Abstract
Background
Recent studies demonstrated that oral anticoagulants (OACs) should be considered for patients with atrial fibrillation and 1 risk factor in addition to sex. Because age is an important determinant of ischemic stroke, the strategy for stroke prevention may be different for these patients in different age strata. The aim of this study was to investigate whether OACs should be considered for patients aged 20 to 49 years with atrial fibrillation and a CHA2DS2‐VASc score of 1 (men) or 2 (women).
Methods and Results
Using the Taiwan National Health Insurance Research Database, 7374 male patients with atrial fibrillation and a CHA2DS2‐VASc score of 1 and 4461 female patients with atrial fibrillation and a CHA2DS2‐VASc score of 2 and all without antithrombotic therapies were identified and stratified into 3 groups by age. The threshold for the initiation of OACs for stroke prevention was set at a stroke rate of 1.7% per year for warfarin and 0.9% per year for non–vitamin K antagonist OACs. Among male patients aged 20 to 49 years with a CHA2DS2‐VASc score of 1, the risk of ischemic stroke was 1.30% per year and ranged from 0.94% per year for those with hypertension to 1.71% for those with congestive heart failure. Among female patients aged 20 to 49 years with a CHA2DS2‐VASc score of 2, the risk of ischemic stroke was 1.40% per year and ranged from 1.11% per year for those with hypertension to 1.67% for those with congestive heart failure.
Conclusions
For atrial fibrillation patients aged 20 to 49 years with 1 risk factor in addition to sex, non–vitamin K antagonist OACs should be considered for stroke prevention to minimize the risk of a potentially fatal or disabling event.
Keywords: age, atrial fibrillation, CHA2DS2‐VASc score, ischemic stroke, non–vitamin K antagonist oral anticoagulants
Subject Categories: Atrial Fibrillation
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and is associated with ≈5‐fold increased risk of ischemic stroke in patients with versus without AF.1 AF‐related stroke is more likely to be fatal, is frequently recurrent, and causes more severe functional disabilities than non–AF‐related stroke.2
The risk of AF‐related stroke is not homogeneous and depends on the age and comorbidities of each patient. Current clinical guidelines suggest the use of CHA2DS2‐VASc score (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age 65–74 years, female sex) for stroke risk stratification, and the use of oral anticoagulants (OACs) is determined accordingly.3, 4 Based on guideline recommendations, OACs should be prescribed for patients with a CHA2DS2‐VASc score ≥2 (class I recommendation) and omitted for male patients with a CHA2DS2‐VASc score of 0 and female patients with a CHA2DS2‐VASc score of 1. For patients with 1 risk factor in addition to sex (ie, CHA2DS2‐VASc score 1 [men] or 2 [women]), the European Society of Cardiology (ESC) guidelines suggest that stroke prevention with OACs should be considered, especially using non–vitamin K antagonist OACs (NOACs).3 Our previous study demonstrated that the annual risk of ischemic stroke was 2.75% for Asian men with AF and a CHA2DS2‐VASc score of 1 and 2.55% for Asian women with AF and a CHA2DS2‐VASc score of 2,5 which exceeds the treatment threshold for the initiation of warfarin (1.7% per year) or use of NOACs (0.9% per year).6
Although these data support the use of OACs for Asians AF patients with a CHA2DS2‐VASc score of 1 (men) or 2 (women), the risk of ischemic stroke for these patients stratified by age has not been studied previously. It is unclear whether OACs should be prescribed for Asian AF patients aged <50 years because data are limited. This study aimed to investigate the risk of ischemic stroke in Asian AF patients with 1 stroke risk factor in addition to sex, stratified by age.
Methods
Database
The study protocol of the present study is similar to that of our previous studies.5, 7, 8, 9, 10, 11 This study used Taiwan's National Health Insurance Research Database (NHIRD), released by the Taiwan National Health Research Institutes. The National Health Insurance (NHI) system is an obligatory nationwide health insurance program that provides comprehensive medical care coverage to all Taiwanese citizens. The NHIRD consists of detailed health care data from >23 million enrollees, representing >99% of Taiwan's residents. In this cohort data set, the patients' original data have been encrypted to protect their privacy, and the encrypting procedure was consistent. Linkage of the claims belonging to the same patient was feasible within the NHI database and can be tracked continuously. The huge sample size of this database provided a good opportunity to study the risk of ischemic stroke in AF patients with a CHA2DS2‐VASc score of 1 (men) or 2 (women), stratified by age.
Study Cohort
From January 1, 1996, to December 31, 2003, a total of 153 036 AF patients aged ≥20 years were identified from the NHIRD as the study population. AF was diagnosed using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) code 427.31. To ensure the accuracy of diagnosis, we defined patients with AF only when it was a discharge diagnosis or was confirmed on at least 2 occasions in the outpatient department. The diagnostic accuracy of AF using this definition in NHIRD has been validated previously.12, 13 The CHA2DS2‐VASc score was calculated for each patient by assigning 1 point each for age between 65 and 74 years, history of hypertension, diabetes mellitus, heart failure, vascular disease (myocardial infarction or peripheral artery disease), and female sex and 2 points each for history of stroke, transient ischemic attack, or age ≥75 years.14 Among the study population, we excluded patients at baseline who received treatment with warfarin or any antiplatelet agent, including aspirin, clopidogrel, dipyridamole, and ticlopidine. Finally, a total of 89 455 patients were enrolled into the study cohort; 12 115 men had a CHA2DS2‐VASc score of 0 to 1, and 7695 women had a CHA2DS2‐VASc score of 1 to 2. A flowchart of the enrollment of the study cohort is shown in Figure 1.
Figure 1.
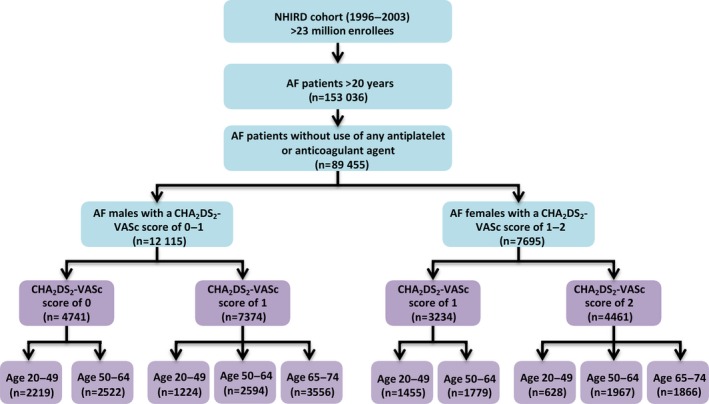
A flowchart of the enrollment of the study cohort. Among 89 455 AF patients who did not receive oral anticoagulants or antiplatelet agents, there were 12 115 male AF patients with a CHA2DS2‐VASc score of 0 to 1 and 7695 female AF patients with a CHA2DS2‐VASc score of 1 to 2. The risk of ischemic stroke was analyzed for these patients and further stratified on the basis of age. AF indicates atrial fibrillation; NHIRD, National Health Insurance Research Database.
Definition of Clinical End Points
The clinical end point was the occurrence of ischemic stroke (ICD‐9‐CM codes 433.x, 434.x, 436), with concomitant imaging studies of the brain, such as computed tomography or magnetic resonance imaging. The accuracy of diagnosis of ischemic stroke in Taiwan's NHIRD has been reported to be ≈94%.15 Another validation study also demonstrated that the diagnostic accuracy of ischemic stroke in NHIRD was high, with a positive predictive value and sensitivity of 88.4% and 97.3%, respectively.16 The annual risk of ischemic stroke was calculated for patients who were stratified into 3 groups based on age (20–49, 50–64, and 65–74 years).
The “Tipping Point” for OAC Use for Stroke Prevention
In an analysis of the “tipping point” for OAC use for stroke prevention using a decision analytic model, Eckman et al estimated thresholds for ischemic stroke risk below which OAC therapy should be withheld and above which OAC therapy should be prescribed.6 Their results demonstrated that anticoagulation with warfarin is preferred at a stroke rate of >1.7% per year, whereas anticoagulation with the safer NOACs leads to lowering of the treatment threshold for anticoagulation to a stroke rate of 0.9% per year.6 Consequently, patients with an annual risk of ischemic stroke >0.9% in our study cohort were assumed to be candidates for NOAC use for stroke prevention. For patients with an annual risk of ischemic stroke >1.7%, OACs with either warfarin or NOACs could be considered.
Statistical Analysis
Incidence rates of ischemic stroke were calculated by dividing the number of events by person‐time at risk. The risk of ischemic stroke was assessed using Cox regression analysis.
The present study was approved by the institutional review board of Taipei Veterans General Hospital, Taipei, Taiwan, and informed consent of study participants was waived.
Results
Table 1 shows the number of ischemic strokes per 100 person‐years for AF patients with a CHA2DS2‐VASc score of 0 to 1 (men) or 1 to 2 (women) and stratified by age. The number of ischemic strokes per 100 person‐years for patients aged 20 to 49 and 50 to 64 years who did not have any risk factors other than sex (ie, CHA2DS2‐VASc 0 in men, 1 in women) were 0.63 and 1.96, respectively. For patients with 1 risk factor in addition to sex (ie, CHA2DS2‐VASc 1 for men, 2 for women), the numbers of ischemic strokes per 100 person‐years were 1.33 for patients aged 20 to 49 years, 2.90 for those aged 50 to 64 years, and 3.60 for those aged 65 to 74 years. Among patients aged 20 to 49 years, the number of ischemic strokes per 100 person‐years ranged from 1.00 for those with hypertension to 1.69 for those with congestive heart failure.
Table 1.
Risk of Ischemic Stroke in AF Patients With a CHA2DS2‐VASc Score of 0 to 1 (Men) or 1 to 2 (Women), Stratified by Age
| Age Groups | CHA2DS2‐VASc Score | Number of Patients | Number of Ischemic Strokes | Person‐Years | Incidencea |
|---|---|---|---|---|---|
| All patients | |||||
| Age 20–49 years | No risk factors in addition to sex (score 0 for men or 1 for women) | 3674 | 234 | 36 942.2 | 0.63 |
| Sex plus 1 additional risk factor (score 1 for men or 2 for women) | 1852 | 211 | 15 838.9 | 1.33 | |
| Congestive heart failure | 766 | 99 | 5843.3 | 1.69 | |
| Hypertension | 705 | 66 | 6614.3 | 1.00 | |
| Diabetes mellitus | 224 | 30 | 1891.1 | 1.59 | |
| Vascular disease | 157 | 16 | 1490.3 | 1.07 | |
| Age 50–64 years | No risk factors in addition to sex (score 0 for men or 1 for women) | 4301 | 729 | 37 265.0 | 1.96 |
| Sex plus 1 additional risk factor (score 1 [men] or 2 [women) | 4561 | 1014 | 34 912.9 | 2.90 | |
| Congestive heart failure | 1350 | 268 | 9535.9 | 2.81 | |
| Hypertension | 2230 | 517 | 18 425.5 | 2.81 | |
| Diabetes mellitus | 679 | 178 | 4317.2 | 4.12 | |
| Vascular disease | 302 | 51 | 2634.2 | 1.94 | |
| Age 65–74 years | Score 1 (men) or 2 (women) | 5422 | 1214 | 33 727.0 | 3.60 |
Number of ischemic strokes per 100 person‐years of follow‐up. AF indicates atrial fibrillation.
Table 2 shows the number of ischemic strokes per 100 person‐years for male AF patients with a CHA2DS2‐VASc score of 0 to 1, stratified by age. Among male patients aged 20 to 49 years with a CHA2DS2‐VASc score of 1, the number of ischemic strokes per 100 person‐years was 1.30, ranging from 0.94 for those with hypertension to 1.71 for those with congestive heart failure.
Table 2.
Risk of Ischemic Stroke in Men With AF and a CHA2DS2‐VASc Score of 0 or 1, Stratified by Age
| Age Groups | CHA2DS2‐VASc Score | Number of Patients | Number of Ischemic Strokes | Person‐Years | Incidencea |
|---|---|---|---|---|---|
| Age 20–49 years | No risk factors in addition to sex (score 0) | 2219 | 119 | 21 888.9 | 0.54 |
| Sex plus 1 additional risk factor (score 1) | 1224 | 134 | 10 328.0 | 1.30 | |
| Congestive heart failure | 474 | 60 | 3511.9 | 1.71 | |
| Hypertension | 485 | 42 | 4459.2 | 0.94 | |
| Diabetes mellitus | 156 | 21 | 1268.3 | 1.66 | |
| Vascular disease | 109 | 11 | 1088.6 | 1.01 | |
| Age 50–64 years | No risk factors in addition to sex (score 0) | 2522 | 434 | 20 799.9 | 2.09 |
| Sex plus 1 additional risk factor (score 1) | 2594 | 584 | 18 655.0 | 3.13 | |
| Congestive heart failure | 791 | 154 | 5312.9 | 2.90 | |
| Hypertension | 1233 | 301 | 9574.2 | 3.14 | |
| Diabetes mellitus | 392 | 99 | 2310.8 | 4.28 | |
| Vascular disease | 178 | 30 | 1457.1 | 2.06 | |
| Age 65–74 years | Score 1 | 3556 | 764 | 20 737.0 | 3.68 |
Number of ischemic strokes per 100 person‐years of follow‐up. AF indicates atrial fibrillation.
Table 3 shows the number of ischemic strokes per 100 person‐years for female AF patients with a CHA2DS2‐VASc score of 1 to 2, stratified by age. Among female patients aged 20 to 49 years with a CHA2DS2‐VASc score of 2, the number of ischemic strokes per 100 person‐years was 1.40 and ranged from 1.11 for those with hypertension to 1.67 for those with congestive heart failure.
Table 3.
Risk of Ischemic Stroke in Women With AF and a CHA2DS2‐VASc Score of 1 or 2, Stratified by Age
| Age Groups | CHA2DS2‐VASc Score | Number of Patients | Number of Ischemic Strokes | Person‐Years | Incidencea |
|---|---|---|---|---|---|
| Age 20–49 years | No risk factors in addition to sex (score 1) | 1455 | 115 | 15 053.3 | 0.76 |
| Sex plus 1 additional risk factor (score 2) | 628 | 77 | 5510.9 | 1.40 | |
| Congestive heart failure | 292 | 39 | 2331.3 | 1.67 | |
| Hypertension | 220 | 24 | 2155.1 | 1.11 | |
| Diabetes mellitus | 68 | 9 | 622.8 | 1.45 | |
| Vascular disease | 48 | 5 | 401.7 | 1.24 | |
| Age 50–64 years | No risk factors in addition to sex (score 1) | 1779 | 295 | 16 465.1 | 1.79 |
| Sex plus 1 additional risk factor (score 2) | 1967 | 430 | 16 257.9 | 2.64 | |
| Congestive heart failure | 559 | 114 | 4223.0 | 2.70 | |
| Hypertension | 997 | 216 | 8851.4 | 2.44 | |
| Diabetes mellitus | 287 | 79 | 2006.4 | 3.94 | |
| Vascular disease | 124 | 21 | 1177.1 | 1.78 | |
| Age 65–74 years | Score 2 | 1866 | 450 | 12 989.9 | 3.46 |
Number of ischemic strokes per 100 person‐years of follow‐up. AF indicates atrial fibrillation.
Figure 2 shows the risk of ischemic stroke represented by hazard ratios for each risk factor component stratified by age. Among patients aged 20 to 49 years, the hazard ratios ranged from 1.59 for patients with hypertension to 2.67 for those with congestive heart failure.
Figure 2.
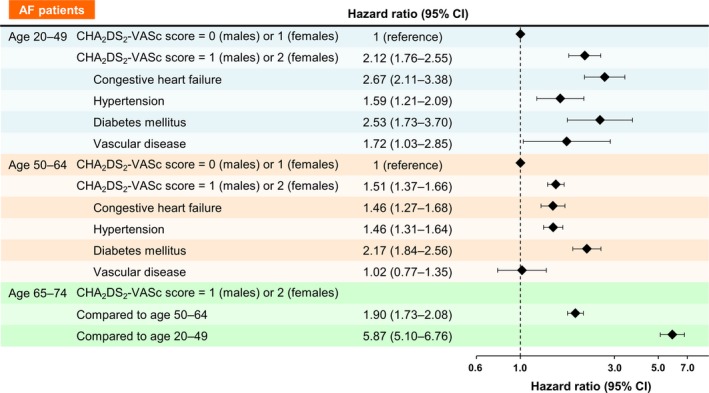
Risk of ischemic stroke represented by hazard ratios for each risk factor component stratified by age. Among patients aged 20 to 49 years, the hazard ratios ranged from 1.59 for patients with hypertension to 2.67 for those with congestive heart failure compared with patients with a CHA2DS2‐VASc score of 0 (men) or 1 (women). AF indicates atrial fibrillation.
Discussion
In this real‐world nationwide cohort study of nonanticoagulated Taiwanese AF patients, we demonstrated that AF patients with 1 risk factor in addition to sex (CHA2DS2‐VASc score 1 for men and 2 for women) had an ischemic stroke rate of 1.33% for patients aged 20 to 49 years, 2.90% for those aged 50 to 64 years, and 3.60% for those aged 65 to 74 years. Consequently, AF patients with 1 risk factor in addition to sex who are aged <50 years should still be considered for stroke prevention using OACs because the annual risk of ischemic stroke (1.33%) was above the tipping point for the use of NOACs (0.9% per year). This approach could minimize the risk of a potentially fatal or disabling thromboembolic event and the public health burden of stroke related to AF.
Stroke Prevention for AF Patients With 1 Risk Factor in Addition to Sex
The 2012 focused update of the ESC AF management guidelines suggested that OACs should be prescribed for AF patients with 1 risk factor in addition to sex.3 Recommendations for these patients were less clear in the 2014 American College of Cardiology and American Heart Association AF guidelines, which suggested that “no antithrombotic therapy, aspirin or an OAC” be considered (class IIb recommendation).4 Numerous registry studies and randomized trials suggested that the risk of ischemic stroke is higher for Asian compared with non‐Asian AF patients.8, 17, 18, 19, 20 We showed, for example, that the annual risk of ischemic stroke was 2.75% for Asian men with AF and a CHA2DS2‐VASc score of 1 and 2.55% for Asian women with AF and a CHA2DS2‐VASc score of 25; therefore, these patients should receive OACs for stroke prevention, given the greater mortality and disability for AF‐related strokes.
Age is an important driver of ischemic stroke risk for AF patients, and the risk of ischemic stroke substantially increases for Asian AF patients aged >50 years.9 Whether OACs should be prescribed for AF patients with a CHA2DS2‐VASc score of 1 (men) or 2 (women) who are aged <50 years is unclear because data are limited, and few such patients were included in clinical trials. In the present study, we demonstrated that the annual risks of ischemic stroke were 1.30% and 1.40% for men and women, respectively, aged 20 to 49 years. Because the proposed treatment thresholds for balancing ischemic stroke reduction against serious bleeding were 1.7% per year for the use of warfarin and 0.9% per year for the use of NOACs,6 stroke prevention using NOACs should be considered for these patients.
As in previous studies, not all risk factors in the CHA2DS2‐VASc score were associated with equal risks of ischemic stroke19, 21; therefore, the annual stroke risk was not the same for our patients aged 20 to 49 years with a CHA2DS2‐VASc score of 1 (men) or 2 (women) and different risk components. The stroke risks were relatively higher for patients with heart failure (1.69% per year) and lower for those with hypertension (1.00% per year). Event rates for 1 stroke risk factor have varied in different studies because of different methodologies and study settings19; however, exclusion of OAC use at any time, even during follow‐up, has resulted in bias from “conditioning on the future” toward lower stroke event rates.22, 23 Because the annual risks of ischemic stroke for male patients aged 20 to 49 years with a CHA2DS2‐VASc score of 1 due to hypertension (0.94%) or vascular disease (1.01%) in the present study were just slightly higher than the treatment threshold for using NOACs (0.9% per year), treatment of these patients in this “gray zone” should be based on shared decision making regarding the risks and benefits of OACs.
Study Limitations
Several limitations of the present study were addressed previously.5, 7, 8, 9, 10, 11 First, the diagnosis of AF and the occurrence of ischemic stroke were based on the diagnostic codes registered by the physicians responsible for the treatment of patients; nonetheless, the accuracy of the diagnosis of AF and ischemic stroke in Taiwan's NHIRD has been validated previously as high.12, 13, 15, 16 We defined patients as having AF only when it was a discharge diagnosis or was confirmed on at least 2 occasions in the outpatient department. To ensure the diagnostic accuracy of AF, patients having AF coding only 1 time at the outpatient clinic were not enrolled. Nevertheless, compared with patients coded with AF only 1 time, patients coded with AF more times might have had longer AF duration and higher AF burden, which could increase stroke risk. Second, the clinical end point of the present study included only ischemic stroke and did not account for transient ischemic attack and other systemic thromboembolism. Because the event rate of the study population could be even higher if transient ischemic attack and other systemic thromboembolic events were included, that would further support the main finding of the present study showing that NOACs should be considered for Asian AF patients aged 20 to 49 years with 1 risk factor in addition to sex. Third, detailed information about personal habits, symptoms, and cardiac function were unavailable in the registry database. Fourth, many young AF patients would have received various treatments (eg, rate/rhythm control, ablation) to relieve their symptoms, and this may have influenced event rates. Last, the present study enrolled only Asian patients, and it remains uncertain whether the results can be extrapolated to other populations. Moreover, the data from which the tipping points were derived for the initiation of OACs were acquired in studies that consisted mainly of white patients; therefore, the treatment thresholds may be different for Asian patients.
Conclusion
For Asian AF patients aged 20 to 49 years with 1 risk factor in addition to sex and a CHA2DS2‐VASc score of 1 (men) or 2 (women), NOACs should be considered for stroke prevention to minimize the risk of a potentially fatal or disabling event. A treatment threshold gray zone exists for male patients aged 20 to 49 years with a CHA2DS2‐VASc score of 1 because of hypertension or vascular diseases; the annual risks of stroke for these patients were just slightly higher than the tipping point for using NOACs. Treatment should be based on shared decision making with patients regarding the risks and benefits of OACs.
Sources of Funding
This work was supported in part by grants from the Ministry of Science and Technology (MOST 104‐2314‐B‐075‐024‐MY3), and Taipei Veterans General Hospital (V100D‐002‐3, V101D‐001‐2, V102B‐025, V103B‐018, and V105B‐023).
Disclosures
Lip has served as a consultant for Bayer/Janssen, Astellas, Merck, Sanofi, BMS/Pfizer, Biotronik, Medtronic, Portola, Boehringer Ingelheim, Microlife and Daiichi‐Sankyo; and speaker for Bayer, BMS/Pfizer, Medtronic, Boehringer Ingelheim, Microlife, Roche and Daiichi‐Sankyo.
(J Am Heart Assoc. 2016;5:e003839 doi: 10.1161/JAHA.116.003839)
References
- 1. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. [DOI] [PubMed] [Google Scholar]
- 2. Lin HJ, Wolf PA, Kelly‐Hayes M, Beiser AS, Kase CS, Benjamin EJ, D'Agostino RB. Stroke severity in atrial fibrillation. The Framingham Study. Stroke. 1996;27:1760–1764. [DOI] [PubMed] [Google Scholar]
- 3. Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P; Guidelines ESCCfP . 2012 Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719–2747. [DOI] [PubMed] [Google Scholar]
- 4. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW; Members AATF . 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:e199–e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chao TF, Liu CJ, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chen TJ, Lip GY, Chen SA. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2‐VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol. 2015;65:635–642. [DOI] [PubMed] [Google Scholar]
- 6. Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: the decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2011;4:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chao TF, Liu CJ, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chen TJ, Lip GY, Chen SA. Using the CHA2DS2‐VASc score for refining stroke risk stratification in ‘low‐risk’ Asian patients with atrial fibrillation. J Am Coll Cardiol. 2014;64:1658–1665. [DOI] [PubMed] [Google Scholar]
- 8. Chao TF, Liu CJ, Tuan TC, Chen SJ, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Chen TJ, Chiang CE, Chen SA. Comparisons of CHADS2 and CHA2DS2‐VASc scores for stroke risk stratification in atrial fibrillation: which scoring system should be used for Asians? Heart Rhythm. 2016;13:46–53. [DOI] [PubMed] [Google Scholar]
- 9. Chao TF, Wang KL, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chung FP, Liao JN, Chen TJ, Chiang CE, Lip GY, Chen SA. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015;66:1339–1347. [DOI] [PubMed] [Google Scholar]
- 10. Chao TF, Liu CJ, Tuan TC, Chen SJ, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Chen TJ, Chiang CE, Chen SA. Rate‐control treatment and mortality in atrial fibrillation. Circulation. 2015;132:1604–1612. [DOI] [PubMed] [Google Scholar]
- 11. Chao TF, Liu CJ, Liao JN, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chung FP, Chen TJ, Lip GY, Chen SA. Use of Oral Anticoagulants for Stroke Prevention in Patients With Atrial Fibrillation Who Have a History of Intracranial Hemorrhage. Circulation. 2016;133:1540–1547. [DOI] [PubMed] [Google Scholar]
- 12. Lin LJ, Cheng MH, Lee CH, Wung DC, Cheng CL, Kao Yang YH. Compliance with antithrombotic prescribing guidelines for patients with atrial fibrillation–a nationwide descriptive study in Taiwan. Clin Ther. 2008;30:1726–1736. [DOI] [PubMed] [Google Scholar]
- 13. Chang CH, Lee YC, Tsai CT, Chang SN, Chung YH, Lin MS, Lin JW, Lai MS. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis. 2014;232:224–230. [DOI] [PubMed] [Google Scholar]
- 14. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. [DOI] [PubMed] [Google Scholar]
- 15. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20:236–242. [DOI] [PubMed] [Google Scholar]
- 16. Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 2015;114:254–259. [DOI] [PubMed] [Google Scholar]
- 17. Siu CW, Lip GY, Lam KF, Tse HF. Risk of stroke and intracranial hemorrhage in 9727 Chinese with atrial fibrillation in Hong Kong. Heart Rhythm. 2014;11:1401–1408. [DOI] [PubMed] [Google Scholar]
- 18. Chiang CE, Wang KL, Lip GY. Stroke prevention in atrial fibrillation: an Asian perspective. Thromb Haemost. 2014;111:789–797. [DOI] [PubMed] [Google Scholar]
- 19. Nielsen PB, Chao TF. The risks of risk scores for stroke risk assessment in atrial fibrillation. Thromb Haemost. 2015;113:1170–1173. [DOI] [PubMed] [Google Scholar]
- 20. Siu CW. One more “C” for CHA2DS2‐VASc score? J Am Coll Cardiol. 2015;65:1602–1603. [DOI] [PubMed] [Google Scholar]
- 21. Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH, Torp‐Pedersen C. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Friberg L, Skeppholm M, Terent A. Benefit of anticoagulation unlikely in patients with atrial fibrillation and a CHA2DS2‐VASc score of 1. J Am Coll Cardiol. 2015;65:225–232. [DOI] [PubMed] [Google Scholar]
- 23. Chan YH, Wu LS, Chang SH, Lee HF, Liu JR, See LC, Yeh YH, Kuo CT. Young male patients with atrial fibrillation and CHA2DS2‐VASc score of 1 may not need anticoagulants: a nationwide population based study. PLoS One. 2016;11:e0151485. [DOI] [PMC free article] [PubMed] [Google Scholar]


