Abstract
The purpose of the present study was to measure six vitamin D metabolites and to find the association between vitamin D deficiency and coronary artery diseases in diabetes (T2DM_CAD). Four groups [control (n = 50), type 2 diabetes (T2DM, n = 71), coronary artery diseases (CAD, n = 28), T2DM_CAD (n = 38)] of total 187 subjects were included in the study. Six vitamin D metabolites (D2, D3, 25(OH)D2, 25(OH)D3, 1,25(OH)2D2, 1,25(OH)2D3), total 25(OH)D and total 1,25(OH)2D were measured by UPLC/APCI/HRMS method in these subjects. Although all the vitamin D metabolites were significantly decreased in T2DM_CAD as compared to both control and T2DM subjects (p < 0.05), only two metabolites i.e., 25(OH)D3 and total 25(OH)D were significantly (p < 0.05) decreased in the T2DM subjects as compared with the control subjects (p < 0.05). Vitamin D3, 1,25(OH)2D2, 25(OH)D, and 1,25(OH)2D levels were significantly decreased in T2DM_CAD subjects as compared with CAD subjects (p < 0.05). Further, multiple logistic regression analysis revealed that total 25(OH)D and total 1,25(OH)2D can be used to predict T2DM (OR 0.82.95% CI 0.68–0.99; p = 0.0208) and T2DM with CAD (OR 0.460, 95% CI 0.242–0.874; p = 0.0177), respectively. Our data concludes that lower concentration of 1,25(OH)2D is associated with type 2 diabetes coexisting with coronary artery diseases in South Indian subjects.
Type 2 diabetes is characterized by hyperglycemia as well as insulin resistance. It is a complex metabolic disease accompanied by several complications such as obesity, hypertension, dyslipidemia and coronary artery disease (CAD). All these complications are interlinked and not understood completely1. As the disease progresses, diabetic patients develop micro and macro vascular complications. Hyperglycemic condition and insulin resistance in adults increases the risk of heart attack, stroke, angina, and coronary artery disease. Cardiovascular risk is two to four fold higher in diabetic subjects as compared to non-diabetic subjects2,3,4. Several factors like obesity, hyperglycemia, hypertension, inflammation, endothelial dysfunction and oxidative stress are responsible for the increased risk of cardiovascular complication among diabetic patients. Among all factors, lower vitamin D level in blood is regarded as one of the important risk factor to develop cardiovascular complication.
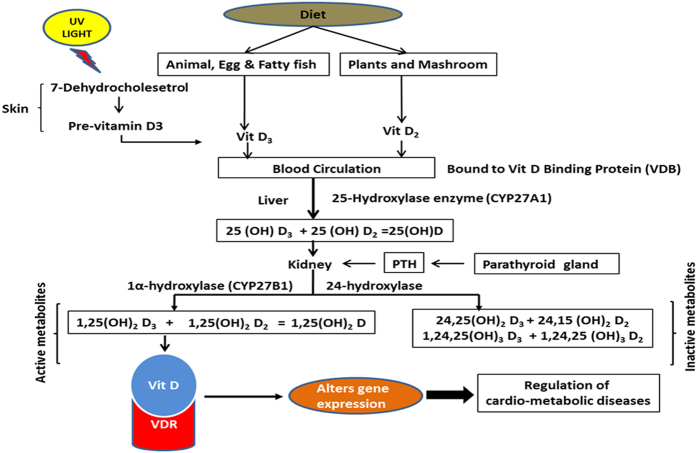
Vitamin D is a secosteroid that exists in two forms i.e., ergocalciferol (D2) and cholecalciferol (D3). Ergocalciferol (D2) is synthesized from the vegetable sources while cholecalciferol (D3) is either synthesized from the epidermis by exposure to the UV radiation (sunlight) or available from oily fish supplementation. Vitamin D (D2 and D3) is converted into its active metabolite 1,25(OH)2D by the two hydroxylation steps. Vitamin D (D2 and D3) are hydroxylated by the liver and converted into 25 hydroxy D [25(OH)D2 and 25(OH)D3]. These two were further hydroxylated into two active metabolites, 1,25(OH)2D [1,25(OH)2D2 and 1,25(OH)2D3] in the kidney. These active metabolites bind with the vitamin D receptor and exert its function5 (Fig. 1). Vitamin D receptors are present in many cells like pancreatic β cells, cardiomyocytes, endothelial cells and vascular smooth muscle cells. Vitamin D plays pivotal role in the bone and mineral metabolism. Vitamin D deficiency is a common health problem worldwide and is the cause for osteoporosis and osteomalacia, rickets and other bone related disorders. In the last decade, researchers observed that lower vitamin D levels were associated with metabolic diseases like type 1 diabetes, obesity, insulin resistance, cardiovascular diseases, and cancer6,7,8. Many studies reported that Indian subjects are more prone to vitamin D deficiency despite the availability of abundant sunshine throughout the year in many parts of India9,10,11,12,13,14,15,16,17. Although, there are some studies from Indian population but none of these studies looked into the association of vitamin D metabolites with coronary artery diseases coexisting with type 2 diabetes. For last few decades more than 50 metabolites of vitamin D have been described18. Among them very few have been quantified in blood.
Figure 1. Vitamin D synthesis and metabolism:
Vitamin D2 is synthesized from food whereas D3 is synthesized from 7-dehydrocholesterol by sun light. Vitamin D2 and D3 hydroxylate at 25 position in the liver to form 25(OH)D2 and 25(OH)D3, then hydroxylate again at position 1α to form active metabolites 1,25(OH)2D2 and 1,25(OH)2D3. These active metabolites participate in the biological activity.
Currently, general awareness of association of vitamin D insufficiency and increased risk of several diseases has been increased. However, it is not clear which vitamin D metabolite should be quantified and what is the association of each metabolite with increased risk of diseases. Among all vitamin D metabolites, only 25(OH)D and 1,25(OH)2D have received great attention. Hence in the present study six vitamin D metabolites have been quantified by UPLC/APCI/HRMS method. Therefore, the purpose of the present study was to measure six vitamin D metabolites, total 25(OH)D and total 1,25(OH)2D levels in control, T2DM, CAD and T2DM with CAD and to find the association between vitamin D deficiency and coronary artery diseases in diabetes.
Results
Four groups (Control, T2DM, CAD and T2DM_CAD) of total 187 subjects were included in this present study. The serum level of total 25(OH)D was well classified in the previous literature19,20. Anthropometric and clinical characteristics of all subjects based on 25(OH)D categories were presented in Table 1. There were no significant differences in age, body mass index (BMI), systolic and diastolic blood pressure (BP), creatinine, estimated glomerular filtration rate (eGFR), uric acid, creatinine kinase myoglobin isoenzyme (CK-MB), and apolipoprotein B (Apo-B). Glycated hemoglobin (HbA1c) levels were increased significantly (p < 0.05) in patients having 20–30 ng/ml and <20 ng/ml at 25(OH)D levels as compared with subjects having >30 ng/ml of 25(OH)D. Similarly, fasting blood sugar (FBS) levels were also increased in patient groups having 25(OH)D levels 20–30 ng/ml and <20 ng/ml as compared with patients having >30 ng/ml.
Table 1. Anthropometric and biochemical variables by serum 25(OH)D concentrations (>30 and 20–30 and <20 ng/ml).
| Variables | All measured participants | 25(OH)D ng/ml |
p value | ||
|---|---|---|---|---|---|
| >30 ng/ml | 20–30 ng/ml | <20 ng/ml | |||
| N (%) | 187 | 111 (59.4) | 40 (21.4) | 36 (19.3) | — |
| Age (years) | 47.8 (8.9) | 47.4 (9.6) | 48.1 (8.4) | 48.8 (7.0) | 0.696 |
| Gender (Male/Female) | 126/61 | 74/37 | 25/50 | 27/9 | — |
| BMI | 26.4 (4.6) | 26.3 (4.7) | 26.6 (5.0) | 26.4 (4.0) | 0.939 |
| Systolic BP (mmHg) | 132.5 (19.2) | 131.9 (16.9) | 135.4 (24.7) | 131.2 (18.9) | 0.565 |
| Diastolic BP (mmHg) | 81.8 (9.8) | 81.8 (9.8) | 82.2 (10.7) | 81.7 (9.3) | 0.972 |
| HbA1C (%) | 6.5 (5.5–8.5) | 6.2 (5.4–8.1) | 7.4 (5.3–88) | 6.9 (5.6–8.9) | 0.0403* |
| FBS (mg/dl) | 130 (99–201) | 113 (97–190) | 174.5 (109.5–235) | 138.5 (105–200) | 0.0622 |
| Creatinine (mg/dl) | 0.9 (0.7–1) | 0.9 (0.7–1) | 0.85 (0.8–0.95) | 0.9 (0.75–1.2) | 0.114 |
| eGFR (mL/min/1.73 m2) | 92.9 (25.1) | 94.4 (25.6) | 94.8 (20.1) | 86.7 (28.2) | 0.245 |
| Uric acid (mg/dl) | 4.6 (1.5) | 4.8 (1.5) | 4.3 (1.5) | 4.4 (1.3) | 0.159 |
| TG (mg/dl) | 152 (108–226) | 160 (113–237) | 136.5 (103.5–172) | 177 (109.5–242.5) | 0.137 |
| HDL-C (mg/dl) | 33 (28–39) | 33 (29–39) | 36.5 (30–42.5) | 31.5 (26–36) | 0.142 |
| CK-MB (mg/dl) | 21.5 (8.5) | 21.2 (7.4) | 21.9 (8.6) | 21.9 (10.1) | 0.869 |
| Apo-B (mg/dl) | 81.7 (68.3–96.6) | 84.7 (71.8–99.6) | 77 (64.2–92.2) | 68.4 (65.7–88.7) | 0.173 |
| 25(OH)D (ng/ml) | 36 (19.5) | 46.5 (18) | 24.5 (3.1) | 14.1 (2.9) | <0.001* |
| 1,25(OH)2D (ng/ml) | 11.1 (9.2–12.3) | 11.6 (10.1–14.2) | 10.6 (8.9–11.6) | 8.3 (8–9.7) | <0.001* |
| Vitamin D2 (ng/ml) | 27.4 (10.5) | 29.7 (10.3) | 26 (10.9) | 20.9 (7) | <0.001* |
| 25(OH)D2 (ng/ml) | 4.5 (3.4–5.9) | 4.5 (3.4–7.3) | 4.5 (3.6–5.9) | 3.5 (2.9–4.5) | 0.0002* |
| 1,25(OH)2D2 (ng/ml) | 4.4 (3.7–5.4) | 4.8 (4.0–6.1) | 4.2 (3.9–4.8) | 3.4 (3.1–4.0) | <0.001* |
| Vitamin D3 (ng/ml) | 18.9 (31.8–23.3) | 22 (18.3–24.5) | 16.3 (13.1–19.2) | 13.3 (12–15) | <0.001* |
| 25 (OH)D3 (ng/ml) | 27.4 (18.3–37.5) | 33.4 (28.5–45–4) | 19.4 (17.4–22) | 10.5 (8.3–11.9) | <0.001* |
| 1,25(OH)2D3 (ng/ml) | 6.3 (5.1–7.3) | 6.8 (5.7–7.5) | 5.6 (4.9–7.1) | 5.1 (4.7–5.3) | <0.001* |
Data are Mean (SD) and Median (Q1–Q3) for normally distributed & non-normally distributed variables, respectively. *p < 0.05 for a test comparing across 25(OH)D groups. Significant values were shown in Bold.
Among all T2DM subjects, 43 subjects had history of hypertension. Among CAD subjects, 23 subjects were diagnosed with acute myocardial infarction (MI) and five were with unstable angina. Among T2DM_CAD subjects, 31 subjects were diagnosed with acute myocardial infraction and 7 were diagnosed with unstable angina.
Distribution of vitamin D2 and D3 metabolites in control, T2DM, CAD and T2DM_CAD groups
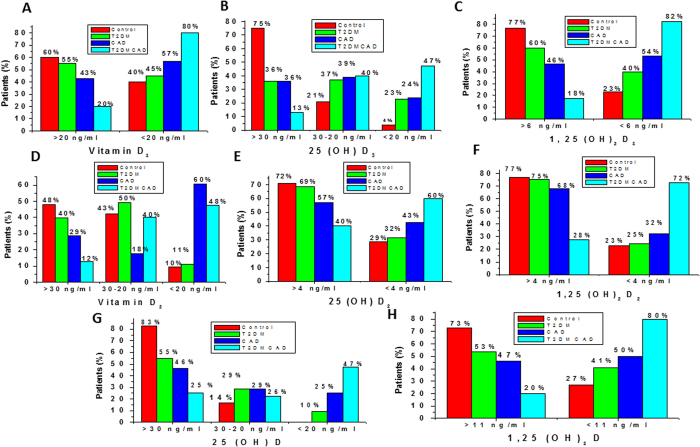
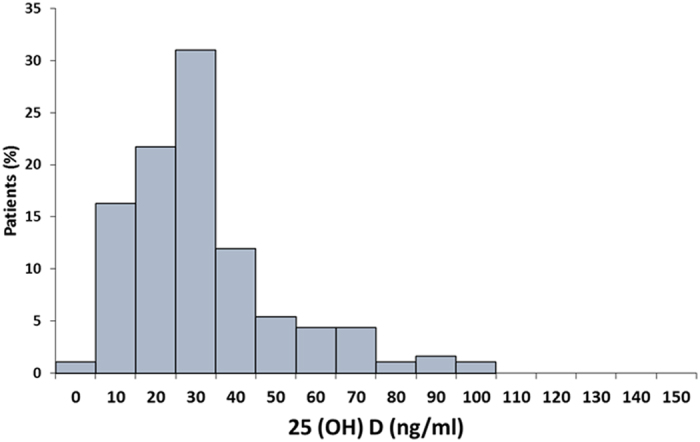
Distribution of total 25(OH)D levels in all subjects was mentioned in Fig. 2. The median total 25(OH)D concentrations in the total subjects was 32.3 (range 7.9–99.0). According to the previous literature, serum total 25(OH)D concentrations were well categorized as sufficient >30 ng/ml, insufficient 30–20 ng/ml and deficient <20 ng/ml20. However, no such categories were established for the other metabolites. In present study, cut off points was set based on the median of the individual metabolites in total subjects. Cutoff values for all three 25(OH)D3, Vitamin D2 and total 25(OH)D metabolites were categorized as >30, 30–20, and <20 ng/ml. Other vitamin D metabolites like vitamin D3 (>20 and <20 ng/ml), 1,25(OH)2D3 (>6 and <6 ng/ml), 25(OH)D2 (>4 and <4 ng /ml), 1,25(OH)2D2 (>4 and <4 ng/ml) and 1,25(OH)2D (>11 and <11 ng/ml) were categorized as stated to find distribution of patients in different groups.
Figure 2. Distribution of serum 25(OH)D concentrations in total subjects.
In the present study, higher percentage of subjects having optimum or higher level of vitamin D3 (>20 ng/ml), 25(OH)D3 (>30 ng/ml) and 1,25(OH)2D3 (>6 ng/ml) metabolites were observed in control group. However, the percentage of diabetes along with CAD subjects were increased when we considered lower concentration of vitamin D3 (<20 ng/ml), 25(OH)D3 (<20 ng/ml) and 1,25(OH)2D3 (<6 ng/ml) metabolites. Lower percentage of T2DM, CAD and T2DM with CAD subjects were observed when we considered higher concentration of vitamin D3 metabolites. However, the percentage has been increased when we consider lower concentration of vitamin D3 metabolites (Fig. 3A,B and C). Similar changes were also observed for all three vitamin D2 metabolites (Vitamin D2, 25(OH)D2, 1, 25(OH)2D2) (Fig. 3D,E and F).
Figure 3. Distribution of vitamin D3, Vitamin D2 and 25(OH)D and 1,25(OH)2D metabolites in control, T2DM, CAD and T2DM_CAD.
(A) Distribution of Vitamin D3 levels according to serum concentration i.e., <20 ng/ml verses >20 ng/ml. (B) Distribution of 25(OH)D3 levels according to serum concentrations i.e., >30 ng/ml, 30–20 ng/ml and <20 ng/ml. (C) Distribution of 1,25(OH)2D3 levels according to serum concentrations i.e., >6 ng/ml verses <6 ng/ml. (D) Distribution of vitamin D2 levels according to serum concentrations i.e., >30 ng/ml, 30–20 ng/ml and <20 ng/ml. (E) Distribution of 25(OH)D2 levels according to serum concentrations i.e., >4 ng/ml verses <4 ng/ml. (F) Distribution of 1,25(OH)2D2 levels according to serum concentration i.e., >4 ng/ml verses <4 ng/ml. (G) Distribution of 25(OH)D levels according to serum concentrations i.e., >30 ng/ml, 20–30 ng/ml and <20 ng/ml. (H). Distribution of 1,25(OH)2D levels according to serum concentrations i.e., >11 ng/ml verses <11 ng/ml.
Distribution of total 25(OH)D and total 1,25(OH)2D in control, T2DM, CAD and T2DM_CAD subjects
In the present study, higher percentage of subjects having optimum levels of total 25(OH)D (>30 ng/ml) and total 1,25(OH)2D (>11 ng/ml) were observed in control subjects. However, the percentage of diabetes along with CAD subjects (47% and 80%) were increased in subjects having lower concentration of total 25(OH)D3 (<20 ng/ml) and total 1,25(OH)2D (<11 ng/ml) when compared with control subjects (25% and 20%) (Fig. 3G and H).
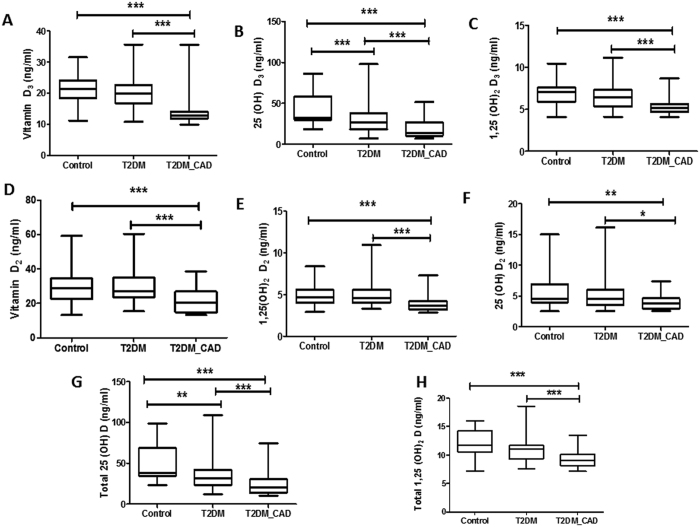
Vitamin D metabolites levels in control, T2DM and T2DM_CAD
All six vitamin D metabolites and total 25(OH)D, total 1,25(OH)2D were significantly lowered in T2DM_CAD group as compared to control group (p < 0.05) (Fig. 4A–H). Similarly, all six vitamin D metabolites levels and total 25(OH)D, total 1,25(OH)2D were significantly (p < 0.05) decreased in T2DM_CAD group as compared to T2DM group (Fig. 4A–H). Only serum 25(OH)D3 and 25(OH)D levels were significantly (p < 0.05) lowered in T2DM group as compared to control (Fig. 4B and G). Results from the present study indicates that T2DM_CAD group patients have more severe vitamin D deficiency as reflected by reduction of all vitamin D metabolites levels in blood compared to T2DM group patients.
Figure 4. Serum vitamin D metabolites levels in control, T2DM and T2DM_CAD groups.
Serum levels of vitamin D3 (A), 25(OH)D3 (B), 1,25(OH)2D3 (C)vitamin D2 (D), 25(OH)D2 (E), 1,25(OH)2D2 (F) 25(OH)D (G), and 1,25(OH)2D (H) were determined in control, T2DM, and T2DM_CAD groups. Data were expressed as median and interquartile range. p < 0.05 was considered significant.
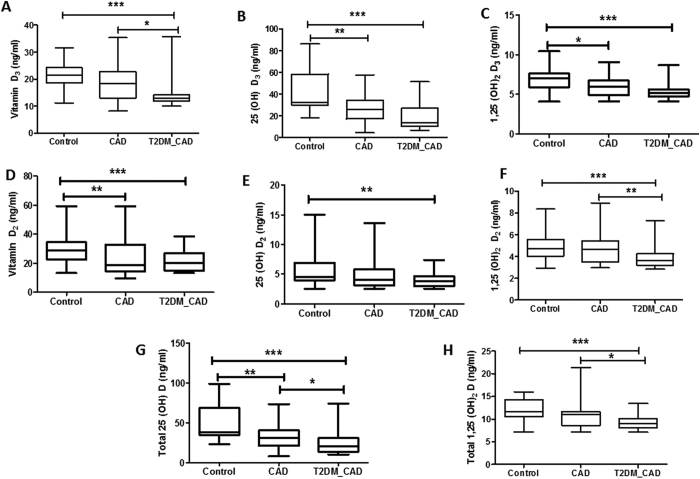
Vitamin D metabolites levels in control, CAD and T2DM_CAD
All six vitamin D metabolites and total 25(OH)D, total 1,25(OH)2D levels in control, CAD and T2DM_CAD group subjects were shown in (Fig. 5A–H). All six Vitamin D metabolites and total 25(OH)D, total 1,25(OH)2D were significantly (p < 0.05) lowered in T2DM_CAD subjects when compared with control subjects (Fig. 5A–H). 25(OH)D3, 1,25(OH)2D3,vitamin D2, and 25(OH)D metabolites were significantly (p < 0.05) lowered in CAD patients as compared with control subjects (Fig. 5B,C,D and G, respectively). Vitamin D3, 1,25(OH)2D2, 25(OH)D, and 1,25(OH)2D metabolites were significantly (p < 0.05) lowered in T2DM_CAD subjects as compared to CAD group subjects (Fig. 5A,F,G and H). These results indicated that T2DM_CAD subjects have severe vitamin deficiency as reflected by reduction of all vitamin D metabolites levels in blood compared with the control subjects.
Figure 5. Serum vitamin D metabolites levels in control, CAD and T2DM_CAD groups.
Serum levels of vitamin D3 (A), 25(OH)D3 (B), 1,25(OH)2D3 (C), vitamin D2 (D), 25(OH)D2 (E), 1,25(OH)2D2 (F), 25(OH)D (G), and 1,25(OH)2D (H) were determined in control, CAD, and T2DM_CAD groups. Data were expressed as median and interquartile range. p < 0.05 was considered significant.
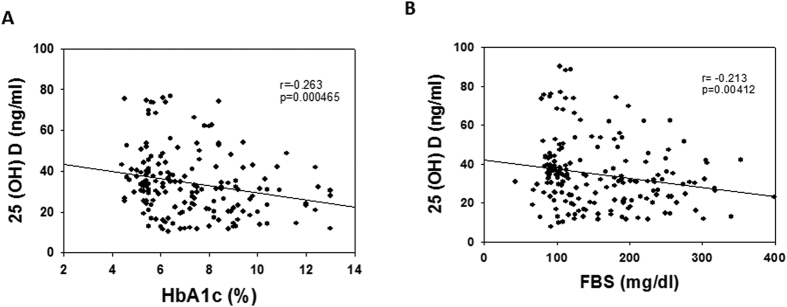
Association between 25(OH)D, FBS and HbA1c in all the subjects
Correlation has been measured to show the association between pairs of variables associated. Spearman correlation is examined between 25(OH)D and HbA1c or FBS. Both pairs of variables showed significant negative correlation between 25(OH)D and FBS (r = −0.213; p < 0.001) (Fig. 6A), and 25(OH)D and HbA1c (r = −0.263; p < 0.001) (Fig. 6B). Present study did not show significant association of 25(OH)D with age, BMI, and CK-MB.
Figure 6.
Scatterplot representing relationship between (A) 25(OH)D and FBS (B) 25(OH)D and HbA1C.
Correlation Analysis
Supplementary File 1: Table S2 shows vitamin D3 is negatively correlated with creatinine (r = 0.201; p = 0.0063) and positively correlated with eGFR (r = 0.146; p = 0.0480), and gender (r = 0.182; p = 0.0135). 25(OH)D3 is negatively associated with HbA1c (r = −0.250; p = 0.0006), and fasting blood glucose (r = −0.216; p = 0.0033). 1,25(OH)2D3 is negatively correlated with HbA1c (r = −0.162; p = 0.0283), and fasting blood sugar (r = −0.148; p = 0.0448). Vitamin D2 is negatively correlated with gender (r = −0.173; p = 0.0189) and CK-MB (r = −0.161; p = 0.0287). Total 25(OH)D negatively associated with HbA1c (r = −0.263; p = 0.0004), fasting blood glucose (r = −0.213; p = 0.0041) and eGFR (r = −0.339; p = 0.0258) whereas positively correlated with diastolic blood pressure (r = 0.318; p = 0.0258) and creatinine (r = 0.316; p = 0.0267).
Logistic Regression Analysis
Univariate logistic regression analysis identified several significant factors that predicted the presence of type 2 diabetes with coronary artery diseases. Multivariate logistic regression analysis showed in Table 2, 3, 4, 5. With control and T2DM, multivariate analysis showed HbA1c (odds ratio (OR) 53.01, 95% confidence interval (CI) 47.6–589.2; p < 0.0001), fasting blood glucose (FBS) (OR 1.07, 95% CI 1.03–1.13; p < 0.0001) and total 25(OH)D (OR 0.92, 95% CI 0.85–0.99; p = 0.021) were predictor for T2DM. In addition, we performed force entry multivariate logistic regression analysis to adjust for the factors suspected of contributing to decrease vitamin D metabolites. In the model 1, HbA1c (OR 1000, 95% CI 1.225->999.0; p < 0.0001), FBS (OR 1.350, 95% CI 0.975–1.870; p < 0.0001), smoking history (OR 0.0003, 95% CI 0.0001–16.09; p = 0.0124) and decreased total 25(OH)D (OR 0.694, 95% CI 0.462–1.041; p < 0.0208) were predictors of T2DM. In the model 2, after adjustment for other established risk factors: age, female, smoking history, alcoholic history and family history, showed that HbA1c (OR 120.69 95% CI 2.39->999.99; p = <0.0001), FBS (OR 1.168, 95% CI 1.017–1.342; p < 0.0001) and decreased total 25(OH)D levels (OR 0.817, 95% CI 0.673–0.993; p = 0.0208) were predictors of T2DM (Table 2).
Table 2. Logistic regression analysis of T2DM vs control subjects.
| Factor | Univariate |
Multivariate |
Model 1 (unadjusted) |
Model 2 (adjusted) |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | 1.03 (0.99–1.08) | 0.1586 | 1.29 (0.826–2.029) | 0.0955 | ||||
| Sex (female) | 1.83 (0.87–3.84) | 0.1107 | 0.001 (0.0001–6.200) | 0.0600 | ||||
| BMI | 1.06 (0.99–1.15) | 0.1165 | ||||||
| HbA1c (%) | 15.49 (5.37–44.69) | <0.0001 | 53.01 (47.69–589.25) | <0.0001 | 1000 (1.23->999.99) | <0.0001 | 120.69 (2.39->999.99) | <0.0001 |
| FBS (mg/dl) | 1.09 (1.05–1.13) | <0.0001 | 1.07 (1.03–1.13) | <0.0001 | 1.350 (0.98–1.87) | <0.0001 | 1.17 (1.02–1.34) | <0.0001 |
| Systolic BP (mmHg) | 1.05 (1.02–1.08) | 0.0002 | 1.34 (0.98–1.83) | 0.1699 | 1.18 (0.98–1.40) | 0.1699 | ||
| Diastolic BP (mmHg) | 1.07 (1.02–1.12) | 0.0024 | ||||||
| Creatinine (mg/dl) | 1.77 (0.46–6.88) | 0.41 | ||||||
| eGFR (ml/min/1.72 m2) | 0.98 (0.97–1.00) | 0.121 | ||||||
| Uric acid (mg/dl) | 0.76 (0.58–0.99) | 0.0451 | ||||||
| CK-MB (u/l) | 0.93 (0.88–0.98) | 0.0101 | 0.32 (0.09–1.18) | 0.1364 | 0.666 (0.415–1.068) | 0.1364 | ||
| Apo-B (mg/dl) | 0.99 (0.99–1.005) | 0.5924 | ||||||
| Smoking history (years) | 0.86 (0.31–2.36) | 0.7708 | 0.003 (0.0001–16.09) | 0.0124 | ||||
| Alcoholic history (years) | 0.78 (0.33–1.86) | 0.5728 | ||||||
| Family history (years) | 1.46 (0.69–3.07) | 0.319 | ||||||
| D3 (ng/ml) | 0.99 (0.93–1.06) | 0.9288 | ||||||
| 25(OH)D3 (ng/ml) | 0.97 (0.94–0.99) | 0.0022 | ||||||
| 1,25(OH)D3 (ng/ml) | 0.90 (0.73–1.11) | 0.3365 | ||||||
| D2 (ng/ml) | 1.01 (0.98–1.05) | 0.5280 | ||||||
| 25(OH)D2 (ng/ml) | 0.92 (0.82–1.03) | 0.1555 | ||||||
| 1,25(OH)D2 (ng/ml) | 1.04 (0.85–1.28) | 0.6840 | ||||||
| Total 25(OH)D (ng/ml) | 0.97 (0.95–099) | 0.0019 | 0.92 (0.85–0.99) | 0.021 | 0.69 (0.46–1.04) | 0.0208 | 0.82 (0.68–0.99) | 0.0208 |
| Total 1,25(OH)D (ng/ml) | 0.98 (0.87–1.71) | 0.7390 | ||||||
Model 1: unadjusted, Model 2: adjusted for age, sex, smoking history, alcoholic history and family history of diabetes.
Table 3. Logistic regression analysis of T2DM_CAD vs control subjects.
| Factor | Univariate | Multivariate | Model 1 (Unadjusted) | Model 2 (Adjusted) | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | 1.01 (1.04–1.15) | 0.001 | 1.114 (1.024–1.212) | 0.0118 | ||||
| Sex (female) | 0.27 (0.9–0.81) | 0.019 | 0.326 (0.040–2.666) | 0.2960 | ||||
| BMI | 0.98 (0.88–1.073) | 0.602 | ||||||
| HbA1c (%) | 23.31 (3.91–138.99) | 0.0005 | 1000 (0.005–1000) | <0.0001 | ||||
| FBS (mg/dl) | 1.07 (1.04–1.10) | <0.0001 | 1.25 (0.89–1.74) | 0.0001 | ||||
| Systolic BP (mmHg) | 1.04 (1.01–1.07) | 0.023 | ||||||
| Diastolic BP (mmHg) | 1.06 (0.99–1.12) | 0.067 | ||||||
| Creatinine (mg/dl) | 20.49 (2.42–173.36) | 0.0056 | 259.85 (7.48–1000) | 0.0021 | 32.932 (0.459–1000) | 0.1089 | ||
| eGFR (ml/min/1.72 m2) | 0.98 (0.95–0.99) | 0.012 | ||||||
| Uric acid (mg/dl) | 0.90 (0.67–1.22) | 0.493 | ||||||
| CK-MB (u/l) | 5.83 (2.17–15.68) | 0.0005 | 9.903 (0.714–137.319) | 0.0875 | ||||
| Apo-B (mg/dl) | 6.09 (2.39–15.48) | 0.0001 | 0.755 (0.072–8.340) | 0.8335 | ||||
| Smoking history (years) | 1.16 (0.49–2.77) | 0.739 | 1.281 (0.255–6.440) | 0.7636 | ||||
| Alcoholic history (years) | 1.02 (0.97–1.08) | 0.349 | ||||||
| Family history (years) | 0.95 (0.92–0.98) | 0.0003 | ||||||
| D3 (ng/ml) | 0.94 (0.88–1.003) | 0.059 | ||||||
| 25(OH)D3 (ng/ml) | 0.88 (0.83–0.93) | <0.0001 | ||||||
| 1,25(OH)D3 (ng/ml) | 0.354 (0.22–0.56) | <0.0001 | ||||||
| D2 (ng/ml) | 0.88 (0.82–0.94) | <0.002 | ||||||
| 25(OH)D2 (ng/ml) | 0.92 (0.80–1.05) | 0.211 | ||||||
| 1,25(OH)D2 (ng/ml) | 0.39 (0.23–0.67) | 0.0006 | ||||||
| Total 25(OH)D (ng/ml) | 0.91 (0.86–0.95) | <0.0001 | 0.951 (0.899–1.005) | 0.074 | 0.960 (0.902–1.022) | 0.1986 | ||
| Total 1,25(OH)D (ng/ml) | 0.503 (0.37–0.68) | <0.0001 | 6.04 (0.011–19.20) | 0.0017 | 0.572 (0.359–0.912) | 0.019 | 0.460 (0.242–0.874) | 0.0177 |
Model 1: unadjusted, Model 2: adjusted for age, sex, smoking history, alcoholic history and family history of diabetes.
Table 4. Logistic regression analysis of T2DM_CAD vs CAD subjects.
| Factor | Univariate |
Multivariate |
Model 1 (unadjusted) |
Model 2 (adjusted) |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | 1.07 (0.99–1.14) | 0.0541 | 1.08 (0.99–1.16) | 0.072 | ||||
| Sex (female) | 2.05 (0.37–11.38) | 0.4142 | 8.69 (0.38–197.01) | 0.175 | ||||
| BMI | 1.11 (0.97–1.27) | 0.1396 | ||||||
| HbA1c (%) | 243.56 (6.08- >999) | 0.0035 | 1000 (0.02–1000) | <0.0001 | ||||
| FBS (mg/dl) | 1.06 (1.03–1.09) | 0.0002 | 1.16 (0.96–1.39) | 0.0061 | ||||
| Systolic BP (mmHg) | 1.00 (0.98–1.03) | 0.8368 | ||||||
| Diastolic BP (mmHg) | 0.99 (0.95–1.05) | 0.9306 | ||||||
| Creatinine (mg/dl) | 0.89 (0.33–2.45) | 0.8318 | ||||||
| eGFR (ml/min/1.72 m2) | 0.99 (0.97–1.02) | 0.9117 | ||||||
| Uric acid (mg/dl) | 0.68 (0.48–0.96) | 0.0276 | ||||||
| CK-MB (u/l) | 1.01 (0.95–1.06) | 0.8099 | ||||||
| Apo-B (mg/dl) | 0.99 (0.97–0.02) | 0.6418 | ||||||
| Smoking history (years) | 0.89 (0.33–2.39) | 0.8158 | 0.52 (0.07–3.77) | 0.518 | ||||
| Alcoholic history (years) | 2.40 (0.87–6.62) | 0.0896 | 10.23 (1.24–84.47) | 0.031 | ||||
| Family history (years) | 2.87 (0.89–9.23) | 0.0771 | 3.96 (0.91–17.29) | 0.067 | ||||
| D3 (ng/ml) | 0.98 (0.94–1.03) | 0.5086 | ||||||
| 25(OH)D3 (ng/ml) | 0.96 (0.92–0.99) | 0.0284 | ||||||
| 1,25(OH)D3 (ng/ml) | 0.59 (0.37–0.93) | 0.0220 | ||||||
| D2 (ng/ml) | 0.99 (0.94–1.04) | 0.6456 | ||||||
| 25(OH)D2 (ng/ml) | 0.96 (0.87–1.06) | 0.4450 | ||||||
| 1,25(OH)D2 (ng/ml) | 0.50 (0.31–0.82) | 0.0063 | ||||||
| Total 25(OH)D (ng/ml) | 0.96 (0.93–0.99) | 0.0346 | 0.70 (0.42–1.17) | 0.0411 | 0.99 (0.96–1.05) | 0.96 | 0.98 (0.93–1.05) | 0.652 |
| Total 1,25(OH)D(ng/ml) | 0.64 (0.47–0.87) | 0.0040 | 0.64 (0.44–0.94) | 0.022 | 0.58 (0.35–0.95) | 0.031 | ||
Model 1: unadjusted, Model 2: Adjusted for age, sex, smoking history, alcoholic history and family history of diabetes.
Table 5. Logistic regression analysis of T2DM_CAD vs T2DM subjects.
| Factor | Univariate |
Multivariate |
Model 1 (unadjusted) |
Model 2 (adjusted) |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Age | 1.07 (1.01–1.14) | 0.026 | 1.09 (0.98–1.21) | 0.131 | ||||
| Sex (female) | 0.16 (0.05–0.06) | 0.0032 | 0.59 (0.07–4.88) | 0.629 | ||||
| BMI | 0.92 (0.82–1.03) | 0.1411 | ||||||
| HbA1c (%) | 1.29 (0.97–1.73) | 0.075 | 1.43 (1.01–2.02) | 0.0433 | 1.58 (0.92–2.69) | 0.095 | ||
| FBS (mg/dl) | 1.002 (0.99–1.01) | 0.539 | ||||||
| Systolic BP (mmHg) | 1.03 (1.00–1.06) | 0.047 | ||||||
| Diastolic BP (mmHg) | 1.05 (0.99–1.12) | 0.0841 | ||||||
| Creatinine (mg/dl) | 12.74 (1.30–124.5) | 0.0287 | ||||||
| eGFR (ml/min/1.72 m2) | 0.98 (0.96–1.003) | 0.103 | 1.02 (0.98–1.06) | 0.301 | ||||
| Uric acid (mg/dl) | 1.46 (0.99–2.16) | 0.056 | 1.93 (1.03–3.62) | 0.0413 | 2.27 (1.25–4.13) | 0.0069 | 2.82 (1.05–7.55) | 0.0392 |
| CK-MB (u/l) | 8.89 (2.28–34.59) | 0.0016 | ||||||
| Apo-B (mg/dl) | 15.39 (3.89–60.8) | <0.001 | 48.48 (4.89–479.83) | 0.0009 | 26.44 (2.12–329.73) | 0.011 | ||
| Smoking history (years) | 0.702 (0.26–1.90) | 0.487 | ||||||
| Alcoholic history (years) | 1.12 (1.04–1.22) | 0.0051 | 1.11 (1.004–1.24) | 0.0411 | 1.13 (1.03–1.24) | 0.0125 | 1.10 (0.98–1.24) | 0.1109 |
| Family history (years) | 0.98 (0.95–1.01) | 0.1734 | ||||||
| D3 (ng/ml) | 1.00 (0.94–1.05) | 0.994 | ||||||
| 25(OH)D3 (ng/ml) | 0.98 (0.94–1.02) | 0.364 | ||||||
| 1,25(OH)D3 (ng/ml) | 0.64 (0.39–1.03) | 0.068 | ||||||
| D2 (ng/ml) | 0.91 (0.84–0.98) | 0.0083 | ||||||
| 25(OH)D2 (ng/ml) | 1.03 (0.91–1.156) | 0.6803 | ||||||
| 1,25(OH)D2 (ng/ml) | 0.58 (0.33–1.01) | 0.0547 | ||||||
| Total 25(OH)D (ng/ml) | 0.99 (0.95–1.03) | 0.5163 | ||||||
| Total 1,25(OH)D (ng/ml) | 0.69 (0.48–0.99) | 0.0477 | 0.314 (0.15–0.68) | 0.0030 | 0.53 (0.32–0.88) | 0.0130 | 0.29 (0.122–0.67) | 0.0041 |
Model 1: unadjusted, Model 2: Adjusted for age, sex, and alcoholic history.
With control and T2DM_CAD, multivariate analysis showed HbA1c (odds ratio (OR) 1000, 95% confidence interval (CI) 0.005–1000; p < 0.0001), fasting blood sugar (OR 1.25, 95% CI 0.89–1.74; p < 0.0001) and total 1,25(OH)2D (OR 6.04, 95% CI 0.011–19.20; p = 0.0017) were predictor for T2DM_CAD. In addition, we performed force entry multivariate logistic regression analysis to adjust for the factors suspected of contributing to decrease vitamin D metabolites. In the model 1, creatinine (OR 259.85, 95% CI 7.48–1000; p < 0.0021) and decreased total 25(OH)D (OR 0.951, 95% CI 0.359–0.912; p = 0.019) were predictors of T2DM_CAD. In the model 2, after adjustment for other established risk factors: age, female, smoking history, alcoholic history and family history, showed that age (OR 1.114 95% CI 1.024–1.212; p = 0.0118) and total 1,25(OH)2D (OR 0.460, 95% CI 0.242–0.874; p = 0.0177) were predictors of T2DM_CAD (Table 3).
With CAD and T2DM_CAD, multivariate analysis showed HbA1c (odds ratio (OR) 1000, 95% confidence interval (CI) 0.016–1000; p < 0.0001), FBS (OR 1.56, 95% CI 0.960–1.39; p = 0.0061) and total 25(OH)D (OR 0.701, 95% CI 0.42–1.17; p = 0.0411) were predictor for T2DM_CAD. In addition, we performed force entry multivariate logistic regression analysis to adjust the factors suspected of contributing to the decrease of vitamin D metabolites. In the model 1, decreased 1,25(OH)2D (OR 0.64, 95% CI 0.44–0.94; p = 0.022) is predictors of T2DM_CAD. In the model 2, after adjustment for other established risk factors: age, female, smoking history, alcoholic history and family history, showed that alcoholic history (OR 10.23 95% CI 1.24–84.47; p = 0.031) is predictors of T2DM_CAD (Table 4).
With T2DM and T2DM_CAD, multivariate analysis showed uric acid (odds ratio (OR) 1.93, 95% confidence interval (CI) 1.03–3.62; p = 0.0413), alcoholic history (OR 48.48, 95% CI 4.89–479.83; p = 0.0009), CK-MB (OR 1.11, 95% CI 1.004–1.24; p = 0.0411), and total 1,25(OH)2D (OR 0.314, 95% CI 0.15–0.68; p = 0.0030) were predictor for T2DM_CAD. In addition, we performed force entry multivariate logistic regression analysis to adjust for the factors suspected of contributing to decrease vitamin D metabolites. In the model 1, HbA1C (OR 1.43, 95% CI 1.01–2.02; p = 0.0433), uric acid (OR 2.27, 95% CI 1.25–4.13; p = 0.0069), decreased total 1,25(OH)2D (OR 0.53, 95% CI 0.32–0.88; p = 0.0130) were predictors of T2DM_CAD. In the model 2, after adjustment for other established risk factors: age, female, smoking history, alcoholic history, and family history, showed that uric acid (OR 2.82 95% CI 1.05–7.55; p = 0.0392), alcoholic history (OR 26.44, 95% CI 2.12–329.73; p = 0.011), and total 1,25(OH)2D (OR 0.29, 95% CI 0.122–0.67; p = 0.0041) were predictors of T2DM_CAD (Table 5).
Discussion
In the present study, both vitamin D2 and vitamin D3 metabolites levels were measured in Indian subjects associated with type 2 diabetes and coronary artery diseases. As per the previous literature, in Indian subjects prevalence of vitamin D deficiency is 70–100%, despite living in the 8.4° to 37.6° north latitude and sufficient sunlight exposure throughout the year in most of the places9,10,11,12,13,14,15,16,17. Unlike previous studies, our study found that 83% of control subjects were vitamin D sufficient i.e., more than 30 ng/ml 25(OH)D levels and only 13% subjects were insufficient i.e., below <20 ng/ml. Maximum percentage of healthy subjects have normal range (30–40 ng/ml) of 25(OH)D i.e., within optimum levels. Our results differ from the other Indian studies where maximum number of people were vitamin D deficient7,8,9,10,11,12,13,14,15,16,17. This difference might be due to the use of different kind of detection methods. Previously, radio immune assay (RIA) method was used to find out vitamin D levels from Indian subjects. However, in the present study UPLC/APCI/HRMS method has been used to measure vitamin D metabolites in Indian subjects.
Type 2 diabetes and coronary artery diseases are two pathological conditions closely related to each other21,22. Severity of the disease complications generally increases when diabetes coexists with coronary artery diseases. Different type of pathological changes like oxidative stress, advanced end glycation products, hyperglycemia and inflammation are involved in cardiovascular complications in diabetes23. Researchers reported that vitamin D deficiency is associated with insulin resistance in type 2 diabetic patients6,24 and coronary artery disease25. Roy et al. reported that severe vitamin D deficiency is a risk for acute myocardial infraction in Indians14. Recently, Oh et al. showed that deletion of vitamin D receptor in macrophage promotes insulin resistance and monocyte cholesterol transport to accelerate atherosclerosis in mice. This study suggests that vitamin D plays important role in inflammation that causes development of atherosclerosis in type 2 diabetes26. Herrmann et al. reported that serum 25(OH)D is a predictor of macrovascular and microvascular complications in patients with type 2 diabetes27. Several other researchers reported that low levels of vitamin D(25(OH)D3) were associated with asymptomatic CAD in high-risk type 2 diabetic patients with elevated urinary albumin excretion rate28. However, there is no study yet to find the association of vitamin D deficiency with coronary artery diseases in type 2 diabetes. This is the first cross sectional study to compare six vitamin D metabolites and total 25(OH)D, total 1,25(OH)2D in control, T2DM, CAD and T2DM with CAD patients from south part of India.
The present study shows that 83% and 73% of control subjects have sufficient total 25(OH)D (>30 ng/ml) and total 1,25(OH)2D (>11 ng/ml) levels, respectively. However, the percentage of diabetes and diabetes with CAD subjects were increased when we considered insufficient 25(OH)D and 1,25(OH)D2 levels. All the vitamin D metabolites were significantly lowered in T2DM with CAD subjects when compared with control and T2DM subjects. However, only 25(OH)D3 and total 25(OH)D levels were significantly decreased in the T2DM subjects as compared with control subjects. The study also indicated that T2DM patients with total 1,25(OH)2D deficiency are more prone to coronary artery diseases. It was observed that deficiency of vitamin D metabolites were associated with coronary artery diseases among diabetic patients. However, this deficiency is much less for T2DM or CAD alone. Significant negative correlation was observed between total 25(OH)D and HbA1c or FBS but not with BMI. Similar to our study, other studies also showed that total 25(OH)D levels were negatively correlated with HbA1C and blood glucose29 but not with the BMI30. Interestingly, our data found a significant correlation between vitamin D metabolites and the prevalence of CAD among T2DM patients.
To further confirm the causal relationship between lower levels of plasma vitamin D metabolites and T2DM or T2DM with CAD, multivariate logistic regression was performed. The analysis of our results revealed that while lower serum 25(OH)D predicts type 2 diabetes, lower serum 1,25(OH)2D predicts coronary artery diseases in type 2 diabetes. Although, we have not able to investigate the mechanism behind the role of vitamin D on diabetes and CAD, several previous literatures shed light regarding the molecular effect of Vitamin D. 1,25(OH)2D stimulates the expression of insulin receptors, which in turn will affect insulin sensitivity31. 1,25(OH)2D may also enhance insulin sensitivity by activating peroxisome proliferator-activated receptor delta (PPAR-δ), which is a transcription factor regulates the metabolism of fatty acids in skeletal muscle and adipose tissue32. Vitamin D insufficiency has been associated with increased fat infiltration in skeletal muscle and contributes to decrease in insulin sensitivity33. Similar to diabetes, lower concentration of 1,25(OH)2D is associated with athreosclerosis and coronary artery disease through affecting vitamin D receptor signaling. Impairment of VDR signaling accelerates foam cell formation in diabetics26.
Unlike previous studies, the strength of the present study is to measure six vitamin D metabolites by novel and specific mass spectrometry assay in four different groups like control, T2DM, CAD, and T2DM with CAD.
Limitations
Several limitations of our study should be noted. (1) It was a single-center one-point time study from South part of India. (2) We have small sample size in each group. (3) Although we adjusted for potential confounders, we cannot eliminate the possibility of residual confounding factors influencing our results. (4) We have not measured parathyroid hormone and fibroblast growth factor (FGF-23) levels in blood. (5) This study is an observational study and does not address causality.
Conclusion
In conclusion, vitamin D metabolites were decreased in T2DM with CAD subjects as compared with control, T2DM, and CAD subjects. Vitamin D metabolites like 25(OH)D can be used to predict T2DM while 1,25(OH)2D can be used to predict CAD in T2DM. Further studies are required to show that vitamin D supplementation may be beneficial to reduce coronary artery diseases among diabetic patients.
Materials and Methods
Patient Selection
In the present cross sectional study, serum samples from 187 patients, including male and female aged 35–65 years, were randomly taken from the Mediciti Hospital, Hyderabad, India.
Subjects were allocated into four study groups as mentioned below:
Group 1: Control (n = 50).
Group 2: Type 2 diabetes mellitus (T2DM, n = 71).
Group 3: Coronary artery disease (CAD, n = 28).
Group 4: Coronary artery disease with Type 2 diabetes mellitus (T2DM_CAD, n = 38).
Inclusion and Exclusion Criteria
Group 1 Control subjects had no prior history of T2DM, hypertension, coronary artery diseases or any other cardiovascular diseases, and were not taking medication for any chronic medical condition. Fasting blood glucose, HbA1c and blood chemistry were normal. Group 2 (T2DM) included subjects with HbA1c levels ≥ 6.5% as per American Diabetes Association (ADA) guidelines with proven history of T2DM but no other complications. Group 3 (CAD) included subjects with narrowing or blockage of one or more epicardial coronary artery with greater than 25% stenosis shown in coronary angiography and diagnosed by cardiologists3. This group had no prior history of T2DM. Group 4 (T2DM_CAD) included subjects with coronary artery disease as defined for group 3 but patient had HbA1c levels ≥6.5% and prior history of T2DM3. Exclusion criteria defined for this study were clinical or laboratory evidence of liver failure, renal failure (plasma creatinine levels >1.5 mg/dl), type 1 diabetes, cancer, thyroid disease and pregnancy; and subjects on vitamin D treatment therapy were also excluded in this study. The study conforms to the principles outlined in the Declaration of Helsinki and was approved by the Mediciti Ethics Committee (Institutional Ethics Committee), Hyderabad. All patients were given detailed information of the study. Informed consent was obtained from all the subjects.
Selection process for patients with coronary artery diseases
Coronary artery disease patients were identified in the cardiac catheterization unit of Mediciti Hospital. After coronary angiogram, all patients were evaluated by cardiologists in the inpatient setting. If patients were found to have any evidence of CAD, demographic, clinical, and angiographic data were collected from all such patients. Fasting samples were collected prior to the percutaneous coronary intervention or coronary artery bypass graft.
Sample collection process
Clinical history and complete physical examination including measurements of blood pressure were collected and conducted for all the participants. Blood samples were collected by venipuncture after an overnight fast, using Becton Dickison Vacutainer® Red colour coded tubes and blood was allowed to clot by leaving at room temperature for 15 min. After centrifugation at 1500 g for 15 min at 4 °C, serum was collected in 1.2 ml cryo vials and immediately stored at −80 °C until testing.
Clinical and biochemical parameters
Height and weight were obtained using standardised techniques and instruments. The body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters [weight (kg)/Height (m2)]. Fasting blood glucose levels were measured by the Free Style optimum glucometer (Abbott Diabetes Care, Australia). HbA1c levels were measured by the Bayer A1C Now+ Multi test A1C system (Catalog no.08842610). Creatinine, uric acid, total cholesterol, triglycerides, high density lipoprotein (HDL) cholesterol, and CK-MB levels were measured by Siemens automated analyser (Dimension Xpandplus). Estimated glomerular filtration rate (eGFR) calculated from creatinine by using Modification of Diet in Renal Disease (MDRD) formula. Low density lipoprotein (LDL) cholesterol concentrations were calculated by using the Friedewald formula. ApoB (mg/dl) was calculated based on the formula ApoB = −33.12 + 0.675*LDL + 11.95*ln (Triglycerides)34.
Sample preparation and analytical method for estimation of vitamin D metabolites
Serum vitamin D metabolites concentrations were determined by liquid chromatography–Orbitrap mass spectrometry (UPLC/APCI/HRMS). Stock solutions of vitamin D3 and vitamin D2 and its respective metabolites (25(OH)D3, 1,25(OH)2D3, 25(OH)D2 and 1,25(OH)2D2) were prepared in ethanol; Calibration curve (5–200 ng/ml) and quality control sample was prepared from stock solution using methanol; Similarly the dihydrotachysterol 50 ng/ml was used as an internal standard (IS).
100 μl of serum (test sample) was added with 10 ul of IS solution followed by 1 ml of hexane:heptane:acetone in the ratio of 45:40:15. After vertex it properly, the solution was incubated in a shaker for 10 min. The supernatant was separated after centrifugation at 6000 rpm at 4 °C. Supernatant was collected and evaporated using scan vac speed vacuum concentrator. After re-dissolving the concentrate sample in 100 μl of methanol, 10 ul of dissolved sample was used for analysis.
Separation of metabolites was achieved using waters Xselect CSH phenyl hexyl column (150 mm*4.6 mm ID; particle size 3.5 um) with gradient mode. Both mobile phase i.e., mobile phase A (10 mM of ammonium formate in methanol) and mobile phase B (ACN: Acetone: IPA (5:4:1)) were set as follows: (Tmin/% proportion of solvent (B): 0/5, 0–5/95, 5–6/5, and 6–8/5. The flow rate of the mobile phase was 1.00 ml/min while the column temperature and the injection volume was set as 25 °C and 10 μL, respectively. Mass spectrometric detection was carried out by Orbitrap mass analyzer (Exactive Thermo Scientific, Germany) equipped with an atmospheric pressure chemical ionization (APCI) source. The data acquisition was under the control of Xcalibur software. The typical operating source conditions for MS scan in positive ion APCI mode were optimized as follows sheath gas flow rate 65; Aux gas flow rate 20; Discharge current 10.00 μA; Capillary temperature 300 °C; Capillary voltage 50 V; Tube lens voltage 85.0 V; Skimmer voltage 18.00 V and vaporizer temperature 380 °C. For full scan MS mode, the mass range was set at m/z 100–500. All the spectra were recorded under identical experimental conditions and scan rate of 4.9 scan/sec. The full-scan mode across m/z 250–500 that include vitamin D, its metabolites and IS.
For quantification, EICs of [M + H]+ at m/z 385.34649, [M + H − H2O]+ at m/z 383.33084 and [M + H − H2O]+ at m/z 399.32576 for VitD3, 25(OH)D3 and 1,25(OH)D3, respectively with a 5 ppm range centered on the exact m/z value were generated. Similarly, EICs of [M + H − H2O]+ at m/z 379.33593, [M + H − H2O]+ at m/z 395.33084 and [M + H – H2O]+ at m/z 411.32576, and [M + H − H2O]+ at m/z 381.31519 for VitD2, 25(OH)D2 and 1,25(OH)D2 and IS, respectively (Supplemental File: Figs S1–S7). The developed method was validated according to U.S Food and Drug Administration (FDA) guideline for the validation of the bioanalytical method. Details of the method were provided briefly in supplementary file (Supplemental File 1: Table S1).
Statistical analysis
Normally distributed variables were summarized as mean and standard deviation, while non-normally distributed variables were expressed as median and interquartile ranges. One-way analysis of variance (ANOVA) was used to determine whether there are any significant differences between the means of three independent (unrelated) groups of 25(OH)D. Anthropometric and clinical characteristics were presented by 25(OH)D categories (>30, 20–30 and <20 ng/ml). Kruskal-Wallis test was used for comparing non-normally distributed variables with post-hoc Dunn’s multiple comparison test. One-way ANOVA with Bonferroni test was used for normally distributed variable. Kruskal-Wallis test was used to compare vitamin D metabolites levels in control, CAD and T2DM_CAD groups and control, T2DM and T2DM_CAD groups. Spearman rank order correlation was used to find correlation among 25(OH)D, HbA1c, FBS and BMI. Total 25(OH)D [sum of 25(OH)D+ 25(OH)D3] and total 1,25(OH)2D [sum of 1,25(OH)2D2 + 1,25(OH)2D3] were evaluated for overall comparison. Multivariate logistic regression analysis was also performed to test the association of the serum 25(OH)D level with the presence of T2DM (i.e. the dependent variable). Two forced-entry multivariate regression models were performed (i.e. unadjusted and adjusted). The dependent variable was involved as a compound end point: patients with T2DM or CAD or both complications (coded as 1) and patients with neither T2DM nor CAD (coded as 0 i.e. control). Univariate analysis was used to identify covariates as potential confounders on the basis of their significance (p < 0.05). ORs with 95% CIs were used to report the results. Distribution data were presented with Origin 6.0. Box and whisker plots were made with GraphPad Prism version 5.01. Statistical analysis was performed with SAS® V.9.4 software.
Additional Information
How to cite this article: Adela, R. et al. Lower Vitamin D Metabolites Levels Were Associated With Increased Coronary Artery Diseases in Type 2 Diabetes Patients in India. Sci. Rep. 6, 37593; doi: 10.1038/srep37593 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
S.K.B. and R.A. is thankful to Dr. KVS Rao, Head, DDRC (THSTI) for providing necessary support and providing THSTI-DDRC core fund, and DBT for providing Ramalingaswamy fellowship. Authors are thankful to Dr. J S Yadav (Former Director, CSIR-IICT) and Dr. S Chandrasekhar (Director, CSIR-IICT), Hyderabad for facilities and cooperation. Financial support was provided partially by CMET (CSC0110) and AARF (CSC0406) projects. R.M.B and M.M.B are thankful to CSIR, New Delhi, for awarding Senior Research Fellowship and Junior Research Fellowship, respectively.
Footnotes
Author Contributions Conceived and designed the Study: R.A. and S.K.B. Performed the Vitamin D metabolites method design and analysis: R.M.B., M.M.B. and R.S. Analyzed the data: R.A. and G.V. Wrote the paper: R.A., R.M.B., R.S. and S.K.B. Clinical characteristic measurement: RA. Subjects recruitment done by P.N.C.R. and R.A.
References
- Silva A. P., Fragoso A. & Neves P. L. Vitamin D, Type 2 Diabetic and Cardiovascular Disease: Myth or Reality? Int J Diabetes Clin Diagn. 1, 105 (2014). [Google Scholar]
- Guariguataa L. et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pr. 103, 137–149 (2014). [DOI] [PubMed] [Google Scholar]
- Adela R. et al. Hyperglycaemia enhances nitric oxide production in diabetes: a study from South Indian patients. PLoS One 10, e0125270 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 35, 564–571 (2012). [Google Scholar]
- Bartoszewicz Z. et al. Can we accurately measure the concentration of clinically relevant vitamin D metabolites in the circulation? The problems and their consequences. Endokrynol Pol. 64, 238–245 (2013). [PubMed] [Google Scholar]
- Talaei A., Mohamadi M. & Adgi Z. The effect of vitamin D on insulin resistance in patients with type 2 diabetes. Diabetol Metab Syndr. 5, 8 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozos I. & Marginean O. Links between vitamin d deficiency and cardiovascular diseases. Biomed Res Int. 2015, 109275 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie C. J., Lee J. H. & Milani R. V. Vitamin D and cardiovascular disease will it live up to its hype? J Am Coll Cardiol. 58, 1547–1556 (2011). [DOI] [PubMed] [Google Scholar]
- Vishwanath P., Kulkarni P. & Prashant A. Vitamin D deficiency in India: Are we over concerned? Int J HealthAlliedSci. 3, 77–78 (2014). [Google Scholar]
- Goswami R. et al. Prevalence and significance of low 25-hydroxyvitamin D concentrations in healthy subjects in Delhi. Am J Clin Nutr. 72, 472–475 (2000). [DOI] [PubMed] [Google Scholar]
- Harinarayan C. V., Ramalakshmi T., Prasad U. V. & Sudhakar D. Vitamin D status in Andhra Pradesh: a population based study. Indian J Med Res. 127, 211–218 (2008). [PubMed] [Google Scholar]
- Goswami R. et al. Presence of 25(OH)D deficiency in a rural North Indian village despite abundant sunshine. J Assoc Physicians India. 56, 755–757 (2008). [PubMed] [Google Scholar]
- Garg M. K. et al. The relationship between serum 25-hydroxy vitamin D, parathormone and bone mineral density in Indian population. Clin Endocrinol (Oxf). 80, 41–46 (2014). [DOI] [PubMed] [Google Scholar]
- Roy A. et al. Independent association of severe vitamin D deficiency as a risk of acute myocardial infarction in Indians. Indian Heart J. 67, 27–32 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- OKeefe E. L., DiNicolantonio J. J., Patil H., Helzberg J. H. & Lavie C. J. Lifestyle Choices Fuel Epidemics of Diabetes and Cardiovascular Disease Among Asian Indians. Prog Cardiovasc Dis. 58, 505–513 (2016). [DOI] [PubMed] [Google Scholar]
- Khadgawat R. et al. High prevalence of vitamin D deficiency in Asian-Indian patients with fragility hip fracture: a pilot study. J Assoc Physicians India. 58, 539–542 (2010). [PubMed] [Google Scholar]
- Khadgawat R. et al. The Effect of Puberty on Interaction between Vitamin D Status and Insulin Resistance in Obese Asian-Indian Children. Int J Endocrinol. 2012, 173581 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerwekh J. E. Blood biomarkers of vitamin D status. Am J Clin Nutr. 87, 1087S–1091S (2008). [DOI] [PubMed] [Google Scholar]
- Nitta K. Impact of vitamin D metabolism on cardiovascular disease. Int J Clin Med. 2, 531–537 (2011). [Google Scholar]
- Sachs M. C. et al. Circulating vitamin D metabolites and subclinical atherosclerosis in type 1 diabetes. Diabetes Care. 36, 2423–2429 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffner S. M., Lehto S., Ronnemaa T., Pyorala K. & Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 339, 229–234 (1998). [DOI] [PubMed] [Google Scholar]
- Preis S. R. et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the framingham heart study 1950 to 2005. Circulation 119, 1728–1735 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedicino D. et al. Adaptive immunity, inflammation, and cardiovascular complications in type 1 and type 2 diabetes mellitus. J Diabetes Res. 2013, 184258 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y. et al. Blood 25-hydroxy vitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 36, 1422e8 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C. Role of vitamin D in cardiometabolic diseases. J Diabetes Res. 2013, 243934 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J. et al. Deletion of macrophage vitamin D receptor promotes insulin resistance and monocyte cholesterol transport to accelerate atherosclerosis in mice. Cell Reports 10, 1872–1886 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann M. et al. Serum 25-hydroxyvitamin D: a predictor of macrovascular and microvascular complications in patients with type 2 diabetes. Diabetes Care 38, 521–528 (2015). [DOI] [PubMed] [Google Scholar]
- Joergensen C. et al. Vitamin D levels and asymptomatic coronary artery disease in type 2 diabetic patients with elevated urinary albumin excretion rate. Diabetes Care 35, 168–172 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajbaf F. et al. The Association between 25-Hydroxyvitamin D and Hemoglobin A1c Levels in Patients with Type 2 Diabetes and Stage 1-5 Chronic Kidney Disease. Int J Endocrinol 2014, 142468 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemente-Postigo M. et al. Serum 25-Hydroxyvitamin D and Adipose Tissue Vitamin D Receptor Gene Expression: Relationship With Obesity and Type 2 Diabetes. J Clin Endocrinol Metab. 100, E591–E595 (2015). [DOI] [PubMed] [Google Scholar]
- Mitri J. & Pittas A. G. Vitamin D and diabetes. Endocrinol Metab Clin North Am. 43, 205–232 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop T. W. et al. The human peroxisome proliferator-activated receptor delta gene is a primary target of 1alpha, 25-dihydroxyvitamin D3 and its nuclear receptor. J Mol Biol. 349, 248–260 (2005). [DOI] [PubMed] [Google Scholar]
- Gilsanz V. et al. Vitamin D status and its relation to muscle mass and muscle fat in young women. J Clin Endocrinol Metab. 95, 1595–1601 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermans M. P., Ahn S. A. & Rousseau M. F. Discriminant ratio and biometrical equivalence of measured vs. calculated apolipoprotein B100 in patients with T2DM. Cardiovasc Diabetol. 12, 39 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.