Abstract
Rationale: Radiologist reports of pulmonary nodules discovered incidentally on computed tomographic (CT) images of the chest may influence subsequent evaluation and management.
Objectives: We sought to determine the impact of the terminology used by radiologists to report incidental pulmonary nodules on subsequent documentation and evaluation of the nodules by the ordering or primary care provider.
Methods: We conducted a retrospective cohort study of patients with incidentally discovered pulmonary nodules detected on CT chest examinations performed during 2010 in a large urban safety net medical system located in northeastern Ohio.
Measurements and Main Results: Twelve different terms were used to describe 344 incidental pulmonary nodules. Most nodules (181 [53%]) were documented in a subsequent progress note by the provider, and 140 (41%) triggered subsequent clinical activity. In a multivariable analysis, incidental pulmonary nodules described in radiology reports using the terms density (odds ratio [OR], 0.06; 95% confidence interval [CI], 0.01–0.47), granuloma (OR, 0.07; 95% CI, 0.01–0.65), or opacity (OR, 0.09; 95% CI, 0.01–0.68) were less likely to be documented by the provider than those that used the term mass. Patients with nodules described in radiology reports using the term nodule (OR, 0.15; 95% CI, 0.02–0.99), nodular density (OR, 0.09; 95% CI, 0.01–0.63), granuloma (OR, 0.06; 95% CI, 0.01–0.69), or opacity (OR, 0.05; 95% CI, 0.01–0.43) were less likely to receive follow-up than were patients with nodules described using the term mass. The factor most strongly associated with follow-up of pulmonary nodules was documentation by the provider (OR, 5.85; 95% CI, 2.93–11.7).
Conclusions: Within one multifacility urban health system in the United States, the terms used by radiologists to describe incidental pulmonary nodules were associated with documentation of the nodule by the ordering physician and subsequent follow-up. Standard terminology should be used to describe pulmonary nodules to improve patient outcomes.
Keywords: solitary pulmonary nodule, multiple pulmonary nodules, CT scan, clinical decision making
Computed tomographic (CT) scanners are widely available, and their use continues to increase (1). Recently, it was reported that 23 chest CT scans are performed for every 1,000 patients, which approximates to 7 million scans being performed annually (2). This surge in imaging has led to an increase in the identification of incidental findings, particularly those of incidental pulmonary nodules. It is estimated that each year over 1.2 million Americans are diagnosed with a new pulmonary nodule (3).
While guidelines regarding the management of pulmonary nodules have been released (4–6), uptake among patients, providers, and health care systems continues to evolve (7–9). As a result, there is substantial variation in pulmonary nodule evaluation. Radiologists may play an important role in the evaluation of incidental pulmonary nodules, as their interpretation of chest CT images may guide subsequent follow-up. For example, Blagev and colleagues found that incidental pulmonary nodules identified on pulmonary angiograms ordered in the emergency department infrequently underwent further evaluation (29%), particularly when the incidental pulmonary nodules were mentioned only in the findings section of the radiologic report (0%) (10). It remains unclear if similar findings occur with reports of CT scans and, if so, what other aspects of the radiologic report are associated with recognition and evaluation of the nodule by the ordering physician.
We sought to identify factors in the radiology report that were associated with documentation and follow-up of incidental pulmonary nodules by the ordering or primary care provider. We also wanted to determine whether certain words used by radiologists to describe incidental pulmonary nodules were associated with provider documentation and follow-up.
Methods
Subjects
This retrospective cohort study was conducted at an urban safety net medical system in northeastern Ohio that includes a large tertiary care hospital, a level I trauma center, and over a dozen ambulatory centers in poor and wealthy communities. We manually reviewed the radiology reports of all nonhospitalized patients undergoing incident CT scans incorporating all lung fields that were performed in 2010. Patients who underwent CT scans for surveillance of previously diagnosed cancer were excluded. CT scan slices were 3 mm thick with soft tissue reconstructions. High-resolution CT scan protocols included contiguous imaging. The study was approved by the institutional review board of The MetroHealth System, Cleveland, Ohio (protocol number 14-00396).
Study Variables
Patients whose radiology reports described new incidental pulmonary nodules were included in the study. Incidental pulmonary nodules were defined as discrete lesions up to 3 cm in diameter that were completely surrounded by lung and without associated atelectasis or adenopathy (11, 12). The term used to describe the nodule was recorded on standardized abstraction forms, as were the nodule characteristics, total number of nodules, sections of the report where the nodule was described, ordering provider, primary care provider, whether the radiologist mentioned communicating the findings to the ordering or primary care provider, the type of CT scan performed, and the interpreting radiologist. The radiology report was also reviewed for the type of follow-up recommended by the radiologist, including mention of the Fleischner Society Guidelines for management of pulmonary nodules (4). The Department of Radiology provided information regarding which radiologists had completed a fellowship in chest and body imaging.
Patient demographic information was downloaded from the electronic health records. Downloaded data included patient age, sex, race, ethnicity, language preference, smoking status, primary care provider, and insurance status. Patient mortality was determined by electronic health record review and by query of the Ohio Death Certificate Registry 24 months following the incident CT scan.
Outcomes
The primary outcome was progress note documentation of the incidental pulmonary nodule by the patient’s primary care provider or the provider who ordered the incident CT scan over the subsequent 2 years. The secondary outcome was subsequent evaluation of the nodule by subspecialist consultation (oncology, pulmonary, or thoracic surgery), imaging (CT or PET), or biopsy over 2 years. Health information for patients who received subsequent care at another facility was not obtained.
Data Abstractor Training
Prior to study initiation, a comprehensive chart review methodology was constructed. Standardized abstraction forms were created and pilot tested on CT scan reports of 100 patients not included in the study. Six physician reviewers (M.N.I., C.J.S., J.D., K.K., C.C., and N.T.) reviewed the study methodology and collectively reviewed patient charts until an agreement of greater than 90% was achieved on abstracted data. Upon initiation of the study, all charts were reviewed by at least two reviewers. Any discrepancies were adjudicated by a third reviewer. Data abstraction forms were entered into the study database in duplicate. Discrepancies were adjudicated by a third investigator.
Statistical Analysis
We employed descriptive statistics (percentages, means, and SDs) to describe the characteristics of the patients and the radiology reports. Because nodule size was not normally distributed, median and interquartile range were reported. The chi-square test and Student’s t test were used to determine the univariate relationship between nodule documentation in provider progress notes and patient and radiology report characteristics. The Mann-Whitney U test was used to evaluate the relationship between nodule size and nodule documentation.
Logistic regression was used to determine the multivariable relationship between nodule documentation by providers (dependent variable) and patient and radiology report characteristics. Variables that were included in the model a priori were age, sex, race, ethnicity, language, insurance status, smoking status, type of CT scan, tertiles of nodule size, term used to describe the nodule, number of nodules, radiologist specialty, where the nodule was mentioned in the radiology report, whether the radiology report mentioned the need for follow-up, whether the radiology report mentioned communicating the findings to the ordering physician, and the number of visits with the primary care provider over the next 2 years. A similar approach was used to determine the multivariable relationship between subsequent evaluation of pulmonary nodules and patient and radiology report characteristics. Documentation of the nodule in provider progress notes was also added to this model.
In both models, tertiles of nodule size were used to reflect the skewed distribution of the variable. P values less than 0.05 or 95% confidence intervals (CIs) that excluded 1.00 were considered statistically significant. All statistical analyses were performed using Stata statistical software (release 14; StataCorp, College Station, TX).
Results
Patient Characteristics
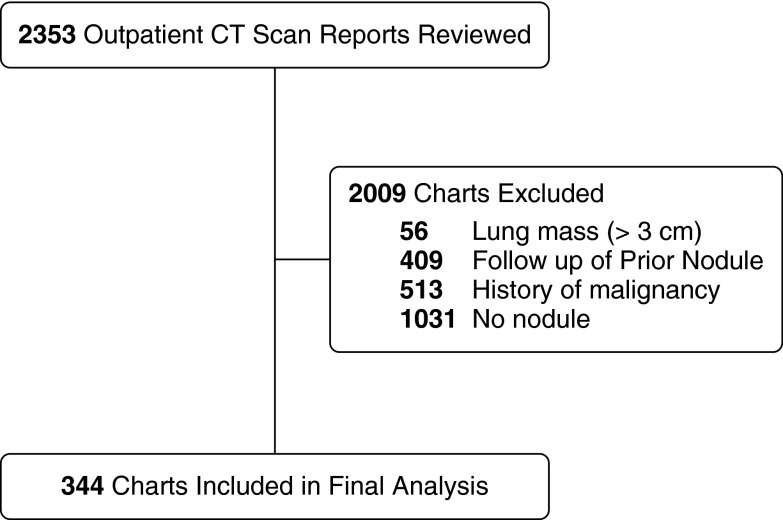
In 2010, 2,353 patients underwent CT scans in the ambulatory setting that incorporated all portions of the lungs (Figure 1). Of the 2,353 patients, 344 (15%) were diagnosed with new incidental pulmonary nodules in the reports of 20 radiologists. The demographic characteristics of the 344 patients with new incidental pulmonary nodules are listed in Table 1. Over half (182 [53%]) of the patients with nodules were women. The patients’ average age was 53.5 ± 16.4 years. Patients with nodules were mostly non-Hispanic black (97 [28%]) or from another racial or ethnic group (112 [33%]). Smoking status was not available for 121 (35%) patients. Of the 223 patients with a documented smoking status, 76 (22%) were current smokers, and 81 (24%) were former smokers. CT scans of the chest with contrast (128 [37%]) were most commonly performed, followed by CT angiograms to detect pulmonary emboli (76 [22%]).
Figure 1.
Study flow diagram. CT = computed tomographic.
Table 1.
Comparison of nodule documentation and follow-up among study patients
| Characteristics | Documentation of Nodule |
Follow-Up of Nodule |
|||||
|---|---|---|---|---|---|---|---|
| All Patients (n = 344) | Documentation (n = 181) | No Documentation (n = 163) | P Value* | Follow-Up (n = 140) | No Follow-Up (n = 204) | P Value† | |
| Sex | |||||||
| Female | 182 (53) | 101 (56) | 81 (50) | 0.26 | 79 (56) | 103 (50) | 0.28 |
| Male | 162 (47) | 80 (44) | 82 (50) | 61 (44) | 101 (50) | ||
| Age, yr, mean ± SD | 53.5 ± 16.4 | 58.0 ± 14.7 | 48.4 ± 16.7 | <0.001 | 57.8 ± 12.9 | 50.5 ± 17.8 | <0.001 |
| Race and/or ethnicity | |||||||
| White, not Hispanic | 135 (39) | 80 (44) | 55 (34) | <0.001 | 63 (45) | 72 (35) | <0.001 |
| Black, not Hispanic | 97 (28) | 61 (34) | 36 (22) | 53 (38) | 44 (22) | ||
| Other or not reported | 112 (33) | 40 (22) | 72 (44) | 24 (17) | 88 (43) | ||
| Preferred language | |||||||
| English | 277 (81) | 158 (87) | 119 (73) | 0.001 | 125 (89) | 152 (75) | 0.001 |
| Other | 67 (19) | 23 (13) | 44 (27) | 15 (11) | 52 (25) | ||
| Insurance | |||||||
| Uninsured | 72 (21) | 38 (21) | 34 (21) | 0.04 | 38 (27) | 34 (17) | 0.03 |
| Medicaid/Medicare | 167 (49) | 98 (54) | 69 (42) | 67 (48) | 100 (49) | ||
| Private | 105 (30) | 45 (25) | 60 (37) | 35 (25) | 70 (34) | ||
| Smoking | |||||||
| Never | 66 (19) | 33 (18) | 33 (20) | <0.001 | 22 (16) | 44 (21) | 0.005 |
| Former | 81 (24) | 57 (32) | 24 (15) | 45 (32) | 36 (18) | ||
| Current | 76 (22) | 45 (25) | 31 (19) | 34 (24) | 42 (21) | ||
| Not assessed | 121 (35) | 46 (25) | 75 (46) | 39 (28) | 82 (40) | ||
| CT type | |||||||
| CT of chest with contrast | 128 (37) | 83 (46) | 45 (28) | <0.001 | 70 (50) | 58 (28) | <0.001 |
| CT angiogram (PE protocol) | 76 (22) | 32 (17) | 44 (27) | 21 (15) | 55 (27) | ||
| CT of chest without contrast | 71 (20) | 45 (25) | 26 (16) | 36 (26) | 35 (17) | ||
| CT of chest, abdomen, and pelvis with contrast | 47 (14) | 14 (8) | 33 (20) | 3 (2) | 44 (22) | ||
| CT of chest, abdomen, and pelvis without contrast | 6 (2) | 1 (0.5) | 5 (3) | 2 (1) | 4 (2) | ||
| High-resolution chest CT | 10 (3) | 5 (3) | 5 (3) | 7 (5) | 3 (1.5) | ||
| Other | 6 (2) | 1 (0.5) | 5 (3) | 1 (1) | 5 (2.5) | ||
| Nodule size was reported | 222 (65) | 136 (75) | 86 (53) | <0.001 | 102 (73) | 120 (59) | 0.008 |
| Nodule size, mm, median (IQR) | 6.0 (4.0–9.9) | 7.0 (4.2–11) | 5.0 (3–8) | <0.001 | 7.65 (5–12) | 5 (3–8) | <0.001 |
| Nodule number | |||||||
| Single | 168 (49) | 79 (44) | 89 (55) | 0.04 | 68 (49) | 100 (49) | 0.9 |
| Multiple | 176 (51) | 102 (56) | 74 (45) | 72 (51) | 104 (51) | ||
| Radiologist’s description of nodule | |||||||
| Mass | 14 (4) | 11 (6) | 3 (2) | 0.002 | 11 (8) | 3 (2) | 0.002 |
| Nodule | 180 (52) | 106 (59) | 74 (46) | 0.002 | 81 (58) | 99 (48) | |
| Ground glass | 15 (4) | 8 (4) | 7 (4) | 6 (4) | 9 (4) | ||
| Density | 18 (5) | 6 (3) | 12 (7) | 9 (6) | 9 (4) | ||
| Nodular density | 49 (14) | 26 (14) | 23 (14) | 17 (12) | 32 (16) | ||
| Granuloma | 20 (6) | 3 (2) | 17 (11) | 3 (2) | 17 (8) | ||
| Opacity | 24 (7) | 9 (5) | 15 (9) | 4 (3) | 20 (10) | ||
| Other | 24 (7) | 12 (7) | 12 (7) | 9 (6) | 15 (7) | ||
| Radiologist’s specialty | |||||||
| Not chest and body | 151 (44) | 79 (44) | 72 (44) | 0.92 | 57 (41) | 94 (46) | 0.32 |
| Chest and body | 193 (56) | 102 (56) | 91 (56) | 83 (59) | 110 (54) | ||
| Report location where nodule was mentioned | |||||||
| Findings and impression | 291 (85) | 174 (96) | 117 (72) | <0.001 | 132 (94) | 159 (78) | < 0.001 |
| Findings only | 50 (14) | 7 (4) | 43 (26) | 8 (6) | 42 (21) | ||
| Impression only | 3 (1) | 0 | 3 (2) | 0 | 3 (1) | ||
| Radiologist’s report recommended follow-up | 197 (57) | 132 (73) | 65 (40) | <0.001 | 97 (69) | 100 (49) | <0.001 |
| Fleischner statement included | 27 (8) | 16 (9) | 11 (7) | 0.47 | 9 (6) | 18 (9) | 0.42 |
| Radiologist’s report mentioned communication of findings to ordering provider | 20 (6) | 10 (6) | 10 (6) | 0.81 | 8 (6) | 12 (6) | 0.95 |
| Number of PCP visits in subsequent 2 yr, mean ± SD | 1.91 ± 3.68 | 2.75 ± 4.34 | 0.98 ± 2.47 | <0.001 | 2.73 ± 3.99 | 1.35 ± 3.35 | <0.001 |
| Death | 34 (10) | 24 (13) | 10 (6) | 0.03 | 15 (11) | 19 (9.5) | 0.71 |
Definition of abbreviations: CT = computed tomography; IQR = interquartile range; PCP = primary care provider; PE = pulmonary embolism.
Data are presented as number (percent) unless otherwise specified.
P value represents comparison of characteristics between group with documentation and group with no documentation.
P value represents comparison of characteristics between group with follow-up and group with no follow-up.
Nodule Characteristics
The size of the nodule was mentioned in the radiology reports of 224 (65%) patients. Among those nodules with a size reported, the median greatest diameter was 6.0 mm (IQR, 4.0–9.9 mm). The majority of nodules were multiple (176 [51%]).
Radiologists recommended follow-up of 197 (57%) of the incidental pulmonary nodules. The Fleischner Society guidelines were mentioned in 27 (8%) radiology reports, and the recommended time for follow-up was mentioned in 148 (43%) reports. When the Fleischner Society guidelines and time of follow-up were mentioned in the same report, the time of follow-up was not always consistent with the actual Fleischner guidelines. The median number of months recommended for follow-up was 6, with a range from 1 to 12 (IQR, 3–6). A follow-up was recommended without mention of time in 13 (5%) reports. There was no relationship between reported nodule size and mention of the Fleischner Society guidelines (P = 0.67). No follow-up was mentioned in 136 (39%) of the reports, while 14 (4%) reports commented that no additional follow-up was needed.
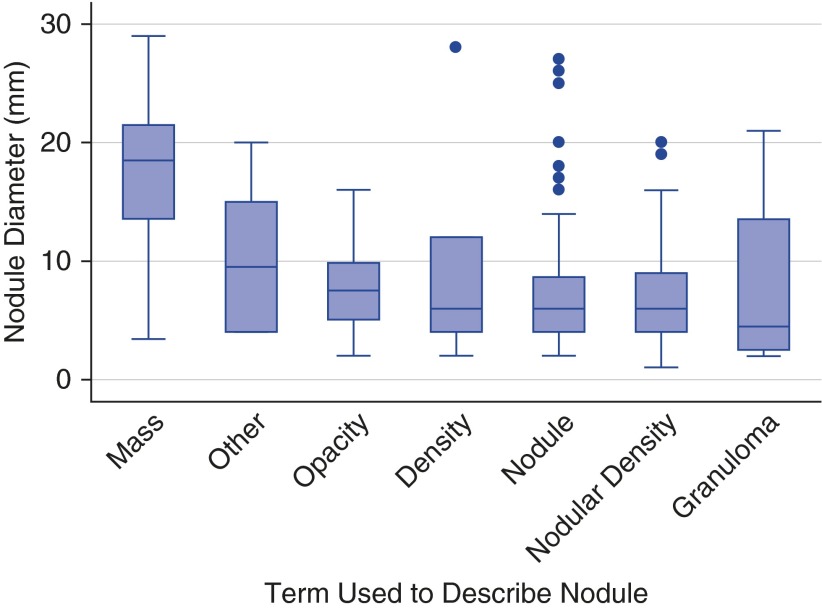
Twelve different terms were used to describe the incidental pulmonary nodules that were identified. The most common term was nodule (180 [52%]), followed by nodular density (49 [14%]) and opacity (24 [7%]). Despite no nodules being larger than 3 cm in diameter, the term mass was used in 14 patients (4%). Additional terms (<1%) used less frequently to describe incidental pulmonary nodules included nodular opacity, irregular nodularity, lesion, nodular scarring, and hypodensity. The association between median greatest nodule size and term used to describe the nodule in the radiology report is depicted in Figure 2.
Figure 2.
Relationship between reported nodule diameter and term used to describe nodule in radiologists’ reports (n = 224). Ground-glass nodules were not included, owing to the small sample in which size was reported.
Nodules were described as calcified (33 [9.5%]), noncalcified (31 [8.9%]), regular (20 [5.8%]), or irregular (14 [4%]). None were described as spiculated or solid, but one was described as nonspiculated (<1%) and another as part solid. Among nodules that were characterized as calcified, terms used to describe them were nodule, nodular density, granuloma, and opacity. Six noncalcified nodules were classified as a granuloma.
Radiologist Characteristics
Of the 20 radiologists who reported the incidental pulmonary nodules, 7 (35%) received additional training in chest and body imaging. The average years in practice following residency was 15.6 ± 8.5 years for chest and body–trained radiologists, compared with 19.2 ± 10.4 years for radiologists who were not trained in chest and body imaging (P < 0.001). Chest and body radiologists identified incidental pulmonary nodules in 193 (56%) patients, while radiologists without chest and body training identified pulmonary nodules in 151 (44%) patients. Similar terms were used to describe the nodules among radiologists in both groups, but the proportion of the terms used differed (P = 0.01). Chest and body radiologists were as likely as non–chest and body radiologists to use the terms nodule (54% vs. 50%; P = 0.38) and granuloma (4% vs. 9%; P = 0.05). However, chest and body radiologists were less likely to use the term mass (1% vs. 8%; P = 0.001).
Patient Outcomes
Among the patients with nodules, 181 (53%) had their nodules documented by their primary care provider or the provider who ordered the CT scan. In a univariate analysis, when the size of the nodule was mentioned in the radiology report, providers were more likely to describe the nodule in their follow-up progress notes (75% vs. 53%; P < 0.001). In a univariate analysis of radiology reports that recorded nodule size, larger-diameter nodules were also more likely to be documented by providers in follow-up (9.5 ± 6.8 mm vs. 6.1 ± 4.1 mm; P < 0.001). However, in a multivariable analysis of nodule, patient, and radiologist characteristics associated with documentation of the nodules by providers in follow-up, neither nodule size nor whether the nodule size was reported was found to be significant (Table 2).
Table 2.
Multivariable logistic regression models identifying factors associated with documentation and follow-up of incidental pulmonary nodules
| Factor | Documentation, OR (95% CI) | Follow-Up, OR (95% CI) |
|---|---|---|
| Sex | ||
| Female | Reference | Reference |
| Male | 1.16 (0.64–2.13) | 0.89 (0.47–1.68) |
| Age, by decade increment | 1.14 (0.93–1.41) | 1.16 (0.92–1.48) |
| Race and/or ethnicity | ||
| White | Reference | Reference |
| Black | 0.98 (0.49–1.94) | 1.54 (0.76–3.11) |
| Other or not reported | 0.41 (0.18–0.94) | 0.22 (0.08–0.59) |
| Preferred language | ||
| English | Reference | Reference |
| Other | 1.06 (0.42–2.66) | 1.48 (0.47–4.66) |
| Insurance | ||
| Uninsured | Reference | Reference |
| Medicaid/Medicare | 1.04 (0.48–2.26) | 0.21 (0.08–0.49) |
| Private | 0.80 (0.36–1.79) | 0.25 (0.10–0.64) |
| Smoking | ||
| Never | Reference | Reference |
| Former | 2.10 (0.87–5.06) | 1.74 (0.69–4.38) |
| Current | 1.12 (0.47–2.65) | 1.33 (0.52–3.38) |
| Not assessed | 0.71 (0.32–1.60) | 1.78 (0.70–4.55) |
| CT type | ||
| CT chest with contrast | Reference | Reference |
| CT angiogram (PE protocol) | 0.56 (0.25–1.28) | 0.38 (0.16–0.94) |
| CT chest without contrast | 0.77 (0.35–1.73) | 0.60 (0.27–1.31) |
| CT chest, abdomen, and pelvis with contrast | 0.4 (0.16–1.01) | 0.06 (0.01–0.25) |
| CT chest, abdomen, and pelvis without contrast | 0.08 (0–1.12) | 0.93 (0.06–13.2) |
| High-resolution chest CT | 0.2 (0.04–0.94) | 1.88 (0.33–10.6) |
| Other | 0.12 (0–2.25) | 0.25 (0.01–3.93) |
| Nodule size | ||
| <4.6 mm | Reference | Reference |
| 4.6–8 mm | 1.15 (0.51–2.63) | 1.79 (0.73–4.38) |
| 8–30 mm | 2.35 (0.95–5.8) | 3.04 (1.19–7.77) |
| Not reported | 1.06 (0.45–2.49) | 1.79 (0.69–4.62) |
| Nodule number | ||
| Single | Reference | Reference |
| Multiple | 1.65 (0.94–2.9) | 0.74 (0.40–1.36) |
| Radiologist’s description of nodule | ||
| Mass | Reference | Reference |
| Nodule | 0.24 (0.04–1.32) | 0.15 (0.02–0.99) |
| Ground glass | 0.2 (0.02–1.7) | 0.15 (0.01–1.67) |
| Density | 0.06 (0.01–0.47) | 0.30 (0.03–2.71) |
| Nodular density | 0.24 (0.04–1.32) | 0.09 (0.01–0.63) |
| Granuloma | 0.07 (0.01–0.65) | 0.06 (0.01–0.69) |
| Opacity | 0.09 (0.01–0.68) | 0.05 (0.01–0.43) |
| Other | 0.16 (0.02–1.06) | 0.21 (0.02–1.80) |
| Radiologist’s specialty | ||
| Not chest and body | Reference | Reference |
| Chest and body | 1.09 (0.61–1.95) | 1.76 (0.94–3.29) |
| Report location where nodule was mentioned | ||
| Findings and impression | Reference | Reference |
| Findings only | 0.30 (0.10–0.85) | 0.74 (0.24–2.27) |
| Impression only | Omitted | Omitted |
| Radiologist’s report recommended follow-up | 2.57 (1.31–5.06) | 1.03 (0.49–2.20) |
| Radiologist’s report mentioned communication of findings to ordering provider | 0.61 (0.18–2.08) | 0.52 (0.13–2.06) |
| Number of PCP visits in subsequent 2 yr | 1.11 (1.01–1.21) | 1.04 (0.96–1.12) |
| PCP-documented nodule | — | 5.85 (2.93–11.7) |
Definition of abbreviations: CI = confidence interval; CT = computed tomography; OR = odds ratio; PCP = primary care provider; PE = pulmonary embolism.
Patients met with their primary care providers 1.91 ± 3.68 times following identification of the pulmonary nodule over the subsequent 2 years. In the univariate analysis, patients who had their nodules documented met more frequently with their providers (2.73 ± 4.33 times vs. 1 ± 2.47 times; P < 0.001). This association was also found in the multivariable analysis (OR, 1.11; 95% CI, 1.01–1.21).
Additional factors that were independently associated with documentation of the incidental pulmonary nodule by the ordering or primary care provider are listed in Table 2. Minorities who were not black were less likely than white individuals to have a nodule documented independent of their language preference (OR, 0.41; 95% CI, 0.18–0.94). When the radiologists mentioned the nodule only in the findings section of the report, the nodule was less likely to be documented (OR, 0.30, 95% CI, 0.1–0.85). Incidental pulmonary nodules described in the radiology report as density (OR, 0.06; 95% CI, 0.01–0.47), granuloma (OR, 0.07; 95% CI, 0.01–0.65), and opacity (OR, 0.09; 95% CI, 0.01–0.68) were less likely to be documented than nodules described as mass. There was no difference in documentation between patients who had CT scans interpreted by radiologists with chest and body training and those patients who had CT scans interpreted by radiologists without chest and body training (OR, 1.09; 95% CI, 0.61–1.95).
Of the newly diagnosed incidental pulmonary nodules, 140 (41%) received subsequent follow-up. The forms of follow-up included repeat CT (107 [76%]), pulmonary referral (54 [39%]), bronchoscopy (16 [11%]), CT-guided biopsy (11 [8%]), and thoracic surgery referral (7 [5%]). Many patients received more than one form of follow-up, such as repeat CT scan and subspecialty referral.
The majority (114 [63%]) of documented nodules received follow-up, but only 27 of the 67 (40%) of those that did not receive documentation were followed (P < 0.001). The factor most strongly associated with follow-up of the nodule was documentation by the ordering or primary care provider (OR, 5.85; 95% CI, 2.93–11.7). Additional factors that were independently associated with follow-up of the incidental pulmonary nodules are listed in Table 2. Patients with incidental pulmonary nodules whose radiology report used the term nodule (OR, 0.15; 95% CI, 0.02–0.99), nodular density (OR, 0.09; 95% CI, 0.01–0.63), granuloma (OR, 0.06; 95% CI, 0.01–0.69), or opacity (OR, 0.05; 95% CI, 0.01–0.43) were less likely to receive follow-up compared with patients with reports using the term mass. There was no difference in follow-up between patients who had CT scans interpreted by radiologists with chest and body training and those patients who had CT scans interpreted by radiologists without chest and body training (OR, 1.76; 95% CI, 0.94–3.29).
Of the 34 pulmonary nodules that underwent biopsy, 26 (76%) were found to be cancerous (lung and other malignancies). Noncancerous diagnoses included granulomatosis with polyangiitis, sarcoidosis, and chronic granulomatous infections. Within 2 years of pulmonary nodule diagnosis, 34 (10%) patients died. Most patients who died had documentation of their pulmonary nodules (26 [76%]). There was no difference in mortality at 2 years between those who underwent follow-up (15 [11%]) and those who did not (19 [9%]; P = 0.71).
Discussion
Over half of the patients with incidental pulmonary nodules detected by CT scans at a large urban safety net medical system had some form of documentation by the ordering or primary care provider. However, fewer than half of the patients underwent follow-up. In addition, there was significant variability in documentation and follow-up of the nodules, depending on the terms used by the radiologists to describe them. This suggests that the language used by interpreting radiologists may significantly impact nodule documentation, evaluation, and management.
Preston Hickey, the first editor of the American Journal of Roentgenology, is credited with encouraging use of the word radiograph as standard terminology to describe images produced by X-rays (13). In 1904, recognizing the emerging importance of the radiologic report, he coined the term interpretation to describe the systematic method of describing radiologic findings and their implications (14). Throughout his career, he continued to push for adoption of standardized nomenclature and reporting similar to that used in pathology (15). The Hickey method remains the foundation upon which many modern radiology reports are based (13). However, despite the many advances that have occurred in radiology since Hickey’s tenure, there remains a need for a systematic approach to reporting radiologic findings that communicates clinically relevant information to the ordering physician (16, 17).
In addition to terminology, there is significant variability in conformity with nodule management guidelines, despite the fact that the Fleischner Society guidelines were released in 2005 (4). In a 2010 survey of 834 radiologists, 78% were aware of the guidelines, and 59% worked in practices that used some form of nodule guidelines. However, management decisions that were consistent with the guidelines ranged from 35 to 61% (18). A 2011 survey of 27 radiologists at 3 geographically dispersed academic institutions adhered with the guidelines 69% of the time (19). Radiologists’ guideline adherence for nodules may be affected by practice location, particularly if the practice is located in an endemic region of granulomatous disease (20).
The American College of Radiology has developed the Lung Imaging Reporting and Data System (Lung-RADS) as a quality assurance tool to standardize lung cancer screening CT reporting and management recommendations (http://www.acr.org/quality-safety/resources/lungrads). Implementation of the Lung-RADS system may be an effective way of improving the performance of lung cancer screening programs (21). While assessment categories and management recommendations for Lung-RADS have been developed, a complete lexicon to standardize the language used in CT reports has yet to be released. With incorporation into the electronic health record and standardization of terminology, Lung-RADS may be an even more effective tool for improving patient outcomes.
Variability in radiologist reporting is not unique to pulmonary findings. For example, in CT and magnetic resonance imaging of the thyroid, radiologists disagree on when to report incidental nodules, particularly in patients with a history of lung cancer (22). In a study of calcifications detected by mammography, radiologists inconsistently used terminology to describe their findings—more than 50 terms were used to describe the findings (23). This suggests that standardized reporting across radiology may remain as important today as it was when Hickey advocated for it.
Our findings are consistent with those of others. A recent evaluation of 300 patients with pulmonary nodules revealed that the strongest predictor of guideline-inconsistent management was guideline-inconsistent radiologist recommendations (24). In a cohort of 419 patients with incidentally detected lung nodules on CT scans, radiologists recommended additional CT surveillance in 74% of patients (25). Only 48% of the patients underwent at least one recommended surveillance chest CT scan. The likelihood of CT surveillance increased if the result of the CT scan was communicated to the patient (OR, 2.2, 95% CI, 1.3–4.0) or the referring physician (OR, 2.8; 95% CI, 1.7–4.5). In our present study, radiologists recommended follow-up less often (56%), and 41% of patients underwent nodule follow-up. After adjusting for other factors such as nodule terminology, we did not find that radiologist documentation of communication with the provider increased documentation or follow-up of the nodule. This suggests that factors such as nodule terminology may confound the relationship between documentation of communication with the provider and documentation or follow-up of the nodule. These findings should be clarified in subsequent studies and may reinforce the need to promote a standard lexicon in nodule documentation.
Recent work has helped to elucidate the reasons why primary care practitioners depend on the findings of the radiology report of incidental pulmonary nodules to guide their follow-up decisions. A focus group study of primary care providers determined that they lack the time, knowledge, and resources necessary to provide adequate services to patients with incidental pulmonary nodules (9). In addition, many expressed that they did not include patients when making decisions regarding nodule follow-up. There may be opportunities to develop joint radiology and primary care interventions to enhance nodule evaluation and management.
Strengths and Limitations
The strengths of this study include the large sample size of patients across diverse ambulatory settings, including urgent care and emergency departments. The study population underwent CT scans in usual care settings rather than in the context of a study or other specialized setting. Each CT scan report was reviewed manually in duplicate by trained physician abstractors. The electronic health record of each patient was reviewed over 2 years following nodule identification to determine whether the nodule had been documented, whether subsequent management had occurred, and whether the patient had died.
This study has several limitations. The study included patients in a single health care system. It is possible that patients underwent further evaluation of their nodules in another health care system. However, recent data suggest that patients who receive care in different systems are particularly vulnerable to lack of follow-up (25, 26). Regardless of where follow-up occurred, initial documentation of the incidental pulmonary nodules by the ordering provider should have occurred. Studies of trauma patients with incidental findings detected on imaging have confirmed lower rates of both documentation (15–48%) and follow-up (49%) (27, 28). This is likely due to poor communication between health care systems as well as between providers and patients.
The low mortality rate precluded us from determining which terms used by radiologists to describe incidental pulmonary nodules were independently associated with death. In addition, the study design precludes us from determining the specific reasons why radiologists chose the terms used to describe nodules. Also, some subgroups had relatively few patients.
Conclusions
The term used by radiologists to describe incidental pulmonary nodules is associated with provider documentation and nodule follow-up. Additional work is needed to determine the best ways of increasing provider recognition, communication, and management of incidental pulmonary nodules. In particular, it is important to determine if standardized terminology within CT scan reports results in improved patient outcomes.
Footnotes
Supported in part by grants P60MD002265 and UL1RR024989 from the National Institutes of Health and grants R39OT22056 and R39OT26989 from the U.S. Department of Health and Human Services, Health Resources & Services Administration.
Author Contributions: Full access to all of the data in the study and responsibility for the integrity of the data and the accuracy of the data analysis: J.D.T.; study conception and design; collection and assembly of data; analysis and interpretation of the data; critical revision of the manuscript for important intellectual content; and administrative, technical, or material support: all authors; drafting of the manuscript: M.N.I., E.S., A.M.H., V.K., and J.D.T.; statistical expertise: A.M.H., V.K., C.S., and J.D.T.; obtaining of funding: J.P., M.C., C.S., and J.D.T.; and study supervision: M.N.I., A.M.H., V.K., C.S., and J.D.T.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008;27:1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, Greenlee RT, Kruger RL, Hornbrook MC, Roblin D, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA. 2012;307:2400–2409. doi: 10.1001/jama.2012.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gould MK, Tang T, Liu ILA, Lee J, Zheng C, Danforth KN, Kosco AE, Di Fiore JL, Suh DE. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015;192:1208–1214. doi: 10.1164/rccm.201505-0990OC. [DOI] [PubMed] [Google Scholar]
- 4.MacMahon H, Austin JHM, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Jr, Swensen SJ. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395–400. doi: 10.1148/radiol.2372041887. [DOI] [PubMed] [Google Scholar]
- 5.Ost DE, Gould MK. Decision making in patients with pulmonary nodules. Am J Respir Crit Care Med. 2012;185:363–372. doi: 10.1164/rccm.201104-0679CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, Wiener RS. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e93S–e120S. doi: 10.1378/chest.12-2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slatore CG, Press N, Au DH, Curtis JR, Wiener RS, Ganzini L. What the heck is a “nodule”? A qualitative study of veterans with pulmonary nodules. Ann Am Thorac Soc. 2013;10:330–335. doi: 10.1513/AnnalsATS.201304-080OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiener RS, Slatore CG, Gillespie C, Clark JA. Pulmonologists’ reported use of guidelines and shared decision-making in evaluation of pulmonary nodules: a qualitative study. Chest. 2015;148:1415–1421. doi: 10.1378/chest.14-2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golden SE, Wiener RS, Sullivan D, Ganzini L, Slatore CG. Primary care providers and a system problem: a qualitative study of clinicians caring for patients with incidental pulmonary nodules. Chest. 2015;148:1422–1429. doi: 10.1378/chest.14-2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blagev DP, Lloyd JF, Conner K, Dickerson J, Adams D, Stevens SM, Woller SC, Evans RS, Elliott CG. Follow-up of incidental pulmonary nodules and the radiology report. J Am Coll Radiol. 2014;11:378–383. doi: 10.1016/j.jacr.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Ost D, Fein A. Evaluation and management of the solitary pulmonary nodule. Am J Respir Crit Care Med. 2000;162:782–787. doi: 10.1164/ajrccm.162.3.9812152. [DOI] [PubMed] [Google Scholar]
- 12.Kanne JP, Jensen LE, Mohammed TLH, Kirsch J, Amorosa JK, Brown K, Chung JH, Dyer DS, Ginsburg ME, Heitkamp DE, et al. Expert Panel on Thoracic Imaging. ACR Appropriateness Criteria® radiographically detected solitary pulmonary nodule. J Thorac Imaging. 2013;28:W1–W3. doi: 10.1097/RTI.0b013e31827657c8. [DOI] [PubMed] [Google Scholar]
- 13.Gagliardi RA. Preston M. Hickey. AJR Am J Roentgenol. 1990;155:235–236. doi: 10.2214/ajr.155.2.2115245. [DOI] [PubMed] [Google Scholar]
- 14.Gagliardi RA. The evolution of the X-ray report. AJR Am J Roentgenol. 1995;164:501–502. doi: 10.2214/ajr.164.2.7839998. [DOI] [PubMed] [Google Scholar]
- 15.Hickey PM. Standardization of roentgen-ray reports. AJR Am J Roentgenol. 1922;9:422–425. [Google Scholar]
- 16.Wallis A, McCoubrie P. The radiology report—are we getting the message across? Clin Radiol. 2011;66:1015–1022. doi: 10.1016/j.crad.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260:174–181. doi: 10.1148/radiol.11101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenberg RL, Bankier AA, Boiselle PM. Compliance with Fleischner Society guidelines for management of small lung nodules: a survey of 834 radiologists. Radiology. 2010;255:218–224. doi: 10.1148/radiol.09091556. [DOI] [PubMed] [Google Scholar]
- 19.Johnson PT, Horton KM, Megibow AJ, Jeffrey RB, Fishman EK. Common incidental findings on MDCT: survey of radiologist recommendations for patient management. J Am Coll Radiol. 2011;8:762–767. doi: 10.1016/j.jacr.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Esmaili A, Munden RF, Mohammed TLH. Small pulmonary nodule management: a survey of the members of the Society of Thoracic Radiology with comparison to the Fleischner Society guidelines. J Thorac Imaging. 2011;26:27–31. doi: 10.1097/RTI.0b013e3181d73a78. [DOI] [PubMed] [Google Scholar]
- 21.McKee BJ, Regis SM, McKee AB, Flacke S, Wald C. Performance of ACR Lung-RADS in a clinical CT lung screening program. J Am Coll Radiol. 2015;12:273–276. doi: 10.1016/j.jacr.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Hoang JK, Riofrio A, Bashir MR, Kranz PG, Eastwood JD. High variability in radiologists’ reporting practices for incidental thyroid nodules detected on CT and MRI. AJNR Am J Neuroradiol. 2014;35:1190–1194. doi: 10.3174/ajnr.A3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alberdi E, Taylor P, Lee R, Fox J, Todd-Pokropek A. Eliciting a terminology for mammographic calcifications. Clin Radiol. 2002;57:1007–1013. doi: 10.1053/crad.2002.1066. [DOI] [PubMed] [Google Scholar]
- 24.Wiener RS, Gould MK, Slatore CG, Fincke BG, Schwartz LM, Woloshin S. Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: too much and too little care. JAMA Intern Med. 2014;174:871–880. doi: 10.1001/jamainternmed.2014.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ridge CA, Hobbs BD, Bukoye BA, Aronson MD, Boiselle PM, Leffler DA, Sternberg SB, Roberts DH. Incidentally detected lung nodules: clinical predictors of adherence to Fleischner Society surveillance guidelines. J Comput Assist Tomogr. 2014;38:89–95. doi: 10.1097/RCT.0b013e3182a939a5. [DOI] [PubMed] [Google Scholar]
- 26.Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194–199. doi: 10.1136/bmjqs.2010.044339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paluska TR, Sise MJ, Sack DI, Sise CB, Egan MC, Biondi M. Incidental CT findings in trauma patients: incidence and implications for care of the injured. J Trauma. 2007;62:157–161. doi: 10.1097/01.ta.0000249129.63550.cc. [DOI] [PubMed] [Google Scholar]
- 28.Munk MD, Peitzman AB, Hostler DP, Wolfson AB. Frequency and follow-up of incidental findings on trauma computed tomography scans: experience at a level one trauma center. J Emerg Med. 2010;38:346–350. doi: 10.1016/j.jemermed.2008.01.021. [DOI] [PubMed] [Google Scholar]