Abstract
Objective
First line treatments for posttraumatic stress disorder (PTSD) are often implemented twice per week in efficacy trials. However, there is considerable variability in the frequency of treatment sessions (e.g., once per week or twice per week) in clinical practice. Moreover, clients often cancel or reschedule treatment sessions leading to even greater variability in treatment session timing. The goal of the current study is to investigate the impact of PTSD treatment session frequency on treatment outcome.
Method
136 women [Mage = 32.16 (9.90)] with PTSD were randomized to receive cognitive processing therapy (CPT) or prolonged exposure (PE). PTSD symptom outcome was measured using the Clinician Administered PTSD Scale, and session frequency and consistency were measured using dates of treatment session attendance. Session frequency was operationalized using average days between session and consistency was defined by the standard deviation of the number of days between treatment sessions.
Results
Piecewise growth curve modeling revealed that higher average days between sessions was associated with significantly smaller PTSD symptom reduction with more frequent sessions yielding greater PTSD symptom reduction (p < .001, d = .82). Higher consistency was also associated with significantly greater PTSD symptom reduction (p < .01, d = .48). The substantially larger effect size for frequency suggests that average days between treatment sessions impacts treatment outcome more than consistency. Follow-up analyses revealed a longer time interval between sessions 4 and 5 was associated with smaller reductions in PTSD treatment outcome.
Conclusions
More frequent scheduling of sessions may maximize PTSD treatment outcomes.
Keywords: treatment outcome, session timing, posttraumatic stress disorder, cognitive processing therapy, prolonged exposure
Given the relatively high rate of dropout in trauma-focused psychotherapy (Imel, Laska, Jakupcak, & Simpson, 2013), there has been increased attention to identifying moderators of treatment outcome and predictors of treatment dropout, with most of this work focusing on demographic variables (e.g., educational level, age, time since trauma event). Unfortunately, findings from these studies have been mixed. (e.g., Cloitre, Stovall-McClough, Miranda, & Chemtob, 2004; Foa, Riggs, Massie, Yarczower, 1995; Iverson et al., 2011; Rizvi, Vogt, & Resick, 2009; van Minnen, Arntz, Keijers, 2002). Accordingly, there remain more questions than answers with respect to understanding moderators of treatment outcome.
One factor that may serve as an important indicator of treatment outcome is the time between treatment sessions. Manualized evidence-based treatments for anxiety and traumatic stress disorders make recommendations about session timing (e.g., Foa, Yadin, Lichner, 2012; Foa, Hembree, & Rothbaum, 2007; Resick et al, 2002), with some trauma-focused protocols recommending twice weekly sessions. Furthermore, PTSD efficacy trials for both Prolonged Exposure (PE; Foa, Rothbaum, Riggs, & Murdock, 1991) and Cognitive Processing Therapy (CPT; Resick & Schnicke, 1992) have often used a twice per week session format (e.g., Monson et al., 2006; Resick et al, 2002; 2008; Resick et al. 2015; Foa, Rothbaum, Riggs, & Murdock, 1991), while some PTSD treatment studies followed a weekly format (e.g., Bryant et al. 2008; Foa et al., 2005; Schnurr et al., 2007; Galovski, Blain, Mott, Elwood & Houle, 2012). Despite the clear protocols used in these randomized controlled trials, participants reschedule and cancel appointments, impacting the frequency of session attendance. This pattern of rescheduling and canceling appointments has led to efficacy protocols having guidelines about the maximum amount of time that is permitted to complete treatment. For instance, Resick and colleagues (2008) aimed to have participants attend twice weekly sessions for 6 weeks, however, they required completion of treatment in 12 weeks given the expectation that some participants would not attend sessions as indicated in the protocol or there might be competing appointments or illness.
Further complicating this issue is that the twice per week protocol used in randomized controlled trials for trauma-focused treatment are rarely followed in clinical practice settings (Spoont, Murdoch, Hodges, & Nugent, 2010). In clinical practice settings treatment sessions are more often scheduled once per week or less frequently depending on the demands and available resources in a particular clinic. Indeed, the clinical demands (e.g., too many clinical hours, significant administrative responsibilities, clinics being understaffed) of mental health care clinics may not permit more frequent scheduling of treatment sessions (Finley et al., 2015). Importantly, the efficacy data obtained in randomized controlled trials may not translate to clinical practice settings given the differences in frequency of treatment sessions. Although speculative, it is possible that inconsistent treatment session attendance may be a proxy variable for treatment engagement. To date, session timing has been examined in depression, and broadly across psychopathology in naturalistic data (e.g., Cuijpers, Huibers, Ebert, Koole, & Andersson, 2013; Erekson, Lambert, & Eggett, in press). Findings demonstrate an association between concentrating sessions over a shorter duration and greater symptom change. Other research has examined the impact of 18-hours of cognitive behavioral therapy for PTSD over 5 to 7 workdays compared to weekly treatment (Ehlers et al., 2010; Ehlers et al., 2014). Results indicate comparable findings to weekly treatment delivered over 3-months. Taken together, it is important to investigate whether frequency of treatment sessions affects PTSD treatment outcome with gold standard PTSD treatments, including PE and CPT.
The primary goal of the current study is to examine whether session frequency (i.e., mean number of days between sessions) and consistency (standard deviation of number of days between session) predicts PTSD treatment outcome at both post-treatment assessment and at the follow-up assessments (3-months, 9-months, 5-years). Given the recommended twice-weekly sessions, we hypothesize that both frequency and consistency of sessions will be significantly related to PTSD treatment outcome. The second goal of the study is exploratory. Specifically, given anecdotal evidence of treatment dropout around certain treatment-related assignments (e.g., in vivo exposures, imaginal exposures, writing a trauma account) for both PE and CPT (sessions 2–3, 3–4, 4–5) and evidence of early dropout (i.e., session 3; Khele-Forbes, Meis, Spoont, & Polusney, 2015), exploratory analyses will examine whether length of time between these particular sessions impacts outcome.
Method
Participants
Data were drawn from women who met eligibility criteria for a randomized controlled trial comparing CPT and PE (Resick et al., 2002). The ITT sample of the trial consisted of 171 participants. Because the current study focused on timing between sessions, we included data from 136 participants (79.5% of the ITT) who attended at least the first two treatment sessions. Participants were included in the study if they were 18 years of age or older, female, and met criteria for DSM-IV diagnosis of PTSD related to interpersonal violence. Participants were excluded for current psychosis, current suicidality, current diagnosis of substance dependence, illiteracy, or currently engaged in an abusive relationship or a dangerous situation such as being stalked. Participants were recruited from the greater metropolitan St. Louis, Missouri area. The sample included in the current study had a mean age of 32.16 (SD = 9.90), mean of 14.59 (SD = 2.31) years of education, a mean of 103.75 (SD = 100.55) months since their primary trauma, and were self-identified as 75.7% White, 19.9% Black, and 4.4% other.
Measures
Clinician-Administered PTSD Scale-DSM-IV (CAPS; Blake et al., 1995)
The CAPS is a 17-item clinician-administered measure for PTSD diagnostic criteria outlined in the Diagnostic Statistical Manual of Mental Disorders-IV (DSM-IV; American Psychiatric Association, 1994). The measure yields both a diagnostic measure and a total severity score that includes both symptom frequency and intensity scores, which are each rated separately. The CAPS has demonstrated strong psychometric properties (Blake et al., 1995; Weathers, Keane, & Davidson, 2001). The CAPS was the primary treatment outcome measure, which was assessed as the total PTSD symptom severity score taken at baseline, post-treatment, and at follow up assessments (3-month, 9-month, 5-year).
Session Timing
Session and assessment dates were recorded at each visit and used to calculate both session frequency and consistency. Session frequency was computed as a mean number of days between session, and session consistency was the standard deviation of the number of days between sessions.
Procedure
The study was conducted in accordance with approved procedures from the Institutional Review Board (IRB) of the University of St. Louis, Missouri, with the new analyses approved by the IRB of VA Boston Healthcare System. As previously reported (e.g., Resick et al., 2002), participants completed a brief telephone screen prior to their initial assessment, at which time written informed consent was obtain prior to the baseline assessment. All eligible participants were then randomized to one of the treatment conditions prior to the start of treatment. Some of these participants dropped out prior to attending the first session (see, Gutner, Gallagher, Baker, Sloan, & Resick, 2016).
All women were randomly assigned to receive PE, CPT, or minimal attention waitlist (MA; Resick et al., 2002). PE and CPT were scheduled with the intention of having twice weekly sessions over the course of 6-weeks. PE (Foa, Hearst, Dancu, Hembree, & Jaycox, 1994) and CPT (Resick & Schnicke, 1993) are gold standard PTSD treatments that utilize different mechanisms of change for symptom reduction (Gallagher & Resick, 2012). PE is designed to facilitate recovery of PTSD through extinction learning during imaginal and in vivo exposures. Alternatively, CPT is founded in cognitive theory and relies on modification of distorted beliefs and cognitive processing of emotional information for symptom reduction. Both conditions had a total of 13 hours in treatment. The PE condition involved a total of nine sessions, the first of which was 60 minutes, with the remainder lasting for 90 minutes a session. With respect to CPT, there were 12, 60-minute sessions with the exception of sessions 4 and 5, which were 90 minutes in duration in order to match the number of therapy hours of PE. For the MA condition, participants were informed that they would be eligible for treatment after a 6-week waiting period (and had been pre-randomized after initial assessment despite both the staff and participant initially remaining blind to randomized condition), with check-in phone calls from clinicians every 2 weeks to ensure there were no emergencies requiring immediate attention. At the conclusion of the 6-week period (which served as a no-treatment control condition), individuals in the MA condition began the therapy they had been randomized to and are included in this study.
Data Analytic Plan
Analyses were all retrospective and conducted with archival data previously collected by Resick and colleagues (2002). Piecewise multilevel growth curve modeling was used to examine change over time in PTSD symptoms with the software package Hierarchical Linear and NonLinear Modeling (HLM 6.34: Raudenbush, Bryk, & Congdon, 2005) using full maximum likelihood estimation. Multilevel growth curve modeling is particularly well-suited for the current data because there was considerable amount of variation in the timing of the assessments, particularly for the long-term follow-up assessment. To account for this variability we modeled time as number of days since baseline assessment. Piece-wise modeling of the outcomes over time was used to estimate different slopes from pre- to post-treatment (epoch 1) and post-treatment to long-term follow-up (epoch 2) using procedures described by Singer and Willett (2003, Chapter 6). Trajectories of both epochs were tested simultaneously by including two time variables: (a) the number of days since baseline assessment with the baseline assessment coded as zero, and (b) the number of days since the post-treatment assessment (with all time points prior to post-treatment coded as zero). The coefficient for the first time variable represents change over time from pre- to post-treatment (epoch 1), while the coefficient for the second time variable represent the difference in rate of change between epoch 1 and epoch 2 (the follow-up period). To estimate change during epoch 2, the time variables were recoded such that the variable representing number of days since baseline assessment was centered at the post-treatment assessment and the second time variable represented the number of days since baseline assessment with post-treatment assessments coded as zero. This re-parameterization sets up the identical overall model as the first; however, the time coefficients provide slightly different information with the first being change during the follow-up period and the second, as with the original parameterization, represents the difference in rate of change between the two epochs.
All time coefficients described above were modeled as random effects, which specifies variation in the time coefficients across participants. Predictor variables (average number of days between sessions, standard deviation of days between sessions, a dummy coded treatment variable, and interactions terms) and one covariate (percent of sessions attended) were included as Level-2 predictors for each of the time coefficients described above to evaluate how they influenced change in PTSD symptoms (Cohen, Cohen, West, & Aiken, 2003). Continuous predictor variables and covariates were grand mean centered, treatment condition was modeled using a dummy coded variable, and product terms were used to analyze interactions. Cohen’s d (d; .25 small, .50 medium, .80 large; Cohen, 1988) was calculated as an estimate of effect size using the formula . Another advantage of multilevel growth curve modeling is that it allowed us to conduct the data on the largest sample size possible because it is robust to missing data at Level 1 (i.e., measures assessed over time).
Results
Table 1 displays the descriptive statistics for all of the time and predictor variables as well as the covariate, percent sessions attended. None of these variables differed significantly as a function of treatment condition. The range of timing between sessions across the sample were as follows: average days between sessions (2–32), Session 2 to 3 (2–19), Session 3 to 4 (2–71), and Session 5 (1–22). Mean number of days between treatment sessions (r = −.09, p = .287) and consistency (r = .034, p = .701) were not significantly related to pretreatment CAPS scores. Percent of treatment sessions attended exhibited significant negative associations with average frequency (r = −.24, p = .006) and average consistency (r = −.19, p = .031), speaking to the need to include this variable as a covariate. Of note, percent of treatment sessions attended did not include those who completed only one session, as these individuals were not included in analyses. We examined associations between mean number of days between treatment sessions, consistency, and several demographic variables including age, years of education, minority status, income level, and years since index rape. The only significant associations to emerge were between minority status and mean number of days between sessions (r = .29, p = .001) and minority status and consistency (r = .22, p = .015) indicating that compared to participants identifying as Caucasian, participants identifying as belonging to a minority ethnic group tended to have more time elapsed between sessions and attend sessions in a less consistent manner.1
Table 1.
Descriptive Statistics for CAPS scores at each assessment and Predictors and Covariate
| Variable | One-Way | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | CPT | PE | ANOVA | |||||||||
| N | M | SD | n | M | SD | n | M | SD | F | df | p | |
| CAPS Pre-Treatment | 136 | 74.82 | 18.80 | 68 | 74.60 | 18.79 | 68 | 75.03 | 18.94 | |||
| CAPS Post-Treatment | 110 | 23.67 | 19.35 | 55 | 22.82 | 16.94 | 55 | 24.53 | 21.62 | |||
| CAPS 3-Month Follow-Up | 101 | 28.04 | 22.20 | 50 | 26.06 | 19.33 | 51 | 29.98 | 24.74 | |||
| CAPS 9-Month Follow-Up | 80 | 24.46 | 20.10 | 41 | 26.85 | 22.69 | 39 | 21.95 | 16.89 | |||
| CAPS Long Term Follow-Up | 109 | 24.96 | 24.64 | 54 | 25.28 | 24.35 | 55 | 24.65 | 25.14 | |||
| Average Days Between Sessions | 136 | 5.48 | 3.29 | 68 | 5.82 | 4.01 | 68 | 5.15 | 2.34 | 1.44 | 1, 134 | 0.23 |
| Standard Deviation of Days | ||||||||||||
| Between Sessions | 127 | 3.27 | 4.45 | 65 | 3.78 | 5.80 | 62 | 2.73 | 2.24 | 1.77 | 1, 125 | 0.19 |
| Days Between Sessions 2 and 3 | 126 | 5.08 | 2.82 | 64 | 5.09 | 2.59 | 62 | 5.06 | 3.06 | 0.00 | 1, 124 | 0.95 |
| Days Between Sessions 3 and 4 | 123 | 5.07 | 6.55 | 64 | 5.97 | 8.85 | 59 | 4.08 | 1.80 | 2.57 | 1, 121 | 0.11 |
| Days Between Sessions 4 and 5 | 115 | 4.77 | 3.34 | 59 | 5.02 | 3.88 | 56 | 4.52 | 2.66 | 0.64 | 1, 113 | 0.43 |
| Percent of Sessions Completed | 136 | 0.88 | 0.26 | 68 | 0.88 | 0.26 | 68 | 0.88 | 0.26 | 0.00 | 1, 134 | 0.96 |
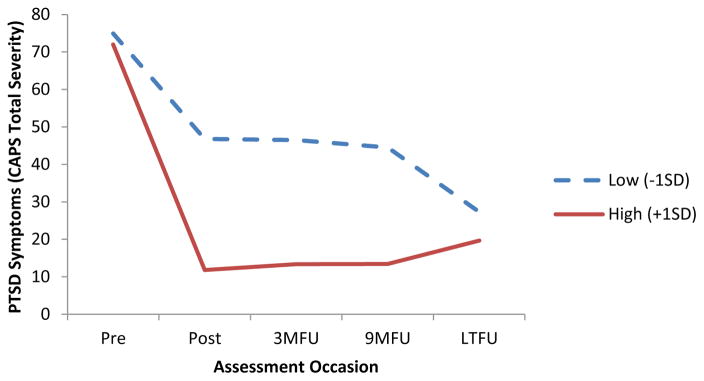
Table 2 provides the coefficients for the predictor x time (analyses labeled “a”) and predictor x time interactions (analyses labeled “b”)2. Analysis 1a indicated that the percent of treatment sessions attended significantly impacted change from both pre- to post-treatment and post-treatment through the long-term follow-up period. Figure 1 illustrates that participants who attended more sessions (labeled high in Figure 1) showed larger decreases pre- to post-treatment relative to those who attended fewer sessions (labeled low in Figure 1); however, this effect reversed from post-treatment through the long-term follow-up, as percentage of sessions attended was significantly and positively associated with change during the follow up period with those showing high levels of percentage attended exhibiting slight increases during this period and those exhibiting low levels of percentage attended exhibiting slight decreases in PTSD symptoms. Percentage of sessions attended was included as a covariate in all subsequent analyses. Because this covariate was grand mean centered, all subsequent analyses can be interpreted as the effect when holding percent sessions attended constant at its mean.
Table 2.
Coefficients for the Predictor x Time and Predictor x Time Interactions
| Change During Treatment | Change During Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | t | p | d | b | t | p | d | |||
| Analysis | Predictor | |||||||||
| 1a | Percent Sessions Attended | Overall | −0.86 | −4.56 | .000 | −0.79 | 0.02 | 4.37 | .000 | 0.75 |
| 2a | Frequency (M) | Overall | 0.05 | 4.76 | .000 | 0.82 | 0.00 | 0.54 | .593 | 0.09 |
| 2b | Frequency (M) | PE | 0.06 | 4.60 | .000 | 0.80 | 0.00 | 0.94 | .349 | 0.16 |
| CPT | 0.05 | 3.42 | .001 | 0.60 | 0.00 | −0.39 | .694 | −0.07 | ||
| Group x Time | 0.01 | 0.54 | .590 | 0.09 | 0.00 | 0.99 | .323 | 0.17 | ||
| 3a | Consistency (SD) | Overall | 0.02 | 2.67 | .009 | 0.48 | 0.00 | 0.66 | .512 | 0.12 |
| 3b | Consistency (SD) | PE | 0.03 | 1.37 | .174 | 0.25 | 0.00 | 1.00 | .319 | 0.18 |
| CPT | 0.02 | 2.16 | .032 | 0.39 | 0.00 | −0.36 | .722 | −0.06 | ||
| Group x Time | 0.01 | 0.23 | .818 | 0.04 | 0.00 | 1.04 | .299 | 0.19 | ||
| 4a | Days btw S2 and S3 | Overall | 0.02 | 1.13 | .260 | 0.20 | 0.00 | −0.97 | .333 | −0.18 |
| 4b | Days bw S2 and S3 | PE | 0.00 | 0.09 | .929 | 0.02 | 0.00 | −0.68 | .497 | 0.00 |
| CPT | 0.04 | 1.94 | .054 | 0.35 | 0.00 | −0.55 | .582 | −0.10 | ||
| Group x Time | 0.04 | 1.43 | .155 | 0.26 | 0.00 | −0.18 | .860 | 0.00 | ||
| 5a | Days btw S3 and S4 | Overall | 0.02 | 1.13 | .260 | 0.20 | 0.00 | 0.52 | .601 | 0.00 |
| 5b | Days btw S3 and S4 | PE | 0.00 | 0.09 | .929 | 0.02 | 0.00 | −1.01 | .313 | 0.00 |
| CPT | 0.04 | 1.94 | .054 | 0.35 | 0.00 | 0.66 | .513 | 0.12 | ||
| Group x Time | 0.04 | 1.43 | .155 | 0.26 | 0.00 | 1.10 | .275 | 0.00 | ||
| 6a | Days btw S4 and S5 | Overall | 0.02 | 2.58 | .011 | 0.49 | 0.00 | −0.18 | .858 | −0.03 |
| 6b | Days btw S4 and S5 | PE | 0.02 | 2.26 | .026 | 0.43 | 0.00 | 1.00 | .322 | 0.00 |
| CPT | 0.02 | 1.96 | .052 | 0.37 | 0.00 | −1.66 | .099 | −0.32 | ||
| Group x Time | 0.00 | −0.28 | .781 | 0.00 | 0.00 | −1.75 | .083 | 0.00 | ||
Note. CPT = cognitive processing therapy; PE = prolonged exposure; SD = standard deviation; M = mean; btw = between; df = degrees of freedom; S2 = session 2; S3 = session 3; S4 = session 4; S5 = session 5. Bold text indicates statistically significant results.
Figure 1.
Symptoms change over time by session attendance. Session attended was analyzed using a continuous percentage of sessions attended variable. Only to depict the nature of this effect, we show the trajectory for participants who fell 1 SD above the mean of percentage of sessions attended (labeled “Low”) and for participants who fell 1 SD above the mean of percentage of sessions attended (labeled “High”). As Table 2 indicates, percentage of sessions attended was negatively associated with PTSD symptom change (i.e., higher percentage attended corresponds to larger decreases in PTSD symptoms), and the effect reversed during the follow-up period (i.e., higher percentage attended corresponded to smaller decreases or slight increases in PTSD symptoms during the follow-up period in comparison to lower percentage attended).
Analysis 2a indicated that the mean number of days between treatment sessions significantly predicted change in PTSD symptoms during treatment, but not during the follow-up period. Participants with shorter average time between sessions showed larger decreases in PTSD symptoms pre- to post-treatment compared to participants with longer average time between sessions when controlling for percent sessions attended3, with no difference in change during the follow-up period as a function of average time between sessions. Analysis 2b indicated that the impact of average time between sessions did not significantly vary as a function of treatment condition. In other words, the more frequently sessions were attended, the better the outcome for both CPT and PE.
Consistency as indexed by the within-subjects standard deviation of days between treatment sessions was related to the change in PTSD in a manner similar to average time between sessions (see Analysis 3a). However, the effect size for average time between sessions (d = .82, indicating a large effect) was substantially larger than the effect size for consistency (d = .48, indicating a medium effect) suggesting that average days between treatment sessions impacts treatment outcome more than consistency. We did not evaluate a model with both of these variables predicting the outcome variable because the mean is used to calculate standard deviation, thus they should not be evaluated simultaneously in a regression analysis. Analysis 3b indicated that the impact of consistency did not significantly vary across treatment conditions.
Analyses 4–6 were exploratory and were conducted to identify the interval between sessions that most impacted treatment outcome. The coefficients in Table 2 indicated that the time between sessions 4 and 5 was the only interval that significantly impacted change in PTSD symptoms, with longer time intervals associated with smaller decreases in PTSD symptom severity during treatment (See Analysis 6a). This effect did not significantly differ across treatment conditions (See Analysis 6b). The intervals between sessions 2 and 3 and between sessions 3 and 4 were not significantly associated with change in PTSD symptoms from pre- to post-treatment or post-treatment through the follow-up period.
Discussion
The current study provides initial evidence that timing of sessions plays an important role in PTSD treatment outcome. More specifically, we found that when controlling for amount of sessions attended, the more frequently sessions are attended (i.e., fewer average days between sessions), the greater symptom improvement over the course of treatment (i.e., in the short-term). These findings speak to the potential utility of more frequent sessions improving outcomes in the context of brief evidence based psychotherapy for PTSD. While consistency of session timing was also examined, the substantially larger effect size for frequency suggests that frequency impacts treatment outcome more than consistency does. Furthermore, the analyses examining the 5-year follow-up data demonstrated that the effects were maintained at follow-up with no significant change in either direction.
Importantly, these results demonstrate that even in the context of a controlled efficacy trial with high rates of treatment fidelity (see Resick et al., 2002), there remain relevant malleable factors that impact treatment outcome, namely the timing of sessions. While our data are not able to speak to the ideal timing of days in between sessions, they do highlight the benefit of attending treatment sessions more frequently to maximize treatment gains. That is, attending sessions more frequently than once per week (average of 5.48 days between sessions, collapsed across treatment condition) appears to significantly increase in the amount of PTSD symptom reduction over the course of treatment. These results are consistent with recent research on PE demonstrating the potential benefit of intensive daily sessions on outcome (Blount, Cigrang, Foa, Ford, & Peterson 2014). Although this paper did not compare results to standard PE, the study demonstrated that PE over a shorter period of time resulted in significant symptom change. The current findings are also consistent with literature that has demonstrated the similar benefits of more intensive protocols compared to standard weekly treatment (e.g., Ehlers et al., 2010; Ehlers et al., 2014) on symptom improvement. Taken together, these finding have important implications for clinical practice, a setting in which treatment sessions generally occur less frequently than efficacy trials. The findings of this study indicate that PTSD treatment outcome effects are likely dampened in clinical practice settings given the general structure of weekly (or less) treatment sessions, and discussing this with patients may increase frequency of session attendance. If outcomes are improved by more frequent sessions, the backlog of clients might be remediated somewhat, although it may seem counter-intuitive to clinicians and agencies initially. Given our data study suggests more frequent sessions improves outcome and those in the study who attended session more often demonstrated significantly greater symptom improvement, we would encourage researchers and clinicians to schedule twice-weekly session for CPT and PE. This is consistent with the respective efficacy trials (e.g., Resick et al., 2002; Foa, Rothbaum, Riggs, & Murdock, 1991).
Although both CPT and PE treatment manuals encourage twice-weekly sessions for 6 weeks, the implications for improved outcome are likely not fully understood and require further examination. The current study did not directly examine treatment occurring once a week versus twice a week. Gaining greater knowledge regarding the difference in efficacy when sessions occur once per week versus twice per week would be important given that these treatments are typically implemented once per week in clinical practice. Although scheduling of sessions is important, it is equally important to acknowledge that even when sessions are scheduled to occur once or twice per week, clients tend to reschedule or cancel treatment sessions, which further impacts frequency of sessions. In these circumstances it is critical to understand why individuals are rescheduling and/or canceling treatment sessions and the frequency with which they do so.
Although some data support the generalizability of efficacious treatments in routine care (e.g., Stirman, 2008; Zappert & Westrup, 2008), the timing with which treatment is delivered in these settings may play a crucial role and deserves greater research attention. Results from the current study suggest that one way to potentially increase treatment response rates outside of these RCTs may be to administer more frequent sessions over a shorter duration of time, to maximize symptom improvement in routine clinical care. This would allow for the examination of the impact of weekly frequency on outcome in routine care, and may also help individuals engage and remain in treatment for the full duration. Receiving the same treatment over a shorter duration (6 versus 12 weeks) may serve as a proxy for decreasing avoidance and providing more support through more frequent therapist interaction. Furthermore, if sessions are scheduled more frequently and a session is canceled due to illness or other practical difficulties, therapy is still occurring on a weekly basis rather than perhaps having a week or two in between sessions.
The exploratory analyses demonstrated the potential benefit on symptom outcome of having fewer days between sessions 4 and 5 for PTSD treatment, regardless of the type of treatment (e.g., CPT or PE). Given that both CPT and PE contain assignments in session 4 that involve require patients to directly confront the content of their trauma (e.g., trauma account is assigned in session 3, and the first imaginal exposure occurs in session 3), we added an exploratory aim to examine the potential impact of session timing between these sessions on treatment outcome. Results revealed that the longer time in between these sessions, after which exposure assignments are first introduced, were related to smaller symptom reduction, regardless of treatment type. While these exploratory results could be spurious, these sessions involve the more in depth discussion of trauma details. Although they do not align with the first introduction of the trauma account across both treatments, it is important to further explore the potential importance of these sessions and to replicate these findings. Notably, these findings counter the common clinical perception that exposure-based techniques are not well tolerated. Furthermore, the data may suggest clinicians should pay attention to session timing around the period after which the trauma accounts are introduced, as increased avoidance may manifest in a delay in attendance at the subsequent sessions and impact symptom reduction.
While these analyses were exploratory, it is interesting to highlight the potential role of timing around potentially more difficult assignments in treatment. Although we were not able to directly measure avoidance, it is possible that the longer time between sessions may be a proxy for avoidance related to confronting the details of the index trauma. Furthermore, the current study is not powered to examine whether session timing is a mechanism of change or a correlate of other variables not directly examined. Future research should examine whether it is a mechanism or simply a correlate.
Several limitations of the current study should be considered. First, this study only included women, which impacts generalizability of the findings. Second, the data are part of a RCT with high rates of treatment fidelity. Although the data are helpful as a first step in understanding the impact of session timing on outcome, these data are not likely representative of routine care. Third, given the relatively low standard deviation in average days between sessions, future research should replicate and extend the current findings to investigate whether or not there is an ideal threshold for session timing. The pattern in the current dataset may not reflect routine care that may have higher averages of days between session due to factors such as clinical availability and cancelations. Additionally, we suggest that session attendance may be a proxy for treatment engagement, however, we do not include a measure of engagement in the current study and are unable to address to this issue more specifically. Finally, it is important to recognize that the current study did not collect data on the reason for the frequency of session scheduling. For example, it is possible that factors such as vacation, illness, or avoidance could have been playing a role in session timing.
The current study has a number of clinical implications. First, it highlights the importance of discussing the impact of frequent session attendance with patients. The current study provides empirical support for the importance of regular session attendance by demonstrating that the more frequently the sessions are attended, the better the expected treatment outcome, above and beyond the number of sessions attended. This is consistent with prior research in depression and naturalistic treatment (e.g., Cuijpers et al., 2013; Erekson et al., in press). Furthermore, carefully monitoring when patients cancel sessions and directly addressing the reason for cancelation may be beneficial. A pattern of frequent canceling and rescheduling should be discussed with the patient to convey the potential impact of frequency of attendance on outcome. Future research should continue to investigate the importance of session timing on treatment outcome.
Acknowledgments
This work was supported by National Institute of Mental Health Grant NIH-1 R01-MH51509 and National Institute of Mental Health Grant NIH-2 R01-MH51509 awarded to Patricia A. Resick while at the University of Missouri–St. Louis. Dr. Gutner was supported by a National Institute of Mental Health grant (1K23MH103396-01A1).
Footnotes
Public Health Significance Statement: This study suggests that more frequent spaced sessions of psychotherapy for PTSD results in greater reductions in symptoms during the course of treatment.
We conducted follow-up analyses including minority status as a covariate. This did not change the pattern of results and had minimal impact on the estimated coefficients.
All main effects (i.e., predictor and time) as well as the covariate percent sessions attended were included in the models. However, to facilitate interpretation only the coefficients for the predictor x time and condition x predictor x time interactions are presented. A table with the coefficients for the intercept terms and main effects can be obtained from the first author.
Because percent sessions attended was included in all analyses, the phrase “when controlling for percent sessions attended” applies throughout; however, to we will no longer add it to increase the readability of the results section.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM- IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Blount TH, Cigrang JA, Foa EB, Ford HL, Peterson AL. Intensive outpatient prolonged exposure for combat-related PTSD: A case study. Cognitive and Behavioral Practice. 2014;21(1):89–96. doi: 10.1016/j.cbpra.2013.05.004. [DOI] [Google Scholar]
- Bryant RA, Moulds ML, Guthrie RM, Dang ST, Mastrodomenico J, Nixon RD, … Creamer M. A randomized controlled trial of exposure therapy and cognitive restructuring for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2008;76:695–703. doi: 10.1037/a0012616. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough K, Miranda R, Chemtob CM. Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse-related Posttraumatic Stress Disorder. Journal of Consulting and Clinical Psychology. 2004;72(3):411–416. doi: 10.1037/0022-006X.72.3.411. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Cuijpers P, Huibers M, Ebert DD, Koole SL, Andersson G. How much psychotherapy is needed to treat depression? A metaregression analysis. Journal of Affective Disorders. 2013;149(1):1–13. doi: 10.1016/j.jad.2013.02.030. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, Albert I, Clark DM. A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry. 2014;171(3):294–304. doi: 10.1176/appi.ajp.2013.13040552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Hackmann A, Grey N, Liness S, Wild J, … McManus F. Intensive cognitive therapy for PTSD: A feasibility study. Behavioural and Cognitive Psychotherapy. 2010;38(04):383–398. doi: 10.1017/S1352465810000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erekson DM, Lambert MJ, Eggett DL. The relationship between session frequency and psychotherapy outcome in a naturalistic setting. Journal of Consulting and Clinical Psychology. 2015;83(6):1097–1107. doi: 10.1037/a0039774. [DOI] [PubMed] [Google Scholar]
- Finley EP, Garcia HA, Ketchum NS, McGeary DD, McGeary CA, Stirman SW, Peterson AL. Utilization of evidence-based psychotherapies in Veterans Affairs posttraumatic stress disorder outpatient clinics. Psychological Services. 2015;12(1):73–82. doi: 10.1037/ser0000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715–723. doi: 10.1037/0022-006X.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. Journal of consulting and clinical psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide (Treatments that work) Oxford University Press; USA: 2007. [Google Scholar]
- Foa EB, Riggs DS, Massie ED, Yarczower M. The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behavior Therapy. 1995;26:487–499. [Google Scholar]
- Foa EB, Yadin E, Lichner TK. Exposure and Response (Ritual) Prevention for Obsessive-Compulsive Disorder. New York: Oxford University Press; 2012. [Google Scholar]
- Foa EB, Hearst DE, Dancu CV, Hembree E, Jaycox LH. Unpublished manuscript. Medical College of Pennsylvania, Eastern Pennsylvania Psychiatric Institute; 1994. Prolonged exposure (PE) manual. [Google Scholar]
- Gallagher MW, Resick PA. Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: Preliminary evidence for the differential effects of hopelessness and habituation. Cognitive Therapy and Research. 2012;36(6):750–755. doi: 10.1007/s10608-011-9423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Blain LM, Mott JM, Elwood L, Houle T. Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. Journal of consulting and clinical psychology. 2012;80(6):968–981. doi: 10.1037/a0030600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutner CA, Gallagher MW, Baker AS, Sloan DM, Resick PA. Time course of treatment dropout in cognitive behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice and Policy. 2016;8:115–121. doi: 10.1037/tra0000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, Simpson TL. Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):394–404. doi: 10.1037/a0031474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iverson KM, Resick PA, Suvak M, Walling S, Taft C. Intimate partner violence exposure predicts PTSD treatment engagement and outcome in Cognitive Processing Therapy. Behavior Therapy. 2011;42:236–248. doi: 10.1016/j.beth.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8:107–114. doi: 10.1037/tra0000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 6: Hierarchical linear and nonlinear modeling [Computer software and manual] Lincolnwood, IL: Scientific Software International; 2005. [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting And Clinical Psychology. 2008;76(2):243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A Comparison of Cognitive-Processing Therapy With Prolonged Exposure and a Waiting Condition for the Treatment of Chronic Posttraumatic Stress Disorder in Female Rape Victims. Journal of Consulting and Clinical Psychology. 2002;70(4):867–879. doi: 10.1037/0022-006X.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM … On behalf of the STRONG STAR Consortium. A Randomized Clinical Trial of Group Cognitive Processing Therapy Compared With Group Present-Centered Therapy for PTSD Among Active Duty Military Personnel. Journal of Consulting and Clinical Psychology. 2015;83:1058–1068. doi: 10.1037/ccp0000016. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke M. Cognitive processing therapy for rape victims: A treatment manual. Vol. 4. Sage; 1993. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037/0022-006X.60.5.748. [DOI] [PubMed] [Google Scholar]
- Rizvi SL, Vogt DS, Resick PA. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy. 2009;47(9):737–743. doi: 10.1016/j.brat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, … Turner C. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA. 2007;297(8):820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willet JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Spoont MR, Murdoch M, Hodges J, Nugent S. Treatment receipt by veterans after a PTSD diagnosis in PTSD, mental health, or general medical clinics. Psychiatric Services. 2010;61(1):58–63. doi: 10.1176/appi.ps.61.1.58. [DOI] [PubMed] [Google Scholar]
- Stirman SW. The applicability of randomized controlled trials of psychosocial treatments for PTSD to a veteran population. Journal of Psychiatric Practice. 2008;14(4):199–208. doi: 10.1097/01.pra.0000327309.58411.e0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Minnen A, Arntz A, Keijsers GJ. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy. 2002;40(4):439–457. doi: 10.1016/S0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JT. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression & Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Zappert LN, Westrup D. Cognitive processing therapy for posttraumatic stress disorder in a residential treatment setting. Psychotherapy: Theory, Research, Practice, Training. 2008;45(3):361–376. doi: 10.1037/0033-3204.45.3.361. [DOI] [PubMed] [Google Scholar]