Abstract
Background:
The study was designed to assess the role of preoperative neutrophil, lymphocyte, and neutrophil-lymphocyte ratio (NLR) in predicting survival outcomes of ABO-incompatible liver transplantation (LT).
Materials and Methods:
We retrospectively collected the demographic and clinical characteristics of 71 patients with end-stage liver cirrhosis following ABO-incompatible LT in this study. Kaplan–Meier survival analysis and Cox multiple factors regression analysis were performed to determine the independent risk factors from preoperative blood parameters for poor prognosis.
Results:
The 1-, 3-, and 5-year overall survival were 94.9%, 80.0%, and 80.0% in the normal NLR group, respectively, and 59.4%, 55,4%, and 55.4% in patients with up-regulated NLR, respectively (P = 0.001). Furthermore, no significant difference was observed on post-LT complications between normal NLR and high-NLR groups. The high NLR was identified as the only independent prognostic risk factor for recipient survival (P = 0.015, 95% confidence interval = 3.573 [1.284–9.943]).
Conclusion:
The preoperative high NLR could be considered as a convenient and available indicator for selecting ABO-incompatible LT candidates.
Keywords: ABO-incompatible liver transplantation, hepatitis B, liver failure, neutrophil-lymphocyte ratio
INTRODUCTION
End-stage liver cirrhosis (ESLC) is a fatal clinical condition and frequently accompanied with mental alteration, ascites, jaundice, coagulopathy, and persistent deterioration of liver function.[1] Once a complication of ESLC develops, the 5-year survival rate decreased to low than 20%, and patients should be recommended to take liver transplantation (LT).[2] Advances in transplantation have improved long-term survival rates to more than 70% at 5 years after LT.[3] In the case of life-threatening hepatic failure and donation severe shortage, ABO-incompatible LT (ABO-i LT) has been suggested as an optimal option for rescuing life.
Recently, some parameters from blood were identified as promising markers for prognosis of patients with diverse diseases. Among them, the elevated preoperative neutrophil-lymphocyte ratio (NLR) is a useful predictor for overall survival rates in colorectal cancer, hepatocellular carcinoma (HCC), or nontumoros diseases.[4,5,6] In addition, the patients characterized by thrombocytopenia and declining platelet counts were associated with an ominous prognosis.[7,8] Nagai et al. demonstrated that the restoration of posttransplant absolute lymphocyte count can be a novel prognostic factor for the recurrence of hepatitis C and HCC.[9,10] Hellberg and Kδllskog previously revealed that neutrophil contributed to mediating postischemic kidney dysfunction.[11] Given this, the study was designed to determine the effect of presurgery blood parameters on outcomes of patients with ESLC after ABO-i LT.
MATERIALS AND METHODS
Patients and blood parameters collection
A total of 84 ESLC patients undergoing ABO-i LT from the first affiliated hospital, Zhejiang University School of Medicine between January, 2004, and December, 2011, were enrolled in our study. The AB blood type recipients and O blood type donors were excluded from the study. An NLR ≥5 was considered as a significant elevation according to previously reported cutoff.[12] The cutoff of neutrophil, lymphocyte count, and platelet were acquired according to their median, respectively. Patients with preoperative sepsis, autoimmune hepatitis, HCC, steroids administration before LT, illicit drug abuse, and loss to follow-up were excluded from our study. ESLC was defined as decompensated chronic liver cirrhosis. All LT were performed following obtaining informed consent from all patients, and this study was approved by the Ethical Review Board of the first affiliated hospital of the medical school of Zhejiang University (No. 2012ZX10002-017).
Management for patients following liver transplantation
The improved strategy in our center for reducing anti-ABO antibodies consisted of rituximab, basiliximab, and intravenous immunoglobulin (IVIG). Rare ABO-i LT patients received splenectomy were due to the serious hypersplenism which commonly diagnosed by stubborn decreasing of white blood cell, lymphocyte, platelet, and neutrophil. Our immunosuppression protocol following ABO-i LT adopted a standard protocol of quadruple regimen consisted of basiliximab, methylprednisolone, tacrolimus, and mycophenolate mofetil (MMF). The median serum tacrolimus concentration was 8.9 ± 4.3 ng/ml in the high-NLR group, and 9.2 ± 6.5 in the normal NLR group presenting no significant difference between two groups. MMF was administrated with fixed dosage (0.5 g Bid). Our immunosuppression protocol following ABO-i LT adopted an standard protocol of quadruple regimen. Basiliximab was injected twice at postoperative day 1 and 4. Methylprednisolone (initially 1000 mg then tapered and withdraw at 1st month), tacrolimus (initially plasma target level: 10–12 ng/ml and titrated down to 8–10 ng/ml), and MMF (500 mg twice daily) were administered for maintaining the immunosuppressive effect after surgery. Furthermore, piperacillin-tazobactam, fluconazole, and ganciclovir were adopted postoperatively as an anti-infection strategy. Patients with hepatitis B virus were intravenously injected with lamivudine and hepatitis B immunoglobulin to prevent the recurrence of hepatitis B after LT.
Statistical analysis
The quantitative and qualitative variables were presented as mean with standard deviation and frequency, respectively. Fisher's exact test, independent sample t-test, and Pearson's χ2 test were performed to evaluate the differences in the clinicopathologic factors of ABO-i LT patients with high and normal NLRs. The Kaplan–Meier method and Cox proportional hazard model analysis were used to determine the risk factors for poorer prognosis. The patient characteristics were valued using univariate analysis first, and then risk factors with P < 0.1 were selected and entered into Cox proportional hazard model analysis to estimate their hazard ratio. The software program SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) was used for analyzing data, and statistical significance was adopted at P < 0.05.
RESULTS
Patient demographics and outcomes
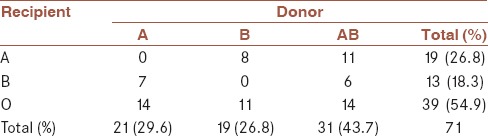
Of the 84 adult recipients who underwent emergency ABO-i LT for ALF at our hospital, 13 (15.5%) were excluded (seven recipients had steroids administration before LT, three were loss to follow-up, two were autoimmune hepatitis, and one had drug abuse). The study populations consisted of 47 males and 24 females and the median age at diagnosis was 47.9 years. All patients were caused by hepatitis B infection. Of 71 patients, 13 (18.3%) received preoperative artificial liver support, three (4.2%) underwent splenectomy along with LT [Table 1]. The blood type combinations between donors and recipients included the following pairings: A to B, O; AB to A, B, O; B to A, O; whereas AB blood type recipients and O blood type donors were excluded from the study [Table 2].
Table 1.
Patient demographics and clinical characteristics
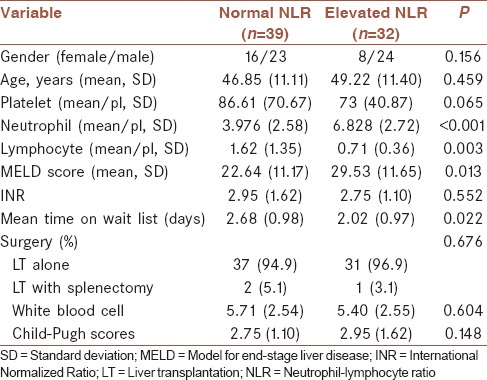
Table 2.
Blood type combinations between donors and recipients
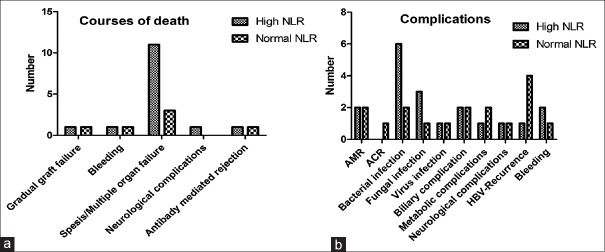
The median follow-up period was 41.2 months and the courses of death during study period included multiple organ failure/sepsis, cerebral hemorrhage, antibody-mediated rejection (AMR), neurological complications, and gradual graft failure. Among them, sepsis was the main death factor [Figure 1a]. Of 14 dead patients were due to sepsis, 11 (78.6%) with high NLR and three with normal NLR. The 1-, 3-, and 5-year overall survival rates of the study population were 78.8%, 68.0%, and 68.0%, respectively.
Figure 1.
The relationship of complications, courses of death, and neutrophil-lymphocyte ratio. (a) Suggested that sepsis was the main course of death, specially, in the high neutrophil-lymphocyte ratio group (P = 0.025), (b) the infection complications was more in the high neutrophil-lymphocyte ratio group than in the normal group but presented no statistical significance (P = 0.056)
Correlation between blood parameters and outcomes after ABO-incompatible liver transplantation
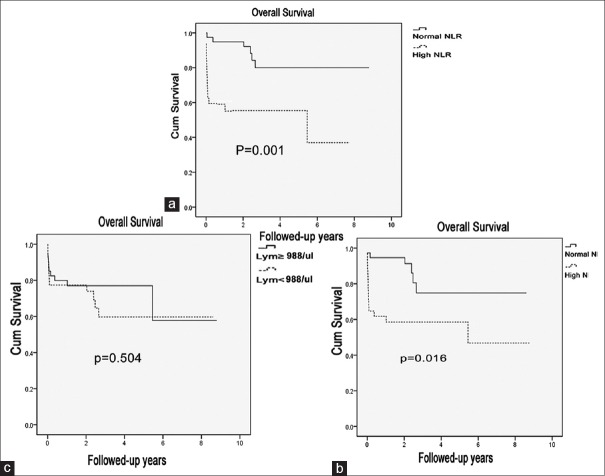
The abnormal renal function was defined by high creatinine (>133 μmol/L). We found that the patients with high serum creatinine were respectively 26 in the high-NLR group and seven in the normal NLR group, but LT receptors with pretransplant high serum creatinine did not presented poorer prognosis including survival outcomes and complications. Of all factors, only high NLR had remarkable effect on survival outcomes after ABO-i LT and related results were presented in Table 3. The 1-, 3-, and 5-year overall survival were 94.9%, 80.0% and 80.0% in the normal NLR group respectively, and 59.4%, 55,4% and 55.4% in patients with up-regulated NLR respectively [P = 0.001, Figure 2a]. We also analyzed the effect of elevated NLR on complications and found none correlation between them [Figure 1b].
Table 3.
Univariate and multivariate analysis of factors affecting overall survival after ABO-incompatible liver transplantation
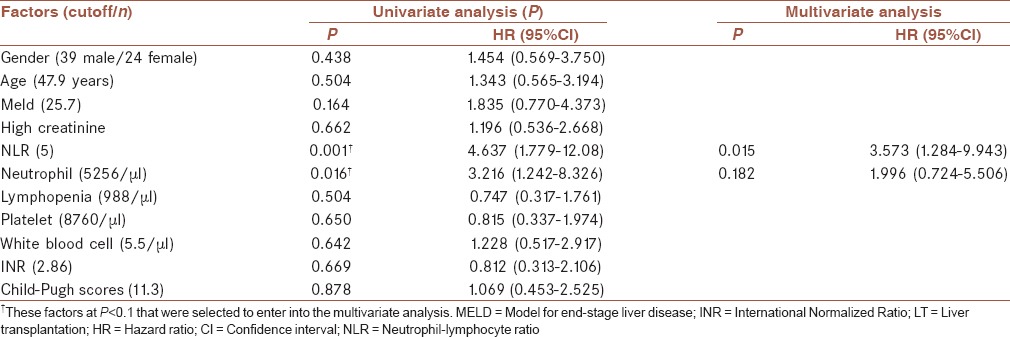
Figure 2.
Kaplan–Meier chart comparing both overall survivals for patients classified according to the neutrophil-lymphocyte ratio (a), neutrophil count (b), and lymphocyte count (c) preoperatively. The curves presented different survival rates of patients with ABO-incompatible liver transplantation with different preoperative neutrophil-lymphocyte ratio or neutrophil count, but bot with different lymphocyte count
The role of neutrophil and lymphocyte in neutrophil-lymphocyte ratio
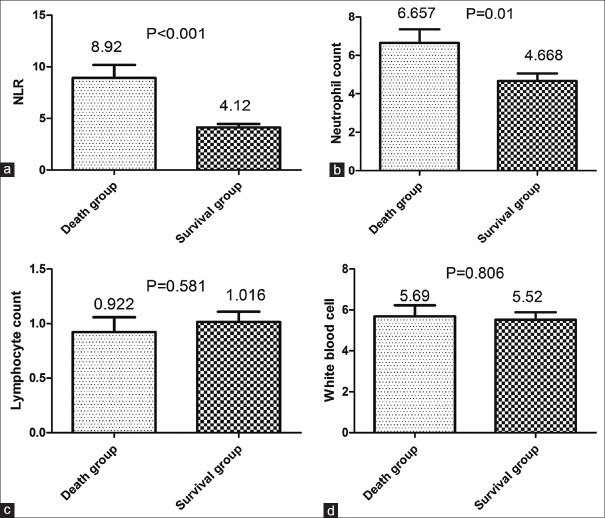
The median counts of neutrophil and lymphocyte were significantly different between the elevated NLR group and the normal NLR group (P < 0.001, P = 0.003 respectively). The 1-, 3- and 5-year recipient survival rates were 61.8%, 58.5% and 58.5%, respectively, in the high neutrophil group, and 94.6%, 74.8% and 74.8%, respectively in the low-neutrophil group [P = 0.016, Figure 2b]. However, we found that the 1-, 3- and 5-year overall survival rates were 77.4%, 59.7% and 59.7% in the lymphopenia group, respectively, and 79.9%, 77.1% and 77.1% in the normal-lymphocyte group, respectively [P = 0.504, Figure 2c]. In addition, we further divided patients into a death group and a survival group and found that there were a significant difference in NLR and neutrophil count whereas not in lymphocyte count and white blood cell [Figure 3]. These results suggested that the high-neutrophil count was the main cause for high NLR inducing poorer recipient survival. In addition, high neutrophil and high NLR presented P < 0.1 in univariate analysis; these factors were further selected and entered into Cox proportional hazard model analysis to estimate their hazard ratio, and only high NLR remains statistical significance [Table 3].
Figure 3.
The difference of pretreatment neutrophil-lymphocyte ratio (a), neutrophil count (b), lymphocyte count (c) and white blood cell (d), between the survival and death groups in the retrospective cohort. There were a significant difference in neutrophil-lymphocyte ratio and neutrophil count, whereas not in lymphocyte count and white blood cell
DISCUSSION
To date, most of the researchers payed attention to preexisting anti-ABO antibody titer that neglects other potential predictors. Moreover, Egawa et al. found the preoperative high anti-ABO IgM did not have any significance in predicting the frequency of AMR and 5-year survival rate following ABO-i LT.[13]
Recently, several studies reported that NLR could predict the long-term outcomes of patients with HCC after LT and even was selected to challenge the Milan criteria as a precise predictive marker.[5,14] NLR was a miniature of systemic inflammation and easily calculated by routine examine of peripheral blood samples. Our results presented that elevated NLR was significantly associated with poorer both overall survival and graft survival, in our study population.
The reactive neutrophilia and lymphocytopenia were a physiological response to the immune system to a variety of stressful events, so the high preoperative NLR not only showed the presence of immune dysfunction but also the severity of affliction. The immune dysfunction of patients with ESLC undoubtedly promoted postsurgery infection. Besides, in high-NLR group, patients presented more serious lymphocytopenia that increases the susceptibility to infection. Furthermore, the sepsis rather than AMR was the crucial cause of patients death after ABO-i LT in the study and a previously reported literature,[15] which suggested that the increased postoperative infection diseases are the mechanism underlying high NLR influencing survival outcomes of ABO-i LT, and the carefully perioperative management for preventing infection is very important. Although the accurate mechanism underlying NLR influencing survival outcomes in various diseases was not clear, our data still provided some hint.
We found that high NRL group presented a higher model for end-stage liver disease (MELD) score comparing with the normal NLR group. In the previously published literature, LT patients with higher MELD score presented poorer survival outcomes, but the cutoff of high MELD score was extraordinary different in the different LT cohort. In our previously published data, we found MELD score ≥28 was an independent risk factor. Therefore, we added the analysis of MELD score ≥28 predicting prognosis of ABO-i LT recipients. We found that ABO-i LT recipients with MELD score ≥28 presented a significant trend of poorer graft survival outcomes (P = 0.047, less than MELD score ≥25.7). In addition, by the Cox proportional hazard model analysis, we defined that high MELD score could not interfere in NLR as a predictor for ABO-i LT recipients.
The combination of plasma exchange PE, graft local infusion (GLI), splenectomy, rituximab, and IVIG is a standard protocol of reducing anti-ABO antibody titer and the incidence of AMR. However, recently several studies presented some different viewpoints. Raut et al. reported that preoperative rituximab could effectively prevented AMR irrespective of splenectomy, and not any immunological benefit was obtained due to splenectomy during the initial 8 weeks.[16] Ikegami et al. indicated that the new protocol using PE, rituxamab, and IVIG without GLI in four cases after ABO-i living donor LT seemed to be a safe treatment because GLI leaded to various catheter-associated complications.[17] In addition, Urbani et al. and Ikegami et al., respectively reported that AMR was highly associated with postoperative rebound elevation of isoagglutinin titer, and high-dose IVIG was very effective.[18,19] In this study, all of the voluntary donor livers come from the accidentally dead people, so we were not sure the blood type pairs of LT before the operation. In addition, receptors were with a life-threatening condition. The two reasons urged us to make an emerge ABO-i LT without PE. All patients were administered the improved protocol, and there were only two episodes of AMR presented in the study. The low incidence of AMR provided a possibility for rituximab totally substituting for PE and highlighted the role of high-dose IVIG and subsequent quadruple immunosuppressive scheme involving steroids in treatment and/or prophylaxis of severe AMR. The small sample size is a limitation in this study, the larger sample size and the further investigation for the effect of high NLR and the improved protocol on long-term survival outcomes are needed in future study.
CONCLUSION
We found that high NLR was the independent risk factor for poorer overall survival after ABO-i LT, which might be selected as an index for rearranging the ABO-i LT candidates list. The high neutrophil count rather than lymphopenia contributed to the effect of elevated NLR on postoperative survival outcomes. Furthermore, the improved protocol for decreasing antibody titer is worthy to be recommended.
Financial support and sponsorship
This work was supported by National S and T Major Project (No. 2012ZX10002-017), National Natural Science Foundation of China (81373160, 81302074) and NSFC for Innovative Research Group (81121002) and National Natural Science Foundation of Zhejiang Province (LQ13H160004), Scientific Plan of Medicine Care in Zhejiang Province (20147283).
Conflicts of interest
The authors have no conflicts of interest.
AUTHORS’ CONTRIBUTION
ShZ and LZ contributed in the conception of the work, BL and LG, ZhZh conducted the study, revised the draft, and others fished the data collection and analysis.
REFERENCES
- 1.Liou IW. Management of end-stage liver disease. Med Clin North Am. 2014;98:119–52. doi: 10.1016/j.mcna.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Ginés P, Quintero E, Arroyo V, Terés J, Bruguera M, Rimola A, et al. Compensated cirrhosis: Natural history and prognostic factors. Hepatology. 1987;7:122–8. doi: 10.1002/hep.1840070124. [DOI] [PubMed] [Google Scholar]
- 3.Aranzana EM, Coppini AZ, Ribeiro MA, Massarollo PC, Szutan LA, Ferreira FG. Model for End-Stage Liver Disease, Model for Liver Transplantation Survival and Donor Risk Index as predictive models of survival after liver transplantation in 1,006 patients. Clinics (Sao Paulo) 2015;70:413–8. doi: 10.6061/clinics/2015(06)05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sugiura T, Uesaka K, Kanemoto H, Mizuno T, Okamura Y. Elevated preoperative neutrophil-to-lymphocyte ratio as a predictor of survival after gastroenterostomy in patients with advanced pancreatic adenocarcinoma. Ann Surg Oncol. 2013;20:4330–7. doi: 10.1245/s10434-013-3227-8. [DOI] [PubMed] [Google Scholar]
- 5.Li MX, Liu XM, Zhang XF, Zhang JF, Wang WL, Zhu Y, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: A systematic review and meta-analysis. Int J Cancer. 2014;134:2403–13. doi: 10.1002/ijc.28536. [DOI] [PubMed] [Google Scholar]
- 6.Torun S, Tunc BD, Suvak B, Yildiz H, Tas A, Sayilir A, et al. Assessment of neutrophil-lymphocyte ratio in ulcerative colitis: A promising marker in predicting disease severity. Clin Res Hepatol Gastroenterol. 2012;36:491–7. doi: 10.1016/j.clinre.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Patel N, Mody GM. Acute presentation of thrombocytopaenia in systemic lupus erythematosus is associated with a high mortality in South Africa. Lupus. 2014;23:204–12. doi: 10.1177/0961203313512009. [DOI] [PubMed] [Google Scholar]
- 8.Moreau D, Timsit JF, Vesin A, Garrouste-Orgeas M, de Lassence A, Zahar JR, et al. Platelet count decline: An early prognostic marker in critically ill patients with prolonged ICU stays. Chest. 2007;131:1735–41. doi: 10.1378/chest.06-2233. [DOI] [PubMed] [Google Scholar]
- 9.Nagai S, Abouljoud MS, Kazimi M, Brown KA, Moonka D, Yoshida A. Peritransplant lymphopenia is a novel prognostic factor in recurrence of hepatocellular carcinoma after liver transplantation. Transplantation. 2014;97:694–701. doi: 10.1097/01.TP.0000437426.15890.1d. [DOI] [PubMed] [Google Scholar]
- 10.Nagai S, Yoshida A, Kohno K, Altshuler D, Nakamura M, Brown KA, et al. Peritransplant absolute lymphocyte count as a predictive factor for advanced recurrence of hepatitis C after liver transplantation. Hepatology. 2013;10:1002. doi: 10.1002/hep.26536. [DOI] [PubMed] [Google Scholar]
- 11.Hellberg PO, Källskog TO. Neutrophil-mediated post-ischemic tubular leakage in the rat kidney. Kidney Int. 1989;36:555–61. doi: 10.1038/ki.1989.230. [DOI] [PubMed] [Google Scholar]
- 12.Bertuzzo VR, Cescon M, Ravaioli M, Grazi GL, Ercolani G, Del Gaudio M, et al. Analysis of factors affecting recurrence of hepatocellular carcinoma after liver transplantation with a special focus on inflammation markers. Transplantation. 2011;91:1279–85. doi: 10.1097/TP.0b013e3182187cf0. [DOI] [PubMed] [Google Scholar]
- 13.Egawa H, Teramukai S, Haga H, Tanabe M, Fukushima M, Shimazu M. Present status of ABO-incompatible living donor liver transplantation in Japan. Hepatology. 2008;47:143–52. doi: 10.1002/hep.21928. [DOI] [PubMed] [Google Scholar]
- 14.Wang GY, Yang Y, Li H, Zhang J, Jiang N, Li MR, et al. A scoring model based on neutrophil to lymphocyte ratio predicts recurrence of HBV-associated hepatocellular carcinoma after liver transplantation. PLoS One. 2011;6:e25295. doi: 10.1371/journal.pone.0025295. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Egawa H, Ohdan H, Haga H, Tsuruyama T, Oike F, Uemoto S, et al. Current status of liver transplantation across ABO blood-type barrier. J Hepatobiliary Pancreat Surg. 2008;15:131–8. doi: 10.1007/s00534-007-1298-2. [DOI] [PubMed] [Google Scholar]
- 16.Raut V, Mori A, Kaido T, Ogura Y, Taku I, Nagai K, et al. Splenectomy does not offer immunological benefits in ABO-incompatible liver transplantation with a preoperative rituximab. Transplantation. 2012;93:99–105. doi: 10.1097/TP.0b013e318239e8e4. [DOI] [PubMed] [Google Scholar]
- 17.Ikegami T, Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Harada N, et al. Rituximab, IVIG, and plasma exchange without graft local infusion treatment: A new protocol in ABO incompatible living donor liver transplantation. Transplantation. 2009;88:303–7. doi: 10.1097/TP.0b013e3181adcae6. [DOI] [PubMed] [Google Scholar]
- 18.Urbani L, Mazzoni A, De Simone P, Catalano G, Coletti L, Montin U, et al. Treatment of antibody-mediated rejection with high-dose immunoglobulins in ABO-incompatible liver transplant recipient. Transpl Int. 2007;20:467–70. doi: 10.1111/j.1432-2277.2006.00447.x. [DOI] [PubMed] [Google Scholar]
- 19.Ikegami T, Taketomi A, Soejima Y, Iguchi T, Sanefuji K, Kayashima H, et al. Successful ABO incompatible living donor liver transplantation in a patient with high isoagglutinin titer using high-dose intravenous immunoglobulin. Transplant Proc. 2007;39:3491–4. doi: 10.1016/j.transproceed.2007.09.028. [DOI] [PubMed] [Google Scholar]