Abstract
Although interstitial lung disease accounts for the majority of deaths of patients with systemic sclerosis, treatment options for this manifestation of the disease are limited. Few high-quality, randomized, controlled trials exist for systemic sclerosis–related interstitial lung disease, and historically, studies have favored the use of cyclophosphamide. However, the benefit of cyclophosphamide for this disease is tempered by its complex adverse event profile. More recent studies have demonstrated the effectiveness of mycophenolate for systemic sclerosis–related interstitial lung disease, including Scleroderma Lung Study II. This review highlights the findings of this study, which was the first randomized controlled trial to compare cyclophosphamide with mycophenolate for the treatment of systemic sclerosis–related interstitial lung disease. The results reported in this trial suggest that there is no difference in treatment efficacy between mycophenolate and cyclophosphamide; however, mycophenolate appears to be safer and more tolerable than cyclophosphamide. In light of the ongoing advances in our understanding of the pathogenic mechanisms underlying interstitial lung disease in systemic sclerosis, this review also summarizes novel treatment approaches, presenting clinical and preclinical evidence for rituximab, tocilizumab, pirfenidone, and nintedanib, as well as hematopoietic stem cell transplantation and lung transplantation. This review further explores how reaching a consensus on appropriate study end points, as well as trial enrichment criteria, is central to improving our ability to judiciously evaluate the safety and efficacy of emerging experimental therapies for systemic sclerosis–related interstitial lung disease.
Keywords: scleroderma, pulmonary fibrosis, therapeutics
Systemic sclerosis (SSc) has the highest cause-specific mortality of all of the connective tissue diseases (1). Although SSc often affects multiple organ systems, pulmonary involvement, and in particular interstitial lung disease (ILD), is the leading cause of death (2). ILD is present on high-resolution computed tomography (HRCT) in 55% of patients with SSc on initial evaluation (3), but the prevalence is higher (96%) among patients with abnormal pulmonary function test (PFT) results (4). The most common form of ILD appreciated in SSc is nonspecific interstitial pneumonitis (NSIP); however, other histopathological manifestations exist, including usual interstitial pneumonitis, organizing pneumonia, and diffuse alveolar damage (5).
Despite the substantial disease burden associated with SSc-ILD, there are currently no U.S. Food and Drug Administration (FDA)–approved medications for treating this condition. The present review describes an evidence-based treatment approach for managing SSc-ILD. This review also describes novel treatment strategies and opportunities for further research in treating this important clinical dimension of SSc.
Clinical Presentation
The most common initial symptoms of SSc-ILD are fatigue, exertional dyspnea, and dry cough, although early SSc-ILD is often asymptomatic. On physical examination, bibasilar fine inspiratory crackles may be appreciated by auscultation. Specific laboratory findings can support a diagnosis of SSc-ILD. For example, the presence of anti–topoisomerase I antibody is associated with an increased risk of SSc-ILD (sensitivity, 45%; specificity, 81%) (6), whereas anti-centromere antibodies rarely exist in patients with SSc-ILD (7). Demographic risk factors for SSc-ILD include African-American race (8). In addition, male sex is associated with greater severity of SSc-ILD (9). To affirm the diagnosis of SSc-ILD, several diagnostic studies may be employed, generally in combination.
Pulmonary Function Testing
In SSc-ILD, pulmonary function tests (PFTs) generally show a restrictive ventilatory defect with a decreased FVC and/or TLC with a relatively preserved FEV1 and a normal or increased FEV1/FVC ratio. In addition, the single-breath diffusing capacity of the lung for carbon monoxide (DlCO) is generally decreased, variably out of proportion or in proportion to the reduction in the alveolar volume (Va) with a decreased or normal DlCO/Va ratio. Notably, patients with early SSc-ILD may have normal PFT findings or an isolated reduction in DlCO. Moreover, multiple factors may affect PFT findings, including pulmonary vascular disease (in which typically the DlCO is substantially reduced in relation to both the Va and the FVC), an extrapulmonary restrictive disorder (e.g., respiratory muscle weakness due to an inflammatory myositis), as well as smoking-related emphysema, thereby limiting the interpretation of this testing modality (10).
High-Resolution Computed Tomographic Chest Imaging
Ground-glass attenuation and fine reticulation, characteristic of NSIP, are the most frequently observed features on high-resolution computed tomographic (HRCT) chest imaging (11), although coarse reticulations with architectural distortion are often present as well, consistent with a fibrotic form of NSIP (NSIPF). HRCT imaging is both sensitive and specific for SSc-ILD and is particularly helpful in discriminating between alternative causes of dyspnea and PFT abnormalities in the patients with SSc (10).
Bronchoalveolar Lavage
Although bronchoalveolar lavage (BAL) is sometimes performed to exclude infection during initial investigational efforts, this procedure is seldom performed routinely to diagnose SSc-ILD. Historically, some authorities theorized that BAL may detect early, subclinical SSc-ILD; however, studies have demonstrated that BAL provides limited prognostic information regarding disease progression (12) and treatment response (13).
Lung Biopsy
Like BAL, lung biopsy is not routinely employed to diagnose SSc-ILD. However, biopsy may be indicated in atypical presentations of SSc-ILD or when signs of granulomatous disease, malignancy, or infection are present.
Natural History and Predictors of Disease Progression
Early observational cohort studies of patients with SSc illuminated important features of SSc-ILD disease progression. One large study of 890 patients with SSc found that SSc-ILD progressed more rapidly in the first 4 years of systemic disease (8), indicating that lung injury and fibrosis are early complications. Another study, by Steen and Medsger (14), demonstrated that among patients who ever reached an FVC of less than 55% predicted, the majority (62%) did so within the first 5 years after the onset of the first SSc-related symptom. These studies suggest that patients with evidence of restrictive lung disease (by PFTs or HRCT) within 4–5 years of systemic disease onset are more likely to exhibit progressive fibrotic lung disease.
In addition to the timing of ILD detection, numerous studies have revealed clinical and biological factors that predict disease progression in SSc-ILD as demonstrated in Table 1 (8, 15–28). Identifying those patients with the highest risk of developing severe SSc-ILD is central to understanding which patients may derive the greatest benefit from SSc-ILD–targeted therapies. Conversely, in patients with intrinsically stable SSc-ILD, the introduction of SSc-ILD–targeted therapy may pose more risk than benefit.
Table 1.
Clinical and biological factors associated with progression of systemic sclerosis–associated interstitial lung disease
| Factor | Study Type (n) |
|---|---|
| Low baseline FVC | |
| Morgan et al., 2003 (15) | Single-center, prospective cohort (561) |
| Plastiras et al., 2006 (16) | Single-center, retrospective cohort (78) |
| Nihtyanova et al., 2014 (17) | Single-center, prospective cohort (398) |
| Steen et al., 1994 (8) | Single-center, retrospective cohort (890) |
| Low baseline DlCO | |
| Morgan et al., 2003 (15) | Single-center, prospective cohort (561) |
| Nihtyanova et al., 2014 (17) | Single-center, prospective cohort (398) |
| Extent of ILD on HRCT | |
| Goh et al., 2008 (18) | Single-center, prospective cohort (330) |
| Moore et al., 2013 (19) | Multicenter, retrospective cohort (172) |
| Khanna et al., 2011 (20) | Multicenter, randomized controlled trial (placebo group, 79) |
| Anti-topoisomerase I antibodies | |
| Assassi et al., 2010 (21) | Single-center, prospective cohort (125) |
| Nihtyanova et al., 2014 (17) | Single-center, prospective cohort (398) |
| Diffuse cutaneous sclerosis | |
| Nihtyanova et al., 2014 (17) | Single-center, prospective cohort (398) |
| IL-6 | |
| De Lauretis et al., 2013 (22) | Single-center, exploratory (74) and test cohorts (212) |
| C-reactive protein (CRP) | |
| Liu et al., 2013 (23) | Single-center, prospective cohort (266) |
| Monocyte chemoattractant protein-1 (MCP-1) | |
| Wu et al., 2013 (24) | Single-center, prospective cohort (266) |
| CC chemokine ligand 18 (CCL18) | |
| Tiev et al., 2011 (25) | Single-center, prospective cohort (83) |
| Schupp et al., 2014 (26) | Single-center, prospective cohort (96) |
| CXCL4 | |
| van Bon et al., 2014 (27) | Single-center prospective cohort (79) |
| Krebs von den Lungen-6 (KL-6) | |
| Yanaba et al., 2004 (28) | Single-center, retrospective cohort (42) |
| Surfactant protein D (SP-D) | |
| Yanaba et al., 2004 (28) | Single-center, retrospective cohort (42) |
Definition of abbreviations: DlCO = diffusing capacity of the lung for carbon monoxide; HRCT = high-resolution computed tomography; ILD = interstitial lung disease.
When to Introduce SSc-ILD–Targeted Therapy
Although no consensus- or evidence-based guidelines exist to instruct clinicians on the appropriate timing of the introduction of SSc-ILD–targeted therapy, most SSc experts draw on their clinical experience and consider the aforementioned risk factors for SSc-ILD progression (i.e., greater extent of ILD at baseline, the presence of anti–topoisomerase I antibodies) to formulate their decision to initiate therapy. At our own institution, we weigh not only the risk factors present for SSc-ILD progression, but also the disease duration, when deciding whether to initiate therapy. For instance, patients who present with early SSc (defined as the onset of the first non-Raynaud’s symptoms attributable to SSc in less than 3 yr) are more likely to experience SSc-ILD progression compared with a patient who has had SSc-ILD for 10 years.
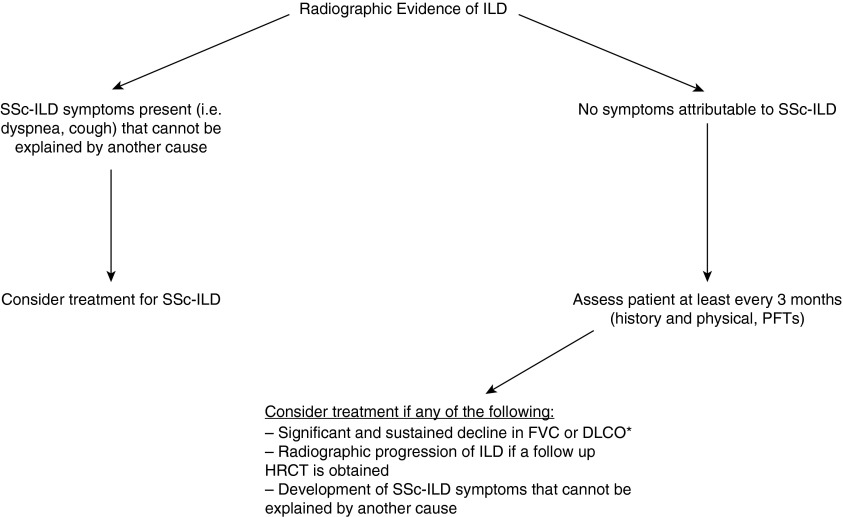
Figure 1 provides a broad outline of our rationale for initiating SSc-ILD–targeted therapy. We screen all patients with SSc for ILD by HRCT scanning at the time of presentation because radiographic signs of ILD can be found in the setting of a normal FVC (29). Notably, our outline does not apply an FVC threshold to guide the introduction for SSc-ILD–targeted therapy. The reason for this omission is that not all patients with an FVC less than 70%, for instance, may benefit from immunosuppressive therapy. As an example, the introduction of immunosuppressive therapy in a patient with an FVC of 67% may pose more harm than risk if this patient was diagnosed with SSc-ILD more than 5 years ago and has had a stable FVC for 2 years. Conversely, the introduction of immunosuppressive therapy may be prudent in a patient with an FVC of 80% if this patient was diagnosed with SSc-ILD within the last 5 years and has experienced a 15% reduction in FVC from the time of diagnosis.
Figure 1.
Proposed algorithm for the initiation of SSc-ILD (systemic sclerosis–associated interstitial lung disease)–targeted therapy. *We consider a clinically significant decline in FVC as greater than 10% and a decline in DlCO (diffusing capacity of the lung for carbon monoxide) as greater than 15%, in the absence of pulmonary hypertension. HRCT = high-resolution computed tomography; PFTs = pulmonary function tests.
Pathogenesis
The pathogenic model for SSc-ILD has rapidly evolved. Although no single pathway underlies the development of this condition, broadly speaking, the hallmark of SSc-ILD is the progression from initial inflammation and injury to an environment promoting a profibrotic milieu (30, 31). Specifically, one of the earliest pathogenic events in SSc-ILD appears to be injury to alveolar epithelial and endothelial cells (30). For example, markers of epithelial damage, such as Krebs von den Lungen-6 (KL-6) serum levels and 99mTc-diethylenetriaminepentaacetic acid (DTPA) clearance, predict both progression and severity of SSc-ILD (28, 32, 33).
Aberrant healing processes appear to accompany persistent injury to alveolar cells (30), leading to changes in epithelial cell morphology (34) and function (35). During this purported reparative phase, T lymphocytes secrete helper T-cell type 2 (Th2) cytokines, such as IL-4, which have direct profibrotic properties (36, 37). Higher IL-4 levels in BAL cells are associated with greater decline in pulmonary function in patients with SSc (38). In addition to Th2 cells, more recent studies have implicated Th17 and Th22 cells in the pathogenesis of SSc-ILD (39, 40).
In addition to the aforementioned cell mediators of fibrosis, transforming growth factor (TGF)-β appears to play a central role in the development and progression of fibrosis in SSc-ILD (30). Gene expression analyses have demonstrated that enhanced expression of TFG-β–dependent signaling pathways is associated with a higher likelihood of ILD in SSc (41). Moreover, SSc fibroblasts may be more resistant to the fibrotic-inhibitory potential of cytokines, such as IFN-γ (42).
A number of articles have elegantly reviewed the pathogenic components of SSc-ILD as described in Table 2 (30, 31, 43–45). These mediators represent potential targets for novel therapies of ILD in SSc.
Table 2.
Clinically and experimentally affirmed mediators of fibrosis relevant to pathogenesis of systemic sclerosis–associated interstitial lung disease*
| Cytokines: | TGF-β, IL-4, IL-6, IL-13, IL-17, IL-22, IL-33 |
| Chemokines: | CXCL12, CXCL4, MCP-1 |
| Cells: | Alveolar epithelial cells, fibroblasts, B cells |
| Growth factors: | CTGF, PDGF, IGFBP-5 |
| Signaling pathways: | Wnt family/β-catenin |
| Peptides: | Endothelin-1, adenosine receptor |
| Lipids: | Lysophosphatidic acid, prostaglandin F |
| Autoantibodies: | Anti–topoisomerase I, anti-fibroblast, anti-PDGF |
| Enzymes: | Thrombin |
Definition of abbreviations: CTGF = connective tissue growth factor; CXCL = chemokine (C-X-C motif) ligand; IGFBP-5 = insulin-like growth factor binding protein 5; MCP-1 = monocyte chemotactic protein 1; PDGF = platelet-derived growth factor; TGF = transforming growth factor.
Early Treatment Approaches
Historical regimens for SSc-ILD predominantly targeted inflammatory pathways. Low-dose glucocorticoids administered in combination with another immunosuppressant medication were the mainstay of treatment for patients with severe or progressive SSc-ILD (46). However, the advent of randomized, controlled clinical trials (RCTs) in SSc-ILD near the turn of the century helped to establish more evidence-based treatment approaches. The results of these trials did not substantiate the continued use of agents, such as d-penicillamine (47), chlorambucil (48), and glucocorticoids (49), for the treatment of SSc-ILD.
Cyclophosphamide
Cyclophosphamide was the first agent that was found in RCTs to stabilize the progression of SSc-ILD (50, 51). Two high-quality studies demonstrated efficacy of oral (51) and pulse (50) CYC compared with placebo for SSc-ILD. These findings were consistent with results from prior uncontrolled studies assessing the efficacy of CYC for treating SSc-ILD (52, 53).
In Scleroderma Lung Study (SLS) I (51), treatment with oral CYC for 12 months was associated with a modest improvement in the primary end point of FVC % predicted (2.53%; P < 0.03) compared with placebo in 158 patients with SSc-ILD. This study also reported improvements in several secondary end points, including patient-reported dyspnea, TLC % predicted, quality of life, and skin thickness, as well as extent of both visually assessed and computer-assisted quantitative lung fibrosis (54, 55). However, the benefits of CYC in SSc-ILD came at the expense of a high degree of adverse effects (51), including increased rates of leukopenia and neutropenia in the CYC arm. Furthermore, an analysis of SLS I data 1 year after treatment cessation revealed the loss of a significant CYC treatment effect (56). Specifically, by 24 months, there was no difference in the FVC or TLC between patients randomized to CYC versus placebo (56).
In the RCT investigating the efficacy of pulse CYC (50), Hoyles and colleagues randomized 45 patients with SSc-ILD to receive low-dose prednisolone and 6 infusions (monthly) of intravenous CYC followed by azathioprine versus placebo. Although there were no statistically significant between-treatment differences noted after 1 year in any of the outcome measures, there was a trend for a favorable effect on FVC in the active treatment group (P = 0.08). Notably, few adverse events were appreciated in the patients treated with intravenous CYC, and there were no differences in the rates of serious adverse effects between study arms. These findings suggest an improved safety profile of intravenous CYC compared with oral CYC, and may explain why pulse CYC is used more commonly in clinical practice.
Azathioprine
To our knowledge, no studies have rigorously evaluated the efficacy of azathioprine for induction therapy in patients with SSc-ILD. As mentioned previously, azathioprine was used after pulse CYC therapy in patients with SSc-ILD (50); however, no RCTs have compared azathioprine with placebo in patients with established SSc-ILD. Although azathioprine is used not infrequently for the management of connective tissue disease–related ILD, there is little evidence supporting the use of this agent for managing SSc-ILD.
Current Treatment Approaches: Mycophenolate
Because the benefit-to-risk ratio of CYC for SSc-ILD is somewhat inconclusive, researchers have been actively pursuing the study of alternative agents for SSc-ILD. Mycophenolate mofetil (MMF) is an immunosuppressive agent with both antifibrotic and immunomodulatory effects and appears to be well tolerated in SSc (57, 58).
A retrospective study of 172 patients with SSc both with and without ILD found a lower frequency of clinically significant pulmonary fibrosis, as well as improved survival, in the MMF-treated cohort (n = 109), compared with patients with SSc receiving other immunosuppressive medications (n = 63) (57). An uncontrolled prospective trial of 13 patients with SSc-ILD, all of whom presented with a significant decrease in FVC in the 12 months preceding trial entry, also demonstrated a significant improvement in FVC after 12 months (59). Additional prospective, observational studies have affirmed that MMF is safe, well tolerated, and may prevent pulmonary function deterioration in SSc-ILD (60–62).
Given the favorable effects of MMF in observational SSc-ILD studies, Tashkin and colleagues designed SLS II, the first RCT to compare MMF and CYC for the treatment of SSc-ILD (63). In this study, 142 patients were randomized between September 2009 and January 2013 and assigned to receive either MMF (titrated as tolerated to 3.0 g/d in divided doses) for 2 years or oral CYC (titrated as tolerated to 2 mg/kg once daily) for 1 year followed by an additional year on placebo, using a double-dummy design to maintain the blinding. The inclusion and exclusion criteria were similar to those for SLS I, and they are described in detail in the main manuscript (63).
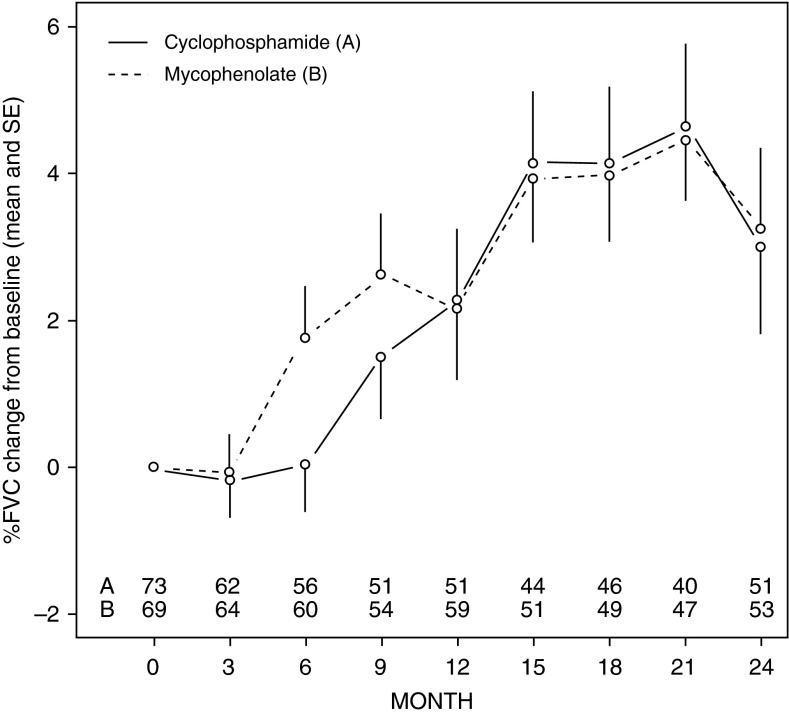
Among the 198 patients who underwent screening for SLS II, 142 were deemed eligible for participation. There were no significant differences in key baseline characteristics between patients assigned to CYC (n = 73) and MMF (n = 69). The primary end point of FVC % predicted significantly improved at 6–24 months in the MMF arm and at 12–24 months in the CYC arm compared with baseline (Table 3). However, there was no significant difference in the course of FVC % predicted over the 24-month trial between treatment arms by a joint model analysis, which controlled for baseline ILD disease severity and for time to withdrawal from treatment, deaths, and treatment failure (Figure 2). Most participants in the MMF (72%) and CYC (67%) arms showed improvements in FVC % predicted, and the majority of these participants had improvements of FVC greater than 5% predicted.
Table 3.
Mean changes (in absolute value) from baseline, with 95% confidence intervals, at 6, 12, 18, and 24 months: FVC % predicted, DlCO % predicted, DlCO/Va % predicted, TLC, mRSS, and TDI by treatment group*
| CYC |
MMF |
ΔMMF – ΔCYC |
||||
|---|---|---|---|---|---|---|
| Change | 95% CI | Change | 95% CI | Δ | 95% CI | |
| FVC % predicted |
||||||
| 6 mo | 0.40 | −0.9 to 1.7 | 0.94 | −0.4 to 2.3 | 0.54 | −1.3 to 2.4 |
| 12 mo | 2.10 | 0.60 to 3.60† | 2.31 | 0.84 to 3.78† | 0.21 | −1.9 to 2.3 |
| 18 mo | 3.16 | 1.69 to 4.64† | 2.54 | 1.12 to 3.96† | −0.62 | −2.7 to 1.4 |
| 24 mo | 2.88 | 1.19 to 4.58† | 2.19 | 0.53 to 3.84† | −0.70 | −3.1 to 1.7 |
| TLC % predicted | ||||||
| 6 mo | 0.11 | −1.34 to 1.56 | 1.37 | −0.16 to 2.85 | 1.26 | −0.9 to 3.4 |
| 12 mo | 0.80 | −0.71 to 2.3 | 0.99 | −0.51 to 2.50 | 0.19 | −2.0 to 2.3 |
| 18 mo | 1.49 | −0.30 to 3.29 | 0.62 | −1.16 to 2.39 | −0.87 | −3.4 to 1.6 |
| 24 mo | 0.45 | −1.43 to 2.32 | 1.24 | −0.68 to 3.18 | 0.80 | −2.0 to 3.6 |
| DlCO % predicted | ||||||
| 6 mo | −3.54 | −5.4 to –1.7† | 0.12 | −1.7 to 2.0 | 3.67 | 1.1 to 6.3 |
| 12 mo | −3.15 | −5.1 to –1.2† | 1.84 | −0.08 to 3.76 | 4.99 | 2.2 to 7.8 |
| 18 mo | −2.17 | −4.2 to –0.12† | 1.09 | −0.88 to 3.06 | 3.26 | 0.41 to 6.1 |
| 24 mo | −2.14 | −4.59 to 0.31 | −0.40 | −2.81 to 2.01 | 1.74 | −1.6 to 5.1 |
| DlCO/Va % predicted |
||||||
| 6 mo | −5.90 | −7.6 to –4.2† | −1.03 | −2.7 to 0.7 | 4.88 | 2.5 to 7.3† |
| 12 mo | −5.94 | −7.7 to –4.1† | −0.03 | −1.8 to 1.8 | 5.90 | 3.4 to 8.4† |
| 18 mo | −4.62 | −6.5 to –2.7† | 1.09 | −0.88 to 3.1 | 3.26 | 0.40 to 6.1† |
| 24 mo | −3.43 | −5.7 to –1.2† | −2.46 | −4.7 to –0.2† | 0.96 | −2.2 to 4.1 |
| TDI | ||||||
| 6 mo | 0.32 | −0.4 to 1.1 | 0.87 | 0.13 to 1.60† | 0.54 | −0.5 to 1.6 |
| 12 mo | 0.89 | 0.12 to 1.67† | 0.87 | 0.11 to 1.64† | −0.02 | −1.1 to 1.1 |
| 18 mo | 1.46 | 0.57 to 2.40† | 0.88 | −0.03 to 1.8 | −0.58 | −1.9 to 1.0 |
| 24 mo | 2.16 | 1.14 to 3.18† | 1.77 | 0.75 to 2.79† | −0.39 | −1.8 to 1.0 |
| mRSS | ||||||
| 6 mo | −1.57 | −2.8 to 0.3 | −0.83 | −2.0 to 0.34 | 0.75 | −0.9 to 2.4 |
| 12 mo | −3.57 | −4.9 to –2.† | −3.33 | −4.7 to –2.0† | 0.24 | −1.7 to 2.2 |
| 18 mo | −4.49 | −5.8 to –3.2† | −4.25 | −5.5 to –3.0† | 0.25 | −1.6 to 2.1 |
| 24 mo | −5.35 | −6.9 to –3.8† | −4.90 | −6.4 to –3.4† | 0.45 | −1.7 to 2.6 |
| QLF-WL‡ | 1.13 | −1.71 to 3.98 | 2.15 | −0.72 to 5.03 | 1.02 | −2.99 to 5.03 |
| QLF-LM‡ | −0.27 | −1.43 to 1.69 | 0.12 | −1.02 to 1.26 | 0.39 | −1.27 to 2.05 |
| QILD-WL‡ | −1.84 | −5.16 to 1.46 | −0.95 | −4.1 to 2.2 | 0.89 | −3.58 to 5.36 |
| QILD-LM‡ | −2.78 | −5.17 to –0.40† | −2.51 | −4.9 to –0.15† | 0.27 | −3.09 to 3.67 |
Definition of abbreviations: Δ = change; CI = confidence interval; CYC = cyclophosphamide; DlCO = diffusing capacity of the lung for carbon monoxide; DlCO/Va = ratio of DlCO to alveolar volume; MMF = mycophenolate mofetil; mRSS = modified Rodnan skin (skin thickness) score; QILD-LM = quantitative interstitial lung disease score-lobe of most involvement; QILD-WL = quantitative interstitial lung disease score-whole lung; QLF-LM = quantitative lung fibrosis score-lobe of most involvement; QLF-WL = quantitative lung fibrosis score-whole lung; TDI = transitional dyspnea index.
With between-treatment differences based on estimates from the joint model from Scleroderma Lung Study II (63).
P < 0.05.
At 24 months.
Figure 2.
Absolute observed changes from baseline in FVC % predicted by treatment arm (all observed data, intention-to-treat principle applied) (63). Group A, cyclophosphamide (CYC); group B, mycophenolate mofetil (MMF). Vertical bars represent the SEM.
Similar to the FVC, both treatments resulted in significant improvements in dyspnea (as measured by the transitional dyspnea index, or TDI) and skin thickness scores (mRSS [modified Rodnan skin score]) from 12 to 24 months after randomization; however, there were no significant between-treatment differences in TDI and mRSS outcomes.
The DlCO % predicted and DlCO/Va % predicted both declined in both treatment arms, although the declines were significantly greater in the CYC versus MMF arms. The latter finding warrants further attention as it could suggest a potential role of MMF in preventing deleterious vascular remodeling and/or the development of pulmonary hypertension, as suggested by observational studies (64) and preclinical data (65).
One of the most striking observations from SLS II was the relatively poor safety and tolerability of CYC compared with MMF. Specifically, a significantly larger proportion of participants assigned to CYC discontinued the drug prematurely, and among participants who withdrew from the study drug, the time interval for withdrawing was significantly shorter in the CYC arm compared with the MMF arm. Furthermore, almost twice as many patients in the CYC arm discontinued the study drug prematurely because of an adverse event, patient request, death, or protocol-defined treatment failure compared with those assigned to MMF. In addition, the only deaths or treatment failures (which transpired while taking the study drug) occurred in patients assigned to CYC. Finally, the serious adverse events judged by the mortality and morbidity committee to be attributable to drug toxicity occurred more often in the patients receiving CYC (n = 8) than among those receiving MMF (n = 3). A limitation of this study was the choice of oral CYC over intravenous CYC, in view of evidence suggesting that intravenous CYC might be safer and better tolerated.
This pivotal trial supports the continued use of CYC and MMF for patients with SSc with clinically significant ILD in the absence of pulmonary hypertension, based on the noted improvements in the FVC, TLC, dyspnea (TDI), and mRSS study end points. However, the findings suggest that SSc providers should closely monitor patients receiving CYC for tolerability and safety issues.
Investigational Therapeutic Targets
A number of investigational therapeutic targets exist for SSc-ILD as summarized below. Table 4 describes additional experimental agents presently under study in SSc-ILD therapeutic clinical trials.
Table 4.
Current active clinical trials investigating experimental therapeutic agents for systemic sclerosis–associated interstitial lung disease*
| Agent | Mechanism of Action | Primary End Point | Design | Phase |
|---|---|---|---|---|
| Pomalidomide | Derivative of thalidomide (antiangiogenic, immunomodulatory) | Change in FVC, mRSS at 52 wk | Double-blind RCT | II |
| Belimumab | BAFF inhibitor | Change in skin score (secondary outcomes: change in FVC, DlCO) at 48 wk | Double-blind RCT | II |
| Tadalafil† | PDE5 inhibitor | Change in FVC over 6 mo | Double-blind RCT | III |
| Nilotinib | Tyrosine kinase inhibitor | Safety and tolerability (secondary outcomes: change in skin score, PFT) at 6 mo | Open-label pilot study | IIa |
| Abatacept | Selective T-cell costimulation modulator | Safety and tolerability; change in skin score (secondary outcomes: change in FVC, joint count) at 12 mo | Double-blind RCT | II |
| Nintedanib | Tyrosine kinase inhibitor | Annual rate of decline in FVC over 12 mo | Double-blind RCT | III |
| Abituzumab | Monoclonal IgG2 antibody targeting αv-integrins | Safety and tolerability; change in FVC at 12 mo | Double-blind RCT | II |
| Bortezomib | TGF-signaling inhibitor | Safety and tolerability (secondary outcomes: FVC, skin score, HRQOL) at 48 wk | Double-blind RCT | II |
| Dabigatran | Thrombin inhibitor | Safety (secondary outcomes: skin score, lung fibroblasts) at 6 mo | Open-label single group | I |
Definition of abbreviations: BAFF = B-cell activating factor belonging to the tumor necrosis factor family; DlCO = diffusing capacity of the lung for carbon monoxide; HRQOL = health-related quality of life; mRSS = modified Rodnan skin (skin thickness) score; PDE5 = phosphodiesterase-5; PFT = pulmonary function test; RCT = randomized controlled trial; TGF = transforming growth factor.
According to clinicaltrials.gov as of May 2016.
Study has been completed; awaiting results.
B-cell depletion
Accumulating evidence supports the possibility that B-cell function may contribute to the pathogenesis of SSc-ILD (66). B-cell infiltration was a prominent finding in lung biopsies from 11 patients with SSc-associated ILD (67). Moreover, in 73 patients with SSc-ILD, ILD progression was associated with a higher CD19 percentage in BAL fluid (68). Clinical evidence exists supporting the therapeutic use of B-cell depletion in SSc-ILD. Open-label trials (69, 70), case reports (71), and one RCT (72) have demonstrated a possible role for rituximab, a chimeric monoclonal antibody against CD20, in the management of patients with SSc-ILD. In one prospective, observational study, 20 patients with SSc with diffuse disease had a significant increase in FVC and TLC at 12 months compared with baseline after treatment with rituximab (8 of whom received repeat infusions of rituximab at undisclosed intervals over the course of the 12-mo trial) (70). A study comparing CYC and rituximab as induction therapy for SSc-ILD is currently underway in the United Kingdom.
Endothelin-1 antagonists
Endothelin-1 stimulates the formation of smooth muscle cells and the production of collagen in fibroblasts (73), and levels of this profibrotic cytokine are elevated in BAL fluid of patients with SSc-ILD (74). Although endothelin receptor antagonists are now used routinely for the management of pulmonary hypertension in SSc (75), the data supporting the use of these agents for SSc-ILD are not convincing (76, 77). A large RCT (n = 163) of patients with SSc-ILD found no difference in change in exercise capacity, FVC, or DlCO in patients receiving bosentan compared with placebo (77).
IL-6 blockade
Serum IL-6 is elevated in patients with SSc (78), especially among patients with diffuse cutaneous SSc (79). Moreover, higher levels of this cytokine are associated with more severe skin involvement and worse long-term survival (79). Exploratory analyses of data from a phase II trial comparing tocilizumab with placebo in patients with SSc (with the primary end point of change in skin score) revealed that fewer patients assigned to tocilizumab demonstrated a decline in FVC % predicted compared with placebo (57 vs. 84%) at Week 48 (80). A phase III trial has been initiated, the results of which should provide further insights into the effectiveness of tocilizumab in preventing disease progression in SSc-ILD.
Tyrosine kinase inhibitors
Small-molecule inhibitors of intracellular kinases have shown some promise for treating SSc-ILD. Preclinical studies demonstrated that imatinib mesylate, which blocks the tyrosine kinase activity of platelet-derived growth factor (PDGF) receptors, inhibited lung fibrosis in the bleomycin-induced mouse model of pulmonary fibrosis (81). However, a phase I/II open-label study of imatinib mesylate for SSc-ILD yielded disappointing findings and an unfavorable safety profile (82). One of the criticisms of this study was that the dose of imatinib mesylate may have been too high. Additional studies have yielded conflicting results regarding treatment with imatinib in SSc, with some studies demonstrating positive findings (83, 84) and others demonstrating negative findings (85, 86). A more recent study assessed the efficacy and safety of low-dose imatinib in 30 patients with SSc and active pulmonary involvement (classified as HRCT-defined ILD or BAL-confirmed alveolitis), unresponsive to CYC (87). This study found that lung function improved or stabilized in 73% of patients after 6 months of treatment and that the lower dose prescribed was well tolerated among the patients. Taken together, the findings of these studies suggest that low-dose imatinib may be efficacious in selected patients with SSc-ILD; however, future RCTs are needed.
Nintedanib is another tyrosine kinase inhibitor, which inhibits several profibrotic pathways and is less selective than imatinib (88). The FDA has approved nintedanib for the treatment of idiopathic pulmonary fibrosis (IPF) (89). Preclinical data have demonstrated that this agent improved fibrosis in bleomycin-induced skin fibrosis, in a chronic graft-versus-host disease model, as well as in tight-skin-1 mice (90). A phase III, double-blind RCT evaluating the efficacy and safety of oral nintedanib in patients with SSc-ILD has commenced.
Antifibrotic therapy
The antifibrotic agent pirfenidone is a pyridine compound approved for the treatment of IPF (91). The antifibrotic properties of pirfenidone are likely mediated through its effects on TGF-β (92). This agent also possesses antiinflammatory properties, which may be attributable to its inhibitory effects on IL-1β, IL-6, tumor necrosis factor-α, and PDGF in animal models of pulmonary fibrosis (92, 93). In a study of six patients with diffuse cutaneous SSc, pirfenidone curtailed collagen production via TGF-β1 and connective tissue growth factor pathways in skin fibroblasts from patients with SSc (94).
Early clinical data suggest that pirfenidone may ameliorate SSc-ILD (95, 96). A case series demonstrated an improvement in FVC % predicted in five patients treated with pirfenidone (95). Furthermore, in a 16-week, open-label trial of pirfenidone in SSc-ILD (n = 63), 10 patients had an increase (≥5%) and 5 patients had a decrease (>5%) in FVC % predicted (the median change from baseline in FVC % predicted was 0.5%) (96). Of note, 40% of the patients enrolled in this trial were also taking mycophenolate. A larger and longer randomized placebo-controlled trial of pirfenidone on a background of mycophenolate in patients with SSc-ILD is currently in the planning stage.
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation (HSCT) has emerged as a potentially effective treatment option for carefully selected patients with progressive diffuse SSc with a poor prognosis (97). To date, nearly all experience is with autologous HSCT (98). Early trials demonstrated the feasibility of autologous HSCT after intense immunosuppression in diffuse SSc and found a significant reduction in skin score, as well as stabilization in pulmonary function (97).
The Autologous Stem Cell Transplantation International Scleroderma (ASTIS) trial was the first completed phase III RCT comparing the efficacy and safety of autologous HSCT versus monthly intravenous CYC for 12 months (99). This 29-center study included 156 patients with diffuse SSc (duration, <4 yr) and without serious comorbidities. In the first year, mortality was higher in the HSCT group (eight treatment-related deaths) compared with the CYC group (no treatment-related deaths); however, over a median follow-up time of 5.8 years, the HSCT group experienced significantly better event-free survival; events included the need for dialysis and the need for oxygen (99). Although no significant changes were seen for DlCO, a modest yet statistically significant increase in FVC was seen in the HSCT group (99). Results of the North American phase III RCT (the SCOT [Scleroderma: Cyclophosphamide or Transplantation] trial) are awaiting publication. Future studies are needed to evaluate long-term potential HSCT-related complications (i.e., infertility, secondary autoimmune disease, and malignancy) to determine the appropriate timing of HSCT and to optimize the patient selection criteria to minimize early HSCT-related mortality.
Lung Transplantation
Deemed a last-resort intervention for patients with end-stage lung disease, lung transplantation is presently performed at select transplantation centers for patients with SSc. The literature in this area is evolving, and although a retrospective cohort study found a 48% increase in the 1-year mortality rate among patients with SSc undergoing lung transplantation in the United States compared with those with non–SSc-ILD (100), other studies have not found any difference in survival after lung transplantation between patients with SSc and non-SSc patients with fibrotic lung diseases (101–104).
Factors associated with higher mortality in patients with SSc-ILD undergoing lung transplantation include older age (104) and elevated body mass index (103). However, contrary to previous thought, severity of esophageal dysfunction by either morphometry or manometry criteria was not associated with survival in patients with SSc-ILD (n = 35) who underwent lung transplantation at a single center (104). These findings are consistent with a prior single-center study, which found no association with the presence of esophageal dysfunction and survival (102). These results should be interpreted with caution, however, as the majority of studies in this area are retrospective analyses and relatively small, single-center experiences. To adequately assess morbidity and mortality outcomes in patients with SSc-ILD undergoing lung transplantation, larger, multicenter studies are needed.
Future Considerations
SSc-ILD Outcome Measures
As novel agents are increasingly introduced into the SSc-ILD research arena, there is a growing need to reach a consensus on the optimal measure(s) of treatment response in SSc-ILD trials (105). Although FVC has traditionally served as the primary end point in SSc-ILD clinical trials (50, 51), treatment with CYC, for instance, has also been associated with improvement in other clinically relevant end points, including TLC, self-reported quality of life, and dyspnea (51), as well as improvement in fibrosis on HRCT imaging (54, 55). Moreover, the FVC is a less direct surrogate measure of lung fibrosis compared with the quantitative fibrosis score derived from quantitative image analysis of HRCT scans and, like other physiological variables such as the TLC, may have diminished reproducibility if certain quality criteria are not met (106).
We created a composite outcome measure composed of structural (HRCT), physiological, and patient-reported end points based on data from SLS I (107). Although single study end points are useful for measuring definitive outcomes such as mortality, a single end point may not be the best measure of overall treatment response in SSc-ILD, based on the logical assumption that clinical outcomes of SSc-ILD result from a combination of patient-oriented outcomes and physiological and anatomical outcomes (108). The efforts of the Outcome Measures in Rheumatology (OMERACT) Connective Tissue Disease—Interstitial Lung Diseases (CTD-ILD) Working Group have underscored the importance of including patient-oriented outcomes in trials, as patients from this working group identified cough and dyspnea as the most important features of their experience with ILD (105). Future studies are needed to validate this composite outcome measure.
Predictors of Treatment Response
In addition to SSc-ILD trial end-point measures, it is essential to reach agreement on optimal predictors of treatment response. Experts concur that future studies should employ “cohort enrichment” paradigms (109), in which patients with SSc-ILD meeting certain criteria are selectively enrolled to maximize response to therapy. Although there is no uniform agreement on how to predict treatment response, there is early evidence from Silver and colleagues (52) that patients with a significant decline in FVC before trial entry may derive the greatest benefit from therapy. Moreover, a retrospective study of 122 patients with SSc-ILD undergoing treatment found that shorter disease duration was the only factor that was associated with improvement in FVC % predicted (110). Specifically, patients with pulmonary symptoms less than 1.9 years from the time therapy was initiated had the best prognosis.
Post hoc analyses of SLS I data revealed that specific baseline variables were independently associated with treatment response (111). For example, patients with 50% or more involvement of reticular infiltrates (in any lung zone, defined as upper, middle, and lower area–equivalent zones in each lung) on HRCT, which is more or less equivalent to approximately 25% involvement of the whole lung, and/or an mRSS of at least 23 at baseline had the best response to CYC therapy. Interestingly, patients with less severe HRCT findings and lower mRSS exhibited no improvement with CYC therapy.
Additional analyses are needed to determine specific enrichment criteria for future SSc-ILD. Analyses are currently underway using SLS II data to ascertain whether baseline severity of quantitative lung fibrosis and mRSS predict CYC- and/or MMF-related treatment response.
Maintenance Therapy
The majority of trials in SSc-ILD have evaluated induction therapy for SSc-ILD. Although there is a general agreement among SSc experts that maintenance therapy is needed to preserve the benefits achieved in the induction phase and to prevent relapses (112), no studies have compared maintenance treatment regimens after an induction phase in SSc-ILD. Furthermore, no studies have identified which patients may derive the greatest benefit from maintenance therapy. There is limited evidence based on a retrospective study of only 20 patients that azathioprine (AZA) may have a role as maintenance therapy in patients who have completed an induction course of intravenous CYC (113).
A more recent study discovered that patients who responded favorably to pulse CYC and were subsequently treated with AZA had a higher incidence of improvement or stabilization in lung function compared with patients who did not respond to pulse CYC and were subsequently treated with MMF (114). However, this study did not evaluate the effectiveness of MMF maintenance therapy in patients who demonstrated a response to induction therapy.
Preliminary results of the ongoing SLS II long-term morbidity and mortality study suggest that mycophenolate appears to be the current drug of choice for maintenance therapy among SSc providers in the United States. Of the patients who have responded to our long-term follow-up survey, approximately 70% started MMF after stopping the study drug, whereas only 3% started AZA. We are collecting outcome data up to 5 years after randomization for this study, and the results may reveal important insights into the role of MMF as maintenance therapy in SSc-ILD.
In addition to selecting an optimal maintenance treatment regimen, more research is also needed to determine the appropriate duration of maintenance therapy. Our practice is to consider treating patients who demonstrate therapy-related improvement or stability in SSc-ILD with maintenance medication for at least 2 years, and in many cases, therapy is often continued for a longer period if there are signs of continued SSc-ILD disease activity, as indicated by serial follow-up spirometry demonstrating further declines in FVC % predicted in conjunction with progression of SSc-ILD on HRCT imaging. Of note, some patients with SSc-ILD will receive immunosuppression for other indications (i.e., progression of cutaneous sclerosis) during and beyond the maintenance phase.
Conclusions
Numerous research studies have propelled advances in the treatment of SSc-ILD. Data from high-quality RCTs substantiate the use of CYC and MMF in patients with severe, progressive SSc-ILD. Preclinical and early clinical data have revealed a number of other promising therapeutic agents on the horizon for SSc-ILD, including rituximab, tocilizumab, pirfenidone, nintedanib, and HSCT. Future studies are needed to determine how to select patients for trials who may derive the greatest benefit from SSc-ILD therapy, how to best measure treatment response, how to manage patients after induction therapy, and how long to treat patients with maintenance medication to optimize long-term outcomes among patients with SSc-ILD.
Footnotes
Supported by the National Heart, Lung, and Blood Institute (R01 HL089758 and R01 HL 089901) (Scleroderma Lung Study II).
Author Disclaimer: The views expressed in this article do not communicate an official position of the NHLBI.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Elhai M, Meune C, Avouac J, Kahan A, Allanore Y. Trends in mortality in patients with systemic sclerosis over 40 years: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford) 2012;51:1017–1026. doi: 10.1093/rheumatology/ker269. [DOI] [PubMed] [Google Scholar]
- 2.Tyndall AJ, Bannert B, Vonk M, Airò P, Cozzi F, Carreira PE, Bancel DF, Allanore Y, Müller-Ladner U, Distler O, et al. Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis. 2010;69:1809–1815. doi: 10.1136/ard.2009.114264. [DOI] [PubMed] [Google Scholar]
- 3.Launay D, Remy-Jardin M, Michon-Pasturel U, Mastora I, Hachulla E, Lambert M, Delannoy V, Queyrel V, Duhamel A, Matran R, et al. High resolution computed tomography in fibrosing alveolitis associated with systemic sclerosis. J Rheumatol. 2006;33:1789–1801. [PubMed] [Google Scholar]
- 4.De Santis M, Bosello S, La Torre G, Capuano A, Tolusso B, Pagliari G, Pistelli R, Danza FM, Zoli A, Ferraccioli G. Functional, radiological and biological markers of alveolitis and infections of the lower respiratory tract in patients with systemic sclerosis. Respir Res. 2005;6:96. doi: 10.1186/1465-9921-6-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouros D, Wells AU, Nicholson AG, Colby TV, Polychronopoulos V, Pantelidis P, Haslam PL, Vassilakis DA, Black CM, du Bois RM. Histopathologic subsets of fibrosing alveolitis in patients with systemic sclerosis and their relationship to outcome. Am J Respir Crit Care Med. 2002;165:1581–1586. doi: 10.1164/rccm.2106012. [DOI] [PubMed] [Google Scholar]
- 6.Reveille JD, Solomon DH American College of Rheumatology Ad Hoc Committee of Immunologic Testing Guidelines. Evidence-based guidelines for the use of immunologic tests: anticentromere, Scl-70, and nucleolar antibodies. Arthritis Rheum. 2003;49:399–412. doi: 10.1002/art.11113. [DOI] [PubMed] [Google Scholar]
- 7.Steen VD. Autoantibodies in systemic sclerosis. Semin Arthritis Rheum. 2005;35:35–42. doi: 10.1016/j.semarthrit.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Steen VD, Conte C, Owens GR, Medsger TA., Jr Severe restrictive lung disease in systemic sclerosis. Arthritis Rheum. 1994;37:1283–1289. doi: 10.1002/art.1780370903. [DOI] [PubMed] [Google Scholar]
- 9.Mayes MD, Lacey JV, Jr, Beebe-Dimmer J, Gillespie BW, Cooper B, Laing TJ, Schottenfeld D. Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large US population. Arthritis Rheum. 2003;48:2246–2255. doi: 10.1002/art.11073. [DOI] [PubMed] [Google Scholar]
- 10.Wells AU. Pulmonary function tests in connective tissue disease [review] Semin Respir Crit Care Med. 2007;28:379–388. doi: 10.1055/s-2007-985610. [DOI] [PubMed] [Google Scholar]
- 11.Desai SR, Veeraraghavan S, Hansell DM, Nikolakopolou A, Goh NS, Nicholson AG, Colby TV, Denton CP, Black CM, du Bois RM, et al. CT features of lung disease in patients with systemic sclerosis: comparison with idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia. Radiology. 2004;232:560–567. doi: 10.1148/radiol.2322031223. [DOI] [PubMed] [Google Scholar]
- 12.Goh NS, Veeraraghavan S, Desai SR, Cramer D, Hansell DM, Denton CP, Black CM, du Bois RM, Wells AU. Bronchoalveolar lavage cellular profiles in patients with systemic sclerosis–associated interstitial lung disease are not predictive of disease progression. Arthritis Rheum. 2007;56:2005–2012. doi: 10.1002/art.22696. [DOI] [PubMed] [Google Scholar]
- 13.Strange C, Bolster MB, Roth MD, Silver RM, Theodore A, Goldin J, Clements P, Chung J, Elashoff RM, Suh R, et al. Scleroderma Lung Study Research Group. Bronchoalveolar lavage and response to cyclophosphamide in scleroderma interstitial lung disease. Am J Respir Crit Care Med. 2008;177:91–98. doi: 10.1164/rccm.200705-655OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steen VD, Medsger TA., Jr Severe organ involvement in systemic sclerosis with diffuse scleroderma. Arthritis Rheum. 2000;43:2437–2444. doi: 10.1002/1529-0131(200011)43:11<2437::AID-ANR10>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 15.Morgan C, Knight C, Lunt M, Black CM, Silman AJ. Predictors of end stage lung disease in a cohort of patients with scleroderma. Ann Rheum Dis. 2003;62:146–150. doi: 10.1136/ard.62.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plastiras SC, Karadimitrakis SP, Ziakas PD, Vlachoyiannopoulos PG, Moutsopoulos HM, Tzelepis GE. Scleroderma lung: initial forced vital capacity as predictor of pulmonary function decline. Arthritis Rheum. 2006;55:598–602. doi: 10.1002/art.22099. [DOI] [PubMed] [Google Scholar]
- 17.Nihtyanova SI, Schreiber BE, Ong VH, Rosenberg D, Moinzadeh P, Coghlan JG, Wells AU, Denton CP. Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheumatol. 2014;66:1625–1635. doi: 10.1002/art.38390. [DOI] [PubMed] [Google Scholar]
- 18.Goh NSL, Desai SR, Veeraraghavan S, Hansell DM, Copley SJ, Maher TM, Corte TJ, Sander CR, Ratoff J, Devaraj A, et al. Interstitial lung disease in systemic sclerosis: a simple staging system. Am J Respir Crit Care Med. 2008;177:1248–1254. doi: 10.1164/rccm.200706-877OC. [DOI] [PubMed] [Google Scholar]
- 19.Moore OA, Goh N, Corte T, Rouse H, Hennessy O, Thakkar V, Byron J, Sahhar J, Roddy J, Gabbay E, et al. Extent of disease on high-resolution computed tomography lung is a predictor of decline and mortality in systemic sclerosis–related interstitial lung disease. Rheumatology (Oxford) 2013;52:155–160. doi: 10.1093/rheumatology/kes289. [DOI] [PubMed] [Google Scholar]
- 20.Khanna D, Tseng CH, Farmani N, Steen V, Furst DE, Clements PJ, Roth MD, Goldin J, Elashoff R, Seibold JR, et al. Clinical course of lung physiology in patients with scleroderma and interstitial lung disease: analysis of the Scleroderma Lung Study Placebo Group. Arthritis Rheum. 2011;63:3078–3085. doi: 10.1002/art.30467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assassi S, Sharif R, Lasky RE, McNearney TA, Estrada-Y-Martin RM, Draeger H, Nair DK, Fritzler MJ, Reveille JD, Arnett FC, et al. GENISOS Study Group. Predictors of interstitial lung disease in early systemic sclerosis: a prospective longitudinal study of the GENISOS cohort. Arthritis Res Ther. 2010;12:R166. doi: 10.1186/ar3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Lauretis A, Sestini P, Pantelidis P, Hoyles R, Hansell DM, Goh NS, Zappala CJ, Visca D, Maher TM, Denton CP, et al. Serum interleukin 6 is predictive of early functional decline and mortality in interstitial lung disease associated with systemic sclerosis. J Rheumatol. 2013;40:435–446. doi: 10.3899/jrheum.120725. [DOI] [PubMed] [Google Scholar]
- 23.Liu X, Mayes MD, Pedroza C, Draeger HT, Gonzalez EB, Harper BE, Reveille JD, Assassi S. Does C-reactive protein predict the long-term progression of interstitial lung disease and survival in patients with early systemic sclerosis? Arthritis Care Res (Hoboken) 2013;65:1375–1380. doi: 10.1002/acr.21968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu M, Pedroza C, Salazar G, Zhou X, Reveille J, Mayes MD, Assassi S. Plasma MCP-1 and IL-10 levels predict long-term progression of interstitial lung disease in patients with early systemic sclerosis [abstract] Arthritis Rheum. 2013;65:S742. doi: 10.1002/acr.21968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tiev KP, Hua-Huy T, Kettaneh A, Gain M, Duong-Quy S, Tolédano C, Cabane J, Dinh-Xuan AT. Serum CC chemokine ligand-18 predicts lung disease worsening in systemic sclerosis. Eur Respir J. 2011;38:1355–1360. doi: 10.1183/09031936.00004711. [DOI] [PubMed] [Google Scholar]
- 26.Schupp J, Becker M, Günther J, Müller-Quernheim J, Riemekasten G, Prasse A. Serum CCL18 is predictive for lung disease progression and mortality in systemic sclerosis. Eur Respir J. 2014;43:1530–1532. doi: 10.1183/09031936.00131713. [DOI] [PubMed] [Google Scholar]
- 27.van Bon L, Affandi AJ, Broen J, Christmann RB, Marijnissen RJ, Stawski L, Farina GA, Stifano G, Mathes AL, Cossu M, et al. Proteome-wide analysis and CXCL4 as a biomarker in systemic sclerosis. N Engl J Med. 2014;370:433–443. doi: 10.1056/NEJMoa1114576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yanaba K, Hasegawa M, Takehara K, Sato S. Comparative study of serum surfactant protein-D and KL-6 concentrations in patients with systemic sclerosis as markers for monitoring the activity of pulmonary fibrosis. J Rheumatol. 2004;31:1112–1120. [PubMed] [Google Scholar]
- 29.Suliman YA, Dobrota R, Huscher D, Nguyen-Kim TD, Maurer B, Jordan S, Speich R, Frauenfelder T, Distler O. Brief report: pulmonary function tests: high rate of false-negative results in the early detection and screening of scleroderma-related interstitial lung disease. Arthritis Rheumatol. 2015;67:3256–3261. doi: 10.1002/art.39405. [DOI] [PubMed] [Google Scholar]
- 30.Akter T, Silver RM, Bogatkevich GS. Recent advances in understanding the pathogenesis of scleroderma-interstitial lung disease. Curr Rheumatol Rep. 2014;16:411. doi: 10.1007/s11926-014-0411-1. [DOI] [PubMed] [Google Scholar]
- 31.Bhattacharyya S, Wei J, Varga J. Understanding fibrosis in systemic sclerosis: shifting paradigms, emerging opportunities. Nat Rev Rheumatol. 2011;8:42–54. doi: 10.1038/nrrheum.2011.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hant FN, Ludwicka-Bradley A, Wang HJ, Li N, Elashoff R, Tashkin DP, Silver RM Scleroderma Lung Study Research Group. Surfactant protein D and KL-6 as serum biomarkers of interstitial lung disease in patients with scleroderma. J Rheumatol. 2009;36:773–780. doi: 10.3899/jrheum.080633. [DOI] [PubMed] [Google Scholar]
- 33.Fanti S, De Fabritiis A, Aloisi D, Dondi M, Marengo M, Compagnone G, Fallani F, Cavalli A, Monetti N. Early pulmonary involvement in systemic sclerosis assessed by technetium-99m-DTPA clearance rate. J Nucl Med. 1994;35:1933–1936. [PubMed] [Google Scholar]
- 34.Willis BC, Borok Z. TGF-β–induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007;293:L525–L534. doi: 10.1152/ajplung.00163.2007. [DOI] [PubMed] [Google Scholar]
- 35.Homer RJ, Herzog EL. Recent advances in pulmonary fibrosis: implications for scleroderma. Curr Opin Rheumatol. 2010;22:683–689. doi: 10.1097/BOR.0b013e32833ddcc9. [DOI] [PubMed] [Google Scholar]
- 36.Postlethwaite AE, Holness MA, Katai H, Raghow R. Human fibroblasts synthesize elevated levels of extracellular matrix proteins in response to interleukin 4. J Clin Invest. 1992;90:1479–1485. doi: 10.1172/JCI116015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parel Y, Aurrand-Lions M, Scheja A, Dayer JM, Roosnek E, Chizzolini C. Presence of CD4+CD8+ double-positive T cells with very high interleukin-4 production potential in lesional skin of patients with systemic sclerosis. Arthritis Rheum. 2007;56:3459–3467. doi: 10.1002/art.22927. [DOI] [PubMed] [Google Scholar]
- 38.Atamas SP, Yurovsky VV, Wise R, Wigley FM, Goter Robinson CJ, Henry P, Alms WJ, White B. Production of type 2 cytokines by CD8+ lung cells is associated with greater decline in pulmonary function in patients with systemic sclerosis. Arthritis Rheum. 1999;42:1168–1178. doi: 10.1002/1529-0131(199906)42:6<1168::AID-ANR13>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 39.Truchetet ME, Brembilla NC, Montanari E, Allanore Y, Chizzolini C. Increased frequency of circulating Th22 in addition to Th17 and Th2 lymphocytes in systemic sclerosis: association with interstitial lung disease. Arthritis Res Ther. 2011;13:R166. doi: 10.1186/ar3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murata M, Fujimoto M, Matsushita T, Hamaguchi Y, Hasegawa M, Takehara K, Komura K, Sato S. Clinical association of serum interleukin-17 levels in systemic sclerosis: is systemic sclerosis a Th17 disease? J Dermatol Sci. 2008;50:240–242. doi: 10.1016/j.jdermsci.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 41.Sargent JL, Milano A, Bhattacharyya S, Varga J, Connolly MK, Chang HY, Whitfield ML. A TGFβ-responsive gene signature is associated with a subset of diffuse scleroderma with increased disease severity. J Invest Dermatol. 2010;130:694–705. doi: 10.1038/jid.2009.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chizzolini C, Rezzonico R, Ribbens C, Burger D, Wollheim FA, Dayer JM. Inhibition of type I collagen production by dermal fibroblasts upon contact with activated T cells: different sensitivity to inhibition between systemic sclerosis and control fibroblasts. Arthritis Rheum. 1998;41:2039–2047. doi: 10.1002/1529-0131(199811)41:11<2039::AID-ART20>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 43.Chizzolini C, Brembilla NC, Montanari E, Truchetet ME. Fibrosis and immune dysregulation in systemic sclerosis. Autoimmun Rev. 2011;10:276–281. doi: 10.1016/j.autrev.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 44.Gilbane AJ, Denton CP, Holmes AM. Scleroderma pathogenesis: a pivotal role for fibroblasts as effector cells. Arthritis Res Ther. 2013;15:215. doi: 10.1186/ar4230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jain S, Shahane A, Derk CT. Interstitial lung disease in systemic sclerosis: pathophysiology, current and new advances in therapy. Inflamm Allergy Drug Targets. 2012;11:266–277. doi: 10.2174/187152812800959013. [DOI] [PubMed] [Google Scholar]
- 46.Au K, Khanna D, Clements PJ, Furst DE, Tashkin DP. Current concepts in disease-modifying therapy for systemic sclerosis–associated interstitial lung disease: lessons from clinical trials. Curr Rheumatol Rep. 2009;11:111–119. doi: 10.1007/s11926-009-0016-2. [DOI] [PubMed] [Google Scholar]
- 47.Clements PJ, Furst DE, Wong WK, Mayes M, White B, Wigley F, Weisman MH, Barr W, Moreland LW, Medsger TA, Jr, et al. High-dose versus low-dose d-penicillamine in early diffuse systemic sclerosis: analysis of a two-year, double-blind, randomized, controlled clinical trial. Arthritis Rheum. 1999;42:1194–1203. doi: 10.1002/1529-0131(199906)42:6<1194::AID-ANR16>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 48.Furst DE, Clements PJ, Hillis S, Lachenbruch PA, Miller BL, Sterz MG, Paulus HE. Immunosuppression with chlorambucil, versus placebo, for scleroderma: results of a three-year, parallel, randomized, double-blind study. Arthritis Rheum. 1989;32:584–593. doi: 10.1002/anr.1780320512. [DOI] [PubMed] [Google Scholar]
- 49.Lynch JP, III, Saggar R, Weigt SS, Zisman DA, White ES. Usual interstitial pneumonia. Semin Respir Crit Care Med. 2006;27:634–651. doi: 10.1055/s-2006-957335. [DOI] [PubMed] [Google Scholar]
- 50.Hoyles RK, Ellis RW, Wellsbury J, Lees B, Newlands P, Goh NS, Roberts C, Desai S, Herrick AL, McHugh NJ, et al. A multicenter, prospective, randomized, double-blind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis Rheum. 2006;54:3962–3970. doi: 10.1002/art.22204. [DOI] [PubMed] [Google Scholar]
- 51.Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, Arriola E, Silver R, Strange C, Bolster M, et al. Scleroderma Lung Study Research Group. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354:2655–2666. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 52.Silver RM, Warrick JH, Kinsella MB, Staudt LS, Baumann MH, Strange C. Cyclophosphamide and low-dose prednisone therapy in patients with systemic sclerosis (scleroderma) with interstitial lung disease. J Rheumatol. 1993;20:838–844. [PubMed] [Google Scholar]
- 53.White B, Moore WC, Wigley FM, Xiao HQ, Wise RA. Cyclophosphamide is associated with pulmonary function and survival benefit in patients with scleroderma and alveolitis. Ann Intern Med. 2000;132:947–954. doi: 10.7326/0003-4819-132-12-200006200-00004. [DOI] [PubMed] [Google Scholar]
- 54.Goldin J, Elashoff R, Kim HJ, Yan X, Lynch D, Strollo D, Roth MD, Clements P, Furst DE, Khanna D, et al. Treatment of scleroderma-interstitial lung disease with cyclophosphamide is associated with less progressive fibrosis on serial thoracic high-resolution CT scan than placebo: findings from the Scleroderma Lung Study. Chest. 2009;136:1333–1340. doi: 10.1378/chest.09-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim HJ, Brown MS, Elashoff R, Li G, Gjertson DW, Lynch DA, Strollo DC, Kleerup E, Chong D, Shah SK, et al. Quantitative texture-based assessment of one-year changes in fibrotic reticular patterns on HRCT in scleroderma lung disease treated with oral cyclophosphamide. Eur Radiol. 2011;21:2455–2465. doi: 10.1007/s00330-011-2223-2. [DOI] [PubMed] [Google Scholar]
- 56.Tashkin DP, Elashoff R, Clements PJ, Roth MD, Furst DE, Silver RM, Goldin J, Arriola E, Strange C, Bolster MB, et al. Scleroderma Lung Study Research Group. Effects of 1-year treatment with cyclophosphamide on outcomes at 2 years in scleroderma lung disease. Am J Respir Crit Care Med. 2007;176:1026–1034. doi: 10.1164/rccm.200702-326OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nihtyanova SI, Brough GM, Black CM, Denton CP. Mycophenolate mofetil in diffuse cutaneous systemic sclerosis: a retrospective analysis. Rheumatology (Oxford) 2007;46:442–445. doi: 10.1093/rheumatology/kel244. [DOI] [PubMed] [Google Scholar]
- 58.Derk CT, Grace E, Shenin M, Naik M, Schulz S, Xiong W. A prospective open-label study of mycophenolate mofetil for the treatment of diffuse systemic sclerosis. Rheumatology (Oxford) 2009;48:1595–1599. doi: 10.1093/rheumatology/kep295. [DOI] [PubMed] [Google Scholar]
- 59.Gerbino AJ, Goss CH, Molitor JA. Effect of mycophenolate mofetil on pulmonary function in scleroderma-associated interstitial lung disease. Chest. 2008;133:455–460. doi: 10.1378/chest.06-2861. [DOI] [PubMed] [Google Scholar]
- 60.Simeón-Aznar CP, Fonollosa-Plá V, Tolosa-Vilella C, Selva-O’Callaghan A, Solans-Laqué R, Vilardell-Tarrés M. Effect of mycophenolate sodium in scleroderma-related interstitial lung disease. Clin Rheumatol. 2011;30:1393–1398. doi: 10.1007/s10067-011-1823-1. [DOI] [PubMed] [Google Scholar]
- 61.Swigris JJ, Olson AL, Fischer A, Lynch DA, Cosgrove GP, Frankel SK, Meehan RT, Brown KK. Mycophenolate mofetil is safe, well tolerated, and preserves lung function in patients with connective tissue disease–related interstitial lung disease. Chest. 2006;130:30–36. doi: 10.1378/chest.130.1.30. [DOI] [PubMed] [Google Scholar]
- 62.Zamora AC, Wolters PJ, Collard HR, Connolly MK, Elicker BM, Webb WR, King TE, Jr, Golden JA. Use of mycophenolate mofetil to treat scleroderma-associated interstitial lung disease. Respir Med. 2008;102:150–155. doi: 10.1016/j.rmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 63.Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, Goldin J, Arriola E, Volkmann ER, Kafaja S, et al. Scleroderma Lung Study II Investigators. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease: Scleroderma Lung Study II (SLS-II), a double-blind, parallel group, randomised controlled trial. Lancet Respir Med 20164708–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saketkoo LA, Lammi MR, Fischer A, Molitor J, Steen VD.PHAROS Investigators. Mycophenolate mofetil (MMF) use in scleroderma patients with pulmonary hypertension: FVC, outcomes, and survival: observations from the Pulmonary Hypertension Recognition and Outcomes in Scleroderma (Pharos) cohort [abstract] Ann Rheum Dis 201574Suppl 2):820 [Google Scholar]
- 65.Zheng Y, Li M, Zhang Y, Shi X, Li L, Jin M. The effects and mechanisms of mycophenolate mofetil on pulmonary arterial hypertension in rats. Rheumatol Int. 2010;30:341–348. doi: 10.1007/s00296-009-0966-8. [DOI] [PubMed] [Google Scholar]
- 66.Bosello S, De Luca G, Tolusso B, Lama G, Angelucci C, Sica G, Ferraccioli G. B cells in systemic sclerosis: a possible target for therapy. Autoimmun Rev. 2011;10:624–630. doi: 10.1016/j.autrev.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 67.Lafyatis R, O’Hara C, Feghali-Bostwick CA, Matteson E. B cell infiltration in systemic sclerosis–associated interstitial lung disease. Arthritis Rheum. 2007;56:3167–3168. doi: 10.1002/art.22847. [DOI] [PubMed] [Google Scholar]
- 68.De Santis M, Bosello SL, Peluso G, Pinnelli M, Alivernini S, Zizzo G, Bocci M, Capacci A, La Torre G, Mannocci A, et al. Bronchoalveolar lavage fluid and progression of scleroderma interstitial lung disease. Clin Respir J. 2012;6:9–17. doi: 10.1111/j.1752-699X.2010.00228.x. [DOI] [PubMed] [Google Scholar]
- 69.Daoussis D, Liossis SN, Tsamandas AC, Kalogeropoulou C, Paliogianni F, Sirinian C, Yiannopoulos G, Andonopoulos AP. Effect of long-term treatment with rituximab on pulmonary function and skin fibrosis in patients with diffuse systemic sclerosis. Clin Exp Rheumatol. 2012;30(2) Suppl 71:S17–S22. [PubMed] [Google Scholar]
- 70.Bosello SL, De Luca G, Rucco M, Berardi G, Falcione M, Danza FM, Pirronti T, Ferraccioli G. Long-term efficacy of B cell depletion therapy on lung and skin involvement in diffuse systemic sclerosis. Semin Arthritis Rheum. 2015;44:428–436. doi: 10.1016/j.semarthrit.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 71.McGonagle D, Tan AL, Madden J, Rawstron AC, Rehman A, Emery P, Thomas S. Successful treatment of resistant scleroderma-associated interstitial lung disease with rituximab. Rheumatology (Oxford) 2008;47:552–553. doi: 10.1093/rheumatology/kem357. [DOI] [PubMed] [Google Scholar]
- 72.Daoussis D, Liossis SN, Tsamandas AC, Kalogeropoulou C, Kazantzi A, Sirinian C, Karampetsou M, Yiannopoulos G, Andonopoulos AP. Experience with rituximab in scleroderma: results from a 1-year, proof-of-principle study. Rheumatology (Oxford) 2010;49:271–280. doi: 10.1093/rheumatology/kep093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Leask A. Possible strategies for anti-fibrotic drug intervention in scleroderma. J Cell Commun Signal. 2011;5:125–129. doi: 10.1007/s12079-011-0122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reichenberger F, Schauer J, Kellner K, Sack U, Stiehl P, Winkler J. Different expression of endothelin in the bronchoalveolar lavage in patients with pulmonary diseases. Lung. 2001;179:163–174. doi: 10.1007/s004080000058. [DOI] [PubMed] [Google Scholar]
- 75.Valerio CJ, Handler CE, Kabunga P, Smith CJ, Denton CP, Coghlan JG. Clinical experience with bosentan and sitaxentan in connective tissue disease–associated pulmonary arterial hypertension. Rheumatology (Oxford) 2010;49:2147–2153. doi: 10.1093/rheumatology/keq241. [DOI] [PubMed] [Google Scholar]
- 76.Furuya Y, Kuwana M. Effect of bosentan on systemic sclerosis–associated interstitial lung disease ineligible for cyclophosphamide therapy: a prospective open-label study. J Rheumatol. 2011;38:2186–2192. doi: 10.3899/jrheum.110499. [DOI] [PubMed] [Google Scholar]
- 77.Seibold JR, Denton CP, Furst DE, Guillevin L, Rubin LJ, Wells A, Matucci Cerinic M, Riemekasten G, Emery P, Chadha-Boreham H, et al. Randomized, prospective, placebo-controlled trial of bosentan in interstitial lung disease secondary to systemic sclerosis. Arthritis Rheum. 2010;62:2101–2108. doi: 10.1002/art.27466. [DOI] [PubMed] [Google Scholar]
- 78.Muangchant C, Pope JE. The significance of interleukin-6 and C-reactive protein in systemic sclerosis: a systematic literature review. Clin Exp Rheumatol. 2013;31(2) Suppl 76:122–134. [PubMed] [Google Scholar]
- 79.Khan K, Xu S, Nihtyanova S, Derrett-Smith E, Abraham D, Denton CP, Ong VH. Clinical and pathological significance of interleukin 6 overexpression in systemic sclerosis. Ann Rheum Dis. 2012;71:1235–1242. doi: 10.1136/annrheumdis-2011-200955. [DOI] [PubMed] [Google Scholar]
- 80.Khanna D, Denton CP, Jahreis A, van Laar JM, Cheng S, Spotswood H, Pope JE, Allanore Y, Muller-Ladner U, Siegel J, et al. Safety and efficacy of subcutaneous tocilizumab in adults with systemic sclerosis: week 48 data from the faSScinate trial [abstract presented at meeting of the European League against Rheumatism (EULAR), Rome, Italy, June 10–13, 2015] Ann Rheum Dis. 2015;74(Suppl 2):87–88. [Google Scholar]
- 81.Daniels CE, Wilkes MC, Edens M, Kottom TJ, Murphy SJ, Limper AH, Leof EB. Imatinib mesylate inhibits the profibrogenic activity of TGF-β and prevents bleomycin-mediated lung fibrosis. J Clin Invest. 2004;114:1308–1316. doi: 10.1172/JCI19603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Khanna D, Saggar R, Mayes MD, Abtin F, Clements PJ, Maranian P, Assassi S, Saggar R, Singh RR, Furst DE. A one-year, phase I/IIa, open-label pilot trial of imatinib mesylate in the treatment of systemic sclerosis–associated active interstitial lung disease. Arthritis Rheum. 2011;63:3540–3546. doi: 10.1002/art.30548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gordon J, Udeh U, Doobay K, Magro C, Wildman H, Davids M, Mersten JN, Huang WT, Lyman S, Crow MK, et al. Imatinib mesylate (Gleevec™) in the treatment of diffuse cutaneous systemic sclerosis: results of a 24-month open label, extension phase, single-centre trial. Clin Exp Rheumatol. 2014;32(6) Suppl 86:S-189–S-193. [PubMed] [Google Scholar]
- 84.Spiera RF, Gordon JK, Mersten JN, Magro CM, Mehta M, Wildman HF, Kloiber S, Kirou KA, Lyman S, Crow MK. Imatinib mesylate (Gleevec) in the treatment of diffuse cutaneous systemic sclerosis: results of a 1-year, phase IIa, single-arm, open-label clinical trial. Ann Rheum Dis. 2011;70:1003–1009. doi: 10.1136/ard.2010.143974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Prey S, Ezzedine K, Doussau A, Grandoulier AS, Barcat D, Chatelus E, Diot E, Durant C, Hachulla E, de Korwin-Krokowski JD, et al. Imatinib mesylate in scleroderma-associated diffuse skin fibrosis: a phase II multicentre randomized double-blinded controlled trial. Br J Dermatol. 2012;167:1138–1144. doi: 10.1111/j.1365-2133.2012.11186.x. [DOI] [PubMed] [Google Scholar]
- 86.Distler O, Distler JHW, Varga J, Denton CP, Lafyatis RA, Wigley FM, Schett GA. Multi-center, open-label, proof of concept study of imatinib mesylate demonstrates no benefit for the treatment of fibrosis in patients with early, diffuse systemic sclerosis [abstract] Arthritis Rheum. 2010;62(Suppl 10):560. [Google Scholar]
- 87.Fraticelli P, Gabrielli B, Pomponio G, Valentini G, Bosello S, Riboldi P, Gerosa M, Faggioli P, Giacomelli R, Del Papa N, et al. Imatinib in Scleroderma Italian Study Group. Low-dose oral imatinib in the treatment of systemic sclerosis interstitial lung disease unresponsive to cyclophosphamide: a phase II pilot study. Arthritis Res Ther. 2014;16:R144. doi: 10.1186/ar4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hilberg F, Roth GJ, Krssak M, Kautschitsch S, Sommergruber W, Tontsch-Grunt U, Garin-Chesa P, Bader G, Zoephel A, Quant J, et al. BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008;68:4774–4782. doi: 10.1158/0008-5472.CAN-07-6307. [DOI] [PubMed] [Google Scholar]
- 89.McCormack PL. Nintedanib: first global approval. Drugs. 2015;75:129–139. doi: 10.1007/s40265-014-0335-0. [DOI] [PubMed] [Google Scholar]
- 90.Huang J, Beyer C, Palumbo-Zerr K, Zhang Y, Ramming A, Distler A, Gelse K, Distler O, Schett G, Wollin L, et al. Nintedanib inhibits fibroblast activation and ameliorates fibrosis in preclinical models of systemic sclerosis. Ann Rheum Dis. 2016;75:883–890. doi: 10.1136/annrheumdis-2014-207109. [DOI] [PubMed] [Google Scholar]
- 91.Noble PW, Albera C, Bradford WZ, Costabel U, Glassberg MK, Kardatzke D, King TE, Jr, Lancaster L, Sahn SA, Szwarcberg J, et al. CAPACITY Study Group. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377:1760–1769. doi: 10.1016/S0140-6736(11)60405-4. [DOI] [PubMed] [Google Scholar]
- 92.Oku H, Shimizu T, Kawabata T, Nagira M, Hikita I, Ueyama A, Matsushima S, Torii M, Arimura A. Antifibrotic action of pirfenidone and prednisolone: different effects on pulmonary cytokines and growth factors in bleomycin-induced murine pulmonary fibrosis. Eur J Pharmacol. 2008;590:400–408. doi: 10.1016/j.ejphar.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 93.Gurujeyalakshmi G, Hollinger MA, Giri SN. Pirfenidone inhibits PDGF isoforms in bleomycin hamster model of lung fibrosis at the translational level. Am J Physiol. 1999;276:L311–L318. doi: 10.1152/ajplung.1999.276.2.L311. [DOI] [PubMed] [Google Scholar]
- 94.Yuko O, Kawaguchi Y, Takagi K, Ichida H, Katsumata Y, Gono T, Okamoto Y. Pirfenidone and BIBF1120 suppress collagen synthesis in skin fibroblast from patients with systemic sclerosis [abstract] Arthritis Rheum. 2013;65:652. [Google Scholar]
- 95.Miura Y, Saito T, Fujita K, Tsunoda Y, Tanaka T, Takoi H, Yatagai Y, Rin S, Sekine A, Hayashihara K, et al. Clinical experience with pirfenidone in five patients with scleroderma-related interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis. 2014;31:235–238. [PubMed] [Google Scholar]
- 96.Khanna D, Albera C, Fischer A, Seibold JR, Raghu G, Khalidi N, Chung L, Schipou E, Chen D, Gorina E. Safety and tolerability of pirfenidone in patients with systemic sclerosis–associated interstitial lung disease: the LOTUSS study [abstract] Ann Rheum Dis. 2015;74:816. [Google Scholar]
- 97.van Laar JM, Naraghi K, Tyndall A. Haematopoietic stem cell transplantation for poor-prognosis systemic sclerosis. Rheumatology (Oxford) 2015;54:2126–2133. doi: 10.1093/rheumatology/kev117. [DOI] [PubMed] [Google Scholar]
- 98.van Laar JM, Sullivan K. Stem cell transplantation in systemic sclerosis. Curr Opin Rheumatol. 2013;25:719–725. doi: 10.1097/01.bor.0000434669.32150.ac. [DOI] [PubMed] [Google Scholar]
- 99.van Laar JM, Farge D, Sont JK, Naraghi K, Marjanovic Z, Larghero J, Schuerwegh AJ, Marijt EW, Vonk MC, Schattenberg AV, et al. EBMT/EULAR Scleroderma Study Group. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: a randomized clinical trial. JAMA. 2014;311:2490–2498. doi: 10.1001/jama.2014.6368. [DOI] [PubMed] [Google Scholar]
- 100.Bernstein EJ, Peterson ER, Sell JL, D’Ovidio F, Arcasoy SM, Bathon JM, Lederer DJ. Survival of adults with systemic sclerosis following lung transplantation: a nationwide cohort study. Arthritis Rheumatol. 2015;67:1314–1322. doi: 10.1002/art.39021. [DOI] [PubMed] [Google Scholar]
- 101.Khan IY, Singer LG, de Perrot M, Granton JT, Keshavjee S, Chau C, Kron A, Johnson SR. Survival after lung transplantation in systemic sclerosis: a systematic review. Respir Med. 2013;107:2081–2087. doi: 10.1016/j.rmed.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 102.Sottile PD, Iturbe D, Katsumoto TR, Connolly MK, Collard HR, Leard LA, Hays S, Golden JA, Hoopes C, Kukreja J, et al. Outcomes in systemic sclerosis–related lung disease after lung transplantation. Transplantation. 2013;95:975–980. doi: 10.1097/TP.0b013e3182845f23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Crespo MM, Bermudez CA, Dew MA, Johnson BA, George MP, Bhama J, Morrell M, D’Cunha J, Shigemura N, Richards TJ, et al. Lung transplantation in patients with scleroderma compared with pulmonary fibrosis: short and long-term outcomes in a single institution. Ann Am Thorac Soc. 2016;13:784–792. doi: 10.1513/AnnalsATS.201503-177OC. [DOI] [PubMed] [Google Scholar]
- 104.Miele CH, Schwab K, Saggar R, Duffy E, Elashoff D, Tseng CH, Weigt S, Charan D, Abtin F, Johannes J, et al. Lung transplant outcomes in systemic sclerosis with significant esophageal dysfunction: a comprehensive single center experience. Ann Am Thorac Soc. 2016;13:793–802. doi: 10.1513/AnnalsATS.201512-806OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Saketkoo LA, Mittoo S, Frankel S, LeSage D, Sarver C, Phillips K, Strand V, Matteson EL OMERACT Connective Tissue Disease–Interstitial Lung Diseases Working Group. Reconciling healthcare professional and patient perspectives in the development of disease activity and response criteria in connective tissue disease–related interstitial lung disease. J Rheumatol. 2014;41:792–798. doi: 10.3899/jrheum.131251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 107.Volkmann ER, Tashkin DP, Li N, Furst DE, Clements PJ, Elashoff RM. Development of a composite outcome measure for systemic sclerosis related interstitial lung disease. Rheumatology (Sunnyvale) 2015;5:154. doi: 10.4172/2161-1149.1000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wells AU. Interstitial lung disease in systemic sclerosis. Presse Med. 2014;43:e329–e343. doi: 10.1016/j.lpm.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 109.Khanna D, Brown KK, Clements PJ, Elashoff R, Furst DE, Goldin J, Seibold JR, Silver RM, Tashkin DP, Wells AU. Systemic sclerosis–associated interstitial lung disease: proposed recommendations for future randomized clinical trials [review] Clin Exp Rheumatol. 2010;28(2) Suppl 58:S55–S62. [PubMed] [Google Scholar]
- 110.Steen VD, Lanz JK, Jr, Conte C, Owens GR, Medsger TA., Jr Therapy for severe interstitial lung disease in systemic sclerosis: a retrospective study. Arthritis Rheum. 1994;37:1290–1296. doi: 10.1002/art.1780370904. [DOI] [PubMed] [Google Scholar]
- 111.Roth MD, Tseng CH, Clements PJ, Furst DE, Tashkin DP, Goldin JG, Khanna D, Kleerup EC, Li N, Elashoff D, et al. Scleroderma Lung Study Research Group. Predicting treatment outcomes and responder subsets in scleroderma-related interstitial lung disease. Arthritis Rheum. 2011;63:2797–2808. doi: 10.1002/art.30438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cappelli S, Guiducci S, Bellando Randone S, Matucci Cerinic M. Immunosuppression for interstitial lung disease in systemic sclerosis. Eur Respir Rev. 2013;22:236–243. doi: 10.1183/09059180.00001813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bérezné A, Ranque B, Valeyre D, Brauner M, Allanore Y, Launay D, Le Guern V, Kahn JE, Couderc LJ, Constans J, et al. Therapeutic strategy combining intravenous cyclophosphamide followed by oral azathioprine to treat worsening interstitial lung disease associated with systemic sclerosis: a retrospective multicenter open-label study. J Rheumatol. 2008;35:1064–1072. [PubMed] [Google Scholar]
- 114.Iudici M, Cuomo G, Vettori S, Bocchino M, Sanduzzi Zamparelli A, Cappabianca S, Valentini G. Low-dose pulse cyclophosphamide in interstitial lung disease associated with systemic sclerosis (SSc-ILD): efficacy of maintenance immunosuppression in responders and non-responders. Semin Arthritis Rheum. 2015;44:437–444. doi: 10.1016/j.semarthrit.2014.09.003. [DOI] [PubMed] [Google Scholar]