Abstract
Background:
Treatment of established cases of Volkmann's ischemic contracture (VIC) of upper limb is very tedious. Since the period of Volkmann, various experimental works are being performed for its treatment, but none are effective. Disabilities from nerve palsy and hand muscle paralysis are more problematic than any other deformity in VIC. To solve these problems, we conducted a study to see the result of neurolysis of median and ulnar nerve and their subcutaneous placement in established cases of VIC.
Materials and Methods:
Twelve cases of established VIC operated between July 2007 and August 2010 with complete records and followup were included in the study. VIC of lower limb and contracture of nonischemic etiology were excluded from the study. Their evaluation was done by the British Medical Research Council grading system for sensory and motor recovery. Followup was done for an average period of 24.3 months (range 15-30 months) (the average age was 8.3 years).
Results:
To study the results, we divided the cases into two series. One group consisted of cases which were operated within 6 months from onset of VIC. The second group consisted of cases which were operated after 6 months from onset of VIC. Our results revealed that there was no statistically significant difference between the two groups operated, though both had significant improvement in motor and sensory recovery in both median and ulnar nerve distribution.
Conclusions:
Neurolysis of the nerves definitely improved the outcome for motor and sensory components of median and ulnar nerves but the timing of the surgery did not play a role in the outcome contrary to the clinical assumption. This study can serve as a template and further such studies could help us find the answer to a long standing issue.
Keywords: Median nerve, motor, neurolysis, retinaculum, sensory, ulnar nerve
MeSh terms: Median nerve, ulnar nerve, compartment syndromes, forearm
INTRODUCTION
Volkmann's ischemic contracture (VIC) is a well-known disease in medical science today, although its existence in literature was since when it was first described by Hildebrand1 when he quoted Hamiltons’ cases (recorded in 1850), followed by Volkmann2 in his famous article. From that period, various authors, namely Thomas (1909),3 Murphy,4 Page,5 Jones,6 Seddon7 and Tsuge (1975)8 have done pioneering experiments to understand the etiology, pathogenesis, management, and most importantly its prevention, but no author till date has claimed a certain method of cure. VIC usually affects children of younger age group and occurs most frequently following mismanaged trauma of upper limb. In developing countries, due to lack of education and lack of awareness, most people take treatment by massage and application of tight bandages and bamboo-stick by bonesetter (pahalwans). This is followed by acute compartment syndrome9 and then VIC. Once established, despite all sophisticated conservative and surgical management, VIC leads to permanent or partial disability to the limb. Among the various anatomical structures involved, nerves and muscles are severely affected. Affection of nerves is both from ischemic pathology (Thomas 1909),3 as well as compressive effect of fibrotic muscle,10 leading to loss of sensation in the distribution of median and ulnar nerve and intrinsic muscle paralysis, which are major problems for a reconstructive surgeon.11 Various causes such as fracture of supracondylar humerus, fracture of both bone forearm, burns, crush injury, aneurysms, hematomas, and forearm fractures have been recognized as causing a peculiar combination of venous and arterial insufficiency which results in delayed appearance of a nerve palsy in hand.12,13,14 Most authors have focused primarily on the forearm flexion contracture, but it is the nerve palsy which is responsible for major functional disability of hand.15 We studied the results of neurolysis and subcutaneous placement of median and ulnar nerve in established cases of VIC retrospectively and prospectively.
MATERIALS AND METHODS
Fifteen cases of established VIC presented between July 2007 and August 2010 comprised these study group. Three were lost to followup, so the study was done only in 12 cases. Established VIC of upper limb with complete records and followup were included in the study. VIC of lower limb and contracture of nonischemic etiology were excluded from the study. Detailed preoperative, postoperative evaluation was done; results were recorded and followup was done at 2 monthly intervals. Classification of VIC cases was done according to Tsuge8 system into three types and these three types are discussed in the following sections:
Mild (localized) type
In this, only a part of flexor digitorum profundus is degenerated. Clinically, it presents as flexion contractures of only 2–3 fingers, most frequently the middle and ring fingers. Usually there is no sensory loss, but if present, it is only slight. If muscle degeneration is slightly more extensive, the little and index fingers may also be affected, also sometimes with contracture of the thumb.
Moderate (classic) type
In this type, the flexor digitorum profundus and flexor pollicis longus are primarily involved and the superficial muscles – the flexor digitorum superficialis and the wrist flexors (flexor carpi radialis and flexor carpi ulnaris) may also be involved. There is flexion contracture of all the fingers and thumb, often with flexion deformity of the wrist. There is also sensory disturbance of the median and ulnar nerves. Intrinsic paralysis causes claw hand deformity.
Severe type
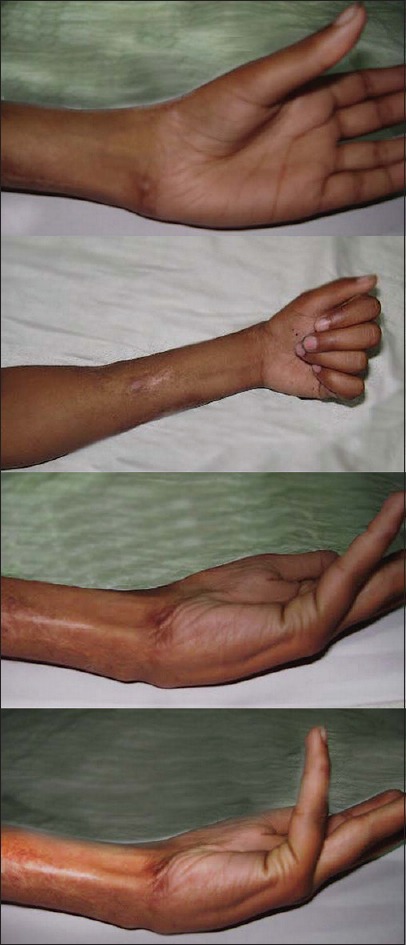
Here, the muscle degeneration involves all the flexors, along with partial involvement of the extensors. There are severe neurological disturbance and severe contractures. In many cases, malunion or nonunion of fracture forearm bones occurs. This group also includes long standing cases, which originally had moderate VIC, but subsequently develop joint contractures. It also includes unsuccessful surgical cases [Figures 1 and 2].
Figure 1.

Clinical photograph showing signs of Volkmann's ischemic contracture
Figure 2.
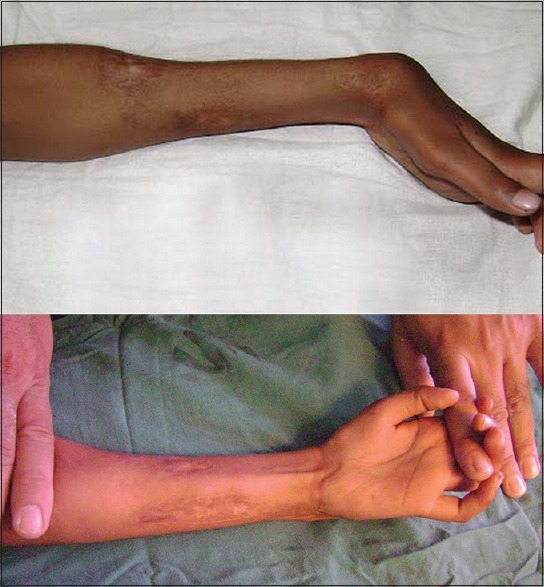
Clinical photograph showing signs of Volkmann's ischemic contracture
For evaluation of compression in median and ulnar nerve, sensory and motor grading was done according to the British Medical Research Council (BMRC)16 grading system preoperatively and postoperatively. The sensory assessment was also done by pinprick (deep and light) and two-point discrimination was looked for in autonomous area of median and ulnar nerve. Motor assessment was done by preparing a muscle chart of hand muscle for both thenar and hypothenar groups.
Operative procedure
Under pneumatic tourniquet with either general anaestheia or regional block, a volar incision originating on the medial aspect of arm 2 cm proximal to the medial epicondyle, extending obliquely across the antecubital fossa to reach the volar aspect of mobile wad, is used. The incision is continued distally in the central part of forearm slightly ulnarly and reaches up to the wrist. At the wrist, the incision should be ulnar to Palmaris longus to avoid injury to palmar cutaneous branch of median nerve. Then, incision crosses the wrist at an angle and reaches up to midpalm for carpal tunnel release. The subcutaneous tissue and deep fascia are incised and muscles are mobilized. Both median and ulnar nerves are isolated along their course and sequentially released at their respective anatomical site of compression, i.e., the median nerve is first identified in the proximal portion of the incision and traced distally to the lacertus fibrosus. It is incised along the course of the nerve. The nerve is then explored to the proximal edge of the pronator teres to ensure that there are no areas of constriction between two heads of the muscle. Muscle is myotomized as needed to ensure decompression, if portion of muscle is fibrotic, the cicatrix is excised. Then, the nerve is traced distally in the deep investing fascia of sublimis muscle which is released and fibrotic part of the muscle is removed and then the nerve is subcutaneously placed. Finally, the carpal tunnel is divided to mobilize the nerve [Figure 3].
Figure 3.

Postoperative photograph showing healing by scar formation
The ulnar nerve is often compressed at the elbow between two heads of flexor carpi ulnaris or proximal to the elbow, where it continues deep to the arcade of Struthers and pierces the intermuscular septum of the arm. Hence, both offending structures in the arm are released if needed and if the nerve appears to be edematous or under tension along its bed in the cubital tunnel, additional procedures like anterior transposition and epicondylectomy are performed. Fibrous cicatrix of muscle or its epimysial edge is myotomized as needed, preventing vincula leashes that contain segmental blood supply to nerve. Finally, Guyon's canal can be opened, if extensive fibrosis is present in forearm and wrist.
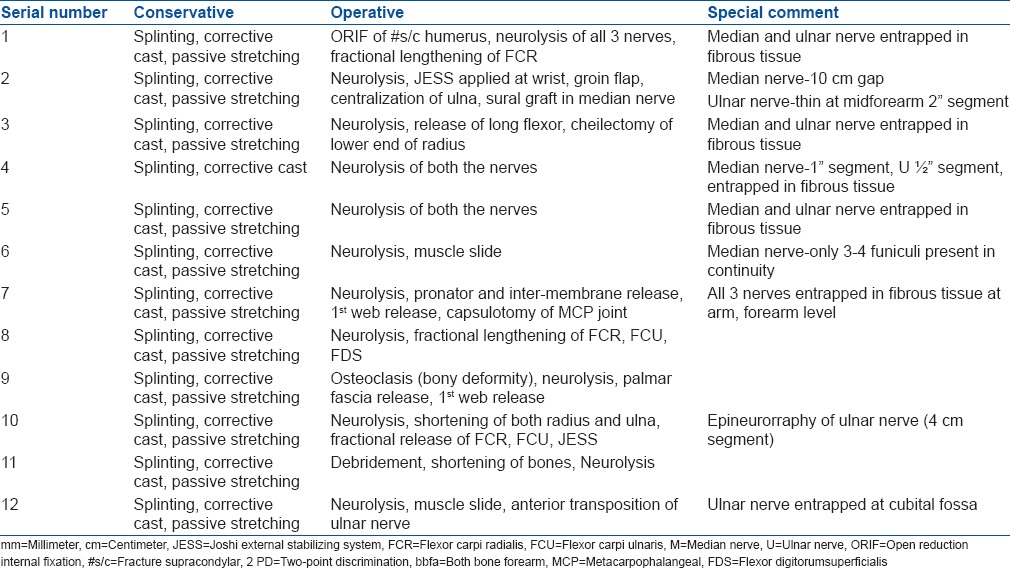
Neurolyis was done in all 12 cases and the nerves found to be entrapped in the fibrous tissue were freed [Figures 4 and 5]. Fractional lengthening of the tendons of flexor compartment was done in three cases palmar fascia release was done in cases with thenaratrophy where decompression at the wrist was necessary. Gradual correction of the skin contracture was brought about by the application of a JESS fixator in two cases [Table 1]. Intraoperatively usage of loop magnification and microscissors for neurolysis aids in achieving good results. The 2 ml syringe needle was used to break adhesions and cicatrix around the nerves.
Figure 4.

Intraoperative photograph showing both ulnar and median nerve
Figure 5.

Neurolysis at 8 months after the onset of deformity showing thinned out nerve
Table 1.
Treatment details
Postoperative period
The wrist is splinted for 3–4 weeks in slight extension to prevent adhesion between nerve and scar. Mobilization was started as soon as patients’ comfort permitted. After 4 weeks, wrist mobilization and progressive strengthening exercises were started [Figure 6].
Figure 6.

Intraoperative photograph showing thinned out, cicatrized nerve along its entire length
RESULTS
There were five moderate and seven severe cases. The average age of patients was 8.3 years. Out of the 12 cases, nine were males and three were females. In 11 cases, right limb which was also the dominant limb was affected. One case included left limb which was nondominant. In our study, the operated cases were divided according to time taken to operate from the onset of VIC. Average followup was 24.3 months (range 15-30 months). Seven cases were operated within 6 months. All seven cases had severe grade of VIC, favorable skin condition, tender nerves throughout the forearm, severe constriction mark at the forearm, and radiological evidence of union of fracture. Other five cases were operated after 6 months. In all these five cases first presentation was after 6 months, skin conditions were not favorable, showing some signs of recovery, fracture was not united or there was presence of a bony deformity. For evaluation, we used the BMRC grading16 system and two-point discrimination, for both motor and sensory recovery, preoperatively and postoperatively [Table 2].
Table 2.
Clinical details of patients
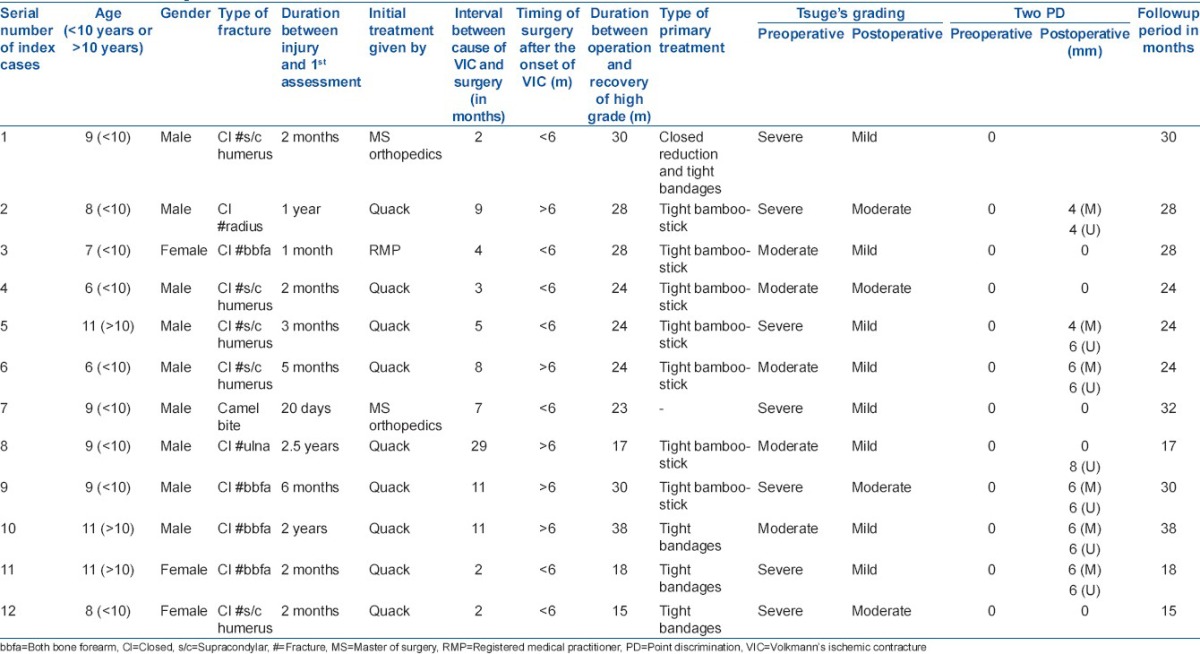
Preoperative and postoperative sensory and motor grades of the seven operated cases within 6 months after onset of VIC are shown in Table 3. Preoperative assessment showed that five cases with median nerve involvement had complete anesthesia (So grade) and four cases with ulnar nerve involvement had complete anesthesia (So grade). All seven cases showed complete motor paralysis (Mo grade) of thenar and hypothenar muscles of the hand. Postneurolysis and adequate followup showed that high grade of sensory recovery (S4, S3+) was seen in two cases of median nerve and four cases of ulnar nerve involvement. High grade of motor recovery (M4) in median nerve was seen in two cases, i.e., the patient was able to use the hand for writing, eating, and perform other activities of daily living (ADL). Similarly, one case with ulnar nerve involvement showed high-grade motor recovery [Figures 7–9].
Table 3.
Motor and sensory grade comparison of seven cases operated within first 6 months of onset of Volkmann's ischemic contracture
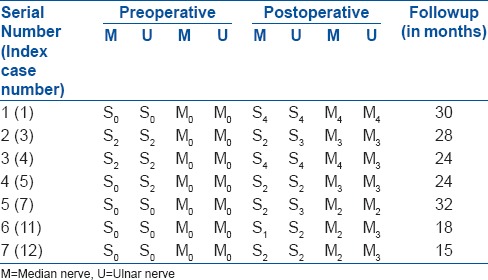
Figure 7.

Clinical photographs showing signs of recovery of both ulnar and median nerve
Figure 9.
Clinical photographs showing functional recovery at 2-year followup
Figure 8.
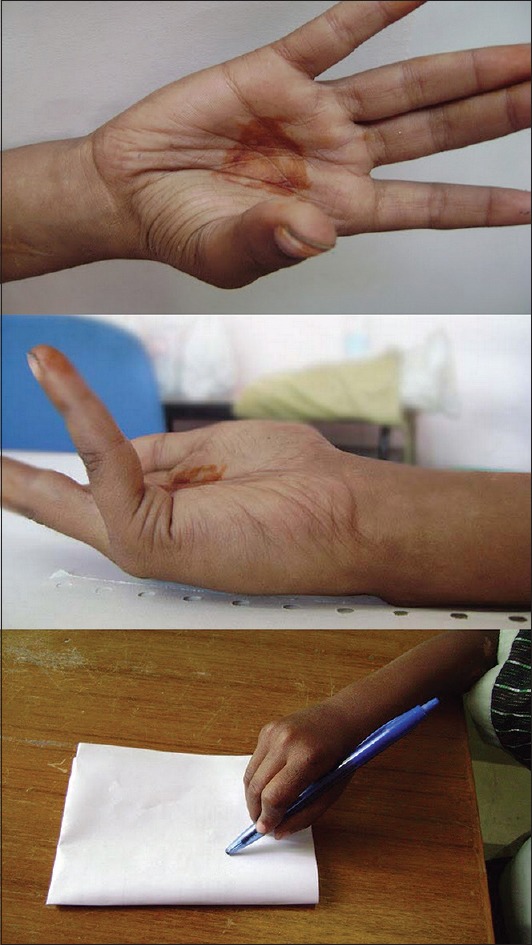
Clinical photographs showing signs of improvement of abductor strength and grip strength
We operated five cases [Table 4] after 1 year either because of late reporting of cases or other problems involved with skeletal management. On their initial evaluation, both median and ulnar showed some sensory (S1 grade) and motor (M3) recovery but they were nonprogressive. After surgical intervention and followup, both median and ulnar nerve showed good sensory (S3+) and motor (M3) recovery except case no eight, where motor recovery was below M0 because intraoperatively there was gap of 10 cm in the median nerve which required sural cable 10 cm grafting. After 2-year followup period, patient shows protective, sensory recovery in median nerve (S3) and motor recovery of M3 grade. A return of protective sensation in the median nerve greatly helps in ADL.
Table 4.
Motor and sensory grade comparison of cases operated 6 months or later after the onset of Volkmann's ischemic contracture
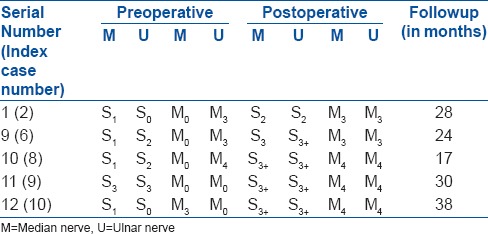
Table 4 shows preoperative and postoperative sensory and motor grades of the five operated cases reporting 6 months after onset of VIC. Preoperative assessment showed that four of five cases with median nerve involvement had low grade anesthesia (S1 grade), and two of five had complete ulnar nerve anesthesia (S0 grade). Four of five cases showed complete (M0 grade) motor paralysis in the median nerve distribution and two of five had complete motor paralysis in ulnar nerve (M0 grade). Postneurolysis and adequate followup showed that high grade of sensory recovery (S3) was seen in four cases of the median nerve and four cases of ulnar nerve involvement. High grade of motor recovery (M4) in median nerve was seen in three cases, i.e. the patient was able to use the hand for writing, eating, and perform other ADL. Similarly, three cases with ulnar nerve involvement showed high-grade motor recovery.
Statistical analysis
It can be noted that significant improvement (P < 0.05) was obtained in motor and sensory grades for both median and ulnar nerves. However, we intended to check whether the timing of the surgery had any implications on the outcome. Data for the two groups was compared using unpaired t-test. Using unpaired t-test, P > 0.05 (two-tailed P = 0.5074) which proved contrary to the clinical assumption [Table 5]. In other words, for motor and sensory components of both the nerves there was no significant difference, whether surgery was done within or after 6 months. This may be due to the small study group.
Table 5.
The statistical analysis and P values of sensory and motor components of median and ulnar nerves
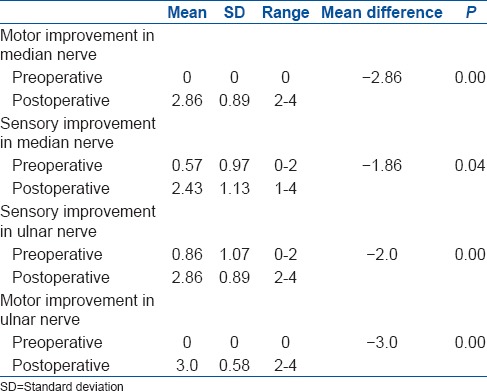
Confidence interval
The mean difference between the two groups is 0.37 with 95’ confidence intervals of 1.58 to 0.83.
Hence, we conclude that neurolysis of the nerves definitely improved the outcome, but the timing of the surgery did not play a role in the outcome.
DISCUSSION
According to the largest Indian series,17 most common cause was fracture of forearm bones followed by fracture of the supracondylar humerus. Similarly, most common cause of VIC in our study was fracture of forearm bones in 6 cases followed by fracture of supracondylar humerus in 5 cases. In 1 case, it was camel bite. In other study by Eichler and Lipscomb,18 supracondylar fracture of humerus was most common cause of VIC.
Our study proposed neurolysis and subcutaneous placement of median and ulnar nerve in cases of VIC. Although it does not have a complete physiological basis, but there is a strong anatomical basis. The study of deep retinacular system in the forearm demonstrates that release of cicatrix compression will result in recovery of sensation, even though motor function is lost.16 The major problem in outlining satisfactory therapy for impending classic contracture in forearm muscle is that the exact pathogenesis of the condition is not clear.
To understand the pathogenesis of the median and ulnar nerve palsy in Volkmann's Syndrome, their anatomic relations to the surrounding structure should be well understood. At the elbow level in upper part of the forearm, the median nerve lies between the two heads of pronator teres and below the lacertus fibrosis. In the forearm, median nerve lies between flexor profundus and flexor sublimis muscle,19,20,21 underneath the investing fascia of sublimis muscle. Careful dissection of the retinacular system of the forearm reveals that the median nerve is in a separate fascial compartment which blends, almost imperceptibly, with the underlying fascia of sublimis muscle. Hence for complete decompression, the entire deep volar retinaculum must be incised. Finally, for mobilization of nerve, carpal tunnel ligament division must be done.
The ulnar nerve is not as clearly incorporated in the deep fascia surrounding the flexor carpi ulnaris such as the median nerve, but the ulnar nerve passes between the two heads of this muscle. Hence, this is the most frequent site of compression. Proximal to the elbow the arcade of Struthers is also a potential site of compression. According to Seddon’s7 “Ellipsoid infarct” concept, involvement of ulnar nerve is less severe than median nerve because of its peripheral location in the forearm.
The effect of double injury on nerve tissue, i.e., local ischemia and compressive cicatrix in the forearm, results in nerves becoming thin cord-like structure (decreased diameter) at different levels and in severe and long standing cases they also showed yellow degeneration. These findings are typically seen in median nerve because of its central location in the forearm while in ulnar nerve these findings are less typical because of its peripheral location. Sometimes, if yellow degeneration is extensive and end-to-end repair is not possible then the secondary reconstruction can be done, i.e., cable grafting (e.g., sural).
In our series, most of the cases took primary treatment in the form of tight bandages with bamboo-stick by bonesetter or tight plaster (one case) leading to acute compartment syndrome.21 Delay in diagnosis and treatment is because of good faith and lack of awareness. This leads to more fibrotic contracture, paralysis, and deformity.22
Tsuge8 believes that “in determining the most opportune time for surgery, there are conflicting situations; i.e., for the muscle, early surgery is not desirable or may even be harmful, whereas for nerve, with the exception of those in which the degree of damage is slight, the more severe the condition, the earlier surgery should be performed.”8 Thus, for mild cases, it is not necessary to rush, whereas in severe cases, fairly early nerve decompression should be carried out.
According to Seddon,10 “Recovery begins at 3rd month and advances then, so one should wait for at least 3 months for spontaneous recovery before embarking other treatment.” Hence, the policy of “Watchful waiting” is not justified when recovery in nerves progresses very slowly or do not progress at all, decompression of nerves should be performed as soon as the condition of the extremity allows for the operation, i.e., between 3 months and 12 months, but not beyond that.
In this study, for Group 1 cases which were operated earlier, propensity of useful sensory recovery (protective sensation above S3 level) was more in ulnar (57.7%) than in median nerve (28.5%) and useful motor recovery (for ADL, above M4 level) in median nerve was (28.5%) more than in ulnar nerve (14.8%). But, Group 2 cases, which were operated late showed similar high grade of sensory (80%) and motor (60%) recovery in both nerves. These results encourage us to believe that exploration for nerve decompression will be beneficial. Statistical results proved that timing of surgery had no implications to the final outcome. This may be due to the small sample size. Assessment of the result of surgery in Volkmann's syndrome is extremely difficult because of various existing variables in spite that the main goal of surgery is to maximize the limb function, to decrease any associated pain, and to restore limb sensibility, if possible.
The study population is too small to be able to provide statistically relevant correlation between surgery and functional outcome. However, our results do indicate some correlation between surgery and final outcome.
Despite the advancement in healthcare, it is not uncommon for a mismanaged forearm or supracondylar fracture to complicate into VIC. We hope our study can serve as a template and can contribute to the decision making in future surgeries for patients with VIC to provide a definitive solution to a long lasting health problem.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hildebrand. German Magazine for Surgery Springerlink. 1890;30:98. [Google Scholar]
- 2.Volkmann R. The ischemic muscular paralyses and contractures. Zentralbl Chir. 1881;8:801–3. [Google Scholar]
- 3.Thomas JJ. III. Nerve involvement in the ischaemic paralysis and contracture of Volkmann. Ann Surg. 1909;49:330–70. doi: 10.1097/00000658-190903000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy JB. myositis. J Med Assoc. 1914;63:1249–55. [Google Scholar]
- 5.Page CM. Operation for the relief of flexion contracture of the forearm. J Bone Joint Surg. 1923;5:233–4. [Google Scholar]
- 6.Jones R. An address on Volkmann's ischaemic contracture, with special reference to treatment. Br Med J. 1928;2:639–42. doi: 10.1136/bmj.2.3536.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seddon HJ. Volkmann's contracture: Treatment by excision of the infarct. J Bone Joint Surg Br. 1956;38-B:152–74. doi: 10.1302/0301-620X.38B1.152. [DOI] [PubMed] [Google Scholar]
- 8.Tsuge K. Treatment of established Volkmann's contracture. J Bone Joint Surg Am. 1975;57:925–9. [PubMed] [Google Scholar]
- 9.McQueen MM, Gaston P, Court-Brown CM. Acute compartment syndrome. Who is at risk? J Bone Joint Surg Br. 2000;82:200–3. [PubMed] [Google Scholar]
- 10.Seddon H. Volkmann's ischaemia. Br Med J. 1964;1:1587–92. doi: 10.1136/bmj.1.5398.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipscomb PR, Burleson RJ. Vascular and neural complications in supracondylar fracture of the humerus in childrens. J Bone Joint Surg. 1995;37-A:487. [PubMed] [Google Scholar]
- 12.Hill RL, Brooks B. Volkmann's ischemic contracture in hemophilia. Ann Surg. 1936;103:444–9. doi: 10.1097/00000658-193603000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanford S. Traumatic ischemia in forearm and leg. Lancet. 1944;1:462. [Google Scholar]
- 14.Parkes A. The treatment of established Volkmann's contracture by tendon transplantation. J Bone Joint Surg Br. 1951;33-B:359–62. doi: 10.1302/0301-620X.33B3.359. [DOI] [PubMed] [Google Scholar]
- 15.Peacock EE, Jr, Madden JW, Trier WC. Transfer of median and ulnar nerves during early treatment of forearm ischemia. Ann Surg. 1969;169:748–56. doi: 10.1097/00000658-196905000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolffe SW, Hotchkiss RN, Pederson WC. In: BMRC grading system. Operative Hand Surgery. 2nd ed. Green DP, editor. New York: Churchill Livingstone; 1988. [Google Scholar]
- 17.Sundararaj GD, Mani K. Pattern of contracture and recovery following ischaemia of the upper limb. J Hand Surg Br. 1985;10:155–61. doi: 10.1016/0266-7681(85)90005-1. [DOI] [PubMed] [Google Scholar]
- 18.Eichler GR, Lipscomb PR. The changing treatment of Volkmann's ischemic contractures from 1955 to 1965 at the Mayo Clinic. Clin Orthop Relat Res. 1967;50:215–23. [PubMed] [Google Scholar]
- 19.Anson BJ, Maddock WC. Callander's Surgical Anatomy. 4th ed. Philadelphia: W.B Saunders Co; 1958. p. 867. [Google Scholar]
- 20.Romanes GA. Cunningham's Textbook of Anatomy. 10th ed. New York: Oxford University Press; 1964. p. 72. [Google Scholar]
- 21.Anson BJ. Morri's Human Anatomy. 12th ed. New York: McGraw-Hill; 1966. p. 7. [Google Scholar]
- 22.Ultee J, Hovius SE. Functional results after treatment of Volkmann's ischemic contracture: A long term followup study. Clin Orthop Relat Res. 2005;431:42–9. doi: 10.1097/01.blo.0000154476.00181.3b. [DOI] [PubMed] [Google Scholar]


