Abstract
Objective
To estimate the lifetime risk of knee osteoarthritis (OA) and total knee replacement (TKR) in persons sustaining ACL tear by age 25.
Methods
We used the Osteoarthritis Policy Model to project the cumulative incidence of symptomatic knee OA requiring TKR in persons with: 1) no prevalent or incident injury; 2) isolated ACL tear, surgically treated; 3) isolated ACL tear, non-operatively treated; or 4) prevalent history or surgically treated ACL and meniscal tear (MT). We estimated MT prevalence and incidence and increased risk of knee OA associated with ACL injury and MT from published literature. We conducted a range of sensitivity analyses to examine the impact of uncertainty in input parameters.
Results
Estimated lifetime risk of symptomatic knee OA was 34% for the cohort with ACL injury and MT, compared to 14% for the no injury cohort. ACL injury without MT was associated with a lifetime risk of knee OA between 16%–17%, depending on ACL treatment modality. Estimated lifetime risk of TKR ranged from 6% in the no injury cohort to 22% for the ACL injury and MT cohort. Subjects in the ACL injury and MT cohort developed OA ~1.5 years earlier (55.7 vs. 57.1) and underwent TKR ~2 years earlier (66 vs. 68) than the cohort without knee injuries.
Conclusions
Sustaining ACL injury early in adulthood leads to greater lifetime risk and earlier onset of knee OA and TKR; concomitant MTs compound this risk. These data provide insight into the impact of sustainable injury prevention interventions in young adults.
Introduction
The knee is one of the most common sites of severe injury, and the prevalence of knee injuries is rising. The annual incidence of ACL injury is approximately 80 per 100,000 inhabitants,1 mostly in active, younger persons2,3 and is increasing annually.4,5 ACL injury rates vary by age, gender, and sport, with reported annual incidence rates as high as 5% in competitive, year-round athletes.6 A large body of evidence suggests that a substantial proportion (40–70% or more) of ACL tears are accompanied by concomitant or subsequent meniscal tears (MT).7,8
These injuries have an enormous societal impact at the time of injury, resulting in reduced quality of life,9 productivity losses, and a substantial economic burden.10 They also have implications for the future: knee injuries, especially ACL injuries and MTs, are considered potent risk factors for the development of knee osteoarthritis (OA).11–13 The rising prevalence of these injuries, particularly in younger individuals, raises concerns regarding their impact on development of post-traumatic knee OA.
Several studies document that knee injuries, particularly those related to MT, are associated with increased likelihood of joint deterioration, resulting in OA. These studies are limited by small sample sizes or limited duration of observation.14–16 Thus, data estimating the lifetime risk of knee OA after ACL tear are inadequate.15,17 Given that ACL injury often occurs in the second and third decade of life, large-scale longitudinal studies of the consequences of these injuries are challenging. Model-based analyses allow synthesis of data from multiple sources, extrapolating beyond the limitations of time horizons, geographic settings, and target populations, thus providing valuable insights on the lifelong impact of these injuries; therefore, we performed a model-based analysis to forecast the lifetime risk of symptomatic knee OA and the proportion of population eligible for total knee replacement (TKR) in persons with a complete ACL tear at age 25.
Materials and Methods
Overview
We used the Osteoarthritis Policy (OAPol) Model,18–20 a validated, widely published computer simulation model of knee OA natural history and management, to forecast lifetime risk of knee OA and TKR following injury in early adulthood. We examined four patient cohorts in order to quantify the varying effects of injury and treatment on development of radiographic symptomatic knee OA. Our control cohort experienced no knee injury throughout their lifetimes, providing a baseline OA risk to which all injury cohorts were compared. The three additional cohorts experienced a baseline ACL injury and differed in the presence of MT and modalities of treatment. One cohort sustained a concurrent MT and surgical treatment for their injuries. We recognize that MTs can be treated surgically through partial resection or repair or be left untreated; due to lack of data on the influence of treatment modality of MT in the presence of ACL tears on the subsequent development of OA, we combined patients with ACL tears and MTs into one cohort, regardless of MT treatment. The two remaining cohorts with baseline ACL tear and no MT differed in the treatment performed, with one cohort undergoing ACL reconstruction and the other receiving non-operative treatment for their ACL injury. We calculated the cumulative (lifetime) incidence of knee OA and TKR and quality-adjusted life-expectancies for each cohort. The details of the study population, simulation model, model input parameters, assumptions, and analyses are detailed below.
Study Population
To examine the relationships between knee injury, treatment, and development of subsequent knee OA, we generated four cohorts of hypothetical individuals aged 25 years, without OA at baseline:
Individuals without any injuries at baseline and remained free from knee-injury through their lifetimes (“No Injury Cohort”, referent group);
Individuals with a surgically treated (reconstructed) ACL tear without concomitant MT at baseline (“Surgically Treated ACL without MT Cohort”);
Individuals with non-operative treatment of ACL tear without concomitant MT (“Non-Operatively Treated ACL without MT Cohort”); and
Individuals with both an ACL tear and MT, treated surgically with ACL reconstruction, at baseline (“ACL with MT Cohort”).
While we recognize that treatment practices vary and therefore additional cohorts could have been included, data are currently lacking to inform additional model cohorts. Information regarding population demographics and model assumptions for each of the above cohorts is provided in the section describing input data.
OAPol Model
The OAPol Model18–20 is a validated, state-transition computer simulation model that describes the natural history and clinical management of knee OA using a series of annual transitions between health states. Health states are defined by injury status, development of symptomatic and radiographic knee OA, and knee OA progression. The OAPol model is implemented as a Monte Carlo simulation, where a random number generator and a set of estimated probabilities are used to determine the pathway between health states that each simulated patient follows. The mechanism by which we modeled the impact of these knee injuries is shown in Appendix Figure 1. Subjects entered the simulation at age 25 without OA and either with or without ACL (surgically or non-surgically treated) or MT, depending on the cohort. After initialization, subjects could remain in their current health state, or transition to a new health state, where they could remain for some number of years before transitioning again. Each of these transitions is represented by arrows in the diagram and has a definable probability of occurring. Additionally, subjects can incur comorbidities, such as coronary heart disease or diabetes, and have a chance of death throughout the simulation. Incidence of knee OA was defined by Kellgren-Lawrence (K-L) grade 2 or higher on knee radiograph with concurrent knee pain. Subjects proceeded through different regimens in accordance with OA care treatment guidelines.21–23 Subjects with K-L grade 3 or 4 and knee pain were eligible for TKR. Each individual’s course is tracked until death, and multiple simulations are aggregated into estimates of population-based outcomes and costs. Further details of model specifications, validation, and data have been previously published.18–20
Input Parameters and Model Assumptions
Model input parameters are listed in Table 1 and summarized below.
Table 1.
Model input parameters
| Cohort | ||||||
|---|---|---|---|---|---|---|
| Parameter | No Injury (referent) Base [95% CI] (Range) |
Surgically Treated ACL without MT Base [95% CI] (Range) |
Non-Operatively Treated ACL without MT Base [95% CI] (Range) |
ACL with MT Base [95% CI] (Range) |
References | |
| Age at baseline | 25 | Assumption | ||||
| Female (%) | 49.1% | 25 | ||||
| Meniscal Tear | MT Prevalence at Baseline | 0% | 0% | 0% | 100% | Assumption |
| MT Annual Incidence Probability (Under age 50) | 0% | 0.61% [0.61%, 0.62%] (0.15 – 1.22%) | 0.92% [0.91%, 0.93%] (0.23 – 1.83%) | N/A | 29 | |
| Relative Risk of OA Incidence due to MT | N/A | 2.89 [2.17, 3.85] (2 – 10) | 2.89 [2.17, 3.85] (2 – 10) | 2.89 [2.17, 3.85] (2 – 10) | 16,37–41 | |
| Relative Risk of OA Progression due to MT | N/A | 3.40 [1.80, 6.20] (2 – 6) | 3.40 [1.80, 6.20] (2 – 6) | 3.40 [1.80, 6.20] (2 – 6) | 7 | |
| ACL Tear | ACL Tear Prevalence at Baseline | 0% | 100% | 100% | 100% | Assumption |
| Relative Risk of OA Incidence due to ACL tear | N/A | 1 (1 – 3) | 1 (1 – 3) | 1 (1 – 3) | 37,41 | |
| Relative Risk of OA Progression due to ACL tear | N/A | 1 (1 – 3.4) | 1 (1 – 3.4) | 1 (1 – 3.4) | 7,41,42,45 | |
Base case assumption is that ACL tears do not carry an increased relative risk of OA incidence or progression. However, we performed a sensitivity analysis that assumed ACL tears themselves have as much of an impact on OA incidence and progression as meniscal tears do in our base case.
Population Demographics
The baseline demographic characteristics, including distributions of sex, race/ethnicity, and comorbidity, were derived for non-obese 25 year olds from the National Health and Nutrition Examination Survey (NHANES) 2009–201024 and US Census Population Estimates 2012.25 Mortality was derived from 2010 CDC Life Tables.26
Prevalence and Incidence of ACL and MT
All three ‘ACL’ cohorts assumed 100% prevalence of ACL tear at baseline. Cohorts with history of isolated ACL injuries were at risk for incident MT. The risk for incident MT varied according to age and whether or not the individual had undergone ACL reconstruction at baseline.27,28 We derived rates of MT from a population-based study examining the incidence of meniscal injuries among active-duty US service members between 1998–2006 and converted adjusted rates per 1000 person-years into annual probabilities.29 Literature evaluating the risk of developing a subsequent MT in an ACL-deficient knee is limited. Using clinical expert consensus, we assumed that the probability of developing a subsequent MT was 50% greater in persons with an ACL-deficient knee. MT occurring in ACL-deficient persons below the age of 50 were assumed to arise on the basis of joint laxity; whereas, MT occurring in older individuals was, conservatively, not attributed to ACL tears but rather to age-related degeneration of joint structures. Thus, to be conservative we explicitly incorporated the increased risk of knee OA due to MT that occurred in young years (age 25); for those aged 50 years or older, that risk was indirectly incorporated into underlying incidence rates of knee OA.30–33
Background OA Incidence and Progression
The probability of knee OA incidence in persons without injuries was derived by calibrating the model to prevalence data from the National Health Interview Survey (NHIS) from 2007–2008, with the results having been previously published.20 Annual OA progression rates (percentage of subjects who worsened in K-L grade in a year) ranged from 1.29% for non-obese K-L grade 3 males to 12.26% for obese K-L grade 2 males.19
Increase in OA Incidence and Progression Due to ACL and Meniscal Injuries
While an association between ACL tears and knee OA has been established, the mechanism by which ACL tears impact OA incidence and progression is less clear.34–36 In the main analysis, we made the conservative assumption that OA incidence is not directly affected by ACL injuries.17,37,38 We recognize that injuries resulting in ACL tears may contribute to broader changes – chondral damage, inflammatory changes – that affect OA development, which we explored via sensitivity analyses. Conversely, based upon similar observational data, we assumed that MTs, either occurring concomitantly with ACL tear or developing over time, are associated with increased risks of OA incidence and progression.37–40 We further assumed that, while isolated ACL tears do not directly increase the risk of OA development,37 they do increase the risk of subsequent MTs, regardless of ACL treatment (with that increase varied according to the type of ACL treatment),27,33 thereby increasing the risk of OA development and progression.41 Thus, in the main analysis, all increased risk of OA due to ACL tear is mediated through the concurrent or subsequent MT. We examined the impact of these assumptions on the robustness of our projections in sensitivity analyses.
Data relating the impact of MT on knee OA and the prevalence of MT with ACL injuries are summarized in Table 1. Among cohorts with a MT (either concomitant to a baseline ACL injury or in a subsequent year), the risk of developing OA was assumed to be increased by a factor of 2.89 (95% CI 2.17 – 3.85) compared to the cohort without any ACL or meniscal injury.41 Likewise, OA progression was increased by a factor of 3.40 (95% CI 1.80 – 6.20) for cohorts with MTs compared to the cohort without injuries.42
Main Analysis
For our main analysis, we assumed injury exerted a continuous effect on OA incidence and progression over a person’s life. We calculated the cumulative (lifetime) incidence of knee OA and TKR. We also calculated quality-adjusted life-expectancies (QALEs), though differences in this outcome only varied in relationship to the impact of the injury on OA and TKR, rather than factoring in differences in other functional limitations due to the injury itself.
Sensitivity Analyses
Because of uncertainties in the relationship between ACL injuries and OA and MT, we included multiple sensitivity analyses to address potential vulnerabilities in the assumptions employed in our main analysis. We performed one-way sensitivity analyses varying: OA incidence and progression rates following MT, MT incidence rates in reconstructed and unreconstructed ACL tears, increased risk of subsequent MT in ACL-deficient knees, and increased risk of OA incidence and progression following ACL tear (zero in the main analysis). In addition, we performed several multi-way sensitivity analyses to examine the interrelationship between input parameters, including: 1) varying OA incidence rate following ACL tear simultaneous to OA incidence rate following MT and 2) varying MT incidence rate simultaneous to OA incidence rate following MT. The inputs used for these analyses were based on reasonable variances found in published literature and can be found in Table 1.
Ethics Statement
The study was approved by the Institutional Review Board of Brigham & Women’s Hospital.
Results
Lifetime Risk of Symptomatic Knee OA and TKR (Table 2)
Table 2.
Risk of osteoarthritis, total knee replacement surgery, total knee replacement revision surgery, and meniscal tear prevalence at age 50 among cohorts with different baseline injury statuses
| Cohort | ||||
|---|---|---|---|---|
| Outcome | No Injury (referent) (Cohort 1) Point Estimate [95% CI] |
Surgically Treated ACL without MT (Cohort 2) Point Estimate [95% CI] |
Non-Operatively Treated ACL without MT (Cohort 3) Point Estimate [95% CI] |
ACL with MT (Cohort 4) Point Estimate [95% CI] |
| Lifetime Risk of OA | 13.5% [13.5%, 3.6%] | 16.2% [15.2%, 17.2%] | 17.3% [15.9%, 18.8%] | 34.2% [26.8%, 41.7%] |
| Lifetime Risk of TKR | 6.0% [6.0%, 6.0%] | 8.0% [7.3%, 8.8%] | 8.9% [7.9%, 10.0%] | 22.3% [16.8%, 27.9%] |
| Lifetime Risk of TKR Revision | 0.8% [0.8%, 0.8%] | 1.1% [1.0%, 1.2%] | 1.2% [1.1%, 1.4%] | 3.9% [2.7%, 5.1%] |
| Meniscal Tear Prevalence at Age 50 | 0% | 14.2% [11.9%, 16.5%] | 20.5% [17.3%, 23.6%] | 100% |
In the cohort without baseline or subsequent knee injuries (No Injury Cohort), the lifetime cumulative incidence of symptomatic knee OA was estimated at 13.5%. Subjects who experienced both an ACL tear and a MT by age 25 (ACL with MT Cohort) were 2.5 times more likely to develop OA, with 34.2% (95% CI 26.8% – 41.7%) developing knee OA over their lifetime and 25.2% (95% CI 19.2% – 31.2%), by age 65 (Figure 1). For the cohort with surgically treated ACL tears and no baseline MT (Surgically Treated ACL without MT Cohort), the cumulative lifetime risk of developing knee OA was estimated at 16.2% (95% CI 15.2% – 17.2%). The estimated risk was somewhat higher at 17.3% (95% CI 15.9% – 18.8%) in Non-operatively Treated ACL without MT Cohort subjects.
Figure 1.
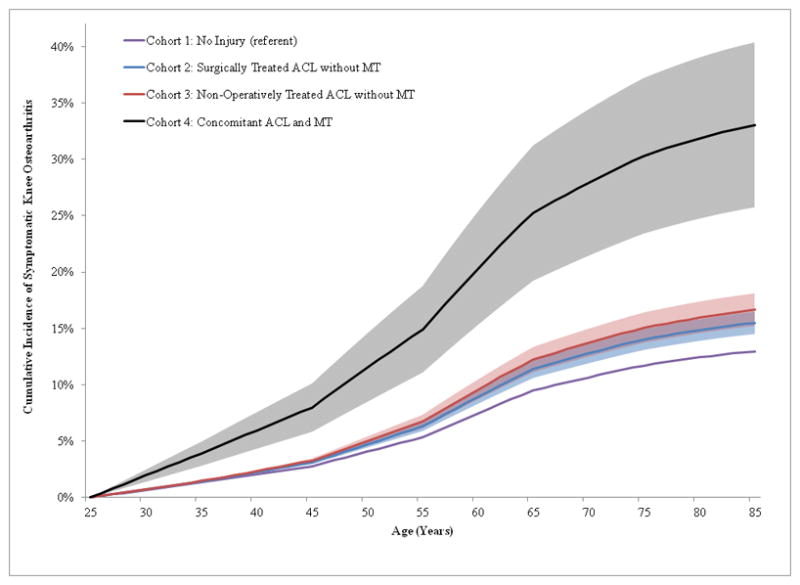
Each cohort was initialized at age 25 with different injury statuses and then tracked to see what proportion developed knee osteoarthritis at some point during an individual’s lifetime. One cohort was initialized without any injury or the possibility of developing an injury in the future to serve as a comparator. Two cohorts began with ACL tears (one treated and the other untreated) and no meniscal tear at baseline, but with a chance to develop a meniscal tear in the future. A fourth cohort had both an ACL tear and a meniscal tear at baseline. Solid lines represent point estimates, and shaded bands indicate 95% confidence intervals.
In the No Injury Cohort, 6.0% of the population underwent TKR surgery. In comparison, the ACL with MT Cohort was nearly four times higher, with 22.3% (95% CI 16.8% – 27.9%) undergoing TKR and 3.9% (95% CI 2.7% – 5.1%) experiencing revision TKR. The Non-operatively Treated ACL without MT Cohort had a lifetime TKR risk of 8.9% (95% CI 7.9% – 10.0%), while the Surgically Treated ACL without MT Cohort had an estimated risk of 8.0% (95% CI 7.3% – 8.8%).
Sensitivity analyses
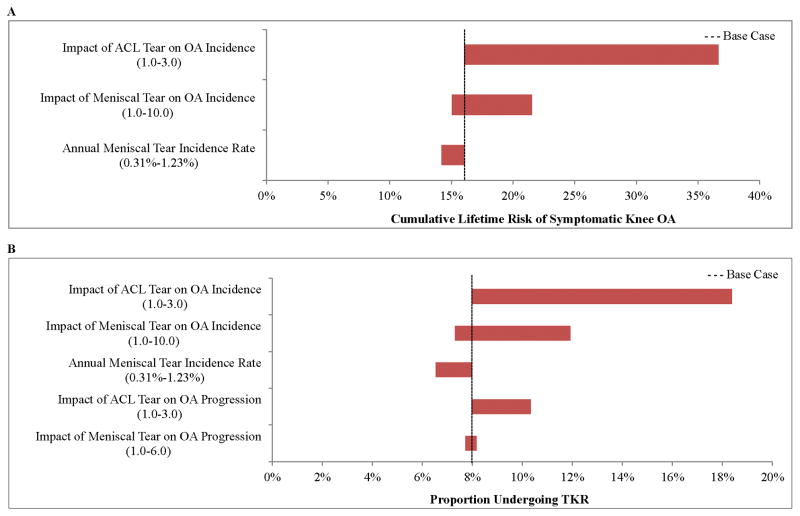
Figure 2 presents two tornado diagrams displaying key one-way sensitivity analyses in the Surgically Treated ACL without MT Cohort. Among this cohort, varying the assumption that ACL tears directly influence OA incidence had the largest impact on lifetime risk of (A) symptomatic knee OA and (B) TKR. In the main analysis, we assumed ACL tears did not directly influence the development of OA. When we assumed that the impact of ACL tears on OA incidence was equal to the impact of MT (a relative risk of 2.89), the lifetime risk of developing knee OA increased from 16.2% to 35.7%. Increasing the direct influence of ACL tears on OA incidence also resulted in an increase in the proportion of the cohort undergoing TKR, ranging from 8.0% in the main analysis to 18.4% when ACL tears were assigned equal influence on OA incidence to MT. Further, varying the impact of MT on OA incidence had a large effect on OA risk and TKR rates, with the parameter carrying the next largest effect being the overall incidence rate of subsequent MT. The relationship between ACL or MT and OA progression was less profound than for OA incidence. Increasing the impact of ACL tears on OA progression increased the proportion of the population undergoing TKR from 8.0% in the main analysis to 10.3%. Increasing the impact of MT on OA progression resulted in less than a 0.5% absolute difference in the proportion of TKRs.
Figure 2.
This figure depicts the results of one-way sensitivity analyses on the cumulative lifetime risk of symptomatic OA (A, horizontal axis) and total knee replacement (B, horizontal axis) in a cohort that had a treated ACL tear at baseline, but no concomitant meniscal tear (Surgically Treated ACL Tear without MT Cohort). The model parameters that were varied are listed on the vertical axis and include: the direct impact of an ACL tear on the incidence of knee OA, the direct impact of a meniscal tear on the incidence of knee OA, the yearly incidence rate of meniscal tears and additionally for TKR risk, the impact of an ACL tear on OA progression and the impact of a meniscal tear on OA progression. The horizontal bars indicate how changes in model input assumptions impact either OA risk or TKR, compared to the base case assumptions which are noted by the vertical dashed lines.
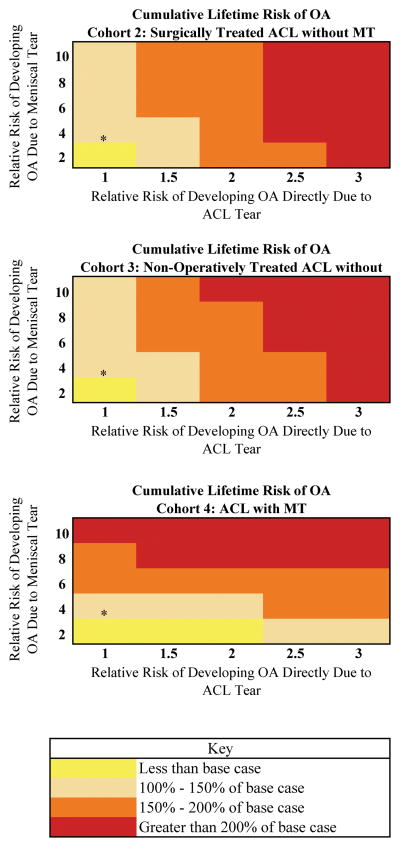
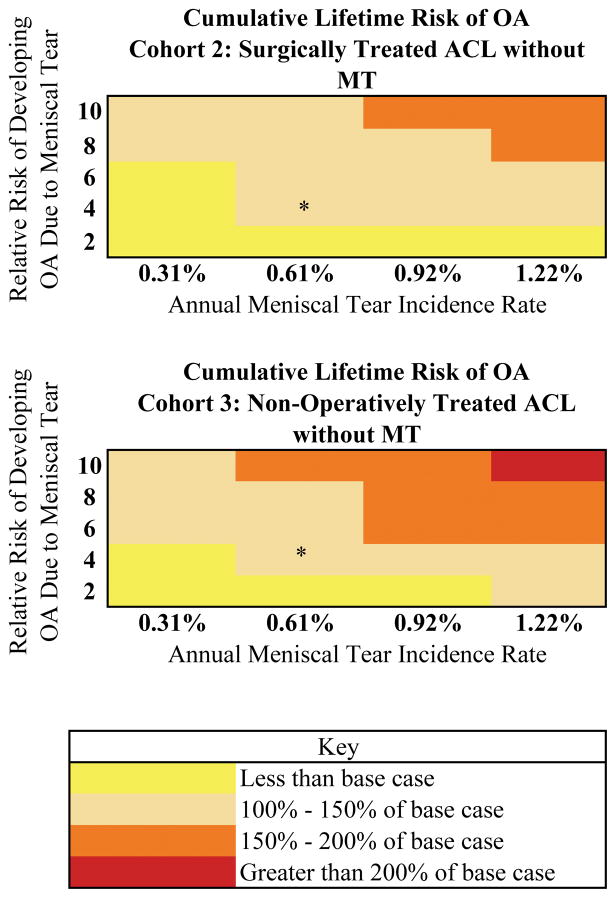
Figure 3 depicts the results of a two-way sensitivity analysis evaluating the influence of ACL and MT on OA incidence and the resulting impact on cumulative lifetime risk of symptomatic OA. For cohorts without MT at baseline (Non-Operatively Treated ACL without MT and Surgically Treated ACL without MT Cohorts), increasing the influence of ACL tears on OA incidence had a greater impact on lifetime OA risk than increasing the influence of MT on OA incidence. Conversely, in the ACL with MT Cohort, increasing the influence of MT on OA incidence had a greater impact on lifetime OA risk than increasing the influence of ACL tears. On the other hand, the influence of simultaneously increasing the relative risk of OA development directly due to MT and the annual MT incidence rate were similar regardless of whether the patients had baseline MTs or not (Figure 4).
Figure 3.
The figure shows the effects of concurrently varying the relative risks of knee OA incidence due to ACL tears and meniscal tears in cohorts with either surgically or non-surgically treated ACL tear without meniscal tear at baseline or in a cohort with prevalent history of ACL tear with concomitant meniscal tear. Asterisk denotes base case assumptions.
Figure 4.
The figure shows the effects of concurrently varying the incidence rate of meniscal tear and the relative risk of knee OA incidence due to meniscal tear in cohorts with either surgically or non-surgically treated ACL tear without meniscal tear at baseline. Asterisk denotes base case assumptions.
Discussion
We used simulation modeling to estimate the cumulative incidence of knee OA and the proportion of the population undergoing TKR following ACL injury with or without concomitant MT in young adults. We found that an early ACL injury with a concomitant MT led to an estimated lifetime risk of knee OA of 34%. Preventing just half of these injuries would reduce the number of persons with OA by about 10%. Cohorts sustaining ACL injury without concomitant MT had estimated lifetime risks of knee OA of 16% to 17%, depending on ACL treatment modality. Similarly, the risk of TKR was 22% in the ACL and MT cohort – nearly four times greater than the no injury cohort – such that reducing half of these injuries would lead to 8% fewer TKR surgeries.
Our results over the shorter duration are consistent with prior systematic reviews of OA after knee injuries, which reported a prevalence of knee OA for subjects with isolated ACL injury of 0% to 13% at 10 years after initial injury. Additionally, the review by Oiestad and colleagues suggests a risk of knee OA of 21% to 48% for patients with combined ACL and meniscal injuries.17 The results of the analyses we present are also consistent with the overall lifetime risk of symptomatic knee OA of 14%, which was established using a cohort with the same starting age.20 An additional analysis by Murphy and colleagues43 reports the lifetime risk of knee OA at 57% for those with history of knee injury; while our estimates for those with ACL injury are more conservative compared to the estimates presented by Murphy et al.,43 it is likely explained by the differences in obesity distribution (the majority of Johnston County Osteoarthritis Project sample has been reported to be overweight or obese) and lack of specificity of knee injury definition. In addition, we were able to explicitly adjust for mortality in our analyses.
There are limitations to our analysis. In our main analysis, we assumed that isolated ACL tears do not affect OA incidence and progression, an assumption based on limited evidence.17,37,38,44 However, this provides a more conservative estimate of the total impact of ACL tears, and we performed sensitivity analyses to evaluate the potential impact of ACL tears themselves may have on our findings. Our data sources for the increase in relative risk of OA development due to MT or ACL injury were also limited; however, we sought to use more conservative estimates from among those presented in the literature. Our use of MT incidence and progression data from older populations may under- or overestimate the incidence of OA, depending upon individual activity levels and subsequent meniscal injury rates. Where published data were unavailable, we used expert consensus, but tested these assumptions through extensive sensitivity analyses. We assumed continuous risk due to the initial injury, and, while it is unclear whether there is a defined duration during which these injuries impact the incidence of OA, our results are consistent with published estimates of knee OA among younger individuals.45,46 We did not examine the use or timing of ACL reconstruction surgeries, as evidence suggests that the specific treatment used does not have a substantial impact on OA.11 We did not consider gender differences in the impact of early injury on OA incidence and progression, due to lack of compelling evidence suggesting such differences, but we did consider gender-specific baseline OA incidence rates. We assumed all cohorts were 49% female at age 25 years, a proportion derived from US Census population estimates.24 Although literature suggests ACL tears are more common in female athletes than male athletes, athletes are not representative of the general population, which is the cohort of interest in our analyses. A study by Sanders and colleagues evaluating the incidence of ACL tears in a population-based cohort found a significantly higher incidence of ACL injuries in men than women, regardless of age.47 Additionally, data published by Kaiser on the rate of ACL reconstruction indicates that men undergo more ACL reconstructions than women.48 Therefore, assuming a sex distribution comparable to the US population produces estimates of cumulative lifetime incidence applicable to the general population. While our use of multiple data sources required synthesizing parameters gathered from distinct populations, it also allows for greater generalizability of our findings.
Our findings suggest that early traumatic ACL injuries may have dramatic effects on cumulative lifetime incidence of knee OA and the need for TKR. Since knee injuries have been shown to be preventable through the use of targeted training programs,6,49,50 our findings provide important information for policy makers and stakeholders to prioritize programs for injury prevention among young adults at risk of knee injury. Concomitant MT appears to play an important role in OA incidence and progression following early injury, but data are needed to delineate more clearly the persistence, not just the strength, of the effect of injuries on knee OA development and progression. Strategies to prevent early injuries are likely to provide significant societal benefit due to reduction in subsequent rates of OA incidence.
Supplementary Material
The diagram shows a basic sequence of injury and disease states as a subject progresses through the OAPol Model. Death can occur at any time. In addition, the incidence of comorbidities, changes in BMI status, treatment sequences, and many other elements are not shown.
Significance and Innovations.
Early traumatic ACL injuries lead to increased lifetime risk of knee OA and earlier disease onset.
Persons sustaining ACL injury with concomitant meniscal tear in early adulthood are four times more likely to undergo TKR than persons without history of injury.
Acknowledgments
Funding: This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers); NIH/NIAMS (grants AR064320, AR47782, AR057827). Dr. Suter is currently supported in part by the VA Connecticut Healthcare System.
Footnotes
Disclosures: Dr. Suter develops healthcare quality measures for the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services, under Contract Number HHSM-500-2013-13018I-T0001, entitled “Measure & Instrument Development and Support (MIDS)-Development, Reevaluation, and Implementation of Hospital Outcome/Efficiency Measures.”
Author Contributions: Dr. Suter had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conception and design: Suter, Losina
Collection and assembly of data: Suter, Smith, Losina
Analysis and interpretation of the data: Suter, Smith, Katz, Englund, Hunter, Frobell, Losina
Statistical expertise: Losina
Drafting of the article: Suter, Smith, Losina
Critical revision of the article for important intellectual content: Suter, Smith, Katz, Englund, Hunter, Frobell, Losina
Final approval of the article: Suter, Smith, Katz, Englund, Hunter, Frobell, Losina
Obtaining of funding: Suter, Losina
Role of the Funding Source: Harvard Catalyst, NIAMS, and VA Connecticut Healthcare System funded this work but had no role in its design, conduct, or reporting.
References
- 1.Frobell RB, Lohmander LS, Roos HP. Acute rotational trauma to the knee: poor agreement between clinical assessment and magnetic resonance imaging findings. Scand J Med Sci Sports. 2007;17:109–114. doi: 10.1111/j.1600-0838.2006.00559.x. [DOI] [PubMed] [Google Scholar]
- 2.Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Fellander-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40:1808–1813. doi: 10.1177/0363546512449306. [DOI] [PubMed] [Google Scholar]
- 3.Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999:272–282. [PubMed] [Google Scholar]
- 4.Leininger RE, Knox CL, Comstock RD. Epidemiology of 1. 6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35:288–293. doi: 10.1177/0363546506294060. [DOI] [PubMed] [Google Scholar]
- 5.Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat. 1998;13:1–119. [PubMed] [Google Scholar]
- 6.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325. e1326. doi: 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Kilcoyne KG, Dickens JF, Haniuk E, Cameron KL, Owens BD. Epidemiology of meniscal injury associated with ACL tears in young athletes. Orthopedics. 2012;35:208–212. doi: 10.3928/01477447-20120222-07. [DOI] [PubMed] [Google Scholar]
- 8.Samora WP, 3rd, Palmer R, Klingele KE. Meniscal pathology associated with acute anterior cruciate ligament tears in patients with open physes. J Pediatr Orthop. 2011;31:272–276. doi: 10.1097/BPO.0b013e31820fc6b8. [DOI] [PubMed] [Google Scholar]
- 9.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346:f232. doi: 10.1136/bmj.f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brophy RH, Wright RW, Matava MJ. Cost analysis of converting from single-bundle to double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:683–687. doi: 10.1177/0363546508328121. [DOI] [PubMed] [Google Scholar]
- 11.Englund M, Felson DT, Guermazi A, Roemer FW, Wang K, Crema MD, et al. Risk factors for medial meniscal pathology on knee MRI in older US adults: a multicentre prospective cohort study. Ann Rheum Dis. 2011;70:1733–1739. doi: 10.1136/ard.2011.150052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takeda H, Nakagawa T, Nakamura K, Engebretsen L. Prevention and management of knee osteoarthritis and knee cartilage injury in sports. Br J Sports Med. 2011;45:304–309. doi: 10.1136/bjsm.2010.082321. [DOI] [PubMed] [Google Scholar]
- 13.Raynauld JP, Martel-Pelletier J, Haraoui B, Choquette D, Dorais M, Wildi LM, et al. Risk factors predictive of joint replacement in a 2-year multicentre clinical trial in knee osteoarthritis using MRI: results from over 6 years of observation. Ann Rheum Dis. 2011;70:1382–1388. doi: 10.1136/ard.2010.146407. [DOI] [PubMed] [Google Scholar]
- 14.Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B, Aliabadi P, et al. Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum. 1997;40:728–733. doi: 10.1002/art.1780400420. [DOI] [PubMed] [Google Scholar]
- 15.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995;3:261–267. doi: 10.1016/s1063-4584(05)80017-2. [DOI] [PubMed] [Google Scholar]
- 16.Wilder FV, Hall BJ, Barrett JP, Lemrow NB. History of acute knee injury and osteoarthritis of the knee: a prospective epidemiological assessment: The Clearwater Osteoarthritis Study. Osteoarthritis and Cartilage. 2002;10:611–616. doi: 10.1053/joca.2002.0795. [DOI] [PubMed] [Google Scholar]
- 17.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 18.Losina E, Paltiel AD, Weinstein AM, Yelin E, Hunter DJ, Chen SP, et al. Lifetime medical costs of knee osteoarthritis management in the United States: impact of extending indications for total knee arthroplasty. Arthritis Care Res (Hoboken) 2015;67:203–215. doi: 10.1002/acr.22412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holt HL, Katz JN, Reichmann WM, Gerlovin H, Wright EA, Hunter DJ, et al. Forecasting the burden of advanced knee osteoarthritis over a 10-year period in a cohort of 60–64 year-old US adults. Osteoarthritis Cartilage. 2011;19:44–50. doi: 10.1016/j.joca.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME, et al. Lifetime risk and age of diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken) 2012 doi: 10.1002/acr.21898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 22.Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137–162. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 23.Richmond J, Hunter D, Irrgang J, Jones MH, Snyder-Mackler L, Van Durme D, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg Am. 2010;92:990–993. doi: 10.2106/JBJS.I.00982. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) 2009–2010 National Health and Nutrition Examination Survey (NHANES) Data. Hyattsville, MD: National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 25.Annual Estimates of the Hispanic, White, and Black Resident Populations by Sex and Age for the United States: April 1, 2000 to July 1, 2009 (NC-EST2009-04-HISP/WANH/BA) US Census Bureau, Population Division; 2010. June 2010 ed. [Google Scholar]
- 26.Arias E. National Vital Statistics Reports. Vol. 63. Hyattsville, MD: National Center for Health Statistics; 2014. United States Life Tables, 2010. [PubMed] [Google Scholar]
- 27.Anstey DE, Heyworth BE, Price MD, Gill TJ. Effect of timing of ACL reconstruction in surgery and development of meniscal and chondral lesions. Phys Sportsmed. 2012;40:36–40. doi: 10.3810/psm.2012.02.1949. [DOI] [PubMed] [Google Scholar]
- 28.Jiang W, Gao SG, Li KH, Luo L, Li YS, Luo W, et al. Impact of Partial and complete rupture of anterior cruciate ligament on medial meniscus: A cadavaric study. Indian J Orthop. 2012;46:514–519. doi: 10.4103/0019-5413.101040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones JC, Burks R, Owens BD, Sturdivant RX, Svoboda SJ, Cameron KL. Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train. 2012;47:67–73. doi: 10.4085/1062-6050-47.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ichinohe S, Yoshida M, Murakami H, Takayama H, Izumiyama S, Shimamura T. Meniscal tearing after ACL reconstruction. J Orthop Surg (Hong Kong) 2000;8:53–59. doi: 10.1177/230949900000800110. [DOI] [PubMed] [Google Scholar]
- 31.Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87:1639–1642. doi: 10.1302/0301-620X.87B12.16916. [DOI] [PubMed] [Google Scholar]
- 32.Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262–270. doi: 10.1007/s00167-003-0398-z. [DOI] [PubMed] [Google Scholar]
- 33.Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1438–1444. doi: 10.1007/s00167-007-0414-9. [DOI] [PubMed] [Google Scholar]
- 34.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 35.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27:143–156. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 36.Lohmander LS, Roos H. Knee ligament injury, surgery and osteoarthrosis. Truth or consequences? Acta Orthop Scand. 1994;65:605–609. doi: 10.3109/17453679408994613. [DOI] [PubMed] [Google Scholar]
- 37.Neuman P, Englund M, Kostogiannis I, Fridén T, Roos H, Dahlberg LE. Prevalence of Tibiofemoral Osteoarthritis 15 Years After Nonoperative Treatment of Anterior Cruciate Ligament Injury. Am J Sports Med. 2008;36:1717–1725. doi: 10.1177/0363546508316770. [DOI] [PubMed] [Google Scholar]
- 38.Hart AJ, Buscombe J, Malone A, Dowd GS. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br. 2005;87:1483–1487. doi: 10.1302/0301-620X.87B11.16138. [DOI] [PubMed] [Google Scholar]
- 39.Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36:1275–1282. doi: 10.1177/0363546508314721. [DOI] [PubMed] [Google Scholar]
- 40.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Englund M, Guermazi A, Roemer FW, Aliabadi P, Yang M, Lewis CE, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60:831–839. doi: 10.1002/art.24383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 43.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoffelner T, Resch H, Moroder P, Atzwanger J, Wiplinger M, Hitzl W, et al. No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy. 2012;28:517–525. doi: 10.1016/j.arthro.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 45.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20:739–744. doi: 10.1097/01.bot.0000246468.80635.ef. [DOI] [PubMed] [Google Scholar]
- 46.Roos EM. Joint injury causes knee osteoarthritis in young adults. Curr Opin Rheumatol. 2005;17:195–200. doi: 10.1097/01.bor.0000151406.64393.00. [DOI] [PubMed] [Google Scholar]
- 47.Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med. 2016 doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 48.Csintalan RP, Inacio MC, Funahashi TT. Incidence rate of anterior cruciate ligament reconstructions. Perm J. 2008;12:17–21. doi: 10.7812/tpp/07-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lazaro-Haro C, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859–879. doi: 10.1007/s00167-009-0823-z. [DOI] [PubMed] [Google Scholar]
- 50.Silvers HJ, Giza ER, Mandelbaum BR. Anterior cruciate ligament tear prevention in the female athlete. Curr Sports Med Rep. 2005;4:341–343. doi: 10.1097/01.csmr.0000306297.57331.f2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The diagram shows a basic sequence of injury and disease states as a subject progresses through the OAPol Model. Death can occur at any time. In addition, the incidence of comorbidities, changes in BMI status, treatment sequences, and many other elements are not shown.