Sir,
Hydatid disease is a parasitosis, and it is endemic in many sheep-rearing regions in the world, especially in the Middle East and Mediterranean countries.[1,2,3] The reported annual morbidity from the disease in humans is 1.04-2.4 per 1,000,000, while the actual rates are supposed to be more than twice, this difference is probably due to the underreporting of data.[4] The liver (65-75%) and lungs (10-25%) are the organs most commonly involved, followed by peritoneal cavity (8-18%), spleen (2-3%), kidneys (1-4%), uterus and adnexa (0.5-1%), retroperitoneum (0.5-1%), pancreas (0.5-0.8%),[5] subcutaneous tissue (1-2%),[6] mediastinum (0.1-0.5%),[7] gall bladder (≤1%),[8] brain (2%),[9] seminal vesicle,[10] spinal cord,[11] and others (0.1-3%).[5]
A 15-year retrospective study of the cases of hydatid disease treated between January 2000 and December 2014 was done at Sher-i-Kashmir Institute of Medical Sciences (SKIMS), Srinagar, Jammu and Kashmir, India, and associated SKIMS Medical College, a tertiary care center. The main thrust of the study was to know the incidence of atypical forms and infrequent location of the disease and to evaluate diagnostic and therapeutic modalities. These atypical locations included the kidneys, spleen, pancreas, peritoneum, retroperitoneum with extension in the spinal medulla, gallbladder wall cyst, bone, brain, ovary, seminal vesicle, and muscle.
The diagnosis was established by the history, clinical examination, complete blood counts, liver and kidney function tests, serological tests (enzyme-linked immunosorbent assay and indirect hemagglutination test), chest x-ray, ultrasound and magnetic resonance imaging (MRI), or contrast enhanced computerized tomography (CECT). CT was applied in all of our patients as the diagnostic tool of choice [Figures 1–4].
Figure 1.
CECT abdomen of the patient showing cystic lesion in spleen with a calcified wall that on operation proved to be hydatid cyst
Figure 4.
Plain CT scan head of the patient after removal of hydatid cyst showing residual cavity
Figure 2.

MRI brain showing cystic mass in left occipital region with mass effect and midline shift
Figure 3.
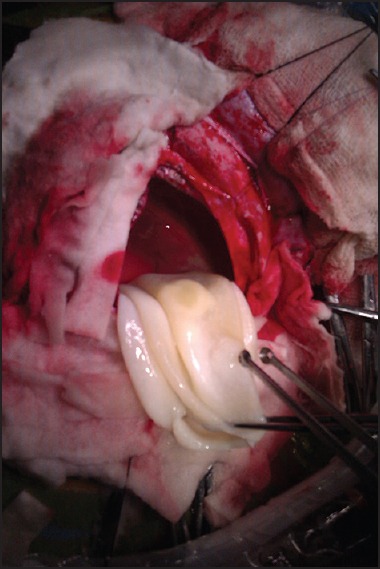
Intraoperative picture of removal of hydatid brain
The treatment for all the patients was surgical. All the patients received preoperative and postoperative albendazole chemotherapy. Out of 527 patients of hydatid disease studied over a period of 15 years, 38 (7.2%) patients had hydatid cyst present at atypical location, with their ages ranging from 17 years to 69 years (mean 36.2 years). Spleen was the most common organ involved when cases of liver [359 (68.1%)] and lung [106 (20.1%)] hydatids were excluded. There were 11 (2.08%) cases of hydatid spleen followed by cases involving pancreas 6 (1.13%); peritoneum 6 (1.13%); brain 4 (0.75%); spinal cord 2 (0.3%); subcutaneous tissue 2 (0.3%); and kidney, ovary, seminal vesicle, mediastinum, muscle, gall bladder, bone 1 (0.19%) case each.
Nonspecific abdominal pain and a nontender palpable abdominal lump were the most predominant symptoms; other symptoms varied according to the localization of the cyst. Palpable lump was also a presenting symptom in the patients with subcutaneous and muscle cysts. Seven patients with atypical locations were asymptomatic, which included three cases with peritoneal hydatid, three cases of isolated splenic hydatid, and one case of renal hydatid. The patients with brain and spinal hydatid presented with neurological symptoms, while the one with seminal vesicle hydatid presented with lower urinary tract symptoms (LUTS). Eosinophilia was observed in 24 out of 38 patients. Medical treatment (albendazole 10 mg/kg) was given preoperatively followed by definitive surgical treatment followed by postoperative chemotherapy for 3 months. None of the patients with hydatid disease at atypical location had a recurrence after the treatment.
Atypical localization of hydatid disease usually poses a diagnostic dilemma. It is well known that specific local or general symptoms and signs of hydatid disease do not exist. The majority of cases are diagnosed following incidental findings at imaging examinations done for some unrelated complaints. The uncommon localization frequently causes diagnostic problems, and specific diagnostic tests do not have 100% reliability in these cases.[10] Surgery is the treatment of choice when location of the cyst is atypical, conservative approaches are used less often.
We conclude that a differential diagnosis of hydatid cyst should be considered whenever a cystic lesion is encountered anywhere in the body depending upon the level of endemicity of the disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dhaliwal RS, Kalkat MS. One-stage surgical procedure for bilateral lung and liver hydatid cysts. Ann Thorac Surg. 1997;64:338–41. doi: 10.1016/S0003-4975(97)00475-X. [DOI] [PubMed] [Google Scholar]
- 2.Topçu S, Kurul IC, Taştepe I, Bozkurt D, Gülhan E, Cetin G. Surgical treatment of pulmonary hydatid cysts in children. J Thorac Cardiovasc Surg. 2000;120:1097–101. doi: 10.1067/mtc.2000.110181. [DOI] [PubMed] [Google Scholar]
- 3.Sayek I, Yalin R, Sanaç Y. Surgical treatment of hydatid disease of the liver. Arch Surg. 1980;115:847–50. doi: 10.1001/archsurg.1980.01380070035007. [DOI] [PubMed] [Google Scholar]
- 4.Arambulo P., 3rd Public health importance of cystic echinococcosis in Latin America. Acta Trop. 1997;67:113–24. doi: 10.1016/s0001-706x(97)00049-1. [DOI] [PubMed] [Google Scholar]
- 5.Palanivelu C. Laparoscopic management of hydatid cysts of liver. In: Palanivelu C, editor. Art of Laparoscopic Surgery: Textbook and Atlas. Jaypee Publishers; 2007. pp. 757–83. [Google Scholar]
- 6.Zulfikaroglu B, Koc M, Ozalp N, Ozmen MM. A rare primary location of echinococcal disease: Report of a case. Ups J Med Sci. 2005;110:167–71. doi: 10.3109/2000-1967-078. [DOI] [PubMed] [Google Scholar]
- 7.Kabiri el H, Zidane A, Atoini F, Arsalane A, Bellamari H. Primary hydatid cyst of the posterior mediastinum. Asian Cardiovasc Thorac Ann. 2007;15:e60–2. doi: 10.1177/021849230701500526. [DOI] [PubMed] [Google Scholar]
- 8.Raza MH, Harris SH, Khan R. Hydatid cyst of gall bladder. Indian J Gastroenterol. 2003;22:67–8. [PubMed] [Google Scholar]
- 9.Greenberg SM. 1st ed. New York: Thieme Medical Publisher; 2001. Handbook of Neurosurgery; pp. 238–9. [Google Scholar]
- 10.Safioleas M, Stamatakos M, Zervas A, Agapitos E. Hydatid disease of the seminal vesicle: A rare presentation of hydatid cyst. Int Urol Nephrol. 2006;38:287–9. doi: 10.1007/s11255-006-6652-9. [DOI] [PubMed] [Google Scholar]
- 11.Drimousis PG, Stamou KM, Koutras A, Tsekouras DK, Zografos G. Unusual site of recurrent musculoskeletal hydatid cyst: Case report and brief review of the literature. World J Gastroenterol. 2006;12:5577–8. doi: 10.3748/wjg.v12.i34.5577. [DOI] [PMC free article] [PubMed] [Google Scholar]


