Abstract
Background
There are poorer outcomes following ST elevation myocardial infarction in blacks compared to white patients despite comparable door‐to‐reperfusion time. We hypothesized that delays to hospital presentation may be contributory.
Methods and Results
We conducted a retrospective analysis of the 1144 patients admitted for STEMI in our institution from 2008 to 2013. The door‐to‐balloon time (D2BT) and symptom‐onset‐to‐door time (SODT) were compared by race. Bivariate analysis was done comparing the median D2BT and SODT. Stratified analyses were done to evaluate the effect of race on D2BT and SODT, accounting for insurance status, age, sex and comorbidities. The mean age was 59±13 years; 56% of this population was black and 41% was white. Males accounted for 66% of this population. The median D2BT was 60 minutes (interquartile range [IQR] 42–82), and median SODT was 120 minutes (IQR 60–720). There was no significant difference in D2BT by race (P=0.86). Black patients presented to the emergency room (ER) later than whites (SODT=180 [IQR 60–1400] vs 120 [IQR 60–560] minutes, P<0.01) and were more likely to be uninsured (P<0.01). After controlling for comorbidities, insurance, and socioeconomic status, blacks were 60% more likely to present late after a STEMI (OR 1.6, P<0.01). A subset analysis excluding transferred patients showed similar results.
Conclusions
Black patients present later to the ER after STEMI with no difference in D2BT compared to whites. This difference in time to presentation may be one of the factors accounting for poor outcomes in this population.
Keywords: disparities, door‐to‐balloon time, outcome, race and ethnicity, ST‐segment elevation myocardial infarction
Subject Categories: Quality and Outcomes, Race and Ethnicity, Percutaneous Coronary Intervention
Introduction
ST‐elevation myocardial infarction (STEMI) continues to be a leading cause of significant morbidity and mortality in the United States.1 Although whites have a higher prevalence of coronary artery disease, some studies have shown that ethnic minorities are associated with greater morbidity and mortality than white patients.2 Historically, favorable statistics regarding the management and outcomes of STEMI in the United States have been observed more often in white cohorts than in minorities.3 Black patients experience lower rates of emergency same‐day primary percutaneous coronary intervention (PCI) for STEMI and statin prescription at discharge compared to whites.4, 5 Large studies describe significantly greater risks of death, myocardial infarction, and need for revascularization following PCI and bleeding following fibrinolysis in blacks.2, 6 Additionally, some studies also report an association between black race and door‐to‐balloon times (D2BT) greater than 90 minutes.3, 7
We know that minimizing delays to treatment, both pre‐ and in hospital, reduces infarct size and mortality and is key to optimizing outcomes of revascularization.8, 9, 10, 11 Accordingly, bodies such as the American College of Cardiology (ACC) and American Heart Association (AHA) emphasize the consistent achievement of established door‐to‐needle and door‐to‐balloon benchmarks.9, 12, 13 A symptom‐onset‐to‐balloon time greater than 3 to 4 hours has been identified as an independent predictor of 1‐year mortality and has been suggested as an important benchmark in STEMI management.14 The lack of adherence to treatment benchmarks has been shown to correlate with an increase in short‐ and long‐term mortality.9, 13
This study was conducted to assess whether black patients are more likely to have longer delays from symptom onset to intervention (total ischemic time) and explored differences in the components of symptom‐onset‐to‐door time and D2BT. We hypothesized that black patients may have longer prehospital and in‐hospital delays to intervention, and this may contribute to the poorer STEMI outcomes found in this population.
Methods
We conducted a retrospective cohort study of consecutive patients, either diagnosed with STEMI between September 2008 and January 2013 at Methodist University Hospital or transferred from outlying facilities, who underwent emergent cardiac catheterization. Methodist University Hospital is a large tertiary hospital located in downtown Memphis, Tennessee. It is the largest primary PCI site in the region and receives transfers from numerous outlying facilities.
All patients admitted with a STEMI during this time period were retrospectively studied. Institutional Review Board approval was obtained with informed consent requirement waived. Information on demographics, risk factors, history, initial vital signs, laboratory data, presenting electrocardiogram, symptom onset time, procedure times, catheterization findings, and outcomes were collected. Data were de‐identified, extracted by medical residents and research assistants, and verified by cardiology fellows and staff cardiologists.
The primary outcome variable in this study was symptom onset to arrival time to the emergency room; secondary outcomes assessed were D2BT and in‐hospital mortality. Race was defined by self‐report and categorized as white, black, Hispanic, and others. Due to the small number of patients in this population identifying as Hispanics, this group was merged with the group called “others.”
The effect of race on these outcomes was explored, accounting for insurance status, socioeconomic status, and other confounders. Insurance was categorized as private, public, or uninsured. The effect of socioeconomic status was assessed using the United States census bureau data (http://quickfacts.census.gov/qfd/meta/long INC110213.htm and http://www.census.gov/hhes/www/income/data/statemedian/). Patients' income was defined based on the median income of the patients' zip code as obtained from census bureau data. Income categories were classified into below poverty line (<$25 000), relatively poor ($25 000–$52 000), above median ($52 000–$75 000), and comfortable (>$75 000). These were defined based on national census bureau data with the poverty line defined as a household income of $25 000 for a family of 4. The national median household income according to the census bureau was $52 000.
Symptom‐onset‐to‐door time (SODT) was defined in minutes from the time symptoms were first noticed to the time of arrival in the emergency room. Dichotomous data are presented as percentages. Continuous variables are presented as medians (interquartile ranges). Bivariate analysis was conducted using chi‐squared to assess for differences in demographics, clinical characteristics, risk factors, and outcomes by race. A binary outcome variable, “late presentation,” was defined as a SODT >180 minutes based on data from prior studies.14, 15, 16
A multivariate logistic regression analysis was then conducted to assess for the effect of race on “late presentation” after an STEMI while controlling for confounders, including age, sex, insurance status, socioeconomic status, diabetes mellitus, previous myocardial infarction, smoking, and mode of transportation to the emergency room. On completion of the initial analysis, further comparisons of patients admitted directly through our emergency room to those transferred from outlying facilities was conducted, and then a subset analysis was conducted assessing differences in SODT excluding all patients transferred from outlying facilities.
Results
Data were obtained on 1144 patients; the mean age was 59±13 years, and 66.3% were males. Whites accounted for 40.5% of the population, and 56.3% were blacks; 78.1% of this population were insured, 29.9% had diabetes mellitus, and 8.5% required bypass surgery. The in‐hospital mortality rate in this population was 6.9% (Table 1). The median D2BT and SODT were 60 and 120 minutes, respectively, and 47.5% of the population presented late after symptom onset. Forty‐one percent of patients had been transferred from outlying facilities.
Table 1.
Baseline Characteristics of Study Population
| Characteristic | n=1144 |
|---|---|
| Age, y (std dev) | 58.8 (±12.9) |
| Male, N (%) | 758 (66.3) |
| BMI, kg/m2 | 28.2 (24.8‐33.1) |
| Race, N (%) | |
| White | 463 (40.5) |
| Black | 644 (56.3) |
| Others | 37 (3.2) |
| Marital status, N (%) | |
| Married | 410 (35.8) |
| Insurance, N (%) | |
| Private | 322 (28.2) |
| Public | 559 (48.9) |
| None | 251 (21.9) |
| Risk factors, N (%) | |
| Diabetes mellitus | 342 (29.9) |
| Hyperlipidemia | 401 (35.1) |
| Hypertension | 767 (67.1) |
| Previous myocardial infarction | 292 (25.5) |
| Congestive heart failure | 103 (9.0) |
| Chronic kidney disease | 63 (5.5) |
| End‐stage renal disease | 36 (3.2) |
| Family history of CAD | 441 (38.6) |
| Tobacco use | 629 (55.0) |
| Outcomes, N (%) | |
| Confirmed STEMI | 755 (66.0) |
| Cerebrovascular accident | 7 (0.61) |
| STEMI due to stent thrombosis | 80 (7.0) |
| Shock | 78 (6.8) |
| Required CABG | 97 (8.5) |
| Death | 79 (6.9) |
| Median household income (IQR) | $32 412 (26 137‐38 826) |
| Median household income categories | |
| <$25 000 | 184 (16.1%) |
| $25 000 to $52 000 | 837 (73.2%) |
| $52 000 to $75 000 | 100 (8.7%) |
| >$75 000 | 11 (1.0%) |
| Times in minutes | |
| Median door to balloon, IQR | 60 (42‐82) |
| Median symptom onset to door, IQR | 120 (60‐720) |
| Late presentation (>180 minutes), N (%) | 429 (47.5) |
BMI indicates body mass index; CABG, coronary artery bypass graft; CAD, coronary artery disease; IQR, interquartile range; std dev, standard deviation; STEMI, ST elevation myocardial infarction.
On bivariate analysis (Table 2), black STEMI patients were more likely to be females (P=0.016), not married, uninsured, and live below the poverty line (all Ps <0.001). Blacks were also more likely to have specific comorbidities including systemic hypertension (P=0.004), congestive heart failure (P<0.001), and end‐stage renal disease (P<0.001), but there was no difference in rates of diabetes mellitus and previous myocardial infarctions. There was no ethnic difference in age at presentation in this study. Although black patients were less likely to require coronary artery bypass graft (CABG) (P<0.01) and to present in shock (P<0.01), there was no difference in mortality between these groups (P=0.38).
Table 2.
Table of Bivariate Analysis Comparing Black to White Population
| White, n=463 | Black, n=644 | P Value | |
|---|---|---|---|
| Age, y, (IQR) | 59 (51, 68) | 57 (50, 65) | |
| Male, N (%) | 327 (71.2) | 411 (64.3) | 0.016 |
| BMI, kg/m2 | 28.7 (25.5‐33.0) | 28.1 (24.4‐33.2) | 0.130 |
| Marital status, N (%) | <0.001 | ||
| Married | 233 (55.1) | 161 (26.3) | |
| Insurance, N (%) | <0.001 | ||
| Private | 178 (38.4) | 133 (20.7) | |
| Public | 202 (43.6) | 353 (54.9) | |
| None | 83 (17.9) | 157 (24.4) | |
| Risk factors, N (%) | |||
| Diabetes mellitus | 131 (28.3) | 206 (32.0) | 0.188 |
| Hyperlipidemia | 166 (35.9) | 228 (35.4) | 0.878 |
| Hypertension | 275 (59.4) | 477 (74.1) | <0.001 |
| Previous MI | 124 (26.8) | 162 (25.2) | 0.542 |
| CHF | 29 (6.3) | 73 (11.3) | 0.004 |
| CKD | 18 (3.9) | 45 (7.0) | 0.028 |
| ESRD | 5 (1.1) | 31 (4.8) | 0.001 |
| Family history of CAD | 221 (47.7) | 214 (33.2) | <0.001 |
| Tobacco use | 258 (55.7) | 359 (55.8) | 0.994 |
| Outcomes, N (%) | |||
| CVA | 1 (0.2) | 6 (1.0) | 0.142 |
| Shock | 42 (9.4) | 34 (5.4) | 0.012 |
| Required CABG | 53 (12.0) | 43 (6.9) | 0.005 |
| Death | 36 (7.8) | 41 (6.4) | 0.367 |
| Median household income | $34 568 | 27 637 | <0.001 |
| Median household income | <0.001 | ||
| <$25 000 | 35 (7.6) | 147 (22.8) | |
| $25 000 to $52 000 | 357 (77.3) | 461 (71.6) | |
| $52 000 to $75 000 | 63 (13.6) | 34 (5.3) | |
| >$75 000 | 7 (1.5) | 2 (0.3) | |
| Poverty | 35 (7.5) | 147 (22.8) | <0.001 |
| Median times in minutes | |||
| Door to balloon time, IQR | 58 (42‐89) | 60 (42‐77) | 0.863 |
| Symptom onset to door, IQR | 120 (60‐560) | 180 (60‐1400) | 0.001 |
| Late presentation (>180 minutes) | 151 (40.7%) | 272 (52.6%) | <0.001 |
Results are from the multivariable model. BMI indicates body mass index; CABG, coronary artery bypass graft; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; CVA, cerebrovascular accident; ESRD, end‐stage renal disease; IQR, interquartile range; MI, myocardial infarction.
In regard to socioeconomic factors, black patients were more likely to be uninsured as compared to whites (24.4% vs 17.9%, P<0.001). They were more likely to live below the poverty line (22.8% vs 7.5%, P<0.001), with a median household income of $27 637 (Table 2).
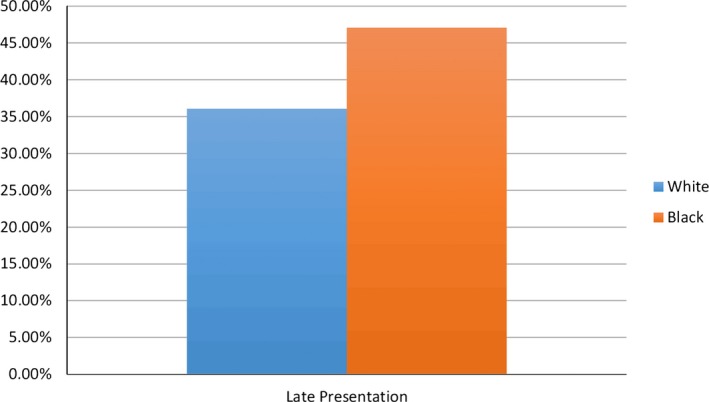
There was no difference in median D2BT (58 vs 60 minutes, P=0.863) (Figure 1). Black STEMI patients presented to the emergency room 1 hour later than their white counterparts (Figure 2). Median time to presentation was 180 versus 120 minutes in the white population (P<0.01). Over 52% of black patients presented to the emergency room “late” after symptom onset (>180 minutes) compared to 40% of white patients (P<0.01) (Figure 3). There was no significant difference in the mode of transportation to the emergency room in these groups: 97.3% versus 96.9% of patients arrived via either air or ground ambulance—85.2% of blacks came in via ground ambulance versus 69.2% of whites; 12.1% of blacks came in via air ambulance versus 27.7% of whites.
Figure 1.
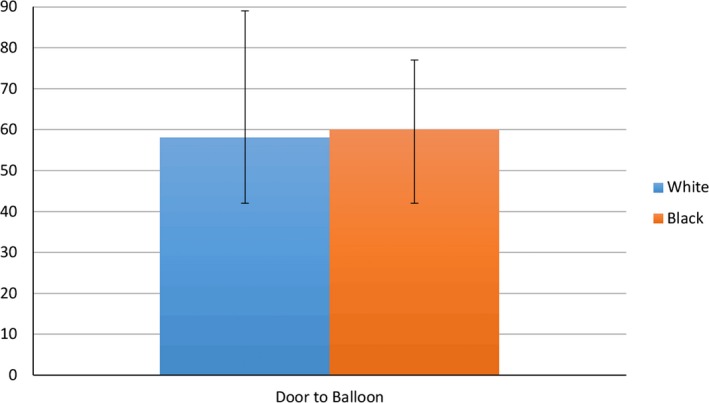
Door‐to‐balloon time according to race (minutes). Error bars represent the interquartile range.
Figure 2.
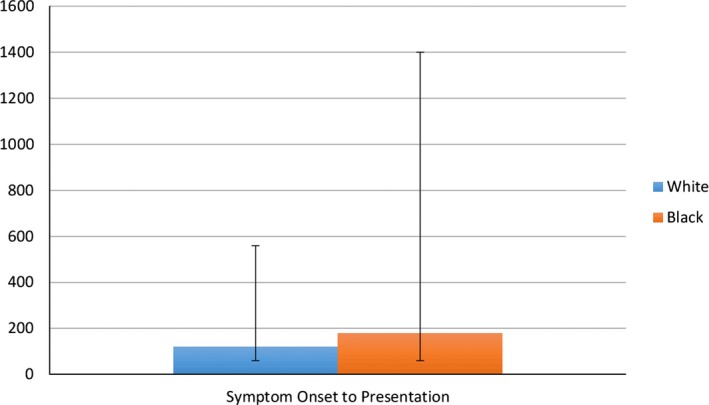
Symptom‐onset‐to‐door time according to race (minutes). Error bars represent the interquartile range.
Figure 3.
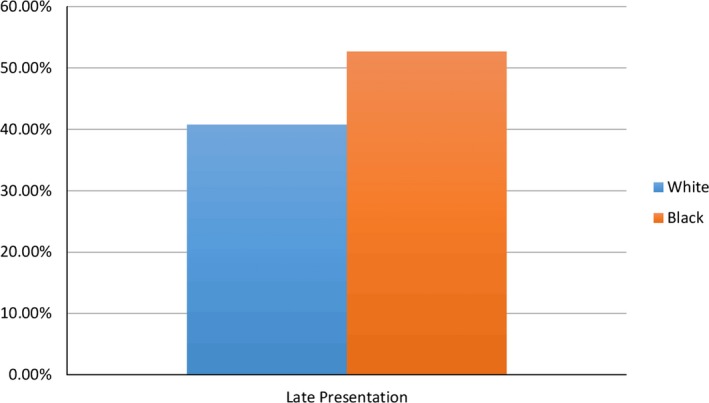
Late presentation (>180 minutes from symptom onset) according to race.
On multivariate analysis, blacks were 60% more likely than white patients to present late to the emergency room after STEMI (OR 1.60, P<0.01). The only other factor shown to predict time to presentation was insurance status. Patients with public insurance were more likely to present late (OR 2.60, P<0.01), and the uninsured were also 61% more likely to present late to the emergency room after STEMI (OR 1.61, P=0.04). Interaction between race and insurance status was tested and was found to be nonsignificant (P=0.36). After controlling for confounders, marital status and socioeconomic status were not shown to be predictors of late presentation in this study. Stratified analysis reporting the SODT comparing blacks versus whites, stratified according to insurance status, was reported (Figure 4) and showed among other things that median SODT among black publically insured patients was 270 (60–1440) versus 150 (60–960) minutes in the white population.
Figure 4.
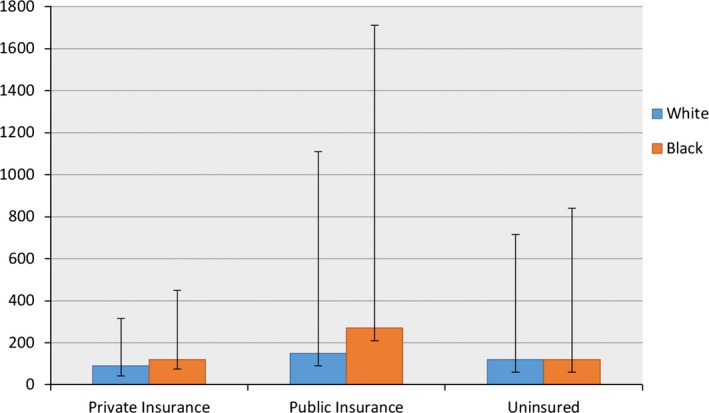
Late presentation (>180 minutes from symptom onset) according to race, excluding patients transferred from other hospitals. Error bars represent the interquartile range.
Of the 466 (41%) patients transferred in from outside facilities, the median age was 59 years, 44% were blacks, and 80% were insured. Compared to those directly admitted, transferred patients were more likely to present in cardiogenic shock (P=0.05) and to require CABG (P<0.01), but this did not translate to a significant mortality difference at discharge (P=0.40). In the subset analysis excluding patients transferred from other hospitals, blacks were still more likely to present late after symptom onset: 47% of black patients presented to the emergency room “late” after symptom onset (>180 minutes) compared to 36% of white patients (P=0.01) (Figure 5).
Figure 5.
Symptom‐onset‐to‐door time according to race and substratified by insurance status.
Discussion
This study showed that in a major urban regional tertiary center, there was a 60‐minute difference in SODT comparing black patients to white patients, with no difference in D2BT and mortality. In addition, this study showed that over 52% of black patients presented to the emergency room “late” after symptom onset (>180 minutes) compared to 40% of whites (P<0.01). After controlling for comorbidities, insurance, and socioeconomic status, blacks were 60% more likely than whites to present late to the emergency room after STEMI (OR 1.60, P<0.01). We also found that patients on public insurance (Medicare and Medicaid) and the uninsured were more likely to present late to the emergency room after STEMI. The parity achieved for in‐hospital care of STEMI patients in our study population irrespective of race and as reflected in comparable D2BT is the result of meticulous planning and a very robust protocol put in place to reduce system delays such as having the emergency medical services activate the STEMI call team from the field and education of health care personnel on cultural awareness. A major strength of this study is that it addresses the “real world” factors influencing outcomes in STEMI patients in the United States. Methodist University hospital, considered the largest referral center for STEMI in the mid‐South, reflects the actual condition of STEMI management in the region and shows the opportunities for improving care in these populations.
Our data suggest that measures being taken to reduce in‐hospital delays in STEMI management have been effective in reducing door‐to‐balloon time, but more work needs to be done to improve symptom‐onset‐to‐arrival time. With no significant difference in mode of transportation to the emergency room, the 60‐minute extra delay in presentation between blacks and whites appears to be driven by individual patient factors. These patient factors present a significant increase in total ischemia time and can potentially be a mechanism for worse STEMI outcomes among blacks. In our patient population, blacks as compared to whites had a lower incidence of multivessel coronary artery disease (52.9% vs 62.8%, P=0.001), need for coronary artery bypass graft (6.9% vs 12.0%, P=0.005), and shock (5.4% vs 9.4%, P=0.012) signifying less disease burden in our black population. Despite a lesser disease burden, our black patients had a similar 30‐day mortality compared to white patients (4.8% vs 5.0%, P=0.90) with a trend toward a worse 1‐year mortality (11.9% vs 9.0%, P=0.21).
The ACC/AHA guidelines proposed a goal of 5 minutes from initial symptom onset to activation of the emergency medical system.12 To achieve this, more work is needed to improve patients' understanding of the clinical symptoms and the importance of timely presentation after STEMI. Minority groups are known to have poor educational and health literacy,17 so targeted efforts in these populations need to be intensified to reduce total ischemia time and improve outcomes. Our findings are similar to those obtained from the Get With The Guidelines (GWTG) registry, which found delays to reperfusion among black patients, showing differences in D2BT, but they did not report data on SODT.7 Another study by Sullivan et al reported a median time from symptom onset to 9‐1‐1 calls of 53 minutes.19 They did not find a significant difference in time to activate Emergency Medical Services (EMS) by race in their study, although they stated that a limitation of their study was missing race information on a significant portion of their patients. Although our study did not collect data on the time to EMS activation, their median time to EMS activation more likely translates to a similar SODT as seen in our study. The median D2BT and SODT observed in this study of 60 and 120 minutes also approaches that observed in most contemporary studies.18
The Zwolle Group reported that, after adjustment for baseline characteristics, each 30‐minute delay between the onset of symptoms and balloon inflation was associated with a relative risk of 1‐year mortality of 1.08 (P=0.04).14 Based on these data, a 60‐minute extra delay observed in blacks in our study should translate to a 16% increase in 1‐year mortality. Our study showed only a trend toward a worse 1‐year mortality in blacks, a likely result of the lesser disease burden for this group in our study population.
As expected from observational studies of this nature, ours has some limitations. As a single‐center study, our findings cannot be generalized to the entire country. Also, this study did not collect data on the distance from EMS pick up to hospital; it would have been interesting to see if this also predicted SODT in this population. This data will not detract from our findings and may actually strengthen them, as the hospital is located downtown in an area predominantly occupied by blacks and, despite this, white patients had shorter SODTs. We could not exclude the influences of patients' recall bias of symptom onset, although this is quite unlikely in this study because we extracted data from patients' records documented immediately on arrival in the hospital. Although it is possible that the recognition of symptoms may have differed between blacks and whites, a prior study by Richards et al19 showed that after controlling for pertinent demographic and clinical characteristics, logistic regression analysis revealed that blacks were more likely than whites to have shortness of breath (odds ratio 3.16; 95% CI 1.49–6.71; P=0.003) and left‐sided chest pain (odds ratio 2.55; 95% CI 1.10–5.91; P=0.03), and yet the mean delay time to hospital presentation was not significantly different between the 2 groups in their relatively small study population.
In conclusion, having shown in our STEMI population that parity can be achieved with regard to in‐hospital care between black and white patients presenting with STEMI as reflected in comparable D2BT, our findings suggest that improving outcomes in black patients will entail significant outreach efforts and community education to improve recognition of symptoms, ensure timely request for emergency medical service, and ultimately reduce SODT.
Disclosures
None.
(J Am Heart Assoc. 2016;5:e003804 doi: 10.1161/JAHA.116.003804)
References
- 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Executive summary: heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. [DOI] [PubMed] [Google Scholar]
- 2. Mehta RH, Stebbins A, Lopes RD, Rao SV, Bates ER, Pieper KS, Armstrong PW, Van de Werf F, White HD, Califf RM, Alexander JH, Granger CB. Race, bleeding, and outcomes in STEMI patients treated with fibrinolytic therapy. Am J Med. 2011;124:48–57. [DOI] [PubMed] [Google Scholar]
- 3. Cavender MA, Rassi AN, Fonarow GC, Cannon CP, Peacock WF, Laskey WK, Hernandez AF, Peterson ED, Cox M, Grau‐Sepulveda M, Schwamm LH, Bhatt DL. Relationship of race/ethnicity with door‐to‐balloon time and mortality in patients undergoing primary percutaneous coronary intervention for ST‐elevation myocardial infarction: findings from Get With the Guidelines—Coronary Artery Disease. Clin Cardiol. 2013;36:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Larsen AI, Tomey MI, Mehran R, Nilsen DW, Kirtane AJ, Witzenbichler B, Guagliumi G, Brener SJ, Généreux P, Kornowski R, Dudek D, Gersh BJ, Stone GW. Comparison of outcomes in patients with ST‐segment elevation myocardial infarction discharged on versus not on statin therapy (from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction Trial). Am J Cardiol. 2014;113:1273–1279. [DOI] [PubMed] [Google Scholar]
- 5. Pathak EB, Strom JA. Disparities in use of same‐day percutaneous coronary intervention for patients with ST‐elevation myocardial infarction in Florida, 2001–2005. Am J Cardiol. 2008;102:802–808. [DOI] [PubMed] [Google Scholar]
- 6. Kumar RS, Douglas PS, Peterson ED, Anstrom KJ, Dai D, Brennan JM, Hui PY, Booth ME, Messenger JC, Shaw RE. Effect of race and ethnicity on outcomes with drug‐eluting and bare metal stents: results in 423 965 patients in the linked National Cardiovascular Data Registry and Centers for Medicare & Medicaid Services payer databases. Circulation. 2013;127:1395–1403. [DOI] [PubMed] [Google Scholar]
- 7. Shavelle DM, Chen AY, Matthews RV, Roe MT, de Lemos JA, Jollis J, Thomas JL, French WJ; ACTION‐GWTG Investigators . Predictors of reperfusion delay in patients with ST elevation myocardial infarction self‐transported to the hospital (from the American Heart Association's Mission: Lifeline Program). Am J Cardiol. 2014;113:798–802. [DOI] [PubMed] [Google Scholar]
- 8. Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994–1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. [DOI] [PubMed] [Google Scholar]
- 9. Lambert L, Brown K, Segal E, Brophy J, Rodes‐Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST‐elevation myocardial infarction. JAMA. 2010;303:2148–2155. [DOI] [PubMed] [Google Scholar]
- 10. Vemulapalli S, Zhou Y, Gutberlet M, Kumar AS, Mills JS, Blaxill J, Smalling R, Ohman EM, Patel MR. Importance of total ischemic time and preprocedural infarct‐related artery blood flow in predicting infarct size in patients with anterior wall myocardial infarction (from the CRISP‐AMI Trial). Am J Cardiol. 2013;112:911–917. [DOI] [PubMed] [Google Scholar]
- 11. Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. [DOI] [PubMed] [Google Scholar]
- 12. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:362–425. [DOI] [PubMed] [Google Scholar]
- 13. Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM; National Cardiovascular Data Registry . Association of door‐to‐balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Luca G, Suryapranata H, Zijlstra F, Van‘t Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ; ZWOLLE Myocardial Infarction Study Group . Symptom‐onset‐to‐balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991–997. [DOI] [PubMed] [Google Scholar]
- 15. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. [DOI] [PubMed] [Google Scholar]
- 16. Rollando D, Puggioni E, Robotti S, De Lisi A, Ferrari Bravo M, Vardanega A, Pattaro I, De Benedetti F, Brignole M. Symptom onset‐to‐balloon time and mortality in the first seven years after STEMI treated with primary percutaneous coronary intervention. Heart. 2012;98:1738–1742. [DOI] [PubMed] [Google Scholar]
- 17. Freedman RA, Kouri EM, West DW, Keating NL. Racial/ethnic disparities in knowledge about one's breast cancer characteristics. Cancer. 2015;121:724–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sullivan AL, Beshansky JR, Ruthazer R, Murman DH, Mader TJ, Selker HP. Factors associated with longer time to treatment for patients with suspected acute coronary syndromes: a cohort study. Circ Cardiovasc Qual Outcomes. 2014;7:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Richards SB, Funk M, Milner KA. Differences between blacks and whites with coronary heart disease in initial symptoms and in delay in seeking care. Am J Crit Care. 2000;9:237–244. [PubMed] [Google Scholar]


