.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 7.Tomycz ND, Chew BG, Chang YF, Darby JM, Gunn SR, Nicholas DH, Ochoa JB, Peitzman AB, Schwartz E, Pape HC, et al. MRI is unnecessary to clear the cervical spine in obtunded/comatose trauma patients: the four-year experience of a level I trauma center. J Trauma. 2008;64(5):1258–63. doi: 10.1097/TA.0b013e318166d2bd. [DOI] [PubMed] [Google Scholar]
- 8.Raza M, Elkhodair S, Zaheer A, Yousaf S. Safe cervical spine clearance in adult obtunded blunt trauma patients on the basis of a normal multidetector CT scan--a meta-analysis and cohort study. Injury. 2013;44(11):1589–95. doi: 10.1016/j.injury.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Soult MC, Weireter LJ, Britt RC, Collins JN, Novosel TJ, Reed SF, Britt LD. MRI as an adjunct to cervical spine clearance: a utility analysis. Am Surg. 2012;78(7):741–4. [PubMed] [Google Scholar]
- 10.Fisher BM, Cowles S, Matulich JR, Evanson BG, Vega D, Dissanaike S. Is magnetic resonance imaging in addition to a computed tomographic scan necessary to identify clinically significant cervical spine injuries in obtunded blunt trauma patients? Am J Surg. 2013;206(6):987–93. doi: 10.1016/j.amjsurg.2013.08.021. discussion 93-4. [DOI] [PubMed] [Google Scholar]
- 11.Kaiser ML, Whealon MD, Barrios C, Kong AP, Lekawa ME, Dolich MO. The current role of magnetic resonance imaging for diagnosing cervical spine injury in blunt trauma patients with negative computed tomography scan. Am Surg. 2012;78(10):1156–60. doi: 10.1177/000313481207801032. [DOI] [PubMed] [Google Scholar]
- 12.Menaker J, Stein DM, Philp AS, Scalea TM. 40-slice multidetector CT: is MRI still necessary for cervical spine clearance after blunt trauma? Am Surg. 2010;76(2):157–63. [PubMed] [Google Scholar]
- 13.Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, Harrigan MR, Rozelle CJ, Ryken TC, Theodore N. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60(Suppl 1):82–91. doi: 10.1227/01.neu.0000430319.32247.7f. [DOI] [PubMed] [Google Scholar]
- 14.Menaker J, Philp A, Boswell S, Scalea TM. Computed tomography alone for cervical spine clearance in the unreliable patient--are we there yet? J Trauma. 2008;64(4):898–903. doi: 10.1097/TA.0b013e3181674675. discussion -4. [DOI] [PubMed] [Google Scholar]
- 15.Chew BG, Swartz C, Quigley MR, Altman DT, Daffner RH, Wilberger JE. Cervical spine clearance in the traumatically injured patient: is multidetector CT scanning sufficient alone? Clinical article. J Neurosurg Spine. 2013;19(5):576–81. doi: 10.3171/2013.8.SPINE12925. [DOI] [PubMed] [Google Scholar]
- 16.Como JJ, Leukhardt WH, Anderson JS, Wilczewski PA, Samia H, Claridge JA. Computed tomography alone may clear the cervical spine in obtunded blunt trauma patients: a prospective evaluation of a revised protocol. J Trauma. 2011;70(2):345–9. doi: 10.1097/TA.0b013e3182095b3c. discussion 9-51. [DOI] [PubMed] [Google Scholar]
- 17.Khanna P, Chau C, Dublin A, Kim K, Wisner D. The value of cervical magnetic resonance imaging in the evaluation of the obtunded or comatose patient with cervical trauma, no other abnormal neurological findings, and a normal cervical computed tomography. J Trauma Acute Care Surg. 2012;72(3):699–702. doi: 10.1097/TA.0b013e31822b77f9. [DOI] [PubMed] [Google Scholar]
- 18.Schuster R, Waxman K, Sanchez B, Becerra S, Chung R, Conner S, Jones T. Magnetic resonance imaging is not needed to clear cervical spines in blunt trauma patients with normal computed tomographic results and no motor deficits. Arch Surg. 2005;140(8):762–6. doi: 10.1001/archsurg.140.8.762. [DOI] [PubMed] [Google Scholar]
- 19.Anekstein Y, Jeroukhimov I, Bar-Ziv Y, Shalmon E, Cohen N, Mirovsky Y, Masharawi Y. The use of dynamic CT surview for cervical spine clearance in comatose trauma patients: a pilot prospective study. Injury. 2008;39(3):339–46. doi: 10.1016/j.injury.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Brohi K, Healy M, Fotheringham T, Chan O, Aylwin C, Whitley S, Walsh M. Helical computed tomographic scanning for the evaluation of the cervical spine in the unconscious, intubated trauma patient. J Trauma. 2005;58(5):897–901. doi: 10.1097/01.ta.0000171984.25699.35. [DOI] [PubMed] [Google Scholar]
- 21.Harris TJ, Blackmore CC, Mirza SK, Jurkovich GJ. Clearing the cervical spine in obtunded patients. Spine (Phila Pa 1976) 2008;33(14):1547–53. doi: 10.1097/BRS.0b013e31817926c1. [DOI] [PubMed] [Google Scholar]
- 22.Steigelman M, Lopez P, Dent D, Myers J, Corneille M, Stewart R, Cohn S. Screening cervical spine MRI after normal cervical spine CT scans in patients in whom cervical spine injury cannot be excluded by physical examination. Am J Surg. 2008;196(6):857–62. doi: 10.1016/j.amjsurg.2008.07.040. discussion 62-3. [DOI] [PubMed] [Google Scholar]
- 23.Patel MB, Humble SS, Cullinane DC, Day MA, Jawa RS, Devin CJ, Delozier MS, Smith LM, Smith MA, Capella JM, et al. Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;78(2):430–41. doi: 10.1097/TA.0000000000000503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Resnick S, Inaba K, Karamanos E, Pham M, Byerly S, Talving P, Reddy S, Linnebur M, Demetriades D. Clinical relevance of magnetic resonance imaging in cervical spine clearance: a prospective study. JAMA Surg. 2014;149(9):934–9. doi: 10.1001/jamasurg.2014.867. [DOI] [PubMed] [Google Scholar]
- 25.Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, Laupacis A, Schull M, McKnight RD, Verbeek R, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. Jama. 2001;286(15):1841–8. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 26.Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510–8. doi: 10.1056/NEJMoa031375. [DOI] [PubMed] [Google Scholar]