Abstract
Introduction
Surgical retained items (RSIs) are associated with increase in perioperative morbidity and mortality. We used a large national database to investigate the incidence, trends and possible predictors for RSIs after major abdominal and pelvic procedures.
Methods
The nationwide inpatient sample data were queried to identify patients who underwent major abdominal and pelvic procedures and discharged with secondary ICD-9-CM diagnosis code of (998.44 and 998.7). McNemar's tests and conditional logistic regression analyses of a 1:1 matched sample were conducted to explore possible predictive factors for RSI.
Results
RSI incidence rate was 13 in 100,000 cases-years from 2007 to 2011 after major abdominal and pelvic procedures. RSI incidence remained steady over the five-year study period. Rural hospitals and elective procedures were associated with a higher RSI incidence rate [(OR 1.391, 95% CL 1.056–1.832), p = 0.019] and [(OR 1.775, 95%CL 1.501–2.098), p < 0.001] respectively.
Conclusions
Our study was able to add more to the epidemiological perspective and the risk profile of retained surgical items in abdominal and pelvic surgery. Surgical cases associated with these factors may need further testing to rule out RSI.
Keywords: Never event, Retained surgical item, Sentinel event, Unretrieved surgical device
Highlights
-
•
Overall incidence for surgical retained items after abdominal and pelvic surgeries is around 13 in 100,000 cases with a steady trend from 2007 to 2011.
-
•
Major elective abdominal and pelvic procedures in rural hospitals are associated with higher rate of surgical retained items.
-
•
Obesity and teaching hospitals are probably associated with higher rate of surgical retained items.
1. Introduction
A retained surgical item (RSI) is any item that is unintentionally left behind in a patient's body in the operative or procedural setting. According to the National Quality Forum (NQF), roughly 2000–4000 RSI cases occur each year in the United States [1]. RSI events are associated with increase in morbidity and mortality and have huge reputational and financial consequences. In fact, it is estimated that the average cost to remove an RSI is $63,631 per hospital stay which does not even approach the potential cost required to settle a malpractice claim and has the potential to reach millions of dollars in settlement agreements [2]. Researchers continue to seek new ways of thinking about human error and operative practices in order to further prevent the occurrence of such sentinel events which really are considered never events. Unlike most studies on this subject, our study serves to incorporate and amalgamate a large surgical population from a national database in order to identify certain characteristics and variables that seem to be linked to the occurrence of RSI events in major abdominal and pelvic surgery. Our goal in this cross-sectional study was to a) asses the trend in the rates of RSI incidents over the study period based on a large, national sample, and b) identify previously under-appreciated patient, procedure, and hospital characteristics that are associated with RSI events.
2. Methods
2.1. Data sources and samples
The data for our study was obtained from the Nationwide Inpatient Sample (NIS) of the Healthcare Cost Utilization Project (HCUP) of the Agency for Healthcare Quality and Research (AHRQ) from 2007 to 2011 [3]. The NIS is a stratified probability sample representing 20% of the United States community non-rehabilitation hospitals. Hospitals were stratified in different groups based on their geographical locations (Northeast, Midwest, South and West regions), and then a sample of hospital discharges were drawn randomly from each group. The NIS hospital sampling and stratification is explained in detail at http://www.hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2012.pdf (last accessed Augustt 11, 2015). Once a hospital was selected, all the discharge data for that year were included in the survey. Approximately 8 million hospital discharges from about 1000 hospitals are available in the database each year. The NIS data contain patient demographics such as age, gender, and race. The dataset also includes primary and secondary diagnoses and procedures (recorded as International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes), hospital characteristics, severity and comorbidity measures, expected payment source, and length of hospital stay. The NIS methodology and information about this database can be accessed at http://www.hcup-us.ahrq.gov/nisoverview.jsp. The NIS consists of publically available, de-identified data, and so the study was considered to be exempt from review by our institutional review board (IRB decision on 03/25/2016).
2.2. Patient selection
For our analysis, we included adult inpatients who had at least one major operating room (OR) abdominal or pelvic procedure (open or laparoscopic) during their hospital stay and were discharged with a primary ICD-9-CM diagnosis code of a major OR abdominal and pelvic surgery and a secondary diagnosis code of 998.4 (foreign body accidently left during a procedure) or a diagnosis code of 998.7 (acute reaction to foreign substance accidently left during a procedure) according to the last update (March 2015) of the AHRQ Patient Safety Indicator 05(PSI 05) technical specifications for retained surgical item or unretrieved device fragment count [4]. The time frame for our study was from 2007 to 2011. Furthermore, we only included abdominal and pelvic surgeries as this focused the similarity in the surgical techniques involved as well as the operating room environment for these procedures, which in turn may lead to better conclusions; the morbidity associated with device retrieval is similar and in most instances involves an additional surgery or interventional procedure.
2.3. Matching of cases and controls
Major abdominal and pelvic procedures with RSIs (cases) were matched with a group of patients of major abdominal and pelvic procedures without RSIs (controls) based on calculated propensity scores. The propensity score is the probability for a patient included in our study to have an RSI. We utilized a multiple logistic regression model to calculate this score after controlling for patient demographics (age, gender and race/ethnicity), health insurance (Medicare, Medicaid, Private insurance and other), year of admission (2007, 2008, 2009, 2010 and 2011), and severity of illness [we used a functional score included in the HCUP databases called All Patient Refined DRG: Severity of Illness Subclass (APRDRG-Severity), 1 = Minor loss of function, includes cases with no comorbidity or complications, 2 = Moderate loss of function, 3 = Major loss of function and 4 = Extreme loss of function]. We choose those variables for matching because from our medical literature review and from clinical experience we thought they are the least to be predictors or risk factors for RSI occurrence from the variables available in the NIS dataset (see Table 2).
Table 2.
Comparison cases and controls in the propensity-matched sample of major abdominal and pelvic procedures. aSeverity of illness as defined in this database: All Patient Refined DRG-Severity of Illness Subclass (APRDRG-Severity), 1 = Minor loss of function, includes cases with no comorbidity or complications, 2 = Moderate loss of function, 3 = Major loss of function and 4 = Extreme loss of function]. Frequency and percentage are used for discrete variables. Mean and standard deviation are used for continuous variables.
| Characteristics | Propensity-matched data set (Abdominal and pelvic major procedures) |
|||
|---|---|---|---|---|
| Cases (n = 1144) | Controls (n = 1144) | p value | ||
| Age, mean (SD), year | 52.62(18.54) | 53.08(18.95) | 0.552 | |
| Female gender | 763(66.70) | 801(70.02) | 0.096 | |
| Race/ethnicity | White | 628(54.86) | 605(52.88) | 0.707 |
| Black | 130(11.36) | 121(10.58) | ||
| Hispanic | 115(10.05) | 142(12.41) | ||
| Other/unknown | 272(23.73) | 276(22.13) | ||
| Severity of illnessa | 1 | 287(25.09) | 287(25.09) | 0.982 |
| 2 | 423(36.98) | 375(32.78) | ||
| 3 | 277(24.21) | 324(28.32) | ||
| 4 | 157(13.72) | 158(13.81) | ||
| Obesity | Yes | 120(10.49) | 131(11.45) | 0.504 |
| No | 1024(89.51) | 1013(88.55) | ||
| Morbid obesity | Yes | 73(6.38) | 59(5.16) | 0.244 |
| No | 1071(93.62) | 1085(94.84) | ||
| Procedure urgency | Elective | 582(51.05) | 422(37.02) | <0.001 |
| Non-elective | 558(48.95) | 718(62.98) | ||
| Teaching hospital | Yes | 600(52.86) | 577(50.93) | 0.378 |
| No | 535(47.14) | 556(49.07) | ||
| Hospital location | Rural | 136(11.98) | 101(8.91) | 0.019 |
| Urban | 999(88.02) | 1032(91.09) | ||
| Hospital RN percentage, mean (SD) | 93.29(6.23) | 93.77(6.75) | 0.089 | |
| Hospital ownership | Public | 138(15.32) | 118(13.11) | 0.439 |
| Private (none-for-profit) | 651(72.25) | 664(73.78) | ||
| Private | 112(12.43) | 118(13.11) | ||
| Hospital bedsize | Small | 120(10.57) | 120(10.59) | 0.495 |
| Medium | 278(24.49) | 256(22.59) | ||
| Large | 737(64.93) | 757(66.81) | ||
| Health insurance | Medicare | 369(32.26) | 384(33.71) | 0.541 |
| Medicaid | 177(15.47) | 159(13.96) | ||
| Private | 498(43.53) | 490(43.02) | ||
| Other/unknown | 100(8.74) | 111(9.31) | ||
| Year of admission | 2007 | 234(20.45) | 233(20.37) | 0.999 |
| 2008 | 243(21.24) | 195(17.05) | ||
| 2009 | 209(18.27) | 295(25.79) | ||
| 2010 | 221(19.32) | 183(16.00) | ||
| 2011 | 237(20.72) | 238(20.80) | ||
2.4. Statistical analysis
All analyses were conducted using SAS software version 9.3 (SAS Inc., Cary, NC). Categorical variables were summarized as frequencies and percentages while continuous variables were summarized as means and standard deviations. Trend in RSI incidence rates in the unmatched abdominal and pelvic surgery sample across the five years study period was assessed by the Cochran-Armitage trend test. Chi-square tests were used to examine the association of RSI incidence with different categorical variables in the unmatched sample. A 1:1 propensity-matched sampling of patients who had RSI with those who did not have RSI was done using a greedy 8 to 1 digit-matching algorithm technique [5]. McNemar's tests were used to describe baseline characteristics of patients in the matched sample for dichotomous variables and assess the differences in the incidence of RSIs between the matched groups. Conditional logistic analyses were utilized to assess other non-dichotomous variables in the matched sample. Wilcoxon signed-rank test is used to compare skewed continuous variables in the matched sample. All tests were two-tailed and a p-value of 0.05 was considered statistically significant.
3. Results
3.1. RSI incidence rate
There were 1144 patients, who met our study inclusion and exclusion criteria, out of 8,677,863 cases (major OR abdominal and pelvis surgeries). The RSI incidence rate was calculated as 13 in 100,000 procedures-years.
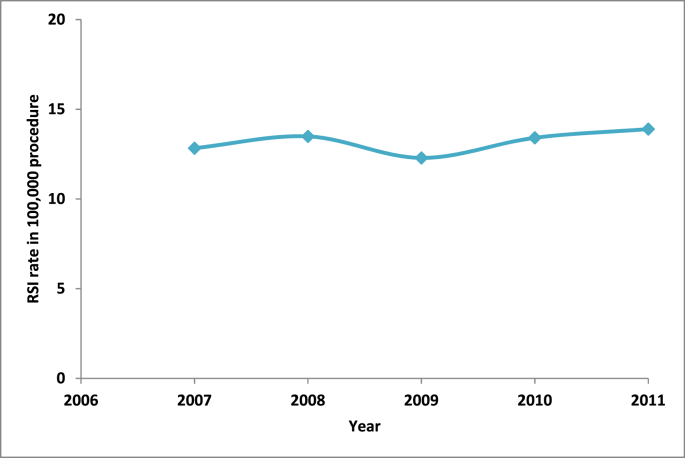
3.2. Unmatched analyses: steady trend in RSI rates
The Cochran-Armitage trend test revealed that the yearly incidence rate of RSI after abdominal and pelvic surgery remained steady over the five-year study period without significant change (p = 0.462) (Fig. 1). RSI incidence rates from the unmatched sample are presented in Table 1. Hospital location (urban vs. rural), hospital bedsize and hospital control and ownership was found to have no effect on the RSI rates in this unmatched sample while elective procedures, morbid obesity and teaching hospitals were found to be associated with significantly higher RSI rates (Table 1).
Fig. 1.
Trend of the retained surgical items rates in major operating room abdominal and pelvic procedures (from 2007 to 2011).
Table 1.
Retained surgical items incidence in various situations. RSI = Retained surgical item.
| Characteristics | Unmatched dataset (Abdominal and pelvic procedures) |
||
|---|---|---|---|
| No of RSI cases in 100,000 procedures | p value | ||
| Procedure urgency | Elective | 16 | <0.001 |
| Non-elective | 11 | ||
| Hospital location | Urban | 13 | 0.214 |
| Rural | 15 | ||
| Teaching hospital | Yes | 15 | <0.001 |
| No | 12 | ||
| Hospital bedsize | Small | 13 | 0.611 |
| Medium | 13 | ||
| Large | 12 | ||
| Hospital ownership | Public | 15 | 0.184 |
| Private (none-for-profit) | 13 | ||
| Private | 13 | ||
| Morbid obesity | Yes | 23 | <0.001 |
| No | 13 | ||
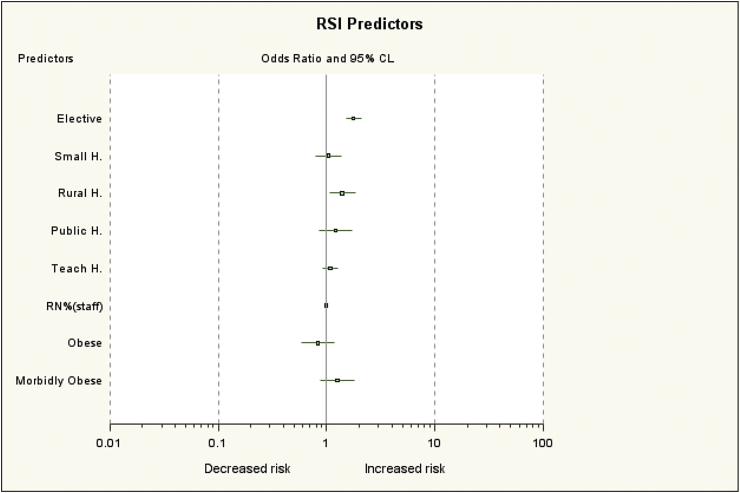
3.3. Matched analyses: hospital location, size and ownership influence RSI rates
After matching some of these differences dissipated in the propensity-matched sample (Fig. 2). In particular, the association between the likelihood of RSI incident and morbid obesity [(OR 1.254, 95%CL 0.880–1.785), p = 0.244] and teaching hospitals [(OR 1.081, 95%CL 0.917–1.274), p = 0.378] becames non-significant (Fig. 2). However, rural hospitals, compared to urban hospitals, were associated with a higher RSI incidence rate [(OR 1.391, 95% CL 1.056–1.832), p = 0.019]. Additionally, elective procedures were still associated with higher incidence of RSI in the propensity matched sample [(OR 1.775, 95%CL 1.501–2.098), p < 0.001]. Hospital bedsize had no effect on the incidence of RSI in the propensity matched sample. The odds ratio for RSI in small hospitals compared to large hospitals was [(OR 1.037, 95% CL 0.792–1.359), p = 0.848] and that for medium size hospitals was [(OR 1.135, 95% CL 0.920–1.399), p = 0.355]. Similarly, hospital ownership and control had no significant association with the RSI incidence. Compared to for-profit private hospitals, public hospitals had an OR of 1.216 [(OR 1.216, 95%CL 0.852–1.736), p = 0.203] while that for the not-for-profit private hospital was 1.032 [(OR 1.032, 95%CL 0.775–1.374), p = 0.538]. Furthermore, the percentage of registered nurses (RN) (compared to other nursing staff) in the hospital had no effects on the RSI rate when it was evaluated in the matched sample [(OR 0.988, 95%CL 0.974–1.002), p = 0.090].
Fig. 2.
Retained surgical items occurrence relationship to various factors, RN%(staff) = the percentage of registered nurses in the hospital of the total hospital nursing staff.
4. Discussion
RSIs are rare events and are considered never events by many healthcare entities. The incidence rate we gleaned was 13 for every 100,000 cases performed in patients who had undergone with at least one major OR abdominal or pelvic surgery; depending on your size of hospital, RSIs could be a reality for many hospitals. Our study revealed that morbid obesity to some degree, major OR procedures, abdominal and pelvic procedures, elective procedures and rural hospitals to be associated with an increased risk for RSIs. Furthermore, teaching hospitals were associated with higher rate of RSI cases before matching; however, we were not able to demonstrate that in the propensity-matched sample. It is not surprising that morbid obesity, abdominal and pelvic procedures and major OR procedures were found to be associated with increased RSI incidence considering the complexity of the surgery involved. The same could be said for presence of trainee in the operating room, although ironic enough it was mentioned as a positive influence on RSI risk by Stawicki and colleagues [6]. Many small studies have identified incorrect sponge counts, morbid obesity, major surgery, emergent cases and length of case as few of many identifiable risk factors for RSI [7], [8], [9]. While the aforementioned risk factors only represent the vast number identified in previous studies, we know now that incidence of RSI may appear to be patient specific and surgery specific [9], [10], [11], although some studies have suggested quite the opposite [12]. We appreciate that our study used a large national sample which has several limitations derived from the use of an administrative dataset obtained retrospectively from patients discharge information, including errors in coding and inability to incorporate relevant data other than what is provided in the dataset. Furthermore, this database has no follow-up information of patients diagnosed with RSI to investigate complications caused by RSI including mortality. Other weaknesses more specific to this study include lack of information regarding the type of the RSI and information in relation to other RSI potential risk factors such as instruments count and blood loss. The very fact that these datasets exist and have the potential to provide important insight into process improvement furthers our assertion that surgeons and physicians must embrace accurate documentation and validate coding. The power of these datasets must be leveraged if we are ever to prevent what many consider “never events” in our era of patient-centric care.
5. Conclusions
Our study was able to add to the risk profile of retained surgical items in abdominal and pelvic surgeries. Surgical cases associated with these factors may need further testing to rule out RSI such as x-rays or ultrasound imaging.
Ethical approval
The dataset used in our study consists of publically available, de-identified data, and so the study was considered to be exempt from review by the University of Texas Southwestern Medical Center, Dallas, Texas Institutional Review Board (UTSW-IRB decision on 03/25/2016).
Sources of funding
Ahmad Elsharydah: departmental support.
Kimberly O. Warmack: departmental support.
Abu Minhajuddin: departmental support.
Susan D. Moffatt-Bruce is supported by the Institute for the Design of Environments Aligned for Patient Safety (IDEA4PS) at The Ohio State University which is sponsored by the Agency for Healthcare Research & Quality (P30HS024379).
Author contribution
Ahmad Elsharydah contributed to:
-
-
the study concept and design, acquisition of data (database), and analysis and interpretation of data.
-
-
drafting/revising the manuscript for important intellectual content.
-
-
approval of the final version to be published.
Kimberly Warmack contributed to:
-
-
analysis and interpretation of data.
-
-
drafting/revising the manuscript for important intellectual content.
-
-
approval of the final version to be published.
Abu Minhajuddin contributed to:
-
-
the study design and analysis and interpretation of data.
-
-
drafting/revising the manuscript for important intellectual content.
-
-
approval of the final version to be published.
Susan D. Moffatt-Bruce contributed to:
-
-
analysis and interpretation of data.
-
-
drafting/revising the manuscript for important intellectual content.
-
-
approval of the final version to be published.
Conflicts of interest
None.
Trial registry number
N/A.
Guarantor
Ahmad Elsharydah.
Potential reviewers
1. Robert R. Cima, M.D. Email: Cima.Robert@Mayo.edu.
2. Amy E. Lincourt, PhD. Senior Email: amy.lincourt@carolinas.org.
References
- 1.Gibbs V. NoThing Left Behind: a national surgical patient-safety project to prevent retained surgical items. New policies, practices and posters. Retained surgical items [online]. [cited 2012 Jun 12]. http://www.nothingleftbehind.org. Accessed April 8, 2016.
- 2.CMS. Fact sheet: Details for: CMS proposes additions to list of hospital-acquired conditions for fiscal year 2009 https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2008-Fact-sheets-items/2008-04-14.html. Accessed April 8, 2016.
- 3.HCUP Nationwide Inpatient Sample (NIS) Agency for Healthcare Research and Quality; Rockville, MD: 2007-2011. Healthcare Cost and Utilization Project (HCUP)www.hcup-us.ahrq.gov/nisoverview.jsp Accessed April 8, 2016. [Google Scholar]
- 4.http://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/V50/TechSpecs/PSI_05_Retained_Surgical_Item_or_Unretrieved_Device_Fragment_Count.pdf. Accessed April 9, 2016.
- 5.Parsons L.S. Proceedings of the Twenty-sixth Annual SAS Users Group International Conference. SAS Institute Inc.; Cary, NC: 2001. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. [Google Scholar]
- 6.Stawicki S.P., Moffat-Bruce S.D., Ahmed H.M. Retained surgical items: a problem yet to be solver. J. Am. Coll. Surg. 2013;216(1):15–22. doi: 10.1016/j.jamcollsurg.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 7.Judson T.J., Howell M.D., Guglielmi C. Miscount incidents: a novel to exploring risk factors for unintentionally retained surgical items. Jt. Comm. J. Qual. Patient Saf. 2013;39(10):468–474. doi: 10.1016/s1553-7250(13)39060-6. [DOI] [PubMed] [Google Scholar]
- 8.Moffat-Bruce S.D., Cook C.H., Steinberg S.M. Risk factors for retained surgical items: a meta-analysis and proposed risk stratification system. J. Surg. Res. 2014;190(2):429–436. doi: 10.1016/j.jss.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 9.Egorova N.N., Moskowitz A., Gelijins A. Managing the prevention of retained surgical instruments: what is the value of counting? Ann. Surg. 2008;247(1):13–18. doi: 10.1097/SLA.0b013e3180f633be. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser C.W., Friedman S., Spruling K.P. The retained surgical sponge. Ann. Surg. 1996;224(1):79–84. doi: 10.1097/00000658-199607000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gawande A.A., Studder D.M., Orav E.J. Risk factors for retained instruments and sponges after surgery. N. Engl. J. Med. 2003;348(3):229–235. doi: 10.1056/NEJMsa021721. [DOI] [PubMed] [Google Scholar]
- 12.Lincourt A.E., Harrell A., Cristiana J. Retained foreign bodies after surgery. J. Surg. Res. 2007;138(2):170–174. doi: 10.1016/j.jss.2006.08.001. [DOI] [PubMed] [Google Scholar]