Abstract
Acute fibrinous and organizing pneumonia (AFOP) is a histological pattern characterized by intra-alveolar fibrin deposition and associated organizing pneumonia. AFOP has been associated with many rheumatologic disorders in the literature but has not been described in association with Sjogren's syndrome.
This paper shows a rare association of AFOP with Sjogren's syndrome. Patient's symptoms promptly improved after treatment with steroid.
1. Introduction
Acute fibrinous and organizing pneumonia (AFOP) is a type of acute or subacute lung injury characterized by a dominant histological pattern of patchy intra-alveolar fibrin and organizing pneumonia which does not meet the histologic criteria for pattern of diffuse alveolar damage (DAD), organizing pneumonia (OP), or eosinophilic pneumonia (EP) [1]. The histological pattern are devoid of hyaline membrane, eosinophils, granulomatous inflammation, extensive pneumonia or abscess [1]. Other minor features include acute or chronic inflammation, type 2 pneumocyte hyperplasia and alveolar expansion with myxoid tissue [1].
This entity was first published by Beasley et al., in 2002. The case of 17 patients showed male and white predominance with average age of 62 years. Average time to onset of symptoms was 19 days, and the most common symptoms includes cough, shortness of breath and constitutional symptoms like fatigue or malaise [1].
AFOP etiology could be idiopathic or due to a wide range of medical conditions including rheumatologic diseases like ankylosing spondylitis, systemic lupus erythematous, polymyositis, polymyalgia and juvenile dermatomyositis [1], [2].
Sjogren's syndrome is a slowly progressive autoimmune disorder that affects many organ systems. Sjogren's syndrome commonly present with symptoms related to decrease lacrimal and salivary gland function [3]. Pulmonary involvement in Sjogren's syndrome is common. Histological pattern seen in Sjogren's syndrome include nonspecific interstitial pneumonia, usual interstitial pneumonia, organizing pneumonia, lymphocytic interstitial pneumonia, primary pulmonary lymphoma and diffuse interstitial amyloidosis [4]. Noncaseating granulomas and bronchiolitis have also been described [5].
Acute fibrinous and organizing pneumonia has not been associated with Sjogren's syndrome to date. We present a case report of AFOP in a patient with Sjogren's syndrome.
2. Case report
We report a case of a 75-year-old female who presented with worsening shortness of breath, wheezing and fatigue of about one week duration. She also had productive cough with white sputum of about three days duration. She was diagnosed of SSA and SSB antibody positive Sjogren's syndrome about nine years before presentation. Her manifestations of Sjogren's syndrome include dry skin, arthritis, rash and pulmonary hypertension in which she was on 3 L of nasal cannula of oxygen at home. Her symptoms had been controlled with mycophenolate mofetil 500mg twice daily, hydroxychloroquine 200mg daily and prednisone 10mg daily. Other past medical history includes pulmonary embolism, gastroesophagus reflux disease, hyperlipidemia and hypertension. She had similar presentation about three months earlier for which she was managed by increasing her prednisone dose. Her symptoms improved and she was back to her baseline. She admits to not taking her prednisone after she felt better.
She originally presented to our clinic on the day of admission with shortness of breath, wheezing, fatigue and productive cough. She was found to be tachypneic, hypoxemic and had diffuse wheezes and rhonchi on lung examination. She was sent to the hospital for further evaluation. She was subsequently admitted.
On admission, she was hypoxic and was placed on 5 L of nasal cannula oxygen. CT angiogram of the chest was done to rule out pulmonary embolism. There was no pulmonary embolism present; however there was bilateral multilobar areas of consolidation (Fig. 1 and Fig. 2).
Fig. 1.
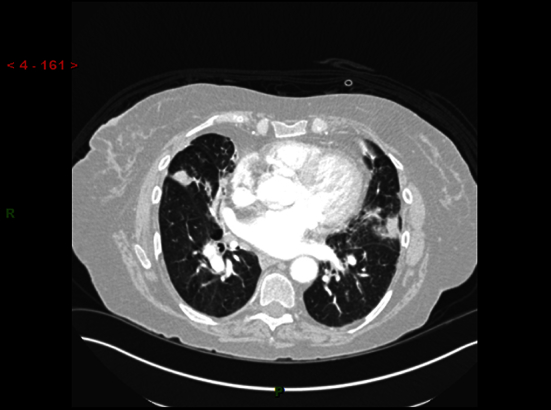
CT scan showing bilateral multilobar areas of consolidation.
Fig. 2.
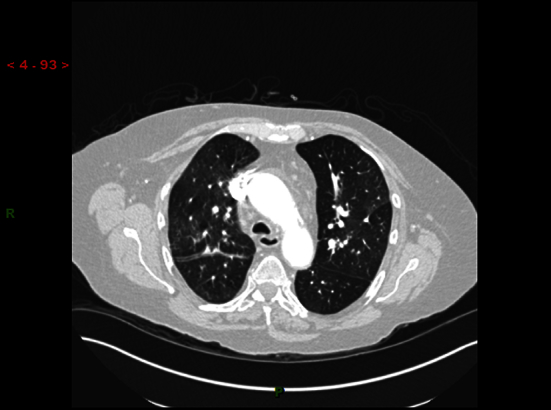
CT scan showing bilateral multilobar areas of consolidation.
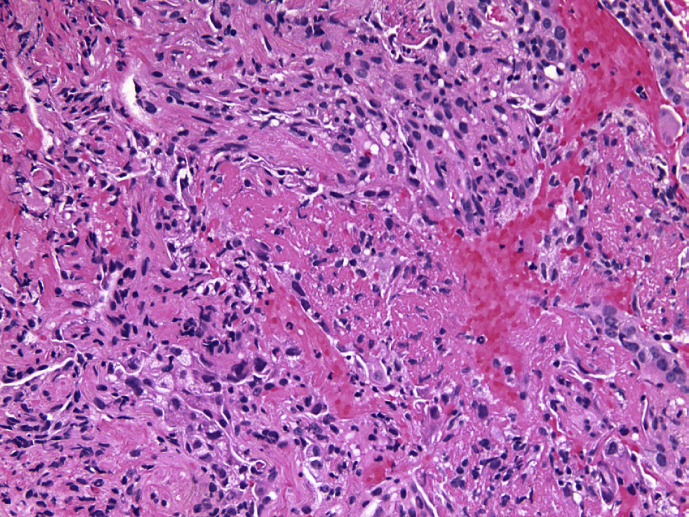
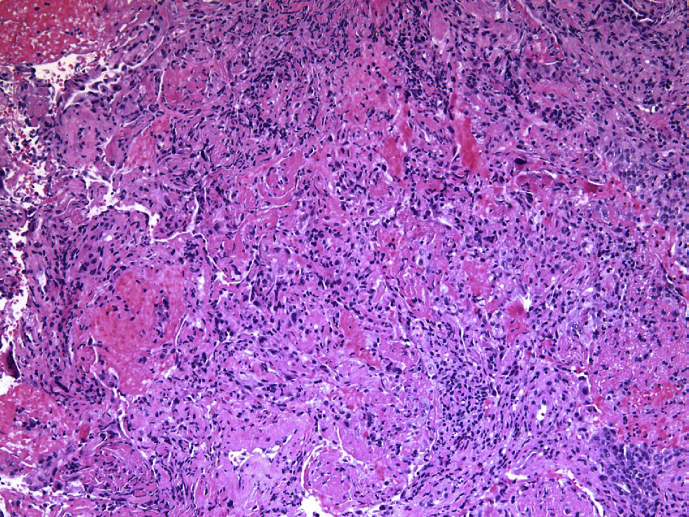
She was started of vancomycin, cepefime and azithromycin for possible pneumonia. She underwent bronchoscopy on hospital day 3, bronchioalveolar lavage (BAL) and transbronchial biopsy was done at the time. BAL showed presence of alveola macrophages, reactive pneumocytes with rare neutrophils and lymphocytes. Transbronchial biospsy revealed fragments of lung parenchyma with focal areas of organization with intraalveolar fibrin accumulation, reactive type II pneumocyte hyperplasia and associated focal acute and chronic inflammation. These were consistent with the diagnosis of acute fibrinous and organizing pneumonia (Fig. 3, Fig. 4).
Fig. 3.
Intra-alveolar fibrin accumulation without hyaline membrane formation (hematoxylin-eosin, original magnification ×100).
Fig. 4.
Organizing pneumonia with focal intra-alveolar fibrin (hematoxylin-eosin, original magnification ×200).
Both BAL and transbronchial biopsy was negative for malignant cells. All respiratory cultures grew normal respiratory flora. She was restarted on prednisone 40mg daily. She improved remarkably after 8 days of hospitalization and was discharged home. She was to restart her mycophenolate mofetil and hydrochloroquine as infectious disease workup was negative. She was to continue prednisone 40mg daily and taper by reduction of 10mg every 2 weeks.
3. Discussion
AFOP is a relatively new entity with less than 115 cases reported in the literature up till 2015 [6]. AFOP have been associated with rheumatologic disease, infections, drug reaction, environmental exposures, autoimmune disease and lung transplantation [1], [6].
We are reporting the first case of AFOP associated with Sjogren's syndrome.
Tissue histopathology is characterized by intra-alveolar fibrin in the form of fibrin ‘‘balls’’ and organizing pneumonia with a patchy distribution [1], [7].
AFOP have histological pattern similar to DAD, OP and EP but has its own distinct histopathology. AFOP pattern can be distinguished from that of DAD because the fibrin in AFOP is organized into balls within the alveolar spaces and the classic hyaline membranes seen in DAD are not seen in AFOP [1]. Histologically, EP may also have prominent intra-alveolar fibrin like AFOP, however the eosinophils predominates in EP [1]. It also present acutely or subacutely just like DAD or OP.
Our patient fulfilled the 3 major criteria including organization of intra-alveolar fibrin, organizing pneumonia and the distribution was patchy. The histopathology pattern also fulfil at least two minor features including type II pneumocyte hyperplasia and presence of acute and chronic inflammation.
The clinical course and radiologic findings are similar to that of OP. Patients with rapidly progressive disease have imaging findings similar to DAD with diffuse but basilar-dependent consolidation and ground glass opacity. Patients with a subacute course have imaging findings that mirror that of OP and can include both focal and diffuse parenchymal abnormality [8]. AFOP can lead to pulmonary fibrosis on imaging just like DAD and OP [8].
The mainstay treatment in the literature for AFOP is steroids; however other immunosuppresants and antibiotics have also been used with varying results (Table 1). Overall, many cases responds to steroids, however, therapeutic modality did not correlate with the outcome [1].
Table 1.
Cases associated with rheumatologic disease are rare with only 8 cases published in the literature.
| Author, year | Age, sex | Rheumatologic disorder | Treatment | Outcome |
|---|---|---|---|---|
| Sauter et al., 2014 [10] | 66, F | Antisynthetase syndrome | Azathioprine | Good |
| Mycophenolate | ||||
| Steroid | ||||
| Valim et al., 2012 [2] | 39, F | Undifferentiated connective tissue disease | Cylophosphamide, steroid | Death |
| Hariri et al., 2010 [11] | 16, M | SLE | Steroid, cyclophosphamide, anticoagulants | Good |
| Balduin et al., 2007 [12] | 47, M | Stigmata of rheumatoid disease | Steroid | Good |
| Prahalad et al., 2005 [13] | 14, F | Juvenile dermatomyositis | Antibiotics, immunoglobulin, cyclophosphamide, steroid and cyclosporine | Death |
| Beasley et al., 2002 [1] | 55, M | Ankylosing spondylitis | Steroid | Good |
| 78, F | Polymyositis | Steroid | Death | |
| 58, F | Fibromyalgia | Antibiotics | Good |
The largest study of patients with AFOP involved a series of 22 patients that have undergone lung transplant. The prognosis was worse in these group of patients versus those with obliterative bronchiolitis [9].
Our patient had a favorable outcome after the diagnosis. However, long term outcome needs to be evaluated.
4. Conclusion
Although AFOP have been associated with other rheumatologic disorders, this is the first case associated with Sjogren's syndrome.
Contributor Information
Adebayo Fasanya, Email: afasanya@wpahs.org.
Viral Gandhi, Email: Viral.GANDHI@ahn.org.
Christina DiCarlo, Email: Christina.DICARLO@ahn.org.
Raghukumar Thirumala, Email: Raghukumar.THIRUMALA@ahn.org.
References
- 1.Beasley M.B., Franks T.J., Galvin J.R., Gochuico B., Travis W.D. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch. Pathol. Lab. Med. 2002;126(9):1064–1070. doi: 10.5858/2002-126-1064-AFAOP. [DOI] [PubMed] [Google Scholar]
- 2.Valim V., Rocha R.H., Couto R.B., Paixao T.S., Serrano E.V. Acute fibrinous and organizing pneumonia and undifferentiated connective tissue disease: a case report. Case Rep. Rheumatol. 2012;2012:549298. doi: 10.1155/2012/549298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassan S.S., Moutsopoulos H.M. Clinical manifestations and early diagnosis of Sjogren syndrome. Arch. Intern Med. 2004;164(12):1275–1284. doi: 10.1001/archinte.164.12.1275. [DOI] [PubMed] [Google Scholar]
- 4.Parambil J.G., Myers J.L., Lindell R.M., Matteson E.L., Ryu J.H. Interstitial lung disease in primary Sjogren syndrome. Chest. 2006;130(5):1489–1495. doi: 10.1378/chest.130.5.1489. [DOI] [PubMed] [Google Scholar]
- 5.Shi J.H., Liu H.R., Xu W.B. Pulmonary manifestations of Sjogren's syndrome. Respiration. 2009;78(4):377–386. doi: 10.1159/000214841. [DOI] [PubMed] [Google Scholar]
- 6.Kuza C., Matheos T., Kathman D., Heard S.O. Life after acute fibrinous and organizing pneumonia: a case report of a patient 30 months after diagnosis and review of the literature. J. Crit. Care. 2016;31(1):255–261. doi: 10.1016/j.jcrc.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatti S., Hakeem A., Torrealba J., McMahon J.P., Meyer K.C. Severe acute fibrinous and organizing pneumonia (AFOP) causing ventilatory failure: successful treatment with mycophenolate mofetil and corticosteroids. Respir. Med. 2009;103(11):1764–1767. doi: 10.1016/j.rmed.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Kligerman S.J., Franks T.J., Galvin J.R. From the radiologic pathology archives: organization and fibrosis as a response to lung injury in diffuse alveolar damage, organizing pneumonia, and acute fibrinous and organizing pneumonia. Radiographics. 2013;33(7):1951–1975. doi: 10.1148/rg.337130057. [DOI] [PubMed] [Google Scholar]
- 9.Paraskeva M., McLean C., Ellis S. Acute fibrinoid organizing pneumonia after lung transplantation. Am. J. Respir. Crit. Care Med. 2013;187(12):1360–1368. doi: 10.1164/rccm.201210-1831OC. [DOI] [PubMed] [Google Scholar]
- 10.Sauter J.L., Butnor K.J. Expanding the spectrum of pulmonary histopathological manifestations of anti-synthetase syndrome: anti-EJ-associated acute fibrinous and organizing pneumonia. Histopathology. 2014;65(4):581–582. doi: 10.1111/his.12420. [DOI] [PubMed] [Google Scholar]
- 11.Hariri L.P., Unizony S., Stone J. Acute fibrinous and organizing pneumonia in systemic lupus erythematosus: a case report and review of the literature. Pathol. Int. 2010;60(11):755–759. doi: 10.1111/j.1440-1827.2010.02586.x. [DOI] [PubMed] [Google Scholar]
- 12.Balduin R., Giacometti C., Saccarola L. Acute fibrinous and organizing pneumonia in a patient with collagen vascular disease “stigma”. Sarcoidosis Vasc. Diffuse Lung Dis. 2007;24(1):78–80. [PubMed] [Google Scholar]
- 13.Prahalad S., Bohnsack J.F., Maloney C.G., Leslie K.O. Fatal acute fibrinous and organizing pneumonia in a child with juvenile dermatomyositis. J. Pediatr. 2005;146(2):289–292. doi: 10.1016/j.jpeds.2004.09.023. [DOI] [PubMed] [Google Scholar]