Abstract
Background
Pathophysiology of attention-deficit hyperactivity disorder (ADHD) is not known, and therefore the present study investigated mitochondrial defects, if any in cybrids created from patients and control population.
Methods
To investigate mitochondrial pathology in ADHD, cybrids cell lines were created from ADHD probands and controls by fusing their platelets with ρ0-cells prepared from SH-SY5Y neuroblastoma cell line. Cellular respiration, oxidative stress, mitochondrial membrane potential and morphology were evaluated employing oxygraph, mitochondria-specific fluorescence staining and evaluation by FACS, and immunocytochemistry. HPLC-electrochemical detection, quantitative RT-PCR and Blue Native PAGE were employed respectively for assays of serotonin, mitochondrial ATPase 6/8 subunits levels and complex V activity.
Results
Significantly low cellular and mitochondrial respiration, ATPase6/8 transcripts levels, mitochondrial complex V activity and loss of mitochondrial membrane potential and elevated oxidative stress were observed in ADHD cybrids. Expression of monoamine oxidizing mitochondrial enzymes, MAO-A and MAO-B levels remained unaffected. Two-fold increase in serotonin level was noted in differentiated cybrid-neurons.
Conclusions
Since cybrids are shown to replicate mitochondrial defects seen in post-mortem brains, these observed defects in ADHD cybrids strongly suggest mitochondrial pathology in this disorder.
General significance
Mitochondrial defects are detected in ADHD cybrids created from patients' platelets, implying bioenergetics crisis in the mitochondria could be a contributory factor for ADHD pathology and/or phenotypes.
Keywords: Cybrids, Mitochondrial membrane potential, ATPase, Respiration, Serotonin, Mitochondrial pathology
1. Introduction
Inattention, impulsiveness and hyperactivity depict phenotypes of attention-deficit hyperactivity disorder (ADHD), a heritable and heterogeneous childhood disorder with a prevalence of 6-7% in children and adolescents [1]. Mitochondrial dysfunction is a suggested vulnerability factor in the pathogenesis of various neuropsychiatric disorders [2], [3], [4], [5]. Bioenergetic crisis during brain development, mitochondrial DNA (mtDNA) mutation or deletion may cause neurodevelopmental disorders. Autism spectrum disorder probands with mitochondrial defects exhibit symptoms of ADHD [6], [7], [8], suggesting possibility of bioenergetics defects in ADHD too [9]. Other than a report on significant stimulant effect of the ADHD drug, methylphenidate on neuronal firing and mitochondrial transport chain (ETC) enzyme activities in rats [10], no report is available on direct involvement of mitochondrial defects in ADHD. We investigated involvement, if any of mitochondrial bioenergetics in the pathophysiology of ADHD, by creating control and ADHD cybrids from an Indian population.
Cybrids, the mitochondrial transgenic cells created by fusion of mitochondria-less neuronal ρ0-cell lines with blood platelets from patients, mimic pathological conditions of disease phenotypes of post-mortem brains as shown for Parkinson’s disease [11] and other diseases [12]. We created cybrids using blood platelets from ADHD probands and ethnically-matched controls, and investigated their mitochondrial status and functions. One-time creation of cybrids has advantage over repeated blood sampling from young volunteers, since cybrids could be cryopreserved, differentiated into neurons and used continually for investigations.
2. Materials and Methods
2.1. Materials
The human neuroblastoma cell line SH-SY5Y was obtained from National Centre for Cell Sciences, Pune, India. Low glucose Dulbecco’s modified Eagle’s medium, minimal essential medium modified for suspension culture (S-MEM), fetal bovine serum, Gentamicin, tetramethylrhodamine, methyl ester (TMRM), were procured from GIBCO, Invitrogen Corporation (CA, USA). Lymphocyte separation medium (LSM), polyethylene glycol 1000, manitol, were purchased from MP Biomedicals (France). PicoGreen®, MitoSOX™ were purchased from Molecular probes (OR, USA). Potassium chloride, KH2PO4, NaCl and Na2HPO4.2H2O, magnesium sulfate, lead nitrate, sucrose, were procured from Sisco Research laboratories (India). Amphotericin B, pyruvate, uridine, ethidium bromide, TRI reagent, 6-aminocaproic acid, Bis-Tris HCl, N-Dodecyl β-D-Maltoside, bis acrylamide, ATP, EGTA were purchased from Sigma (MO, USA). Coomassie Brilliant Blue G-250 and R-250 dyes were purchased from BioRad (CA, USA) and acrylamide was purchased from Merck (Darmstadt, Germany).
2.2. Methods
2.2.1. Cybrid preparation
ADHD probands (two aged 13; one aged 10 years) and ethnically-matched controls (a 5 years-old female, three males- 5 years, 6 years 8 months and 9 years old respectively) were recruited by mental health professionals of Manovikas Kendra following psychological evaluations through Conners’ Parents and Teachers Rating Scale [13] and Wechsler’s Intelligence Scale for Children [14] for assessing inattention/hyperactivity and Intelligence Quotient (IQ) levels, respectively. Patients with other neuropsychiatric disorders, pervasive developmental disorders, mental retardation (IQ > 70) including Fragile-X syndrome were excluded. Informed written consent for participation was obtained from the parents. Institutional Human ethics committee approved the study protocol.
2.2.2. Confirmation of mtDNA transfer
ρ0-Cells prepared from SH-SY5Y cell line were fused with platelets isolated from 3 ADHD male probands and two healthy controls to produce cybrids [15]. Genomic-DNA isolated from SH-SY5Y, ρ0-cells and cybrids created were subjected to long template PCR using internal primers that amplify a 5.8 kb fragment present in both nuclear and mitochondrial genomes and the amplicon was nested with external primers to amplify a 5.9 kb mtDNA-sequence [16]. PicoGreen® and Mitotracker Green® (Invitrogen Corporation, CA) staining were used for examining absence and presence of mtDNA in these cells and to locate mitochondria in live cells, respectively. Images of cells stained with PicoGreen® or Mitotracker Green® were captured using confocal microscope.
2.2.3. Mitochondrial membrane potential and oxidative stress
Mitochondrial membrane potential was evaluated by staining cells with tetramethylrhodamine, methyl ester (TMRM). Equal number (1 × 106 for fluorimetry and 2 × 105 for flowcytometry) of cells were plated in 6 well plates for TMRM staining. Next day cells were trypsinized and the pellet was resuspended in fresh medium containing 50 nM TMRM, incubated at 37 °C for 30 min in the dark in a CO2 incubator. The medium containing the stain was then removed and the cells were washed twice with D-PBS. Red fluorescence was measured using a spectrofluorimeter (PerkinElmer, USA). The excitation and emission wavelengths for TMRM staining were 530 nm and 570 nm respectively. Membrane potential was also measured with the same dye by using flowcytometry in cybrids. Cells were processed in the same way and the population of TMRM stained cells was analysed by flowcytometry (BD LSRFortessa fluorescence activated cell sorting (FACS), Software-FACS Diva 6.2.).
Cells were stained with MitoSOX™ to assess mitochondrial superoxide generation in these cybrids. Cybrids were collected by trypsinization and stained with 2.5 μM of MitoSOX™ for 30 min at 37 °C in the dark in a CO2 incubator. The stain containing medium was then removed and the cells were washed twice with D-PBS. Red fluorescence was measured using a spectrofluorimeter (PerkinElmer, USA, excitation: 510 nm, emission: 580 nm). MitoSOX™ stained cells were also analysed by flowcytometry (BD LSRFortessa fluorescence activated cell sorting (FACS), Software-FACS Diva 6.2.) [19].
2.2.4. Respiration
Whole cell respiration and digitonin permeabilized cells’ mitochondrial respiration were measured in cybrids using Oxygraph respirometer (Hansatech Instruments Ltd, England). Cells were trypsinized and added to the counter chamber of the Oxygraph respirometer containing D-PBS and the rate of oxygen consumption was measured for 8 min. For mitochondrial respiration the cells were permeabilized with digitonin (0.01%), in mitochondria isolation buffer (MIB, 225 mM Manitol, 75 mM Sucrose, 5 mM MOPs, 1 mM EGTA, dissolved in water, pH 7.4). The cells were washed two times to remove traces of digitonin and oxygen consumption was measured for 10 min. The representation of the amount of oxygen consumed was given as nmol of oxygen/min/number of cells use. [17].
2.2.5. Transcriptome analysis of ATP6/8 subunits
For real time PCR, RNA was isolated using TRI reagent according to the manufacturer’s protocol. Five μg of the total RNA was reverse transcribed using MuLV reverse transcriptase (conditions: 70 °C for 5 min, 37 °C for 5 min, then 42 °C for 60 min, and 70 °C 10 min, final hold at 4 °C). Relative quantification was performed using real-time PCR (Thermal Cycler Dice Real Time System TP800, Takara, Japan) with 100 ng of cDNA and SYBR Premix. The thermal cycling involved initial denaturation of 95 °C for 5 min followed by 40 cycles of 95 °C for 20 s, 58 °C for 30 s, 72 °C for 20 s. 18sRNA was used as endogenous control. The primers were designed using Primer 3 software (ATPase 6 - Forward 5'-GCCCTAGCCCACTTCTTACC-3', Reverse 5'-TTAAGGCGACAGCGATTTCT-3'; ATPase 8 - Forward 5'-CACCTACCTCCCTCACCAAA-3’, Reverse 5'-CTAGGATTGTGGGGGCAAT-3', 18srRNA – Forward 5’-CATGGCCGTTCTTAGTTGGT-3’, Reverse 5’ CGGACATCTAAGGGCATCAC-3’), data were analyzed using the 2-∆∆CT method [18].
2.2.6. Complex V activity
For Blue Native - Polyacrylamide gel electrophoresis (BN-PAGE), mitochondria (P2 fraction) were isolated in mitochondria isolation buffer (MIB, 225 mM Manitol, 75 mM Sucrose, 5 mM MOPs, 1mM EGTA, dissolved in water, pH 7.4), after quantification stored in -800C. Next day pellet was dissolved in sample buffer (1 M 6-aminocaproic acid and 50 mM Bis-Tris HCl, dissolved in water, pH 7.0), along with freshly prepared 10% (w/v) N-Dodecyl β-D-Maltoside, kept on ice for 10 min to dissolve the membrane proteins in the solution. Centrifuge the samples at 20,000xg for 30 min at 40C. Collect the supernatant and add the gel loading buffer (5% w/v Coomassie Brilliant Blue G-250 dissolved in 1 M 6-aminocaproic acid).
Gradient gel (5-13%) was prepared by using 30% acrylamide solution (by dissolving 29.22 g of acrylamide, 0.78 g of bis acrylamide in 100 ml of distilled water) in gel buffer (150 mM Bis-Tris, 1.5 mM aminocaproic acid, pH 7.0). The sample protein (60 μg) was run at, 100 V for 4 hrs at 4 0C on this gradient gel using 1X Cathode Buffer (10X Cathode Buffer- 50 mM Tricine, 15 mM bis-Tris HCl, pH 7.0, 0.02% Coomassie G-250) and 1X Anode buffer (10X Anode buffer- 500 mM Bis-Tris HCl, pH 7.0). Two gels were run using same protein, once run was complete one gel was kept for coomassie staining (for protein quantification, 0.25 % coomassie brilliant blue R250 in 40% methanol, 7% acetic acid) for one hour and distained overnight in 10% acetic acid and 10% methanol. Another gel was kept for complex V reaction buffer (35 mM tris, 270 mM glycine, 14 mM magnesium sulfate, 0.2 % lead nitrate, 8 mM ATP, pH 7.8) for overnight at room temperature. Next day gels were photographed, reaction gels shows white bands [19].
2.2.7. Serotonin analysis
For HPLC analysis 5 × 105 cells were plated and differentiated for six days. On the seventh day, the medium was replaced with fresh medium. After 16 h the cells were washed, sonicated in 50 μl of ice-cold 0.4 M perchloric acid, centrifuged at 12,500 rpm for 5 min and 10 μl of the supernatant was injected into the HPLC-ECD system. A standard solution containing 4 pmol of all the biogenic amines (Norepinephrine, DOPAC, Dopamine, 5-HIAA, HVA and 5-HT) were assayed prior to and at the end of the sample injections to confirm the retention time of the analytes in the column. The flow rate was 0.7 ml/min and the electrochemical detection was performed at 0.74 V. The sensitivity of the HPLC-ECD was set at 20 nA [21].
Cybrids cultured on poly-L-lysine coated cover-slips at 105 cells/ml/35 mm dish were immunostained for monoamine oxidase-A (MAO-A) and MAO-B proteins, images were captured employing confocal microscope, and fluorescence Intensity was measured using Image J software (NIH, USA) (Data are not shown)
3. Results
3.1.1. Inheritance of mitochondria
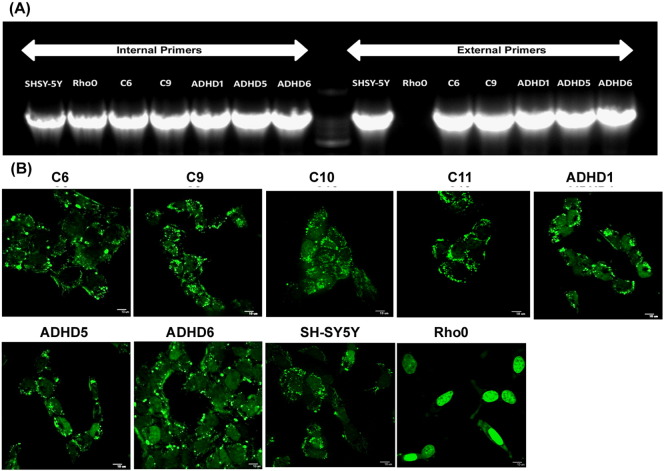
The inheritance of mitochondria was tested in ADHD samples employing long-template PCR method. The primer sets were designed for PCR so that the internal primers amplified a 5.8 kb sequence present in both the nuclear (chromosome 1) and mitochondrial genomes and its amplicon was nested in that of the external primers, which amplified a 5.9 kb mtDNA-specific sequence (Fig. 1A). In case of SH-SY5Y, control and ADHD cybrids PCR product of external and internal primers is obtained, while in ρ0 cells lacking mitochondria, only nuclear sequence amplified by internal primers was observed. PicoGreen dye binds to minor groove of double stranded DNA and gives green fluorescence, so we can see the punctate mitochondria in the cytoplasm of SH-SY5Y cells. The punctate fluorescence is absent in ρ0 cells, but show only nuclear fluorescence because they do not contain mtDNA (Fig. 1B). The punctates observed in control, ADHD cybrids confirm their inheritance of mitochondria from platelets of healthy individuals and patients.
Fig. 1.
Long-template PCR analysis and PicoGreen®staining of cybrids, ρ0-cells and SH-SY5Y cells: (A) Genomic DNA from SH-SY5Y, ρ0-cells, control and ADHD cybrids were amplified using both internal and external primers and subjected to electrophoresis on 0.6% agarose gel. Amplicons are absent in the PCR using external primers for ρ0 cells. (B) Punctated cytoplasm and nuclei are fluorescent in SH-SY5Y cells, control and ADHD cybrids, whereas in ρ0 cells only the nuclei exhibited green fluorescence by Pico-green staining. C6, C9, C10 and C11 are control cybrids, ADHD1, 5 and 6 are cybrids prepared using platelets of ADHD probands. Scale bar represents 10 μm.
3.1.2. ADHD cybrids show reduced mitochondrial mass and membrane potential
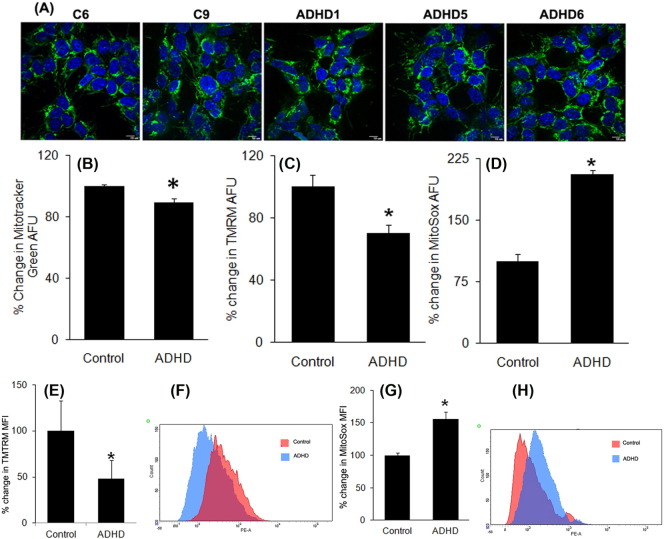
Mitotracker Green enters mitochondrial matrix where it covalently reacts with free thiol groups of cysteine residues of mitochondrial proteins and produce green fluorescence which allows visualization of the mitochondria. SH-SY5Y cells are showing elongated mitochondria and ρ0 cells have fragmented mitochondria (Fig. 2A). Bar diagrams represents the fluorescence intensity in the control and ADHD cybrids measured using Image J software which shows significant reduction in ADHD cybrids compared to controls (Fig. 2B). Mitochondrial membrane potential was examined in cybrid neurons with TMRM staining followed by spectrofluorimetric (Fig. 2C) quantification as well as flow cytometric (Fig. 2E and F) procedure. Significantly low TMRM fluorescence observed in ADHD cybrid-neurons implied higher mitochondrial depolarisation in these cells. Mitochondrial membrane potential was also analysed in differentiated cybrid neurons [20] by fluorimetric and FACS analysis and we observed similar results (data are not shown) as in undifferentiated neurons.
Fig. 2.
Mitotracker Green®,TMRM and MitoSOX™ staining of control and ADHD cybrids: (A) Confocal images of Mitotracker Green® staining of the cybrids. (B) The intensity of Mitotracker Green® fluorescence quantified by Image J software. (C & D) The graphs showing the percent change of TMRM and MitoSOX™ fluorescence staining measured by fluorimetry and (E & G) FACS analysis, in ADHD as compared to the control cybrids. (F & H) are the representative scan of cybrids. Data are presented as Mean ± SEM. Values of p* ≤ 0.05 are considered significant. C6 and C9 are control cybrids, ADHD1, 5 and 6 are cybrids prepared using platelets of ADHD probands. Scale bar represents 10 μm.
3.1.3. Higher mitochondrial oxidative stress in ADHD cybrids
Likewise MitoSOX™ staining was carried out to test the mitochondrial oxidative stress generated in these cybrids neurons employing spectrofluorimetric (Fig. 2D) and flow cytometric (Fig. 2G and H) analyses. Interestingly ADHD cybrids displayed higher levels of superoxide radicals, as evidenced from the significantly increased MitoSOX™ fluorescence in the cells.
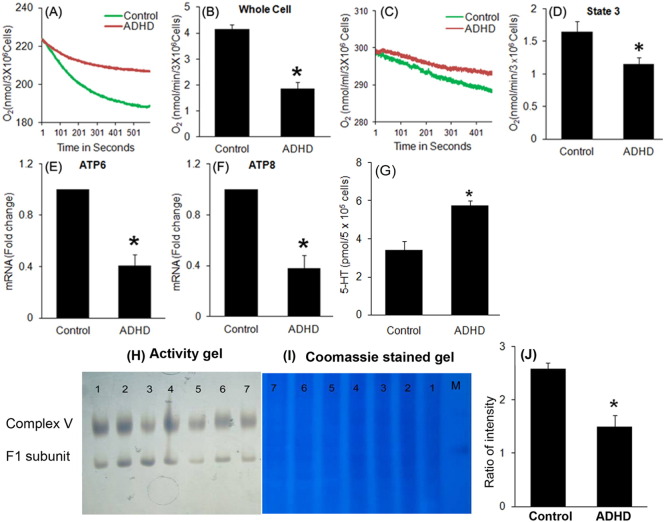
3.1.4. Reduced oxygen consumption due to complex V deficiency in diseased cybrids
Oxygen consumption was monitored in controls and ADHD non-permeabilized (Fig. 3A and B) and permeabilized cells (Fig. 3C and D) employing a sensitive Oxygraph in order to understand the respiratory capability of the cybrids. Significantly reduced rate of respiration found in ADHD cybrids, as well as in the mitochondria of these disease-cybrids, pointed to a significant loss of mitochondrial functions in both these diseases. Lower respiration rate could be resulting from the considerable loss in the ATPase 6/8 transcript levels in ADHD cybrids revealed in quantitative PCR analysis as seen in the present study (Fig. 3E and F).
Fig. 3.
Whole cell and mitochondrial state3 respiration, APTase6/8 subunits expression, complex V activity and serotonin levels in control and ADHD cybrids: Whole cell respiration (A), cellular rate of oxygen consumption per 3 × 106 cells (B), mitochondrial State3 respiration (C), and mitochondrial oxygen consumption rate per 3 × 106 cells in ADHD and control cybrids (D). The cDNA prepared from total RNA of ADHD and control cybrids were subjected to qRT-PCR analysis using specific primers to accurately measure the transcript level of ATPase6/8 (E, F). Levels of serotonin in differentiated control and ADHD cybrid-neurons (G). Complex V activity using BN-PAGE, Activity gel (H), Coomassie staining gel (I). Bar diagram shows the difference in complex V activity analysed by Image software (J). (Control samples- 1 to 4 lanes and ADHD samples- 5 to 7 lanes in both the gels, M lane is marker). Data are presented as Mean ± SEM. Values of p* ≤ 0.05 is considered significant.
3.1.5. Higher level of 5HT in ADHD cybrid neurons and reduced activity of complex V
Serotonin level, measured by HPLC-ECD in differentiated neurons, was found to be higher in ADHD cybrids as compared to controls (Fig. 3G). BN-PAGE in-gel activity studies demonstrated a significant deficiency in mitochondrial complex V activity in ADHD cybrids, when compared to the control cybrids (Fig. 3H to J).
4. Discussion
Most important feature of the present study is the successful creation of control and ADHD cybrids from an east-Indian population. This is confirmed by successful incorporation of mtDNA into ρ0-cells, which did not have mtDNA before fusion with the patient or control platelets. This is the first ever report on production of mitochondrial cell-hybrids (cybrids) for the neurodevelopmental disorder, ADHD. Another important attribute of this study is the finding of significant mitochondrial aberrations and dysfunctions, as evidenced by reduced staining intensity of Mitotracker Green®, TMRM and increase in MitoSOX fluorescence, and significant reduction in oxygen consumption concurrent with low levels of ATPase 6/8 transcripts in ADHD cybrids in comparison to control cybrid-neurons. These observations support a significant bioenergetic crisis in ADHD, which was proposed [9], but never demonstrated. The third important observation made in the present study is the significant increase in the levels of serotonin in the differentiated ADHD cybrid-neurons as compared to control cybrid-neurons, which is a topic of interest and intense debate.
Mitotracker green dye accumulates in the mitochondrial matrix where it covalently reacts with free thiol groups of cysteine residues and produce green fluorescence and allows to visualize the mostly inter-netted, tubular fluorescing mitochondria in the cytoplasm of control cybrids, but punctate (due to fragmented mitochondria) fluorescence in diseased cybrids. Quantification of mitotracker green staining by ImageJ software gives the total mass of the mitochondria present in the cytosol [23] which was found less in ADHD cybrids as compared to the control cybrids. This data speculates that due to fragmentation of mitochondria the total mass in the cytoplasm decreases. Significantly low TMRM fluorescence observed in ADHD cybrid-neurons implied higher mitochondrial depolarisation in these cells. No report is available in literature which deals with mitochondrial membrane potential and ADHD, and therefore the present report is the first in literature. ADHD cybrids displayed higher levels of superoxide radicals, as evidenced from the significantly increased MitoSOX™ fluorescence in the cells. These amply provide proof that in ADHD there exist a serious oxidative stress condition, and that could be detrimental to the health of the neurons. In one study (48 children and adolescents (34 male, 14 female) with ADHD who had no neurological, systemic, or comorbid psychiatric disorders, and 24 sex- and age-matched healthy controls (17 male and seven female), it was observed that ADHD patients have oxidative imbalance [24]. In one another study one group investigated total antioxidative status and total oxidative status of plasma and antioxidant enzyme. Oxidative stress index values and the plasma TOS levels of the patients with ADHD were statistically higher than those of the control group [25]. Sezen et al. [26] also investigated and found that oxidative stress was higher in the ADHD patients than the control group. Bioenergetic dysregulation playing key roles in many neuropsychiatric disorders is recently reviewed [27]. This may result from defective mitochondrial ETC complex function, which is validated by a significant decrease in state3 respiration in ADHD cybrids. Considerable decrease in the ETC complex V ATPase 6/8 subunits in ADHD cybrids further provides positive evidences in this direction. ATPase 6/8 mutations are associated with many neurodevelopmental disorders including autism [28], [29], with which ADHD shows overlapping syndromes [30]. The decreased transcript level of ATP6 and ATP8 subunits may lead to the lower activity of complex V in ADHD cybrids as our BN-PAGE data shows.These evidences firmly suggest that mitochondrial dysfunction exists in ADHD.
The status of mitochondrial energetics in ADHD subjects is not available. However, indirect evidences from pharmacological studies using methylphenidate, which is a drug commonly used to treat ADHD have shown that the drug affects the activity of mitochondrial ETC enzymes and results in increase of the extracellular levels of the catecholamines that stimulate glycolysis and release of lactate from the astrocytes, thereby correcting the energy deficiency, and restoring appropriate firing rates [10]. This has led to the hypothesis that impairment of mitochondrial bioenergetic machinery may play a role in autism and ADHD pathogenesis [9], [31].
Serotoninergic system, known to modulate impulse control and aggression, is challenged in ADHD patients [32]. At a time when mitochondrially-located MAO-A or MAO-B were unaffected in ADHD cybrids, the differentiated cybrid-neurons from ADHD probands exhibited 2-fold increase in serotonin indicating probably an active role of this biogenic amine in the phenotypes of the disease. If this is proved to be true, these cybrid-neurons can be used as a cellular model for ADHD to investigate neuromolecular mechanisms underlying ADHD pathology.
At a time when no direct evidence of mitochondrial dysfunctions in ADHD is available, we created and used ADHD cybrids to assess mitochondrial functions in this neurodevelopmental disorder. Cybrids created by fusion of ρ0-cells and Parkinson’s disease (PD) patient platelets are shown to replicate mitochondrial pathology seen in post-mortem PD brains [11], and differentiation of these cells into neurons are demonstrated to retain the mitochondrial defects [22]. Therefore, ADHD cybrids and the cybrid-neurons created in the present report could be reliable tools to study the mitochondrial dynamics and bioenergetics, and to understand the molecular mechanisms underlying the pathophysiology of ADHD.
In short, this is the first report that identifies mitochondrial dysfunction as an inherent factor of ADHD pathology, and for probable direct role of serotoninergic system in the disease syndromes. Increased serotonin content in the differentiated cybrid-neurons suggests that the mitochondrial defect in these cells can significantly alter the serotonergic neurotransmitter function, which could be a pathological hallmark of ADHD. This study identifies mitochondrial pathology as one of the risk factors for ADHD, and the cybrid model provides a novel, reliable and valid tool to study the molecular basis of ADHD at cellular level.
Source of support
Financial support to IUCBR from Department of Higher Education, Govt. of Kerala through Mahatma Gandhi University, Kottayam is gratefully acknowledged. Department of Biotechnology, Govt. of India grants-in-aid to U.R., K.M. and K.P.M., who are the principal investigators of the project and CSIR-IICB-Supra-institutional project funding (BenD, BSC 0206) of the 12th Five Year Plan by Council of Scientific & Industrial Research (CSIR), Govt. of India to K.P.M. are gratefully acknowledged. P.V. and A.S. are supported by Junior and Senior Research Fellowships from CSIR/UGC, Govt. of India, respectively and D.N.N.N. is DBT-TWAS fellow.
Potential conflicts of interest
The authors declare no conflict of interest.
Transparency document
Transparency document.
Footnotes
The Transparency document associated with this article can be found, in online version.
References
- 1.Willcutt E.G. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics. 2012;9:490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mattson M.P., Gleichmann M., Cheng A. Mitochondria in neuroplasticity and neurological disorders. Neuron. 2008;60:748–766. doi: 10.1016/j.neuron.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scaglia F. The role of mitochondrial dysfunction in psychiatric disease, developmental disabilities. Dev. Disabil. Res. Rev. 2010;16:136–143. doi: 10.1002/ddrr.115. [DOI] [PubMed] [Google Scholar]
- 4.Jeanneteau F., Arango-Lievano M. Linking Mitochondria to Synapses: New Insights for Stress-Related Neuropsychiatric Disorders. Neural Plast. 2016 doi: 10.1155/2016/3985063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris G., Berk M. The many roads to mitochondrial dysfunction in neuroimmune and neuropsychiatric disorders. BMC Med. 2015 doi: 10.1186/s12916-015-0310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gu F., Chauhan V., Kaur K., Brown W.T., LaFauci G., Wegiel J., Chauhan A. Alterations in mitochondrial DNA copy number and the activities of electron transport chain complexes and pyruvate dehydrogenase in the frontal cortex from subjects with autism. Transl. Psychiatry. 2013;3 doi: 10.1038/tp.2013.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taurines R., Schwenck C., Westerwald E., Sachse M., Siniatchkin M., Freitag C. ADHD and autism: differential diagnosis or overlapping traits? A selective review. Atten. Defic. Hyperact. Disord. 2012;4:115–139. doi: 10.1007/s12402-012-0086-2. [DOI] [PubMed] [Google Scholar]
- 8.Musser E.D., Hawkey E., Kachan-Liu S.S., Lees P., Roullet J.B., Goddard K., Steiner R.D., Nigg J.T. Shared familial transmission of autism spectrum and attention-deficit/hyperactivity disorders. J. Child Psychol. Psychiatry. 2014;55:819–827. doi: 10.1111/jcpp.12201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russell V.A., Oades R.D., Tannock R., Killeen P.R., Auerbach J.G., Johansen E.B., Sagvolden T. Response variability in Attention-Deficit/Hyperactivity Disorder: a neuronal and glial energetics hypothesis. Behav. Brain Funct. 2006;2:30. doi: 10.1186/1744-9081-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fagundes A.O., Rezin G.T., Zanette F., Grandi E., Assis L.C., Dal-Pizzol F., Quevedo J., Streck E.L. Chronic administration of methylphenidate activates mitochondrial respiratory chain in brain of young rats. Int. J. Dev. Neurosci. 2007;25:47–51. doi: 10.1016/j.ijdevneu.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Borland M.K., Mohanakumar K.P., Rubinstein J.D., Keeney P.M., Xie J., Capaldi R., Dunham L.D., Trimmer P.A., Bennett J.P., Jr. Relationships among molecular genetic and respiratory properties of Parkinson's disease cybrid cells show similarities to Parkinson's brain tissues. Biochim. Biophys. Acta. 2009;1792:68–74. doi: 10.1016/j.bbadis.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silva D.F., Selfridge J.E., Lu J., Lezi E., Roy N., Hutfles L., Burns J.M., Michaelis E.K., Yan S.S., Cardoso S.M. Bioenergetic flux, mitochondrial mass and mitochondrial morphology dynamics in AD and MCI cybrid cell lines. Hum. Mol. Genet. 2013;22:3931–3946. doi: 10.1093/hmg/ddt247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conners C.K., Sitarenios G., Parker J.D.A., Epstein J.N. Revision and restandardization of the Conners Teacher Rating Scale (CTRS-R): factor structure, reliability, and criterion validity. J. Abnorm. Child Psychol. 1998;26:279–291. doi: 10.1023/a:1022606501530. [DOI] [PubMed] [Google Scholar]
- 14.Silverstein A.B. Reliability of score differences on Wechsler's intelligence scales. J. Clin. Psychol. 1991;47:264–266. doi: 10.1002/1097-4679(199103)47:2<264::aid-jclp2270470212>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 15.King M.P., Attardi G. Human cells lacking mtDNA: repopulation with exogenous mitochondria by complementation. Science. 1989;246:500–503. doi: 10.1126/science.2814477. [DOI] [PubMed] [Google Scholar]
- 16.Appukuttan T.A., Varghese M., Gangopadhyay P.K., Mohanakumar K.P. Creation of cybrids for investigating mitochondrial electron transport chain functions in Parkinson’s disease. J. Cell Tissue Res. 2011;11:2445–2450. [Google Scholar]
- 17.Pandey M., Varghese M., Sindhu K.M., Sreetama S., Navneet A.K., Mohanakumar K.P., Usha R. Mitochondrial NAD +-linked State 3 respiration and complex-I activity are compromised in the cerebral cortex of 3-nitropropionic acid-induced rat model of Huntington's disease. J. Neurochem. 2008;104:420–434. doi: 10.1111/j.1471-4159.2007.04996.x. [DOI] [PubMed] [Google Scholar]
- 18.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 19.Nijtmans L.J., Henderson N.S., Holt I.J. Blue Native electrophoresis to study mitochondrial and other protein complexes. Methods. 2002;26:327–334. doi: 10.1016/S1046-2023(02)00038-5. [DOI] [PubMed] [Google Scholar]
- 20.Feeney C.J., Pennefather P.S., Gyulkhandanyan A.V. A cuvette-based fluorometric analysis of mitochondrial membrane potential measured in cultured astrocyte monolayers. J. Neurosci. Methods. 2003;125:13–25. doi: 10.1016/s0165-0270(03)00027-x. [DOI] [PubMed] [Google Scholar]
- 21.Borah A., Mohanakumar K.P. Long-term L-DOPA treatment causes indiscriminate increase in dopamine levels at the cost of serotonin synthesis in discrete brain regions of rats. Cell. Mol. Neurobiol. 2007;27:985–996. doi: 10.1007/s10571-007-9213-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Appukuttan T.A., Ali N., Varghese M., Singh A., Tripathy D., Padmakumar M., Gangopadhyay P.K., Mohanakumar K.P. Parkinson’s disease cybrids, differentiated or undifferentiated, maintain morphological and biochemical phenotypes different from those of control cybrids. J. Neurosci. Res. 2013;91:963–970. doi: 10.1002/jnr.23241. [DOI] [PubMed] [Google Scholar]
- 23.Agnello M., Morici G., Rinaldi A.M. A method for measuring mitochondrial mass and activity. Cytotechnology. 2008;56:145–149. doi: 10.1007/s10616-008-9143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kul M., Unal F., Kandemir H., Sarkarati B., Kilinc K., Kandemir S.B. Evaluation of Oxidative Metabolism in Child and Adolescent Patients with Attention Deficit Hyperactivity Disorder. Psychiatry Investig. 2015;12:361–366. doi: 10.4306/pi.2015.12.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guney E., Cetin F.H., Alisik M., Tunca H., Tas T.Y., Iseri E., Isik T.Y., Cayci B., Erel O. Attention Deficit Hyperactivity Disorder and oxidative stress: A short term follow up study. Psychiatry Res. 2015;229:310–317. doi: 10.1016/j.psychres.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Sezen H., Kandemir H., Savik E., Basmacı K.S., Kilicaslan F., Bilinc H., Aksoy N. Increased oxidative stress in children with attention deficit hyperactivity disorder. Redox Rep. 2016 doi: 10.1080/13510002.2015.1116729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streck E.L., Gonçalves C.L., Furlanetto C.B., Scaini G., Dal-Pizzol F., Quevedo J. Mitochondria and the central nervous system: searching for a pathophysiological basis of psychiatric disorders. Rev. Bras. Psiquiatr. 2014;36:156–167. doi: 10.1590/1516-4446-2013-1224. [DOI] [PubMed] [Google Scholar]
- 28.Safaei S., Houshmand M., Banoei M.M., Shafa M., Nafissi S., Parivar K., Rostami M., Shariati P. Mitochondrial tRNALeu/Lys and ATPase 6/8 gene variations in spinocerebellar ataxias. Neurodegener. Dis. 2009;6:16–22. doi: 10.1159/000170885. [DOI] [PubMed] [Google Scholar]
- 29.Piryaei F., Houshmand M., Aryani O., Dadgar S., Soheili Z. Investigation of the mitochondrial ATPase 6/8 and tRNALys genes mutations in autism. Cell J. 2012;14:98–101. [PMC free article] [PubMed] [Google Scholar]
- 30.Ghanizadeh A. Co-morbidity and factor analysis on attention deficit hyperactivity disorder and autism spectrum disorder DSM-IV-derived items. J. Res. Med. Sci. 2012;17:368–372. [PMC free article] [PubMed] [Google Scholar]
- 31.Lombard J. Autism: a mitochondrial disorder? Med. Hypotheses. 1998;50:497–500. doi: 10.1016/s0306-9877(98)90270-5. [DOI] [PubMed] [Google Scholar]
- 32.Chantiluke K., Barrett N., Giampietro V., Brammer M., Simmons A., Murphy D.G., Rubia K. Inverse Effect of fluoxetine on medial prefrontal cortex activation during reward reversal in ADHD and autism. Cereb. Cortex. 2015;25:1757–1770. doi: 10.1093/cercor/bht365. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.