Abstract
Introduction
Low-intensity shockwave therapy (LISWT) has recently emerged as a promising method in the treatment of erectile dysfunction (ED).
Aim
To assess the long-term results of the effectiveness and safety of LISWT in patients with ED who are non-responders to phosphodiesterase type 5 inhibitor (PDE5i) treatment.
Methods
This open-label, longitudinal, and observational study investigated an uncontrolled population of 50 consecutive patients whose ED was unresponsive to PDE5i treatment. Patients were treated with a four-session LISWT protocol. During active treatment and follow-up, all patients remained on their regular high on-demand or once-daily PDE5i dosing schedules.
Main Outcome Measures
Effectiveness was assessed according to the International Index of Erectile Function erectile function domain, questions 2 and 3 of the Sexual Encounter Profile, Erection Hardness Scale, and Global Assessment Question scores at baseline and at 3, 6, 9, and 12 months after treatment. Patients were considered responders whenever they showed improvement in erection parameters in all four assessments and responded positively to the Global Assessment Question. Adverse events were recorded. Statistical variables were applied and findings were considered statistically significant at a P value less than < .05.
Results
Eighty percent (mean age = 64.8 years) completed the 12-month follow-up. Positive response rates were 60% of available subjects at the end of the study and 48% of the intent-to-treat population. After the 12-month follow-up, 91.7% of responders maintained their responses. No patient reported treatment-related adverse events.
Conclusion
LISWT in patients with ED unresponsive to PDE5i treatment was effective and safe in 60% of patients treated. The efficacy response was maintained for 12 months in most patients.
Key Words: Low-Intensity Extracorporeal Shockwave Therapy, Erectile Dysfunction, Phosphodiesterase Type 5 Inhibitor
Introduction
Erectile dysfunction (ED) is a medical entity that is highly prevalent in men older than 50 years whose history of vascular risk factors (VRFs) has been a common denominator in the origin of this symptom.1
Many studies have stressed the status of ED as a potential indicator of cardiovascular disease, although other clinical trials have found a high incidence of ED in men with VRFs such as metabolic syndrome, diabetes, and hypertension.2, 3
Since 1998, the phosphodiesterase type 5 inhibitor (PDE5i) has introduced a change in the treatment paradigm for patients with ED because approximately 60% of patients can recover their erectile function and lead a satisfactory sex life.4
Despite the effectiveness of PDE5i in the treatment of ED, 40% to 50% of patients—depending on the etiology of the dysfunction—do not respond to this drug therapy, even after optimization approaches such as treatment combinations have been implemented.5, 6, 7, 8, 9, 10
For some years, low-intensity shockwave therapy (LISWT) has been implemented for the treatment of ED and to optimize the response to PDE5i.
A shockwave is a wave of abrupt pressure (vibration movement) produced by an object that travels faster than the speed of sound (<10 ns) producing external pressure differences and increased temperature.11
Since the 1980s, shockwaves of different intensities have been used therapeutically in medicine. High-intensity shockwaves (pressure = 450 bar) have been implemented in the treatment of urolithiasis, medium-intensity shockwaves (pressure = 200 bar) in the treatment of arthralgia, tendinitis, and bursitis, and more recently LISWT (pressure = 80 bar) in the treatment of ED.
Young and Dyson12 discovered that therapeutic ultrasound encourages angiogenesis by enhancing the expression of vascular endothelial growth factor. Nurzynska et al13 reported that shockwaves have a positive influence on the proliferation and differentiation of cardiomyocytes, smooth muscle, and endothelial cell precursors, with a more obvious effect in cells from a normal heart than from a pathologic heart.
After these initial reports, LISWT was implemented in the treatment of chronic myocardial ischemia and diabetic foot ulcers, among other applications.14, 15, 16, 17, 18
The idea of applying LISWT to the penis stemmed from a study with animals that proved that the energy of shockwaves applied to the myocardium of pigs ameliorates ischemia-induced myocardial dysfunction.14 By extrapolating these findings to ED, it was presumed that shockwaves applied to the penis might increase blood flow and improve endothelial function through the stimulation of angiogenesis in the corpus cavernosum.
The mechanism of action is still not completely elucidated. However, low-intensity energy has been shown to induce the production of a physiologically significant amount of non-enzymatic nitric oxide and activate intracellular cascade pathways that trigger the release of angiogenic factors.19
In this way, shockwaves produce mechanic stress and microtrauma at the cellular level, thus generating a series of biological cascades that favor the release of angiogenic factors leading to neovascularization.
In vivo and in vitro evidences have proved that shockwaves enhance the expression of growth factors related to angiogenesis, increase mRNA and vascular endothelial growth factor cellular levels and its receptor, Flt-1, induce neovascularization, increase blood supply, and significantly increase angiogenic markers.14, 15, 16, 17
In that regard, Qiu et al20 found that shockwave therapy significantly restored erectile function in rats with streptozotocin-induced diabetes mellitus to levels similar to those exhibited by healthy controls, thus validating the animal model as comparable to prior clinical trials performed in humans. According to trial results, improvements in erectile function might be attributable to the positive effects afforded by the shockwaves on endothelial and smooth muscle regeneration in the penis. These effects appear to be mediated by the recruitment of endogenous smooth muscle cells.
Interestingly, the results recently published by Assaly-Kaddoum et al21 showed that LISWT significantly improved erectile function in Goto-Kakizaki rats to the same extent as sildenafil. Furthermore, the effects of LISWT were potentiated with sildenafil. Nevertheless, this was not mediated by a mechanism dependent on nitric oxide and cyclic guanosine monophosphate and the investigators encouraged further investigation of the mechanism of action of these devices.
The first observation studies in patients who responded poorly to PDE5i therapy reported on the efficacy and safety of LISWT devices, especially in patients with ED of vascular origin and in those with a poor response to PDE5i treatment.22, 23
Recently, Kitrey et al24 performed a sham-controlled evaluation of penile LISWT effect in 58 patients unable to achieve sexual intercourse using a PDE5i. In the LISWT and sham groups, 54.1% and 0% of patients, respectively, achieved an erection hard enough for vaginal penetration. According to changes in the International Index of Erectile Function erectile function domain (IIEF-EF) score, treatment was effective in 40.5% of men who received LISWT but in none in the sham group.
Aim
Based on these findings, the aim of this study was to assess the effectiveness and safety of LISWT after 12 months in the treatment of ED in patients with a history of vascular disease or associated VRFs with a low response to PDE5i treatment.
Methods
This study was an open-label, longitudinal, observational, and independent study designed to evaluate the safety and efficacy of LISWT in an uncontrolled population of sexually active men with ED unresponsive to PDE5i treatment and associated VRFs.
This study consisted of a screening phase, a treatment phase, and a 12-month follow-up phase. At the screening phase, patients had an extensive medical and sexological history evaluation and a physical examination.
The inclusion criteria involved sexually active men with ED that was unresponsive to PDE5i treatment and exhibited VRFs (eg, diabetes, hypertension, dyslipidemia, and coronary artery disease). Patients with untreated hypogonadism or a history of pelvic surgery and patients with ED of neurologic origin (resulting from prostatectomy, pelvic surgery, or spinal cord injury) were excluded.
Patients were considered non-responders to PDE5i if they, after completing all optimization measures commonly suggested (correct dose optimization of PDE5i, correction of risk factors, improvement in sexual stimuli, correction of testosterone levels, and proper patient dietary training, especially with the use of short-acting PDE5i), had an IIEF-EF score lower than 26 points when using these drugs.10, 11
Fifty consecutive patients with ED fulfilled the inclusion criteria and accepted the invitation to participate. During LISWT and follow-up, these patients continued with PDE5i treatment at the maximum dose or with a daily dose under the same treatment protocol. Only those patients who completed the 12-month follow-up were considered for result analysis.
Severity of ED was classified into five categories according to the IIEF-EF score.25
The following evaluation criteria were used: IIEF-EF to assess ED severity, questions 2 and 3 from the Sexual Encounter Profile (SEP2 and SEP3) to assess penetration and erection sustainability, the Erection Hardness Score (EHS), and a Global Assessment Question (GAQ): Has the treatment improved the quality of your erections?26, 27, 28, 29
Improvement of the IIEF-EF score was defined as an increase from baseline to follow-up (12 months after treatment) according to the minimal clinically differences suggested by Rosen et al.30
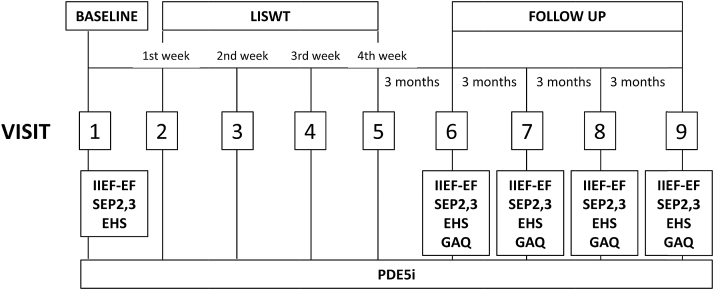
The criterion for treatment success according to the EHS was a score of 3 or 4. Assessment measurements were taken face to face before treatment and 3, 6, 9, and 12 months after LISWT completion (Figure 1).
Figure 1.
Study flowchart. EHS = Erection Hardness Scale; GAQ = Global Assessment Question; IIEF-EF = International Index of Erectile Function erectile function domain; LISWT = low-intensity shockwave therapy; SEP2 and 3 = questions 2 and 3 of Sexual Encounter Profile.
Patients were considered responders to LISWT whenever they showed improvement in erection parameters in all four assessments (IIEF-EF, SEP2, SEP3, and EHS) and responded positively to the GAQ at 3, 6, 9, and 12 months after treatment. Adverse events were recorded.
This trial was performed using Renova, an extracorporeal LISWT device (Direx Argentina, Buenos Aires, Argentina). This equipment uses linear shockwaves and, unlike previous models, spans the entire area of the organ (up to 70 mm) and thus can apply shockwaves with greater precision at the penile crura and corpus cavernosum.31
The subjects started the treatment right after inclusion in the study because they continued their respective current PDE5i therapies.
According to previously published studies, the treatment consisted of applying 14,400 shockwaves during a period of 4 weeks. In each session, the patient received 3,600 shockwaves of 0.09 mJ/mm2: 1,800 were applied to the penis (900 to each corpus cavernosum) and 1,800 were applied to the perineum (900 to each crus). The areas that received treatment were the same at each session. All sessions were performed without anesthesia in an outpatient setting and each lasted 20 minutes.31
The study was conducted according to Good Clinical Practices and the Declaration of Helsinki, it was approved by the local research ethics committee, and all patients signed an informed consent form.
Variables of demographic characteristics of responders and non-responders were calculated using the Mann-Whitney test and Fisher exact test. Efficacy variables were assessed using the Friedman test, and individual comparisons were assessed with the Bonferroni-Dunn method. Statistical variables were applied and findings were considered statistically significant at a P value less than .05.
Main Outcome Measures
Effectiveness was assessed using the IIEF-EF, SEP2 and SEP3 diaries, EHS, and GAQ at baseline and at 3, 6, 9, and 12 months after treatment.
Results
Eighty percent of patients (40 of 50) completed the treatment and 12-month follow-up. Ten patients with similar demographic characteristics were excluded from the study because of loss to the first follow-up.
Median age was 64.8 years and duration of ED was 70.5 months.
The positive response rate was 60% of available subjects at the end of the study and 48% of the intent-to-treat population.
Sixty percent of patients (24 of 40) showed improvement in efficacy parameters in all four assessments (IIEF-EF, SEP2, SEP3, and EHS) and responded positively to the GAQ. These changes were significant from the first follow-up (3 months after treatment).
By the third month after treatment, 91.7% of responders to LISWT (22 of 24) maintained efficacy parameters up to the last follow-up visit 12 months after treatment.
No statistically significant difference was found for age, duration of ED, comorbidities, and dysfunction severity when comparing responders to LISWT (24 of 40) with non-responders to LISWT (16 of 40; Table 1).
Table 1.
Demographic characteristics of patients (responders and non-responders to low-intensity shockwave therapy)
| Responders (n = 24) | Non-responders (n = 16) | P value | |
|---|---|---|---|
| Age (y), mean (range) | 65 (50–82) | 64.4 (48–82) | .8902∗ |
| Duration of ED (mo) | 64.4 | 77.8 | .4385∗ |
| Range (mo) | 12–132 | 8–120 | |
| Vascular risk factors, n (%) | |||
| Hypertension | 14 (58.3) | 11 (68.8) | .7397† |
| Diabetes mellitus | 3 (12.5) | 7 (43.8) | .0588† |
| Dyslipidemia | 11 (45.8) | 9 (56.3) | .7475† |
| Coronary artery disease | 10 (41.7) | 7 (43.8) | .9999† |
| Severity of ED according to IIEF, n (%) | |||
| Severe | 4 (16.7) | 6 (37.5) | .1592† |
| Moderate | 12 (50) | 4 (25) | .1881† |
| Mild to moderate | 4 (16.7) | 4 (25) | .6905† |
| Mild | 4 (16.7) | 2 (12.5) | .9999† |
ED = erectile dysfunction; IIEF = International index of Erectile Dysfunction.
Mann-Whitney test.
Fisher exact test.
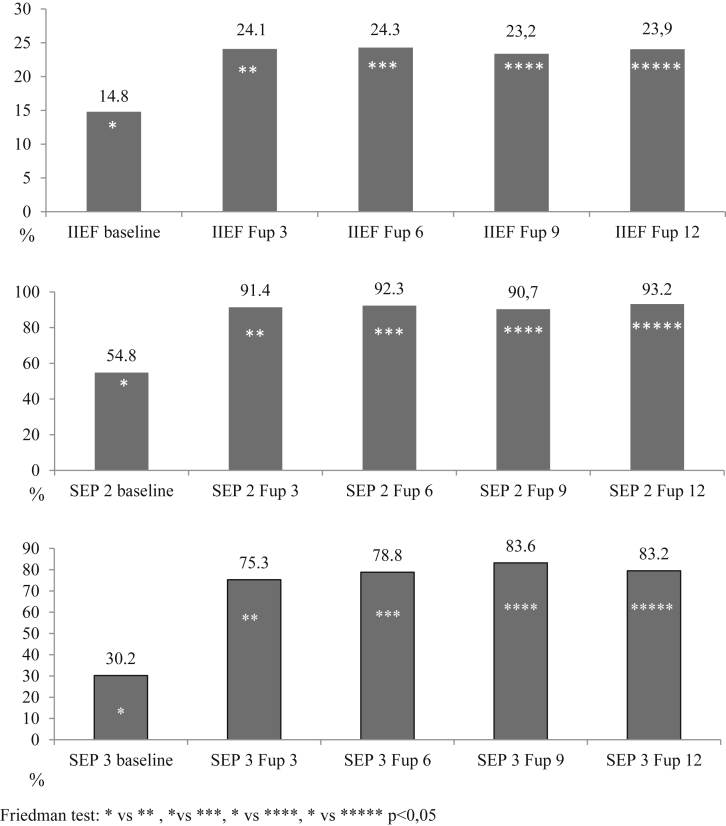
In responders to LISWT, the increase in results obtained through the IIEF-EF score was statistically significant from the 3-month assessment after treatment, reaching a mean of 9.3 points and of 9.1 points by 12 months after treatment (Figure 2).
Figure 2.
Evolution of changes in IIEF-EF score, SEP2, and SEP3 in responders to LISWT (n = 24). P < 0.05 by Friedman test (∗baseline vs ∗∗Fup 3, vs ∗∗∗Fup 6, vs ∗∗∗∗Fup 9, vs ∗∗∗∗∗Fup 12). Fup 3 = 3-month follow-up; Fup 6 = 6-month follow-up; Fup 9 = 9-month follow-up; Fup 12 = 12-month follow-up; IIEF-EF = International Index of Erectile Function erectile function domain; SEP2 and 3 = questions 2 and 3 of the Sexual Encounter Profile.
From 3 months after treatment to the end of follow-up monitoring, significant changes were encountered in the responder group for the EHS and SEP2 and SEP3, with a response rate of almost 80% of attempts (Figure 2).
Improvements in the IIEF-EF score were higher whenever ED was more severe, with changes of 13, 10.5, 6.8, and 4.5 points for patients with severe, moderate, mild to moderate, and mild ED, respectively (Table 2).
Table 2.
IIEF-6 changes according to severity of ED before and 12 months after treatment with shockwaves of low intensity
| ED severity | n | Baseline IIEF-6 score, mean ± SD | Follow-up 12-mo IIEF-6 score, mean ± SD | IIEF-6 improvement points | P value |
|---|---|---|---|---|---|
| Severe | 4 | 9 ± 1.155 | 22 ± 3.651 | 13 | .029 |
| Moderate | 12 | 12.8 ± 1.328 | 23.3 ± 4.619 | 10.9 | .0001 |
| Mild to moderate | 4 | 18.5 ± 1.291 | 25.3 ± 4.113 | 6.8 | .002 |
| Mild | 4 | 22.8 ± 0.500 | 26.3 ± 4.193 | 4.5 | .3429 |
| Total | 24 | 14.7 ± 4.757 | 23.9 ± 4.303 | 9.2 | .0001 |
ED = erectile dysfunction; IIEF-6 = International index of Erectile Dysfunction.
Thirteen patients reached a score of at least 26 points in the IIEF-EF score, and the degree of severity decreased in nine and remained unchanged in two.
Discussion
This study evaluated a group of patients with ED and associated VFRs who responded poorly to PDE5i therapy in a 12-month pilot study. Erectile function was recovered in 60% of patients after treatment with linear-focused LISWT.
Most randomized, double-blinded, sham-control trials have reported the efficacy of LISWT in patients with ED.32, 33, 34
Vardi et al32 presented the first randomized, double-blinded, sham-control trial that demonstrated that LISWT had a positive short-term clinical and physiologic effect on the erectile function of men who respond to oral PDE5i therapy. They found a significantly greater increase in the IIEF-EF score in the treated group than in the sham-treated group. In addition, physiologic penile hemodynamic significantly improved in the treated group but not in the sham group (maximal postischemic penile blood flow = 8.2 vs 0.1 mL/[min · dL], P < .0001) assessed using plethysmography.
However, Yee et al,33 using a similar treatment scheme to the one used in the study by Vardi et al32 and implementing the same shockwave therapy system (Omnispec ED1000; Medispec Ltd, Germantown, MD, USA), did not find significant statistical evidence in the IIEF score and EHS score in a group of 28 patients under LISWT treatment compared with a sham-treated group of 30 patients. Nevertheless, they found a significant difference in patients with severe ED according to the Sexual Health Inventory for Men and concluded that LISWT has clinical efficacy in this subgroup of patients.
More recently, Srini et al,34 in a randomized double-blinded trial with active treatment and sham therapy, reported a positive long-term efficacy in patients with vasculogenic ED treated with linear-focused shockwaves, just as Vardi et al32 had (Omnispec ED1000).
In a narrative review of all published studies, Gruenwald et al35 found that 60% to 75% of treated patients who responded to PDE5i therapy could eliminate their dependency on those drugs and achieve an erection and vaginal penetration and that 72% of non-responders to PDE5i before undergoing LISWT became responders and achieved vaginal penetration.
These investigators used a compact electrohydraulic system fitted with a targeted shockwave source (Omnispec ED1000). Unlike the system used for the present patients, Gruenwald et al35 had to stretch the penis and manually apply the transducer to it proximally, medially, and distally and then apply it to the perineum. With this operator-dependent method, the selected treatment protocol consisted of two sessions per week for a period of 3 weeks and was repeated after a treatment-free interval of 3 weeks.
Chung and Cartmill,36 in an open-label prospective study of 30 patients with ED, assessed the efficacy and safety of an electromagnetic shockwave unit of higher energy density (0.25 mJ/mm2) previously used in the treatment of tenosynovitis and tendinitis (Duolith SD1 Ultra; Storz Medical AG, Tägerwilen, Switzerland). Treatment duration consisted of two sessions per week for a period of 6 uninterrupted weeks. Sixty percent of patients showed an improved erectile response according to the IIEF-5 and the Erectile Dysfunction Inventory of Treatment Satisfaction index 6 weeks after treatment, and this effect remained for 4 months.
The present trial was performed using the Renova NR. Its design makes it operator independent: its transducer can deliver shockwaves after being secured to the penis and the perineum; thus, the operator does not need to hold the device. The transducer spans an area of 70 mm, which allows effective application to each corpus cavernosum. LISWT involves a very small amount of energy (0.09 mJ/mm2), equivalent to 10% of the energy used by conventional lithotripters for the treatment of urinary tract stones.
The efficacy of the Renova NR reported by other investigators was an average improvement of more than four points in the IIEF-EF score, thus going beyond the minimal important differences proposed by Rosen et al30 to consider a treatment of ED effective.
Reisman et al,31 in a multicenter study with a larger number of patients and 6-month follow-up, reported 81% efficacy, whereas Ruffo et al37 reported 76% efficacy in a group of 31 patients and 3-month follow up.
Currently, no available study has directly compared the efficacy of these three different LISWT methods. In the present study, improvements in IIEF-EF, SEP2, SEP3, and EHS scores became evident from the first through the third follow-ups after treatment, with statistically significant values that were maintained to the end of the follow-up phase in 90% of patients.
It is worth pointing out that, unlike what has been reported by other investigators, the present study considered a patient responsive to LISWT when he showed improvement in efficacy in all four assessments and responded positively to the GAQ and not just the IIEF score alone, which reinforces the result of this study. It is well known that changes in IIEF imply only an improvement in score but does not necessarily guarantee a patient's successful or complete sexual intercourse. In contrast, many men consult for the correction of erections insufficient for penetration, yet they are not fully satisfied. Sixty percent of the present patients achieved and maintained an erection after penetration, and they were satisfied with the improvement of their penile rigidity after treatment. This might better explain the lower efficacy compared with other studies.
Factors such as patient age and duration of ED did not influence the results.
An interesting aspect to consider is that patients continued their regular treatment and PDE5i drug throughout LISWT, thus eliminating the resulting bias of suspending and resuming oral treatment as described in other trials. Therefore, each patient was compared with himself before and after shockwave therapy concurrently with PDE5i treatment.
This study has several limitations that are important to consider. First, its lack of a placebo group prevents a proper comparison of the effects of LIWST. As mentioned earlier, other trials have shown significant differences between active and placebo treatments.24, 32, 33, 34 Second, this research extended through a follow-up period of 12 months and sustained the patients' response; thus, there was no placebo treatment, which tends to be brief and not sustained over time, although this aspect has not been fully elucidated. Third, 10 patients were not included in the results owing to lack of follow-up. If one assumes that those 10 patients dropped out because of lack of response or were disappointed with the results, then this could constitute a serious bias when interpreting the results. If this were the case, then the response rate would be of 48% instead of 60%. This value seems more realistic given the weight of the results presented by Kitrey et al24 who obtained approximately 50% recovery in non-responders to PDE5i therapy in a prospective, randomized, double-blinded, sham-controlled study. If the lack of placebo is considered an important bias, then it should be considered representative of a “real-life” setting.
In contrast, whenever independent pilot studies are conducted, the number of patients included tends to be small, and the results cannot be generalized. Nevertheless, however limited the data and the experiences reported in the literature thus far, one can consider these data quite promising.
There is no certainty that these improvements were due to the vascular changes suggested by other investigators because this study had an observational design of clinical practice; patients did not undergo any penile vascular study such as a Doppler evaluation that can show changes in the cavernosal arteries.
There are many uncertainties to LISWT: the published literature is not multicentric and usually has a small number of patients and short follow-up time. It is not clear whether the number of sessions and treatments was sufficient. It does not define the best profile of patients who might benefit from this treatment. The mechanism of action is not clear.
Nevertheless, LISWT has a good safety profile, with no adverse events reported. The effectiveness in clinical and empirical practice is high. This new treatment modality seems promising to optimize treatments of ED, especially in patients with associated VRFs.
The main contribution of this study is adding more data using LISWT with only four sessions and a second-generation device in patients with ED unresponsive to PDE5i and associated VRFs followed for 1 year.
Despite the enthusiasm over these results, it is necessary to have a larger number of long-term multicentric placebo-controlled studies that can prove the efficacy and safety of this innovative treatment tool, thus avoiding false expectations and unnecessary medical expenses.
Conclusions
Extracorporeal LISWT in patients with ED unresponsive to PDE5i treatment was effective and safe in 60% of patients. The efficacy response was maintained for 12 months in most patients. Large-scale, multicentric, long-term, randomized, sham-controlled studies are needed to determine the benefits of this new line of treatment for ED.
Statement of authorship
Category 1
-
(a)Conception and Design
- Amado Bechara; Adolfo Casabé
-
(b)Acquisition of Data
- Amado Bechara; Adolfo Casabé; Walter De Bonis; Pablo Gomez Cicilia
-
(c)Analysis and Interpretation of Data
- Amado Bechara; Adolfo Casabé
Category 2
-
(a)Drafting the Article
- Amado Bechara
-
(b)Revising It for Intellectual Content
- Amado Bechara; Adolfo Casabé
Category 3
-
(a)Final Approval of the Completed Article
- Amado Bechara; Adolfo Casabé; Walter De Bonis; Pablo Gomez Cicilia
Footnotes
Conflict of Interest: The author reports no conflicts of interest.
Funding: None.
References
- 1.Kloner R. Erectile dysfunction and cardiovascular risk factors. Urol Clin N Am. 2005;32:397–402. doi: 10.1016/j.ucl.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Gandaglia G., Briganti A., Jackson G. A systematic review of the association between erectile dysfunction and cardiovascular disease. Eur Urol. 2014;65:968–978. doi: 10.1016/j.eururo.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 3.Seftel A.D., Sun P., Swindle R. The prevalence of hypertension, hyperlipidemia, diabetes mellitus and depression in men with erectile dysfunction. J Urol. 2004;171:2341–2345. doi: 10.1097/01.ju.0000125198.32936.38. [DOI] [PubMed] [Google Scholar]
- 4.Eardley I., Donatucci C., Corbin J. Pharmacotherapy for erectile dysfunction. J Sex Med. 2010;7:524–540. doi: 10.1111/j.1743-6109.2009.01627.x. [DOI] [PubMed] [Google Scholar]
- 5.Gruenwald I., Shenfeld O., Chen J. Positive effect of counseling and dose adjustment in patients with erectile dysfunction who failed treatment with sildenafil. Eur Urol. 2006;50:134–140. doi: 10.1016/j.eururo.2006.01.042. [DOI] [PubMed] [Google Scholar]
- 6.Hatzimouratidis K., Moysidis K., Bekos A. Treatment strategy for “non-responders” to tadalafil and vardenafil: a real-life study. Eur Urol. 2006;50:126–132. doi: 10.1016/j.eururo.2006.02.060. [DOI] [PubMed] [Google Scholar]
- 7.Carvalheira A.A., Pereira N.M., Maroco J., Vera F. Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–2369. doi: 10.1111/j.1743-6109.2012.02787.x. [DOI] [PubMed] [Google Scholar]
- 8.Sommer F., Engelmann U. Future options for combination therapy in the management of erectile dysfunction in older men. Drugs Aging. 2004;21:555–564. doi: 10.2165/00002512-200421090-00001. [DOI] [PubMed] [Google Scholar]
- 9.Dhir R., HCh Lin, Canfield S.E. Combination therapy for erectile dysfunction: an update review. Asian J Androl. 2011;13:382–390. doi: 10.1038/aja.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hakim L., Van der Aa F., Bivalacqua T.J. Emerging tools for erectile dysfunction: a role for regenerative medicine. Nat Rev Urol. 2012;9:520–536. doi: 10.1038/nrurol.2012.143. [DOI] [PubMed] [Google Scholar]
- 11.Ciampa A.R., de Prati A.C., Amelio E. Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett. 2005;579:6839–6845. doi: 10.1016/j.febslet.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Young S.R., Dyson M. The effect of therapeutic ultrasound on angiogenesis. Ultrasound Med Biol. 1990;16:261–269. doi: 10.1016/0301-5629(90)90005-w. [DOI] [PubMed] [Google Scholar]
- 13.Nurzynska D., Di Meglio F., Castaldo C. Shock waves activate in vitro cultured progenitors and precursors of cardiac cell lineages from the human heart. Ultrasound Med Biol. 2008;34:334–342. doi: 10.1016/j.ultrasmedbio.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Nishida T., Shimokawa H., Oi K. Extracorporeal cardiac shock wave therapy markedly ameliorates ischemia-induced myocardial dysfunction in pigs in vivo. Circulation. 2004;110:3055–3061. doi: 10.1161/01.CIR.0000148849.51177.97. [DOI] [PubMed] [Google Scholar]
- 15.Aicher A., Heeschen C., Sasaki K. Low energy shock wave for enhancing recruitment of endothelial progenitor cells: a new modality to increase efficacy of cell therapy in chronic hind limb ischemia. Circulation. 2006;114:2823–2830. doi: 10.1161/CIRCULATIONAHA.106.628623. [DOI] [PubMed] [Google Scholar]
- 16.Kikuchi Y., Ito K., Ito Y. Double-blind and placebo-controlled study of the effectiveness and safety of extracorporeal cardiac shock wave therapy for severe angina pectoris. Circ J. 2010;74:589–591. doi: 10.1253/circj.cj-09-1028. [DOI] [PubMed] [Google Scholar]
- 17.Wang C.J., Kuo Y.R., Wu R.W. Extracorporeal shockwave treatment for chronic diabetic foot ulcers. J Surg Res. 2009;152:96–103. doi: 10.1016/j.jss.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 18.Dumfarth J., Zimpfer D., Vögele-Kadletz M. Prophylactic low energy shock wave therapy improves wound healing after vein harvesting for coronary artery bypass graft surgery: a prospective, randomized trial. Ann Thorac Surg. 2008;86:1909–1913. doi: 10.1016/j.athoracsur.2008.07.117. [DOI] [PubMed] [Google Scholar]
- 19.Gotte G., Amelio E., Russo S. Short time non-enzymatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 2002;520:153–155. doi: 10.1016/s0014-5793(02)02807-7. [DOI] [PubMed] [Google Scholar]
- 20.Qiu X., Lin G., Xin Z. Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. J Sex Med. 2013;10:738–746. doi: 10.1111/jsm.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assaly-Kaddoum R, Giuliano F, Laurin M, et al. Low intensity extracorporeal shockwave therapy (Li-ESWT) improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. J Urol. http://dx.doi.org/10.1016/j.juro.2016.03.147 [E-pub ahead of print]. [DOI] [PubMed]
- 22.Vardi Y., Appel B., Jacob G. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58:243–248. doi: 10.1016/j.eururo.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Grunewald I., Appel B., Vardi Y. Low-intensity extracorporeal shock wave therapy—a novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. J Sex Med. 2012;9:259–264. doi: 10.1111/j.1743-6109.2011.02498.x. [DOI] [PubMed] [Google Scholar]
- 24.Kitrey N.D., Gruenwald I., Appel B. Penile low intensity shock wave treatment is able to shift pde5i nonresponders to responders: a double-blind, sham controlled study. J Urol. 2016;195:1550–1555. doi: 10.1016/j.juro.2015.12.049. [DOI] [PubMed] [Google Scholar]
- 25.Cappelleri J., Rosen R., Smith M. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 26.McMahon C., Smith C., Shabsigh R. Treating erectile dysfunction when PDE5 inhibitors fail. BMJ. 2006;332:589–592. doi: 10.1136/bmj.332.7541.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen R.C., Cappelleri J.C., Gendrano N., III The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14:226–244. doi: 10.1038/sj.ijir.3900857. [DOI] [PubMed] [Google Scholar]
- 28.Porst H., Vardi Y., Akkus E. Standards for clinical trials in male sexual dysfunctions. In: Montorsi F., Basson R., Adaikan G., editors. Sexual medicine sexual dysfunctions in men and women. Third international consultation on sexual medicine. Health Publication Ltd.; Paris: 2010. pp. 567–603.http://www.icud.info/PDFs/SEXUAL-MEDICINE-2010.pdf Available at: [Google Scholar]
- 29.Mulhall J.P., Goldstein I., Bushmakin A.G. Validation of the Erection Hardness Score. J Sex Med. 2007;4:1626–1634. doi: 10.1111/j.1743-6109.2007.00600.x. [DOI] [PubMed] [Google Scholar]
- 30.Rosen R.C., Allen K.R., Ni X. Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. Eur Urol. 2011;60:1010–1016. doi: 10.1016/j.eururo.2011.07.053. [DOI] [PubMed] [Google Scholar]
- 31.Reisman Y., Hind A., Varaneckas A. Initial experience with linear focused shockwave treatment for erectile dysfunction: a 6-month follow-up pilot study. Int J Impot Res. 2015;27:108–112. doi: 10.1038/ijir.2014.41. [DOI] [PubMed] [Google Scholar]
- 32.Vardi Y., Appel B., Kilchevsky A. Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. J Urol. 2012;187:1769–1775. doi: 10.1016/j.juro.2011.12.117. [DOI] [PubMed] [Google Scholar]
- 33.Yee C., Chan E., Hou S.M. Extracorporeal shock wave therapy in the treatment of erectile function. A prospective, randomized, double-blinded, placebo, controlled study. Int J Urol. 2014;21:1041–1045. doi: 10.1111/iju.12506. [DOI] [PubMed] [Google Scholar]
- 34.Srini V.S., Reddy R.K., Shultz T. Low intensity extracorporeal shockwave therapy for erectile dysfunction: a study in an Indian population. Can J Urol. 2015;22:7614–7622. [PubMed] [Google Scholar]
- 35.Gruenwald I.E., Kitey N., Appel B. Low intensity shock wave therapy in vascular disease and erectile dysfunction: theory and outcomes. Sex Med Rev. 2013;1:83–90. doi: 10.1002/smrj.9. [DOI] [PubMed] [Google Scholar]
- 36.Chung E., Cartmill R. Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: an Australian first open-label single-arm prospective clinical trial. BJU Int. 2015;115(Suppl. 5):46–49. doi: 10.1111/bju.13035. [DOI] [PubMed] [Google Scholar]
- 37.Ruffo A., Capece M., Prezioso D. Safety and efficacy of low intensity shockwave (LISW) treatment in patients with erectile dysfunction. Int Braz J Urol. 2015;41:967–974. doi: 10.1590/S1677-5538.IBJU.2014.0386. [DOI] [PMC free article] [PubMed] [Google Scholar]