Abstract
A 57 year healthy farmer with congenital nail pterygium presented with a verrucous growth on nail bed since 8 months. He was not diabetic and HIV rapid card test negative. Our clinical diagnosis was chromoblastomycosis but culture showed growth of curvularia species on two occasions and histopathology showed hyphal and yeast forms of the pigmented fungus. After excision biopsy patient was started on oral itraconazole. This case is reported due to rarity of verrucous cutaneous lesions caused by curvularia in immunocompetent individuals.
Keywords: Congenital nail pterygium, Curvularia, itraconazole, verrucous nail bed growth
Introduction
What was known?
Curvularia species are dematiaceous fungi known to cause nondermatophytic onychomycosis, phaeohyphomycosis, and disseminated infections in immunocompromised patients. Diagnosed by culture and microscopy in repeated sessions. Treatment response is poor to fluconazole and responds well to oral itraconazole.
Curvularia species are ubiquitous fungus among soil and vegetation. They belong to class-eumycetes, family-Pleosporacea. They spread via airborne spores and are a common cause of disease in plants.[1] Curvularia can be microscopically distinguished from other dematiaceous fungi due to the presence of curved conidia.[1] The first reported human case was in 1959 as a corneal infection.[1] Of approximately 40 recognized species, the most common causing human infection is Curvularia lunata.[2]
Curvularia cause nondermatophytic onychomycosis, phaeohyphomycosis, mycetoma, and infection of wounds, sinuses, and eyes. Rarely it can cause central nervous system infections, postsurgical endocarditis, dialysis-related peritonitis, and atypical skin lesions.[3] Here we report a case of an unusual cutaneous lesion caused by Curvularia in a patient with congenital nail pterygium.
Case Report
A 67-year-old male farmer presented with an asymptomatic warty lesion on right thumb over nail bed of 8 months duration. History of pterygium nails since childhood with a family history of similar nail change in father, paternal uncle, and son. No history of diabetes or any other systemic illness.
Physical examination revealed pterygium of all nails except little fingers. There was a brownish verrucous plaque of size 2 cm × 2 cm on nailbed of right thumb [Figure 1].
Figure 1.

Verrucous lesion on nail bed, congenital nail pterygium
The differential diagnosis considered was chromoblastomycosis, verruca vulgaris, tuberculosis verrucosa cutis, and verrucous carcinoma.
Scraping for sclerotic body and Mantoux test were negative. Other routine investigations were noncontributory. HIV screening test was negative.
Excision biopsy was done and sent for histopathology, fungal and acid-fast bacilli culture.
Histopathology revealed hyperkeratosis, parakeratosis, papillomatosis. Yeast and hyphal forms of fungus seen in stratum corneum, which were pigmented on special stains Gomori Methamine silver and Masson Fontana [Figure 2]. No koilocytes were seen and the dermis was normal.
Figure 2.
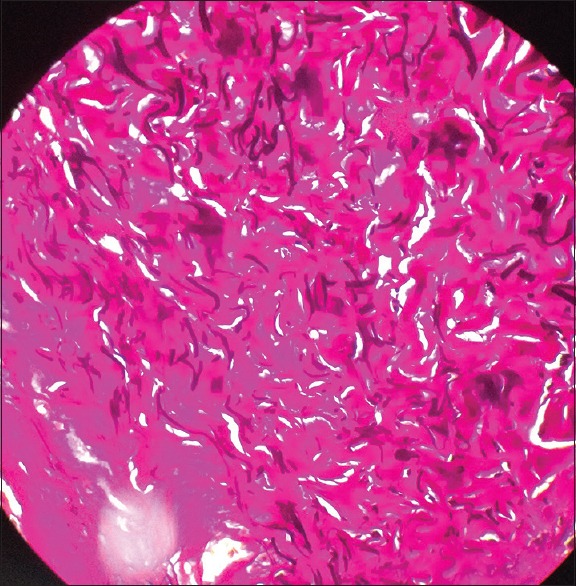
Gomori Methamine silver stain shows brownish spores
Fungal culture in Sabouraud Dextrose agar at 25°C and 37°C showed wooly, blackish colonies at 1-week incubation [Figure 3], and on microscopy dematiaceous fungi with pigmented septate hyphae with conidiophores arising terminally and laterally seen. The brownish conidia were broadly ellipsoidal, smooth-walled and had four septate in most parts [Figure 4]. Fungal culture done with two specimens revealed same growth. The sub-terminal cells of the conidia were curved, larger, and darker which was diagnostic of Curvularia species.
Figure 3.
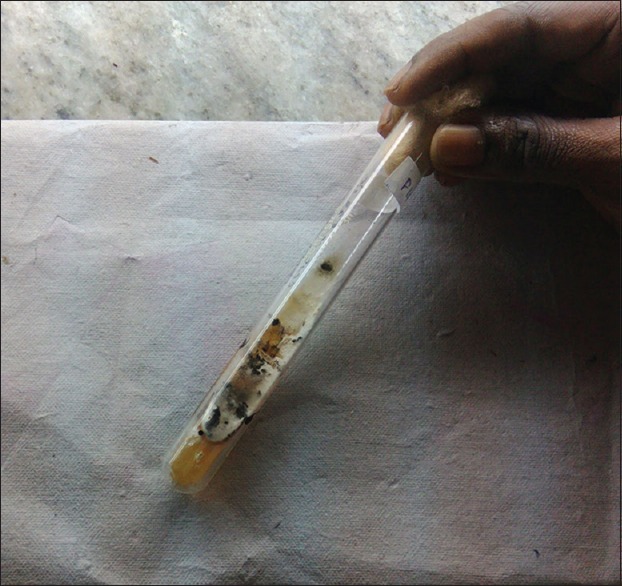
Fungal culture in Sabouraud Dextrose agar shows wooly blackish growth
Figure 4.
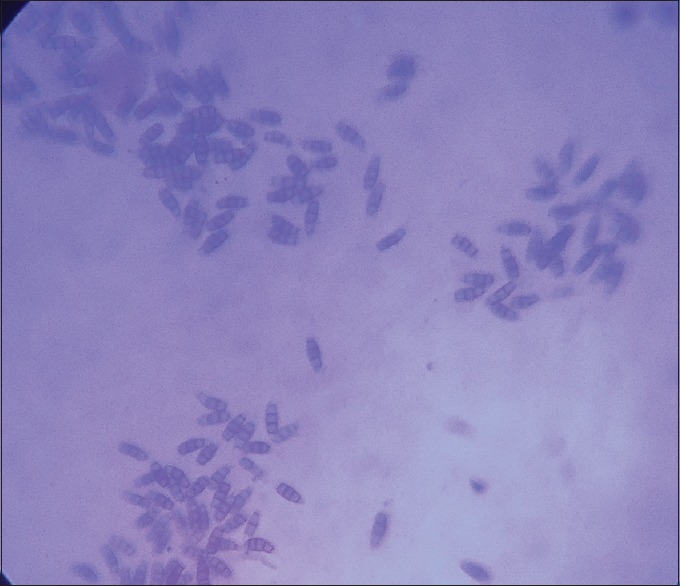
Microscopy shows brownish septate hyphae
Hence, the final diagnosis was verrucous onychomycosis caused by Curvularia.
Patient was started on tab itraconazole 200 mg twice daily after excision biopsy to prevent recurrence.
Discussion
More than 100 species and 60 genera of dematiaceous fungi have been discovered to cause human disease.[1,2] Dematiaceous fungi are deeply pigmented due to melanin within their hyphae and conidia. These melanin also contribute to their pathogenicity.[4]
Curvularia has relatively low virulence, with disease manifestations and severity depending primarily on host factors.[5] Species which cause human infections are C. lunata, Curvularia pallescens, and Curvularia geniculata. The modes of transmission are inhalation and inoculation. It presents as secondary invader following corneal perforation or surgery, in patients with peritoneal and venous catheters and in intravenous (IV) drug abusers. Excluding ocular cases, few Curvularia infections are reported in the literature. Of the reported cases, presentations and treatments vary from case to case.
Cutaneous infections show a predilection for the extremities as in our patient, often following traumatic inoculation. Curvularia species can cause nondermatophytic onychomycosis. However, verrucous onychomycosis is rare. Safdar reported a case of verrucous onychomycosis due to Curvularia in a lymphoma patient on chemotherapy.[6] Dematiaceous fungi produce blackish colored nail lesions clinically, but in our patient the lesion was lightly pigmented.
Other reported skin infections in immunocompromised individuals were an erythematous ecchymotic plaque on forearm,[7] and secondary infection of posttraumatic ulcers with fatal systemic dissemination.[8] In immunocompetent individuals, mycetoma like lesions are reported.[9]
Diagnostic tests to confirm infection include gram and/or Calcofluor-White stains for hyphal elements, Gomori Methenamine silver stain for fungal biomass, Fontana-Masson silver stain for melanin, and panfungal polymerase chain reaction assay[10] for rapid diagnosis.
Curvularia species mature rapidly on semisynthetic media at an optimal temperature of 28.5°C, taking approximately 2 days on blood and chocolate agar and 4 days on Sabouraud agar or brain-heart infusion agar. It forms wooly blackish growth at reverse bottom as in our case. Repeated cultures at least twice should give consistent results for diagnosis.
Microscopic examination of growth shows both hyaline and pigmented septate hyphae in which conidiophores arose terminally or laterally. The brownish conidia are broadly ellipsoidal or clavate, smooth-walled and for the most part contain 4 septa. The conidia are variable in size (21.0–31.0 to 8.5–12.0 μm) and are produced in sympodial order to leave dark brown scars on conidiophores. The sub-terminal cells of the conidia are curved, larger, and darker. Our patient's fungal culture also showed typical features. Two cultures should show the consistent result for a definite diagnosis.
Current options for the treatment of dematiaceous fungi infections include azoles (e.g., voriconazole, itraconazole), amphotericin B, terbinafine, and echinocandins. Of these agents, voriconazole and itraconazole have had the highest consistent in vitro success, with a minimum inhibitory concentration of 0.125 g/mL or less. Dosing can range from 200 to 600 mg daily. Fluconazole was found to have negligible anti-dematiaceous fungi activity. If dissemination is suspected, prompt hospitalization and initiation of IV itraconazole and/or amphotericin B is recommended.
Surgical excision is another option, especially if a drug trial alone does not yield resolution or if there is any sign of local recurrence. Meticulous follow-up is necessary due to the possibility for recurrence and dissemination, especially in immunocompromised.
Our patient is on oral itraconazole and he is under follow-up for last 3 months, no recurrence occurred till now. This case is reported because of rarity of verrucous lesions caused by Curvularia.
What is new?
Curvularia species causing verrucous onychomycosis is rare. Usually, it causes blackish pigmented lesion, but here it was lightly pigmented. Patient had an excellent response to oral itraconazole.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Wilhelmus KR, Jones DB. Curvularia keratitis. Trans Am Ophthalmol Soc. 2001;99:111–30. [PMC free article] [PubMed] [Google Scholar]
- 2.Fan YM, Huang WM, Li SF, Wu GF, Li W, Chen RY. Cutaneous phaeohyphomycosis of foot caused by Curvularia clavata. Mycoses. 2009;52:544–6. doi: 10.1111/j.1439-0507.2008.01646.x. [DOI] [PubMed] [Google Scholar]
- 3.Revankar SG. Phaeohyphomycosis. Infect Dis Clin North Am. 2006;20:609–20. doi: 10.1016/j.idc.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Bonduel M, Santos P, Turienzo CF, Chantada G, Paganini H. Atypical skin lesions caused by Curvularia sp. and Pseudallescheria boydii in two patients after allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001;27:1311–3. doi: 10.1038/sj.bmt.1703072. [DOI] [PubMed] [Google Scholar]
- 5.Silveira F, Nucci M. Emergence of black moulds in fungal disease: Epidemiology and therapy. Curr Opin Infect Dis. 2001;14:679–84. doi: 10.1097/00001432-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Safdar A. Curvularia – Favorable response to oral itraconazole therapy in two patients with locally invasive phaeohyphomycosis. Clin Microbiol Infect. 2003;9:1219–23. doi: 10.1111/j.1469-0691.2003.00791.x. [DOI] [PubMed] [Google Scholar]
- 7.Moody MN, Tschen J, Mesko M. Cutaneous Curvularia infection of the forearm. Cutis. 2012;89:65–8. [PubMed] [Google Scholar]
- 8.Tessari G, Forni A, Ferretto R, Solbiati M, Faggian G, Mazzucco A, et al. Lethal systemic dissemination from a cutaneous infection due to Curvularia lunata in a heart transplant recipient. J Eur Acad Dermatol Venereol. 2003;17:440–2. doi: 10.1046/j.1468-3083.2003.00674.x. [DOI] [PubMed] [Google Scholar]
- 9.Hiromoto A, Nagano T, Nishigori C. Cutaneous infection caused by Curvularia species in an immunocompetent patient. Br J Dermatol. 2008;158:1374–5. doi: 10.1111/j.1365-2133.2008.08528.x. [DOI] [PubMed] [Google Scholar]
- 10.Alex D, Li D, Calderone R, Peters SM. Identification of Curvularia lunata by polymerase chain reaction in a case of fungal endophthalmitis. Med Mycol Case Rep. 2013;2:137–40. doi: 10.1016/j.mmcr.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


