Abstract
Objective
A stated goal of the preparticipation physical evaluation (PPE) is to reduce musculoskeletal injury, yet the musculoskeletal portion of the PPE is reportedly of questionable use in assessing lower extremity injury risk in high school-aged athletes. The objectives of this study are: (1) identify clinical assessment tools demonstrated to effectively determine lower extremity injury risk in a prospective setting, and (2) critically assess the methodological quality of prospective lower extremity risk assessment studies that use these tools.
Data Sources
A systematic search was performed in PubMed, CINAHL, UptoDate, Google Scholar, Cochrane Reviews, and SportDiscus. Inclusion criteria were prospective injury risk assessment studies involving athletes primarily ages 13 to 19 that used screening methods that did not require highly specialized equipment. Methodological quality was evaluated with a modified physiotherapy evidence database (PEDro) scale.
Main Results
Nine studies were included. The mean modified PEDro score was 6.0/10 (SD, 1.5). Multidirectional balance (odds ratio [OR], 3.0; CI, 1.5–6.1; P < 0.05) and physical maturation status (P < 0.05) were predictive of overall injury risk, knee hyperextension was predictive of anterior cruciate ligament injury (OR, 5.0; CI, 1.2–18.4; P < 0.05), hip external: internal rotator strength ratio of patellofemoral pain syndrome (P = 0.02), and foot posture index of ankle sprain (r = −0.339, P = 0.008).
Conclusions
Minimal prospective evidence supports or refutes the use of the functional musculoskeletal exam portion of the current PPE to assess lower extremity injury risk in high school athletes. Limited evidence does support inclusion of multidirectional balance assessment and physical maturation status in a musculoskeletal exam as both are generalizable risk factors for lower extremity injury.
Keywords: preparticipation exam, lower extremity injury, high school sports, injury risk assessment
INTRODUCTION
In 1976, the American Medical Association’s Committee on Medical Aspects of Sports recognized the importance of the preparticipation physical evaluation (PPE) and recommended completion of a PPE before athletic participation.1 PPE screening requirements for high school student athletes in the U.S. are typically determined by state legislation, state athletic associations, or individual school districts.2 The National Federation of State High School Associations considers the PPE a prerequisite to athletics participation, yet its implementation at the secondary school level varies from every year to every 3 years with a majority (36) states requiring a yearly examination.2 Although the PPE was initially intended to fulfill school-based legal and medical requirements, the primary goal of the current examination is to maximize safe participation in physical activities by adolescents. One of the stated goals according to the PPE fourth edition as it applies to the musculoskeletal exam is to predict individuals at risk for musculoskeletal injury during sports participation,2 which is a major source of injuries overall in adolescent population.3–6 Traditionally, the musculoskeletal examination portion of the PPE has been a 2-minute orthopedic screen focused on general range of motion, strength, and joint laxity.7,8 The current PPE exam has minimal evidence to support or refute its capabilities as an effective predictor of future injuries and offers little direction in the prevention of future musculoskeletal injuries.8,9 Research is needed to clearly identify useful screening tests for use in the PPE.
A standard PPE (fourth edition 2010)2 protocol has been recommended by a joint effort of 6 medical associations to be conducted for all youth, regardless of whether individuals are playing sports. With as many as 7,795,658 U.S. adolescents having reportedly participated in sanctioned high school athletics during the 2013 to 2014 school year,10 duplicate athlete participation most likely lowers this value, recommendations for yearly PPE by qualified members of the medical community create imposing demands on health care practitioners to create time-efficient methods for assessing injury and illness risk. To effectively conduct personalized PPEs, it is recommended that physicians evaluate individuals in a private clinical one-on-one setting,2,7 yet this is oftentimes not feasible because of the large number of individuals, and mass screenings are commonly conducted for time efficiency and cost-effectiveness. A primary challenge for these types of large-scale screening PPEs is the lack of objective quantifiable information that can be collected in a short period that provides predictive capabilities for identifying individuals at greater risk for musculoskeletal injury.
The purposes of this study are: (1) to identify clinical assessment tools demonstrated to effectively determine risk for acute and chronic lower extremity injuries in a prospective setting, and (2) to critically assess the methodological quality of prospective lower extremity risk assessment studies that use these tools. We hypothesize that there is no prospective evidence to support routine use of the musculoskeletal (MSK) exam portion of the current PPE and that alternative assessment tools exist that can effectively identify individuals at increased risk for lower extremity injuries. This work addresses a gap in knowledge concerning the efficacy of preparticipation evaluations for the prediction of musculoskeletal injury risk in high school-aged athletics participants as a critical first step for musculoskeletal injury prediction in this age group.
METHODS
Initial Search and Screening
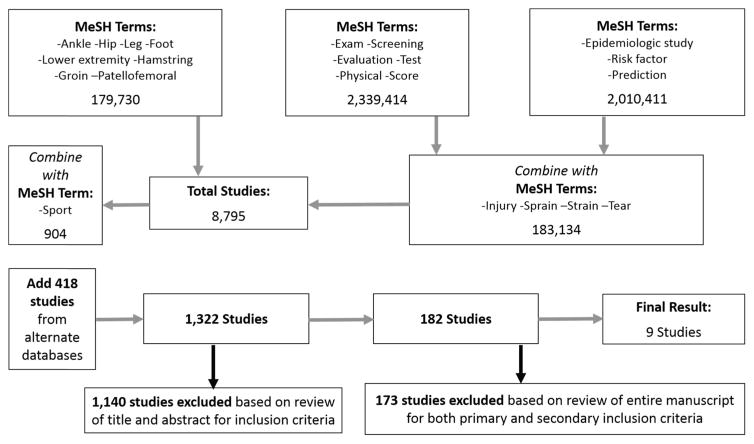
We have adhered to the guidelines outlined in the PRISMA statement for standardized reporting of systematic reviews in the preparation of this article.11 We initially performed a search of the PubMed database (1975 to November 21, 2014) using the MeSH advanced search tool (Figure). A search that included at least 1 term related to injury (eg, sprain, injury, strain, or tear) and either a term related to evaluation (eg, test, physical, exam, screening, etc.) or disease surveillance (eg, risk factor, prediction, or epidemiologic study) resulted in 183 134 hits; this was further narrowed by requiring an additional MeSH term for anatomic site (eg, ankle, hip, leg, foot, etc.) to 8795 hits, which was then narrowed further to 904 studies by inclusion of the MeSH term “sport.” Systematic searches were also performed in CINAHL, UptoDate, Google Scholar, Cochrane Reviews, and SportDiscus and relevant studies previously known by the authors were collected, resulting in 418 additional studies to complete our initial study list for a total of 1322 studies. The titles and abstracts of these 1322 studies were reviewed for our primary inclusion criteria (Table 1); 637 studies from this initial list that were identified as duplicates, review articles, commentary/editorials, or pertaining to an unrelated subject, and an additional 503 studies were excluded that clearly did not meet one or more primary inclusion criteria, resulting in a list of 182 remaining studies. The entire articles of the remaining 182 studies were reviewed for both primary and secondary inclusion criteria (Table 1). For studies in which the secondary criteria were in question, one of the senior authors (JAO) made the final decision for inclusion in the review. Each author made recommendations for studies to include in the systematic review based on the practicality of the clinical screening test and the relevance of the injury risk factor to sports commonly practiced by American high school athletes. A consensus was made from these individual recommendations resulting in the final identification of 9 studies for inclusion in the systematic review (Table 2).
FIGURE.
Initial PubMed MeSH search and subsequent screening process.
TABLE 1.
Study Inclusion Criteria
| Inclusion | Exclusion |
|---|---|
| Primary criteria | |
| Studies investigating lower extremity injury prediction or risk factors | Studies not reporting original research including review articles, expert opinion, or current concepts articles |
| Study population consists primarily of physically active individuals (athletes or military) of any level of experience (eg, recreational, college, professional, etc.) | Posters or abstracts at annual meetings or masters theses without subsequent peer-reviewed publication of a article |
| At least one of the injury risk factors being studied is a physical exam test | Studies investigating risk factors identifiable only by imaging or laboratory testing |
| Study is peer-reviewed | Animal studies |
| Study reports original data | Studies investigating osteoarthritis |
| Level 1–4 evidence according to CEBM criteria | Studies investigating risk factors based on patient history alone (eg, patient demographics, activity level, participating sport, or injury history) |
| Study is reported in English | |
| Secondary criteria | |
| Study population consists primarily of adolescent to young-adult (ages 13–19 yrs) athletes | Length of physical exam test exceeding 15 minutes for single-patient exam format or 1 h for multistation format |
| Clinical screening test be performed in a single-patient exam format or a multistation format | Studies drawing conclusions regarding injury risk or injury prediction based on historical data |
| Prospective study design | |
TABLE 2.
Nine Studies Identified for Inclusion in Systematic Review
| Author | Purpose | Methodology and Participants | Measures | Injury Incidence and Prevalence | Identified Risk Factors | PEDro Score | Limitations | Strengths |
|---|---|---|---|---|---|---|---|---|
| Bennett et al12 | Evaluate foot type as predictor of medial tibial stress syndrome | High school runners, single season n = 125 | Navicular drop, gastroc length, rearfoot angle, tibiofibular varum | 15/125 runners (12% total; 2/57 or 4% men, 13/68 or 19%) or women had MTSS symptoms. Incidence not reported. | Sex and navicular drop associated with MTSS (r2 = 0.18 navicular drop; r2 = 0.24 sex, P < 0.05). OR not reported | 5 | Assessment of MTSS did not explicitly rule out stress fracture with bone scan/radiograph, navicular drop was measured postinjury | Easily obtainable measure, highly specific clinical definition of MTSS |
| Cain et al13 | Evaluate foot pronation/supination as risk factor for foot/ankle overuse injury | High school-aged male indoor soccer players, single season n = 76 | Foot Posture Index, coach-rated ability | 32% of players sustained at least 1 ankle/foot injury during the season. Incidence not reported | Supination and under pronation (FPI score less than 2) associated with foot/ankle overuse injury (sensitivity 89% specificity 50%) | 8 | Male participants only, foot posture index scoring system requiring significant training of novice evaluators (two 2-h sessions) | Playing h factored into analysis, injury defined by self-report of pain resulting in missed h |
| Finnoff et al14 | Evaluate hip strength as a risk factor PFPS in high school runners | High school runners, age 14–18 yrs, single season (n = 98) | Weight, leg lengths, isometric hip strength (external rotation, internal rotation, abduction, adduction, flexion, extension) | 5/98 subjects experiences PFPS symptoms. 2/53 or 3.7% men, 3/44 or 6.8% women. Incidence not reported | Lower hip ER:IR strength ratio increased risk of PFPS (P = 0.08); higher ER:IR ratio was protective (OR < 0.01; CI < 0.01–0.44; P = −0.02). Higher abd strength (OR, 5.4; CI, 1.5–29.5; P < 0.01) and abd: add ratio (OR, 14.14; CI, 0.90–220; P = 0.05) increased risk | 5 | Low recruitment rates, reenrollment of 4/98 subjects across multiple seasons, unable to report reliability data for strength testing | Easily testable in clinic setting, also reported effect of agonist-antagonist strength imbalance in addition to individual muscle groups |
| McHugh et al16 | Evaluate balance and hip strength as predictors of ankle injury | High school-aged male and female football, basketball, gymnastics, and American football players, 2 seasons, (n = 169) | Hip flexion, abduction, adduction, strength through hand-held dynamometer, single-limb balance on tilt board, body mass index, ligamentous laxity | 27 lateral ankle sprains recorded. Incidence 1.47/1000 exposures. Prevalence of injured athletes not reported | Higher body mass index in male athletes and history of previous ankle strain were significant predictors of injury; balance and strength were not (P > 0.05) | 8 | Injury prevalence not reported in detail. Nonstandard report of incidence. Did not discriminate between game or practice time | Large sample size, 2-yr follow-up, men and women included in model, previous injury included in model, power analysis conducted, training h considered in model |
| Myer et al17 | Evaluate joint laxity as ACL injury risk factor in female athletes | Female high school-aged soccer and basketball players, 4 seasons, (n = 95 nested case–control from total n = 1558) | Generalized joint laxity tests, AP tibiofemoral translation (CompuKT knee arthrometer) in bilateral knees | 19/1558 subjects sustained ACL tears (1.2%). Incidence not reported | Side to side differences in knee laxity associated with increased ACL injury risk (OR, 4.0 per 1.3 mm difference; CI, 1.7–9.7). Positive knee hyperextension increased injury risk (OR, 5.0; CI, 1.2–18.4) | 8 | Model restricted to ACL injury only, requires specialized equipment, training h not included in model | Nested case–control design with internally validated prediction model, large sample size, broad population of interest |
| Plisky et al18 | Evaluate balance as a risk factor for lower extremity injury in basketball players | Male and female high school basketball players, single season (n = 235) | SEBT | 54/235 (23%) of athletes sustain a LE injury. Incidence not reported | R/L reach distance disparity >4 cm increased injury risk OR, 2.7; CI, 1.4–5.3 all, 3.0 (1.1–7.7 men). Normalized composite reach distance less than 94% increased LE injury risk (OR, 3.0; CI, 1.5–6.1 all; OR, 6.5; CI, 2.4–17.5 women) | 7 | 19% dropout rate, multiple trials required for accurate SEBT assessment, training h not included in model | Previous injury accounted for in model, large sample size, men and women |
| Turbeville et al19 | Evaluate risk factors for injury in high school American football players | High school-aged male American football players (13–19 yrs), 2 seasons (n = 717) | Report of preseason conditioning, body mass index, grip strength, playing experience | 132 injuries reported among 100/717 (13.9%) players over 2 seasons. 62% were LE injuries; 38% were UE injuries. Incidence not reported | Physical characteristic were not associated with injury risk. Players with previous injuries or more playing experience (OR, 1.34) at increased LE injury risk | 6 | Study-designed for overall injury risk, injury rates underreported relative to historical data, individual training h not included in model | Easily obtainable measures, data applicable to specific positions played, preseason conditioning and use of special equipment (eg, brace) recorded |
| Wang et al20 | Evaluate ankle injury risk factors in high school basketball players | High school male and female basketball players, single season, (n = 42) | Isokinetic ankle strength (Cybex 6000, Biodex dynamometer), ankle ROM, ankle endurance, postural sway (forceplate) | 18/42 (43%) players sustained ankle injuries; incidence not reported | Postural sway was only variable associated with injury (OR, 1.2; CI, 1.09–1.36; P < 0.01) | 6 | 25% dropout rate, specialized equipment required, small sample size | Training h included in model, strict inclusion criteria with control for shoe type, bracing, training surface |
Quality Assessment
The study authors created a modification of the Physiotherapy Evidence Database (PEDro) scale,21,22 a quality assessment tool based on the Delphi list of criteria for quality assessment of randomized clinical trials for conducting systematic reviews (Table 3).23 Original items 2 and 3 pertained to subject allocation, which is not relevant to studies of prospective injury risk factors. Our modified item 2 pertained to prospective collection of all baseline study data, and our modified item 3 pertained to performing a power analysis to ensure an adequate sample size, which is inconsistently reported in sports medicine studies. The language of original item 4 was changed to modified item 5 to reflect an expected difference in some baseline factors in injured versus noninjured study participants. Original items 5 and 6 were combined into modified item 6, as blinding of athletic trainers, athletes, and coaches would be necessary to prevent intentional modification of a perceived injury risk factor (eg, coaches encouraging athletes with low flexibility scores to stretch more often in an effort to reduce injury risk). Finally, original item 9 pertained to correct allocation to treatment or control groups, which was not relevant to prospective injury risk studies; our modified item 9 pertained to accounting for exposure time in matches or practice sessions, thereby allowing for report of injury risk per unit time in addition to absolute risk.
TABLE 3.
Original and Modified PEDro Scales
| Assessment | Revised Category | Original Category |
|---|---|---|
| External validity/applicability | 1. Eligibility criteria were specified | 1. Eligibility criteria were specified |
| Internal validity | 2. All measures were obtained before sports season onset (prospective design) | 2. Subjects were randomly allocated to groups |
| 3. A power analysis was performed to determine sample size | 3. Allocation was concealed | |
| 4. Reliability data was available for all applicable measures | 4. The groups were similar at baseline regarding the most important prognostic indicators | |
| 5. Other than the measures of interest, the groups were similar at baseline regarding the most important prognostic indicators | 5. There was blinding of all subjects | |
| 6. There was blinding of athletes, trainers, and sports coaches to baseline measures of interest | 6. There was blinding of all therapists who administered the therapy | |
| 7. There was blinding of all assessors of injury to baseline measures of interest | 7. There was blinding of all assessors who measured at least 1 key outcome | |
| 8. Measures of at least 1 key outcome were obtained from more than 85% of the subjects initially recruited | 8. Measures of at least 1 key outcome were obtained from more than 85% of the subjects initially allocated to groups | |
| 9. Before injury, both groups had nonsignificant differences in sport exposure (both practice time and match time), or this was corrected for in the statistical analysis if found to be unequal | 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated | |
| Interpretability | 10. The results of between-group statistical comparisons are reported for at least 1 key outcome | 10. The results of between-group statistical comparisons are reported for at least 1 key outcome |
| 11. The study provides both point measures and measures of variability for at least 1 key outcome | 11. The study provides both point measures and measures of variability for at least 1 key outcome | |
| Scoring | Assign 1 point for each item in criteria 2–11 that is met. The first criterion is not included in the total All points are summed to yield a total score of up to 10 points |
|
Reliability of Modified PEDro Scale
The final list of 9 studies was circulated among the study authors for blinded quality assessment. Specifically, each blinded reviewer (JRB and AMWC) independently evaluated the 9 studies with the modified PEDro scale and submitted scoring data directly to a designated unblinded study author (JAO). The blinded authors were instructed not to discuss the studies or their scoring results until all blinded reviewers had submitted scores. After the blinded review, the 2 senior authors (TMB and JAO) performed an unblinded review of the 9 studies. Specifically, each discrepantly scored item among the blinded reviewers was reviewed and the unblinded authors assigned a final “gold standard” score after critically appraising the body of the study article. The blinded scores were non-normally distributed (P = 0.003 Shapiro–Wilk W), and we therefore used nonparametric reliability tests. Inter-rater reliability of individual blinded reviewers was calculated as Spearman rho, and inter-rater reliability of individual items among blinded reviewers was assessed with Fleiss kappa.
Data Collection and Reporting
The primary purpose, length of time, sample size, age and sex of participants, level of competition, and included sports were reported for all included studies (Table 2). Because the purpose of this review is to assess risk factors for lower extremity injury that are identifiable by examination, we have limited our report of study measures and results to risk factors identifiable in a clinical examination setting with limited equipment (Table 2). Measures of estimated effect size and variability were reported as available. We did not perform any secondary statistical tests on the reported data, and the heterogeneity of reporting methods and experimental design among the included studies was such that we could not perform a meta-analysis or similar method of pooled data analysis. Finally, we documented additional specific strengths and weaknesses of the individual studies that were not directly assessed by the modified PEDro scale but are of potential relevance to interpreting the study findings.
RESULTS
Study Characteristics
After our screening process was completed, 9 prospective cohort studies including high school age athletes were identified (Table 2). One study was specific to soccer players,13 3 studies were specific to track and field or running,12,14,15 2 were specific to basketball,18,20 1 was specific to American football,19 and 2 included multiple sports.16,17 Three were limited to male athletes,13,15,19 1 was limited to female athletes,17 and 5 included both sexes. Sample size ranged from 4220 to 155817 athletes, and athletes were followed 2 to 4 sports seasons in 4 studies15–17,19 and a single season for the remaining 5 studies.12–14,18,20 The overall injury prevalence in the reported studies ranged from 1.2% for anterior cruciate ligament (ACL) tears among female high school athletes17 to 43% for ankle injuries among soccer players.20 The most common definition of injury included missed practice or game time (6 of 9 studies).13,15,16,18–20 Injury severity was reported based on time lost in 2 studies15,20 and by a clinical scoring system in 1 study.16 Five studies required clinical evaluation by an athletic trainer, physical therapist, or physician,12,14–16,20 1 study allowed injury report by the coach or athletic trainer,18 and 1 study required diagnostic imaging or arthroscopic visualization.17
Methodological Quality and Modified PEDro Score Reliability
The mean modified PEDro score for the included studies was 6.0 ± 1.5 (Table 3) for the gold standard review, which was not significantly different from the distribution of unblinded scores (median, 8; interquartile range, 6–8; P = 0.95 Wilcoxon rank sum). None of the studies fulfilled all criteria in the modified PEDro scale (modified PEDro score of 10). However, 2 of 9 studies attained a high score of 8 of 10,17,18 and 2 of 9 studies attained a low score of 4 of 10.12,20 Of the individual factors on the modified PEDro scale, item 3 had the lowest percentage of studies that met the specified criteria (1/9 or 11%),16 which was use of a power analysis to determine appropriate sample size. There was moderate correlation among blinded reviewers for both the total study score (Spearman rho = 0.63) and item-specific responses (Fleiss kappa = 0.46).
Identified Clinical Exam Injury Risk Factors
No prospective studies that met our inclusion criteria were identified that included evaluation of all or part of the functional examination recommended in the PPE fourth ed. (the duck walk or single-leg hop).2 Our review identified several clinical examination modalities that have at least preliminary evidence to suggest efficacy in stratifying future lower extremity injury risk. Identified risk factors fell into 7 basic categories: balance,18,20 anatomy,12,13 strength,14 physical maturation status,15 weight,16 and ligamentous laxity.17 Modalities such as the Star Excursion Balance Test (SEBT) and assessment of physical maturation are broadly associated with increased injury risk,15,18 whereas most assessments included in this review are specific to individual injuries.12–20 Our assessments of these risk factors are as follows:
Physical Maturation Status
Delayed physical maturation status is associated with increased acute lower extremity injury in school-aged athletes.24–26 Only 1 study examined the relationship between physical maturation status and overuse lower extremity injury but found that boys under the age of 14 were more likely to get injured.25 This study evaluated physical maturation by comparing participants’ skeletal maturity assessed through radiographs with their chronological ages.25 An early maturer was defined as an individual with a skeletal age 1 year above their chronological age and a late maturer was defined as an individual with a skeletal age 1 year below their chronological age.25 However, determination of maturation status by comparing skeletal maturity and chronological age is problematic for general screening because of the required radiographs. Fourchet et al15 presents an interesting association between age of peak height velocity and overall injury risk in a study population that includes track and field athletes that participate in a variety of events. Age of peak height velocity as a surrogate measure of maturation status can be calculated based on serial height measurements and has the potential for incorporation into a clinical injury risk assessment. One requirement for this type of assessment is either continual yearly access to the same primary care provider or an electronic medical record system that is accessible to allow parents and children to track and maintain their yearly physical maturation information.
Balance
Based on our review, poor balance seems to be a likely risk factor for ankle sprain in high school-aged athletes in sports with a high incidence of ankle injuries, as 2 included studies had positive findings18,20 and 1 had negative findings.16 However, the methodology of each balance testing procedure varied significantly, and differences in study populations limit direct comparison of test results. McHugh et al16 examined frontal plane excursion (uniplanar balance) on a tilt board as measure of percent time out of balance, Wang et al20 used degree of postural sway (multidirectional balance) on a force plate, and Plisky et al18 used a clinical exam (SEBT) of reach distance in multiple planes before losing balance (multidirectional balance). The SEBT relies on minimal equipment and seems to be conducive to a clinical setting. Although Plisky et al reported increased overall lower extremity (LE) injury risk based on SEBT results, injury data regarding anatomic distribution (knee vs ankle vs hip) was not reported and limited the specificity of his results.
Anatomic Factors
Four studies in this review examined anatomic injury risk factors, particularly leg length asymmetry and foot morphology. Leg length asymmetry is proposed to result in asymmetrical gait and postural changes with compensatory imbalances in muscle strength and flexibility,30,31 with some promise as a predictive tool for stress fractures in select populations such as track and field athletes.32 Limb length discrepancy is measured most accurately with radiographic methods,30 which may be inappropriate for general screening in a pediatric population. Finnoff et al14 reported negative findings regarding length discrepancy as a risk factor for patellofemoral pain syndrome (PFPS); however, this measure has not been previously associated with PFPS and seemed to be a secondary aspect of their overall study design. Both excessive foot pronation and supination have also been proposed to increase lower extremity injury risk33–35; correspondingly, a pronatory foot type as measured through navicular drop was associated with increased risk of medial tibial stress syndrome (MTSS) by Bennet et al12 and Cain et al13 reported that supination as measured by the Foot Posture Index was associated with ankle overuse injury. However, the small sample size, single sport design, narrow injury definition, and varied methods of determining foot type in these studies again limit the applicability of this screening modality to a general athletic population.
Strength
Based on our review, maximum isometric strength was not a risk factor for injury but strength ratios between agonistic and antagonistic muscle groups were predictive of injury. Specifically, Wang et al and McHugh et al found no association between ankle injury and leg strength.16,20 In a more generalized model, Turbeville et al19 used hand grip strength as a surrogate measure of overall strength and also found no association with injury of any type among football players. However, when examining strength imbalance, Finnoff et al14 noted a protective effect from a low external rotation (ER): internal rotation (IR) hip strength ratio and an increased risk of PFPS at higher ratios in runners. The narrow scope of this study, both in athlete population and injury of interest, limits the applicability of their findings, and future research of strength imbalance as an injury assessment tool in a multisports setting with a broader definition of injury may be warranted.
Ligamentous Laxity
Myer et al17 was the only study to assess joint laxity in our review, which is a known risk factor for ACL injury.36,37 The authors conclude that screening of ligamentous laxity may effectively identify high school female athletes at increased risk of ACL injury who participate in soccer and basketball.17
DISCUSSION
Injury risk assessment in high school athletes has been a long-standing goal of sports medicine practitioners. One of the challenges of developing an assessment tool to determine relative injury risk is the large range of activities performed by athletes even within a given sport and the wide variation in physical maturity within this age group. Accordingly, multiple assessment strategies have been proposed with varying degrees of specificity to a given population, yielding equally varied results. After extensive review of the literature, we found no evidence to support or refute use of the PPE fourth ed. format for prospective musculoskeletal injury risk assessment in high school-aged athletes. There seems to be a moderate level of evidence supporting several physical examination findings, including ligamentous laxity,17 strength imbalance,14 excessive foot pronation or supination,12,13 physical maturation status,15 and multidirectional balance18,20 in high school-aged athletes as risk factors for future injury, although their utility is often limited to a narrow spectrum of sports or to prediction of specific injuries.
One of the stated goals of the PPE is to identify those at risk for injury. Although self-report of previous injuries38 or the presence of persistent functional deficits28,29,39 are risk factors for future injury, the results of this review demonstrate that there is no objective evidence that the recommended components of the MSK examination portion of the PPE provide relevant prospective risk assessment data in high school-aged athletes. In addition to the general MSK examination, a functional assessment of 2 movements, the duck walk and single-leg hop, is recommended.2 Based on our systematic search of the literature, there are no reported prospective injury risk assessment studies in high school-aged athletes that include evaluation of these movements. However, evidence-based assessments were identified that could replace these qualitative assessments in a clinical setting. In particular, both the SEBT and age of peak height velocity as a measure of physical maturation status are both easily reproducible and associated with overall lower extremity injury risk.15,18 These types of assessments can easily be performed in a primary care provider’s standard office setting and requires minimal training for reliable data collection. One limitation is nonstandard reporting of data (no odds ratio or correlation coefficients reported) and an overly broad definition of injury severely limits the interpretability of peak height velocity for lower extremity injury risk assessment. Future studies that clearly report relative risk and injury data are needed to determine the reliability of age of peak height velocity as an injury risk factor. However, this information does highlight the use of serial type measurements and the importance of primary care provider yearly access to help make better informed decisions using longitudinal tracking on an individual basis. Future studies are indicated to develop a more comprehensive evidence-based examination, but it is clear that sufficient evidence exists to at least moderately improve on the currently recommended assessment process.
Quantitative analysis of knee hyperextension as a surrogate for joint laxity may provide some insight into lower extremity injury risk (ie, ACL injury), which can be readily accomplished in a clinical examination setting, it is likely inappropriate for general screening because of the low overall incidence of ACL injury, but it may be more appropriate as a future component of the PPE for female athletes in high ACL injury risk sports (eg, soccer and basketball). Sport specific PPE testing may not be time efficient, but discussions between primary care providers and their patients will help them discern which specialized tests may be warranted based on an individual’s values and physical activity goals. One generalized risk assessment tool that has had promising results in 2 recent prospective studies of collegiate and professional level athletes is the Functional Movement Screen (FMS).40,41 This screening tool was developed under the premise that functional testing of movements that simultaneously integrate aspects of neuromuscular coordination, balance, strength, and flexibility can effectively determine injury risk because of the likely multifactorial etiology of acute sports injuries.27,42–45 The FMS requires qualitative evaluation of the controlled execution of several movements of varying complexity (deep squat, shoulder mobility, hurdle step, lunge, straight leg raise, push-up, and rotary stability).44,46 With high inter-rater reliability (0.7–0.9)47,48 and minimal equipment needed to perform this screening tool, additional study of the FMS as a generalized lower extremity risk assessment tool in high school athletes is merited.
In an effort to facilitate improved design of future sports injury risk assessment studies and evaluation of methodological quality of previous injury risk studies, the authors have presented our initial experiences with the modified PEDro scale. Our results indicate that this scale provides a reasonable general assessment of study quality. However, it is not meant to substitute well-defined inclusion criteria for a systematic review. Several components of prospective study design were emphasized in our modified scale that are inconsistently present in this field of research, namely participant blinding, sample size estimation, and report of sports exposure hours. We believe that the importance of blinding study participants from the results of risk assessment tools is under-appreciated. Athletes, coaches, and clinicians alike are motivated to keep participants healthy, and blinding is necessary to minimize the likelihood of active attempts to modify the perceived risk factor (even if it is a spurious assumption) in an attempt to prevent injury. In addition, sports exposure is an essential component of injury risk, and it has been well-established that playing time during sporting events confers a higher risk of injury than training hours.49–53 Even if an injury risk assessment study had adequate sample size, it would be underpowered if the enrolled athletes did not have sufficient sports exposure to sustain the anticipated number of injuries.
Limitations of this review are related to the heterogeneity of the selected studies in addition to assumptions of overall study quality made by our modified PEDro score. Our modified scale and the original PEDro are designed to determine the quality of the study design as it is reported in the article, which does not take into account possible discordance in study report and actual study design.22 In addition, because our review centers on risk assessment in a relatively broad athlete population, the studies that met our inclusion criteria had respectively varied study populations, precluding direct comparison between risk assessment tools. The lack of clarity between risk factors for acute and chronic injuries created an additional limitation.
It is possible that some risk factors are different for acute and chronic injuries and because the research reviewed did not consistently distinguish between acute and chronic injuries the results of this review would not clearly identify risk factors that may be indicative of certain types of injury. Finally, because most of sport injury risk assessment studies that met our criteria focused on a given sport or a specific injury, there is a paucity of studies that broadly evaluate a given risk assessment tool for general screening in a setting such as the sports preparticipation evaluation (PPE). There were several common methodological limitations in the identified studies that undoubtedly introduced a bias toward negative findings. There was typically a lack of reported power analyses to determine adequate sample size, despite an abundance of epidemiologic reports from which to draw incidence and prevalence data for acute high school sports injuries when estimating sample size for study design.3–5,54–69 Only one of the studies in this review had a reported method of sample size estimation,16 and athlete exposure hours was only reported in 2/9 studies.15,17 Additionally, injuries were reported in a nonstandard manner ranging from self-report of symptoms to missed practice time to diagnosis by a sports medicine provider. Therefore, to improve efforts at identifying reliable sports injury risk assessment tools, it is imperative that future risk assessment studies demonstrate adequate sample size, report injury risk in a standard manner, record sport exposure time, and use a reliable working injury definition.
In conclusion, no prospective studies were identified in this review that support or refute use of the functional MK examination portion of the currently recommended sports preparticipation evaluation to assess injury risk in high school-aged athletes. There is some prospective evidence to support generalized use of the SEBT and assessment of physical maturation status by age of peak height velocity to prospectively determine lower extremity injury risk. Several injury-specific risk assessment tools, such as the FMS, hip muscle strength ratios, foot pronation measurements, ankle dorsiflexion range of motion, and dynamic functional hop tests may yield improved benefit for prospectively evaluating lower extremity injury risk for high school athletes entering specific sports or positions of increased lower extremity risk exposure.
Footnotes
The authors report no conflicts of interest.
References
- 1.AMA. Medical Evaluation of the Athlete: A Guide. Chicago, IL: American Medical Association; 1976. [Google Scholar]
- 2.Bernhardt DT, Roberts WO, editors. PPE Preparticipation Physical Evaluation. 4. Elk Grove Village, IL: American Academy of Family Physicians, American Academy of Pediatrics, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sport Medicine; 2010. [Google Scholar]
- 3.Rechel JA, Collins CL, Comstock RD. Epidemiology of injuries requiring surgery among high school athletes in the United States, 2005 to 2010. J Trauma. 2011;71:982–989. doi: 10.1097/TA.0b013e318230e716. [DOI] [PubMed] [Google Scholar]
- 4.Swenson DM, Yard EE, Fields SK, et al. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009;37:1586–1593. doi: 10.1177/0363546509332500. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez WG, Yard EE, Comstock RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14:641–645. doi: 10.1197/j.aem.2007.03.1354. [DOI] [PubMed] [Google Scholar]
- 6.Scheidt PC, Harel Y, Trumble AC, et al. The epidemiology of nonfatal injuries among US children and youth. Am J Public Health. 1995;85:932–938. doi: 10.2105/ajph.85.7.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garrick JG. Preparticipation orthopedic screening evaluation. Clin J Sport Med. 2004;14:123–126. doi: 10.1097/00042752-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Gomez JE, Landry GL, Bernhardt DT. Critical evaluation of the 2-minute orthopedic screening examination. Am J Dis Child. 1993;147:1109–1113. doi: 10.1001/archpedi.1993.02160340095022. [DOI] [PubMed] [Google Scholar]
- 9.Best TM. The preparticipation evaluation: an opportunity for change and consensus. Clin J Sport Med. 2004;14:107–108. doi: 10.1097/00042752-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 10.National Federation of State High School Associations. 2013–2014 High School Athletics Participation Survey. Indianapolis, IN: 2015. [Google Scholar]
- 11.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Bennett JE, Reinking MF, Pluemer B, et al. Factors contributing to the development of medial tibial stress syndrome in high school runners. J Orthop Sports Phys Ther. 2001;31:504–510. doi: 10.2519/jospt.2001.31.9.504. [DOI] [PubMed] [Google Scholar]
- 13.Cain L, Nicholson L, Adams R, et al. Foot morphology and foot/ankle injury in indoor football. J Sci Med Sport. 2007;10:311–319. doi: 10.1016/j.jsams.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Finnoff JT, Hall MM, Kyle K, et al. Hip strength and knee pain in high school runners: a prospective study. PM R. 2011;3:792–801. doi: 10.1016/j.pmrj.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Fourchet F, Horobeanu C, Loepelt H, et al. Foot, ankle, and lower leg injuries in young male track and field athletes. Int J Athl Ther Train. 2010;16:19–23. [Google Scholar]
- 16.McHugh MP, Tyler TF, Tetro DT, et al. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34:464–470. doi: 10.1177/0363546505280427. [DOI] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Paterno MV, et al. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med. 2008;36:1073–1080. doi: 10.1177/0363546507313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plisky PJ, Rauh MJ, Kaminski TW, et al. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911–919. doi: 10.2519/jospt.2006.2244. [DOI] [PubMed] [Google Scholar]
- 19.Turbeville SD, Cowan LD, Owen WL, et al. Risk factors for injury in high school football players. Am J Sports Med. 2003;31:974–980. doi: 10.1177/03635465030310063801. [DOI] [PubMed] [Google Scholar]
- 20.Wang HK, Chen CH, Shiang TY, et al. Risk-factor analysis of high school basketball player ankle injuries: a prospective controlled cohort study evaluating postural sway, ankle strength, and flexibility. Arch Phys Med Rehabil. 2006;87:821–825. doi: 10.1016/j.apmr.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 21.Blobaum P. Physiotherapy evidence database (PEDro) J Med Libr Assoc. 2006;94:477. [Google Scholar]
- 22.Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 23.Verhagen AP, de Vet HCW, de Bie RA, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51:1235–1241. doi: 10.1016/s0895-4356(98)00131-0. [DOI] [PubMed] [Google Scholar]
- 24.Backous DD, Friedl KE, Smith NJ, et al. Soccer injuries and their relation to physical maturity. Am J Dis Child. 1988;142:839–848. doi: 10.1001/archpedi.1988.02150080045019. [DOI] [PubMed] [Google Scholar]
- 25.Johnson A, Doherty PJ, Freemont A. Investigation of growth, development, and factors associated with injury in elite schoolboy footballers: prospective study. BMJ. 2009;338:b490. doi: 10.1136/bmj.b490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Le Gall F, Carling C, Reilly T. Biological maturity and injury in elite youth football. Scand J Med Sci Sports. 2007;17:564–572. doi: 10.1111/j.1600-0838.2006.00594.x. [DOI] [PubMed] [Google Scholar]
- 27.Baumhauer JF, Alosa DM, Renstrom AF, et al. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 28.McGuine TA, Greene JJ, Best T, et al. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- 30.McCaw ST, Bates BT. Biomechanical implications of mild leg length inequality. Br J Sports Med. 1991;25:10–13. doi: 10.1136/bjsm.25.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neely FG. Biomechanical risk factors for exercise-related lower limb injuries. Sports Med. 1998;26:395–413. doi: 10.2165/00007256-199826060-00003. [DOI] [PubMed] [Google Scholar]
- 32.Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24:810–818. doi: 10.1177/036354659602400617. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman KR, Brodine SK, Shaffer RA, et al. The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999;27:585–593. doi: 10.1177/03635465990270050701. [DOI] [PubMed] [Google Scholar]
- 34.Murphy DF, Connolly DAJ, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37:13–29. doi: 10.1136/bjsm.37.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Razeghi M, Batt ME. Foot type classification: a critical review of current methods. Gait Posture. 2002;15:282–291. doi: 10.1016/s0966-6362(01)00151-5. [DOI] [PubMed] [Google Scholar]
- 36.Ramesh R, Von Arx O, Azzopardi T, et al. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87:800–803. doi: 10.1302/0301-620X.87B6.15833. [DOI] [PubMed] [Google Scholar]
- 37.Uhorchak JM, Scoville CR, Williams GN, et al. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 38.Steffen K, Myklebust G, Andersen TE, et al. Self-reported injury history and lower limb function as risk factors for injuries in female youth soccer. Am J Sports Med. 2008;36:700–708. doi: 10.1177/0363546507311598. [DOI] [PubMed] [Google Scholar]
- 39.Croisier JL, Ganteaume S, Binet J, et al. Strength imbalances and prevention of hamstring injury in professional soccer players. Am J Sports Med. 2008;36:1469–1475. doi: 10.1177/0363546508316764. [DOI] [PubMed] [Google Scholar]
- 40.Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther. 2007;2:147–158. [PMC free article] [PubMed] [Google Scholar]
- 41.Chorba RS, Chorba DJ, Bouillon LE, et al. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5:47–54. [PMC free article] [PubMed] [Google Scholar]
- 42.Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39:324–329. doi: 10.1136/bjsm.2005.018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meeuwisse WH. Assessing causation in sport injury: a multifactorial model. Clin J Sport Med. 1994;4:166. [Google Scholar]
- 44.Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function-part 1. N Am J Sports Phys Ther. 2006;1:62–72. [PMC free article] [PubMed] [Google Scholar]
- 45.Meeuwisse WH, Tyreman H, Hagel B, et al. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17:215–219. doi: 10.1097/JSM.0b013e3180592a48. [DOI] [PubMed] [Google Scholar]
- 46.Foran B. High-Performance Sports Conditioning. Champaign, IL: Human Kinetics Publishers; 2001. [Google Scholar]
- 47.Gribble P, Brigle J, Pietrosimone B, et al. Intrarater reliability of the functional movement screen. J Strength Cond Res. 2013;27:978–981. doi: 10.1519/JSC.0b013e31825c32a8. [DOI] [PubMed] [Google Scholar]
- 48.Teyhen DS, Shaffer SW, Lorenson CL, et al. Functional movement screen: a reliability study. J Orthop Sports Phys Ther. 2012;42:530–540. doi: 10.2519/jospt.2012.3838. [DOI] [PubMed] [Google Scholar]
- 49.Brito J, Malina RM, Seabra A, et al. Injuries in portuguese youth soccer players during training and match play. J Athl Train. 2012;47:191–197. doi: 10.4085/1062-6050-47.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ekstrand J, Gillquist J, Moller M, et al. Incidence of soccer injuries and their relation to training and team success. Am J Sports Med. 1983;11:63–67. doi: 10.1177/036354658301100203. [DOI] [PubMed] [Google Scholar]
- 51.Gabbett TJ. Incidence of injury in semi-professional rugby league players. Br J Sports Med. 2003;37:36–44. doi: 10.1136/bjsm.37.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hagglund M, Walden M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40:767–772. doi: 10.1136/bjsm.2006.026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peterson L, Junge A, Chomiak J, et al. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28:S51–S57. doi: 10.1177/28.suppl_5.s-51. [DOI] [PubMed] [Google Scholar]
- 54.Borowski LA, Yard EE, Fields SK, et al. The epidemiology of US high school basketball injuries, 2005–2007. Am J Sports Med. 2008;36:2328–2335. doi: 10.1177/0363546508322893. [DOI] [PubMed] [Google Scholar]
- 55.Collins CL, Comstock RD. Epidemiological features of high school baseball injuries in the United States, 2005–2007. Pediatrics. 2008;121:1181–1187. doi: 10.1542/peds.2007-2572. [DOI] [PubMed] [Google Scholar]
- 56.Comstock RD. Epidemiology of knee injuries in adolescents: a review. Clin J Sport Med. 2009;19:153–154. doi: 10.1097/01.jsm.0000347358.48692.8c. [DOI] [PubMed] [Google Scholar]
- 57.Cuff S, Loud K, O’Riordan MA. Overuse injuries in high school athletes. Clin Pediatr. 2010;49:731–736. doi: 10.1177/0009922810363154. [DOI] [PubMed] [Google Scholar]
- 58.Gaunt T, Maffulli N. Soothing suffering swimmers: a systematic review of the epidemiology, diagnosis, treatment and rehabilitation of musculoskeletal injuries in competitive swimmers. Br Med Bull. 2012;103:45–88. doi: 10.1093/bmb/ldr039. [DOI] [PubMed] [Google Scholar]
- 59.Kerr ZY, Collins CL, Fields SK, et al. Epidemiology of player–player contact injuries among US high school athletes, 2005–2009. Clin Pediatr. 2011;50:594–603. doi: 10.1177/0009922810390513. [DOI] [PubMed] [Google Scholar]
- 60.Kerr ZY, Collins CL, Pommering TL, et al. Dislocation/separation injuries among US high school athletes in 9 selected sports: 2005–2009. Clin J Sport Med. 2011;21:101–108. doi: 10.1097/JSM.0b013e31820bd1b6. [DOI] [PubMed] [Google Scholar]
- 61.Krajnik S, Fogarty KJ, Yard EE, et al. Shoulder injuries in US high school baseball and softball athletes, 2005–2008. Pediatrics. 2010;125:497–501. doi: 10.1542/peds.2009-0961. [DOI] [PubMed] [Google Scholar]
- 62.Leininger RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35:288–293. doi: 10.1177/0363546506294060. [DOI] [PubMed] [Google Scholar]
- 63.Marar M, McIlvain NM, Fields SK, et al. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40:747–755. doi: 10.1177/0363546511435626. [DOI] [PubMed] [Google Scholar]
- 64.Nation AD, Nelson NG, Yard EE, et al. Football-related injuries among 6- to 17-year-olds treated in US emergency departments, 1990–2007. Clin Pediatr. 2011;50:200–207. doi: 10.1177/0009922810388511. [DOI] [PubMed] [Google Scholar]
- 65.Nelson AJ, Collins CL, Yard EE, et al. Ankle injuries among United States high school sports athletes, 2005–2006. J Athl Train. 2007;42:381–387. [PMC free article] [PubMed] [Google Scholar]
- 66.Swenson DM, Collins CL, Best TM, et al. Epidemiology of knee injuries among US high school athletes, 2005/06–2010/11. Med Sci Sports Exerc. 2013;45:462–469. doi: 10.1249/MSS.0b013e318277acca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Swenson DM, Yard EE, Collins CL, et al. Epidemiology of US high school sports-related fractures, 2005–2009. Clin J Sport Med. 2010;20:293–299. doi: 10.1097/JSM.0b013e3181e8fae8. [DOI] [PubMed] [Google Scholar]
- 68.Yard E, Comstock D. Injury patterns by body mass index in US high school athletes. J Phys Act Health. 2011;8:182–191. doi: 10.1123/jpah.8.2.182. [DOI] [PubMed] [Google Scholar]
- 69.Yard EE, Schroeder MJ, Fields SK, et al. The epidemiology of United States high school soccer injuries, 2005–2007. Am J Sports Med. 2008;36:1930–1937. doi: 10.1177/0363546508318047. [DOI] [PubMed] [Google Scholar]