Abstract
Objective
To evaluate the predictive value of SYNTAX Score II (SS-II) for percutaneous coronary intervention (PCI) in octogenarian (≥ 80 years old) undergoing PCI.
Methods & Results
Data from three consecutive years of octogenarian undergoing PCI from Ruijin Hospital (Shanghai, China) was retrospectively collected (n = 308). Follow up clinical data at one year including all cause mortality, cardiac mortality and main adverse cardiovascular and cerebrovascular events (MACCE) were collected. Patients were stratified according to tertiles of SS-II for PCI: SS-II ≤ 26 (n = 104), SS-II: 27–31 (n = 102), SS-II > 31 (n = 102). After adjustment for confounding factors, SS-II for PCI was an independent risk factors for all cause mortality (odds ratio: 2.77, 95% CI: 1.13–8.06; P = 0.04). Kaplan-Meier curves showed higher event rates for all cause mortality and cardiac mortality in higher tertile of SS-II for PCI (Log-Rank test P = 0.002 and P = 0.001, respectively). SS-II for PCI predicted one year mortality in octogenarian population undergoing PCI.
Conclusions
In octogenarian, SS-II which incorporated clinical variables with angiographic anatomy variable was suitable in risk stratifying and predicting clinical outcomes at one year.
Keywords: Clinical research, Elderly, Risk stratification
1. Introduction
Percutaneous coronary intervention (PCI) in elderly population is increasing. These patients were often excluded in major randomized controlled trials.[1] Short and long term survival data after PCI in this subset of population were scarce and predominantly came from small observational studies with low level evidence.[2],[3] Furthermore, this cohort is often accompanied with more co-morbidities, more likely to face procedural complications and worse in-patient outcomes and quality of life after PCI compared to younger patients.[4]–[7] Therefore, risk stratification in this population is essential to understand better which patients would likely to have better outcomes with PCI.
Multiple risk stratification models had been suggested to have predicted outcomes in patients undergoing PCI. The SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery) score quantifies coronary lesions with respect to their location and anatomical complexity. The SYNTAX score (SS) was developed to aid clinicians in choosing the optimum revascularization approach in patients with complex coronary artery disease.[8],[9] For many years, it was considered an important tool in decision making between these choices of revascularization and advocated in European and US guidelines.[10],[11] It was validated in numerous studies and shown to be predictive for clinical outcomes in patients undergoing PCI.[12]–[15] However, it was a sole angiographic grading tool only with no consideration for clinical factors.
Clinical factors have been known to have impact on long term outcomes in patients undergoing PCI. Some studies have demonstrated that the addition of clinical variables might provide a better risk stratification and predictive value than anatomical complexity alone.[16]–[19] SYNTAX score II (SS-II) was recently developed by applying a Cox proportional hazards model to the results of the SYNTAX trial. SS-II provided difference in four year mortality rate prediction for patients undergoing PCI or coronary artery bypass surgery (CABG).[20] It was internally validated in the SYNTAX trial and externally validated in the multinational DELTA and Credo-KYOTO registries for eastern population.[20]–[22] The purpose of our study was to determine the usefulness of SS-II in predicting clinical outcomes in octogenarian population at one year from distinct, regional epidemiological characteristics.
2. Methods
2.1. Study population
Data from three consecutive years of octogenarian undergoing PCI from Ruijin Hospital (Shanghai, China) were retrospectively collected. Inclusion criteria were all patients at their eight decade of life undergoing PCI with drug eluting stent (DES) for single or multivessel disease. Exclusion criteria were previous CABG history and the presence of other severe diseases with less than one year survival. From a total of 345 patients who fitted the inclusion criteria, nine patients were excluded from missing angiographic data and 13 patients were excluded from missing follow up data. After excluding patients with previous CABG history, a total of 308 patients were finally included in analysis.
2.2. SS-II
SS-II has been described previously.[20] In briefs, SS-II was derived using the predefined algorithm by including anatomical SS, the presence of left main disease and six different clinical variables into account resulting in SS-II. The six clinical variables include age, creatinine clearance (CrCl), left ventricular ejection fraction (LVEF), sex, chronic obstructive pulmonary disease (COPD), and peripheral vascular disease (PVD). CrCl was defined by the Cockcroft and Gault formula.[23] LVEF was taken by transthoracic echocardiography or diagnostic left ventriculography. COPD followed EuroSCORE definition which was defined by the use of long term bronchodilators or steroids for lung disease.[24] PVD followed Arterial Revascularization Therapies Study Part I (ARTS I) definition.[25] The SS-II resulted in two different score for PCI and CABG each. Each score showed four year mortality rate prediction following revascularization with PCI or CABG. Theoretically, revascularization method should be chosen based on which mode of revascularization had the better mortality rate prediction.
2.3. Study endpoints and data collection
The purpose of this study was to assess the capabilities of SS-II for PCI in risk stratifying and predicting one year clinical outcomes in octogenarian undergoing PCI. The primary endpoints were all cause mortality and cardiac mortality at one year. Cardiac mortality was defined as all death attributable from cardiovascular causes and all death from unknown or was not attributable from non-cardiovascular events. Secondary endpoint was main adverse cardiovascular and cerebrovascular events (MACCE) at one year. MACCE was defined as a composite of all cause mortality, myocardial infarction, stroke, cardiac hospitalization and target lesion revascularization (TLR).
Baseline data were collected from hospital database and assessed retrospectively. Follow up data were collected from hospital database for primary and secondary endpoints at one year or by telephone interview if no data from hospital database was available. Anatomical SS was calculated using the online version of SS score calculator (www.syntaxscore.com) by two cardiologists blinded to the study baseline and follow up data. In case of disagreement, a third observer was involved and the final decision was made by consensus. SS-II for PCI was calculated using a normogram presented by Farooq, et al.[20] Patients were stratified according to tertiles of SS-II for PCI and baseline clinical characteristics and clinical outcomes were compared across these groups.
2.4. Statistical analysis
Data were presented as mean ± SD if continuous and presented as number (percentages) if categorical. Differences between groups for continuous data were evaluated with the Students t test or Mann-Whitney U test as appropriate. For categorical variables, differences between groups were evaluated with the Chi-square test. Patients were stratified according to tertile distribution of SS-II for PCI (SS-II ≤ 26, SS-II: 27–31 and SS-II > 31) and the clinical outcomes between these groups were determined using the Kaplan-Meier and compared using the Log-Rank test. Clinical outcomes according to tertiles of anatomical SS were also determined using the same method. Possible association between anatomical SS and SS-II for PCI with all cause mortality was performed using multivariable regression analysis with adjustment for age, sex, body mass index, smoking history, diabetes mellitus (DM), hypertension, hyperlipidemia, multivessel disease, COPD and CrCl. All statistical analysis was performed using SPSS 23.0 for Windows (SPSS, Inc. Chicago, IL, USA). All tests were two-sided with an overall significance of alpha = 0.05.
3. Results
3.1. Baseline characteristics
All data from 80–89 years old patients undergoing PCI in Ruijin hospital (Shanghai, China) between 2012 until 2014 were collected. On the basis of exclusion criteria, a total of 308 patients were finally included in analysis. Mean value of SS-II for PCI was 28.66 ± 6.38. Baseline characteristics and the comparison between groups were presented in Table 1. Patients in higher tertile of SS-II for PCI were associated with older, more proportion of female, shorter, more frequently had COPD and previous myocardial infarction with lower weight, LVEF, and CrCl. Angiographic characteristics according to tertiles of SS-II for PCI were presented in Table 2. Patients in higher tertile had more proportion of three vessels disease and involvement of left anterior descending artery (LAD) and right coronary artery (RCA).
Table 1. Baseline clinical characteristics according to SS-II for PCI tertiles.
| Low tertile (n = 104) | Intermediate tertile (n = 102) | High tertile (n = 102) | P Value | |
| Age, yrs | 82.39 ± 2.22 | 82.44 ± 2.34 | 83.29 ± 2.62 | 0.011 |
| Female | 12/104 (11.5%) | 38/102 (37.3%) | 78/102 (76.5%) | < 0.001 |
| Weight, kg | 68.02 ± 9.72 | 62.42 ± 9.35 | 58.73 ± 8.2 | < 0.001 |
| Height, cm | 167.41 ± 6.63 | 163.04 ± 8.05 | 159.19 ± 6.85 | < 0.001 |
| Smoking history | 0.09 | |||
| Current smoker | 10/104 (9.6%) | 5/102 (4.9%) | 5/102 (4.9%) | |
| Ex-smoker | 11/104 (10.6%) | 6/102 (5.9%) | 3/102 (2.9%) | |
| None | 83/104 (79.8%) | 91/102 (89.2%) | 94/102 (92.2%) | |
| Diabetes mellitus | 35/104 (33.7%) | 37/102 (36.3%) | 45/102 (44.1%) | 0.275 |
| Hypertension | 78/104 (75%) | 77/102 (75.5%) | 87/102 (85.3%) | 0.129 |
| Hyperlipidemia | 7/104 (6.7%) | 5/102 (4.9%) | 4/102 (3.9%) | 0.653 |
| Family history of CAD | 1/104 (1%) | 2/102 (2%) | 1/102 (1%) | 0.77 |
| Previous MI | 18/104 (17.3%) | 24/102 (23.5%) | 35/102 (34.3%) | 0.017 |
| Previous PCI | 37/104 (35.6%) | 28/102 (27.5%) | 25/102 (24.5%) | 0.194 |
| Previous stroke | 20/104 (19.2%) | 16/102 (15.7%) | 16/102 (15.7%) | 0.735 |
| COPD | 2/104 (1.9%) | 8/102 (7.8%) | 12/102 (11.8%) | 0.022 |
| LVEF, % | 63.79 ± 6.13 | 61.92 ± 9.65 | 56.9 ± 10.41 | < 0.001 |
| Creatinine, µmol/L | 83.5 ± 21.36 | 94.74 ± 33.19 | 101.47 ± 37.5 | < 0.001 |
| CrCl, mL/min | 59.36 ± 13.53 | 47.15 ± 11.59 | 38.92 ± 10.57 | < 0.001 |
Values are n/N (%) or mean ± SD. CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease; CrCl: creatinine clearance; MI: myocardial infarction; LVEF: left ventricular ejection fraction; PCI: percutaneous coronary intervention; SS-II: SYNTAX score II.
Table 2. Angiographic characteristics according to SS-II for PCI tertiles.
| Total | Low tertile (n = 104) | Intermediate tertile (n = 102) | High tertile (n = 102) | P-value | |
| One, two, or thee vessels disease | < 0.001 | ||||
| One vessel | 133 | 61 (58.7%) | 43 (42.2%) | 29 (28.4%) | |
| Two vessels | 120 | 35 (33.7%) | 44 (43.1%) | 41 (40.2%) | |
| Three vessels | 55 | 8 (7.7%) | 15 (14.7%) | 32 (31.4%) | |
| Chronic total | 41 | 7 (6.7%) | 21 (20.6%) | 13 (12.7%) | 0.013 |
| Occlusion | |||||
| Lesion localization | |||||
| Left main | 19 | 4 (3.8%) | 6 (5.9%) | 9 (8.8%) | 0.329 |
| LAD | 226 | 64 (61.5%) | 77 (75.5%) | 85 (83.3%) | 0.002 |
| LCX | 154 | 52 (50%) | 45 (44.1%) | 57 (55.9%) | 0.244 |
| RCA | 156 | 38 (36.5%) | 53 (52%) | 65 (63.7%) | < 0.001 |
| Number of stents | 1.24 ± 0.57 | 1.45 ± 0.73 | 1.47 ± 0.74 | 0.028 | |
| Stent length, mm | 30.14 ± 17.94 | 35.09 ± 19.47 | 36.99 ± 21.28 | 0.036 | |
| Stent diameter, mm | 2.91 ± 0.47 | 3 ± 0.45 | 2.88 ± 0.4 | 0.128 | |
| Anatomical SS | 12.82 ± 8.6 | 18.95 ± 10.16 | 24.4 ± 11.74 | < 0.001 | |
| SS-II for PCI | 21.85 ± 2.92 | 28.45 ± 1.55 | 35.82 ± 3.6 | < 0.001 | |
Values are n, n (%) or mean ± SD. LAD: left anterior descending artery; LCX: left circumflex artery; PCI: percutaneous coronary intervention; RCA: right coronary artery; SS: SYNTAX score; SS-II: SYNTAX score II.
3.2. Primary and secondary endpoints
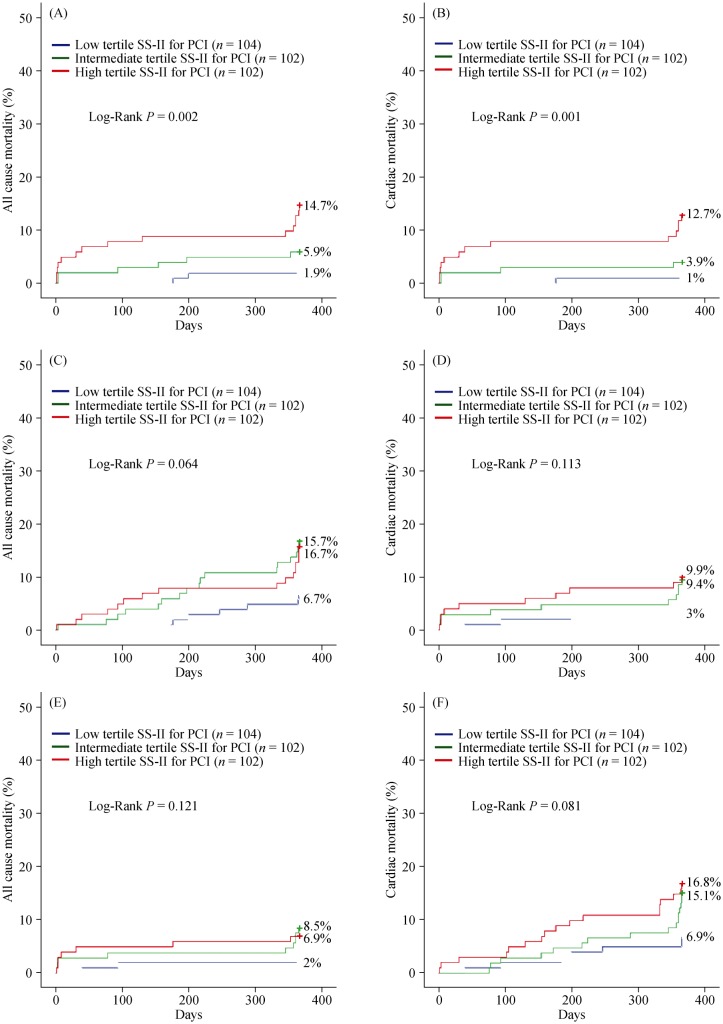
At one year, the rates of all cause mortality, cardiac mortality and MACCE was 7.5%, 5.8% and 13%, respectively. All cause mortality was 1.9%, 5.9%, and 14.7% in low, intermediate and high tertiles of SS-II for PCI, respectively (P = 0.002). Cardiac mortality was 1%, 3.9%, and 12.7% (P = 0.001) and MACCE was 6.7%, 16.7%, and 15.7% (P = 0.065). Primary and secondary endpoints for each tertiles of SS-II were shown in Table 3.
Table 3. Adverse ischemic outcomes at one year of follow up according to SS-II for PCI tertiles.
| Low tertile (n = 104) | Intermediate tertile (n = 102) | High tertile (n = 102) | P Value | |
| All cause mortality | 2 (1.9%) | 6 (5.9%) | 15 (14.7%) | 0.002 |
| Cardiac mortality | 1 (1%) | 4 (3.9%) | 13 (12.7%) | 0.001 |
| Non-cardiac mortality | 1 (1%) | 2 (2%) | 2 (2%) | 0.806 |
| Stroke | 1 (1%) | 4 (3.9%) | 1 (1%) | 0.211 |
| MI | 0 | 1 (1%) | 0 | 0.363 |
| Cardiac Hospitalization | 4 (3.8%) | 7 (6.9%) | 4 (3.9%) | 0.52 |
| TLR | 1 (1%) | 2 (2%) | 1 (1%) | 0.77 |
| MACCE | 7 (6.7%) | 17 (16.7%) | 16 (15.7%) | 0.065 |
Values are n (%). MACCE: major adverse cardiac cerebrovascular events; MI: myocardial infarction; PCI: percutaneous coronary intervention; SS-II: SYNTAX score II; TLR: target lesion revascularization.
3.3. Predictive value of SS-II for PCI and anatomical SS in octogenarian
After adjusting for confounding factors, SS-II for PCI was independently associated with all cause mortality (Odds ratio: 2.77, 95% CI: 1.03–7.42; P = 0.043). Anatomical SS was not associated with all cause mortality after adjusting for the same confounding factors. Multivariable logistic regression analysis for all cause mortality was shown in Table 4. Kaplan-Meier curves showed higher event rates for all cause mortality and cardiac mortality in higher tertile of SS-II for PCI (Log-Rank test P = 0.002 for all cause mortality and Log-Rank test P = 0.001 for cardiac mortality). However, this is not the case for MACCE (Log-Rank test P = 0.065) (Figure 1). Kaplan-Meier curves for all endpoints in anatomical SS showed no significant difference between groups (Log-Rank test P = 0.113, P = 0.121, and P = 0.081 for all cause mortality, cardiac mortality and MACCE respectively). These results suggest that, in octogenarian, scoring system like SS-II which incorporated clinical variable with angiographic variable was more accurate in risk stratifying and predicting mortality at one year.
Table 4. Predictors of mortality after PCI.
| Variables | OR (95% CI) | P value |
| *Logistic regression analysis with anatomical SS | ||
| Sex | 0.46 (0.17–1.25) | 0.126 |
| Age | 1.11 (0.92–1.33) | 0.277 |
| BMI | 0.88 (0.73–1.07) | 0.192 |
| Smoking | 0.99 (0.79–1.23) | 0.905 |
| DM | 1.01 (0.39–2.65) | 0.978 |
| Hypertension | 0.29 (0.1-0.82) | 0.02 |
| Hyperlipidemia | 9.33 (1.89–45.95) | 0.006 |
| MVD | 2.33 (0.76–7.16) | 0.141 |
| COPD | 0.32 (0.03–3.34) | 0.344 |
| CrCl | 0.96 (0.92–1.00) | 0.049 |
| Anatomical SS | 1.56 (0.8–3.06) | 0.192 |
| #Logistic regression analysis with SS-II for PCI | ||
| Sex | 1.04 (0.32–3.43) | 0.945 |
| Age | 1.08 (0.9–1.29) | 0.429 |
| BMI | 0.87 (0.72–1.05) | 0.152 |
| Smoking | 0.98 (0.78–1.22) | 0.821 |
| DM | 1.08 (0.41–2.81) | 0.883 |
| Hypertension | 0.31 (0.11-0.88) | 0.028 |
| Hyperlipidemia | 9.09 (1.8–45.85) | 0.008 |
| MVD | 2.38 (0.8–7.06) | 0.119 |
| COPD | 0.23 (0.02–2.33) | 0.213 |
| CrCl | 0.99 (0.94–1.03) | 0.596 |
| SS-II for PCI | 2.77 (1.03–7.42) | 0.043 |
*Nagelkerke R2 = 0.205, Hosmer-Lemeshow test = 0.894; #Nagelkerke R2 = 0.224, Hosmer-Lemeshow test = 0.431. BMI: body mass index; COPD: chronic obstructive pulmonary disease; CrCl: creatinine clearance; DM: diabetes mellitus; SS: SYNTAX score; SS-II: SYNTAX score II; MVD: multivessel disease; PCI: percutaneous coronary intervention.
Figure 1. Cumulative incidence of primary and secondary endpoints according to SS-II for PCI (A, B, C) and anatomical SS (D, E, F).
PCI: percutaneous coronary intervention; SS: SYNTAX score; SS-II: SYNTAX score II;
4. Discussion
The main results of the present study were as follow: (1) SS-II for PCI predicted mortality among octogenarian patients undergoing PCI; and (2) risk stratification scoring system like SS-II which incorporating clinical variables with angiographic variable stratified octogenarian populations for clinical outcomes more accurate than anatomical SS.
The main strength of the present study was this study investigated the clinical outcomes of octogenarian population which were often excluded and underrepresented in large randomized controlled trials. Elderly population presented with more comorbidities than younger population and faced more procedural complications after PCI.[26],[27] Several studies showed that PCI in elderly population is feasible and risk stratification in this population is essential.[28]–[30] Teqn, et al.[31] found that in patients aged 80 years or more with NSTEMI or unstable angina, an invasive strategy was superior to a conservative strategy in the reduction of composite events (myocardial infarction, need for urgent revascularization, stroke and death). Risk stratification in elderly patients undergoing PCI has been studied in numerous studies. These studies suggested that clinical variables when combined with angiographic variable could predict clinical outcomes better than angiographic variable alone.[2],[3]
Several studies investigated the capabilities of SS-II for PCI to appropriately stratify the risk of all cause mortality in patients in different subset of population after PCI. They suggested that SS-II was a more superior scoring system than anatomical SS in these patients.[22],[32] Similar to our findings, SS-II was more accurate in stratifying the risk of all cause mortality and cardiac mortality in our population. However, when predicting the risk of MACCE, no significant difference between these groups was detected (Log-Rank test P = 0.065).
The present study showed that risk stratification with anatomical SS showed no significant difference in predicting all-cause mortality, cardiac mortality and MACCE in our subjects. After adjusting for confounding factors, anatomical SS was not an independent predictor of mortality. These results suggested that, angiographic variable alone did not suffice to accurately stratify the risk of adverse ischemic outcomes in this population. This could be explained by the fact that octogenarians presented with more comorbidities highlighting the importance of clinical factors in risk stratification model in predicting clinical outcomes after PCI in this population. Several studies showed similar association of anatomical SS with clinical outcomes. In an analysis of CREDO-Kyoto PCI/CABG registry cohort-2 including only triple-vessel coronary artery disease, Tazaki, et al.[33] reported that the benefit of risk stratification with SS in subjects undergoing PCI could not be demonstrated. Other studies showed that addition of clinical variables into anatomical SS were proven to enhance its predictive value such as Clinical SYNTAX score[34] and Logistic clinical SYNTAX score.[35]
The SS-II was developed by applying Cox proportional hazards to the results of the SYNTAX trial.[20] In the SYNTAX trial, increasing age was independently associated with mortality.[36] Hence, one of the clinical variables in calculating SS-II was age. The SS-II was calculated using the normogram which was presented in the development and validation of SYNTAX score II study.[20] The normogram assigned scores for the presence and magnitude of each predictor variable. However, in the age variable, the maximal age was 80 years, indicating that no incremental score was added to the subject above 80 years old. The fact that the maximal score was for 80 years old, indicates that octogenarian population was not or was underrepresented in this study. For the present study, since all the subjects were 80 years old or more, the maximal score (score assigned to 80 years old) was used instead.
The presence of DM was not associated to mortality in our study. This finding further confirmed the concept of SS-II, which did not include the presence of DM to the score. In the SYNTAX trial, DM was not an independent predictor of mortality and did not produce an interaction effect in affecting long term mortality between CABG and PCI.[36] Once again, octogenarian population was also underrepresented in these studies. The present study suggested that, even in octogenarian population, DM was not an independent predictor of mortality in patients undergoing PCI.
The limitations of the present study were as follow: first, this study was retrospective in nature; second, this was a small one center study with only 308 patients, with its limitation; third, anatomical SS calculation is associated with intraobserver and interobserver variability. Indeed, the calculation of anatomical SS in this study was performed by cardiologists with basic training in anatomical SS calculation. At last, the present study included octogenarian undergoing PCI only. Subjects undergoing CABG were not included in analysis.
In conclusion, in octogenarian population undergoing PCI, the SS-II stratifies and predicts mortality at one year more accurate than anatomical SS.
Acknowledgments
All authors reported no conflict of interest regarding this publication.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Vassalli G, d'Angeli I, Scherff F, et al. Comparison of clinical and angiographic prognostic risk scores in elderly patients presenting with acute coronary syndrome and referred for percutaneous coronary intervention. Swiss Med Wkly. 2015;145:w14049. doi: 10.4414/smw.2015.14049. [DOI] [PubMed] [Google Scholar]
- 3.Sinning JM, Asdonk T, Erlhöfer C, et al. Combination of angiographic and clinical characteristics for the prediction of clinical outcomes in elderly patients undergoing multivessel PCI. Clin Res Cardiol. 2013;102:865–873. doi: 10.1007/s00392-013-0599-5. [DOI] [PubMed] [Google Scholar]
- 4.Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises. Circulation. 2003;107:346–354. doi: 10.1161/01.cir.0000048893.62841.f7. [DOI] [PubMed] [Google Scholar]
- 5.Rajani R, Lindblom M, Dixon G. Evolving trends in percutaneous coronary intervention. Br J Cardiol. 2011;18:73–76. [Google Scholar]
- 6.Panasewicz A, Pedersen SS, Veenhuis SJ, et al. Health-related quality of life in the elderly three years after percutaneous coronary intervention. EuroIntervention. 2013;9:373–381. doi: 10.4244/EIJV9I3A60. [DOI] [PubMed] [Google Scholar]
- 7.Murphy JC, Kozor RA, Figtree G, et al. Procedural and in-patient outcomes in patients aged 80 years or older undergoing contemporary primary percutaneous coronary intervention. EuroIntervention. 2012;8:912–919. doi: 10.4244/EIJV8I8A140. [DOI] [PubMed] [Google Scholar]
- 8.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 9.Capodanno D, Capranzano P, Di Salvo ME, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. J Am Coll Cardiol Intv. 2009;2:731–738. doi: 10.1016/j.jcin.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Windecker S, Kolh P, Alfonso F, et al. Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2014;35:2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 11.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–e122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Kim YH, Park DW, Kim WJ, et al. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) score for prediction of outcomes after unprotected left main coronary revascularization. J Am Coll Cardiol Intv. 2010;3:612–623. doi: 10.1016/j.jcin.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Wykrzykowska JJ, Garg S, Girasis C, et al. Value of the SYNTAX score for risk assessment in the allcomers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus ERodable Stent coating) trial. J Am Coll Cardiol. 2010;56:272–277. doi: 10.1016/j.jacc.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 14.Palmerini T, Genereux P, Caixeta A, et al. Prognostic value of the SYNTAX score in patients with acute coronary syndromes undergoing percutaneous coronary intervention: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage StrategY) trial. J Am Coll Cardiol. 2011;57:2389–2397. doi: 10.1016/j.jacc.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 15.Palmerini T, Genereux P, Caixeta A, et al. The prognostic utility of the SYNTAX score on 1-year outcomes after revascularization with zotarolimus- and everolimus-eluting stents: a substudy of the RESOLUTE all comers trial. J Am Coll Cardiol Intv. 2011;4:432–441. doi: 10.1016/j.jcin.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 16.Singh M, Rihal CS, Lennon RJ, et al. Comparison of Mayo Clinic risk score and American College of Cardiology/American Heart Association lesion classification in the prediction of adverse cardiovascular outcome following percutaneous coronary interventions. J Am Coll Cardiol. 2004;44:357–361. doi: 10.1016/j.jacc.2004.03.059. [DOI] [PubMed] [Google Scholar]
- 17.Romagnoli E, Burzotta F, Trani C, et al. EuroSCORE as predictor of in-hospital mortality after percutaneous coronary intervention. Heart. 2009;95:43–48. doi: 10.1136/hrt.2007.134114. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Ahn JM, Park DW, et al. EuroSCORE as a predictor of death and myocardial infarction after unprotected left main coronary stenting. Am J Cardiol. 2006;98:1567–1570. doi: 10.1016/j.amjcard.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 19.Garg S, Serruys PW. Interventional cardiology: coronary angioplasty: do we need to EuroSCORE? Nat Rev Cardiol. 2009;6:267–268. doi: 10.1038/nrcardio.2009.27. [DOI] [PubMed] [Google Scholar]
- 20.Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX. score II. Lancet. 2013;381:639–650. doi: 10.1016/S0140-6736(13)60108-7. [DOI] [PubMed] [Google Scholar]
- 21.Chieffo A, Meliga E, Latib A, et al. Drug eluting stent for left main coronary artery disease. The DELTA registry: a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment. J Am Coll Cardiol Intv. 2012;5:718–727. doi: 10.1016/j.jcin.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Campos CM, van Klaveren D, Iqbal J, et al. Predictive Performance of SYNTAX Score II in patients with left main and multivessel coronary artery disease-analysis of CREDO Kyoto registry. Circ J. 2014;78:1942–1949. doi: 10.1253/circj.cj-14-0204. [DOI] [PubMed] [Google Scholar]
- 23.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 24.Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881–882. doi: 10.1016/s0195-668x(02)00799-6. [DOI] [PubMed] [Google Scholar]
- 25.Serruys PW, Unger F, Sousa JE, et al. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117–1124. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 26.Pang J, Zhang Z, Zheng T, et al. The clinical, angiographic and prognosis characteristics of elderly patients with acute ST-segment elevation myocardial infarction-the first elderly STEMI population study in northwest of China. Int J Cardiol. 2015;179:326–328. doi: 10.1016/j.ijcard.2014.11.094. [DOI] [PubMed] [Google Scholar]
- 27.Marcolino MS, Simsek C, de Boer SP, et al. Short and long-term outcomes in octogenarians undergoing percutaneous coronary intervention with stenting. EuroIntervention. 2012;8:920–928. doi: 10.4244/EIJV8I8A141. [DOI] [PubMed] [Google Scholar]
- 28.Biondi Zoccai G, Abbate A, D'Ascenzo F, et al. Percutaneous coronary intervention in nonagenarians: pros and cons. J Geriatr Cardiol. 2013;10:82–90. doi: 10.3969/j.issn.1671-5411.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen PF, Wang DN, Chen K, et al. Outcomes of percutaneous coronary intervention in patients ≥ 75 years: one-center study in a Chinese patient group. J Geriatr Cardiol. 2015;12:626–633. doi: 10.11909/j.issn.1671-5411.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shanmugam VB, Harper R, Meredith I, et al. An overview of PCI in the very elderly. J Geriatr Cardiol. 2015;12:174–184. doi: 10.11909/j.issn.1671-5411.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teqn N, Abdelnoor M, Aaberge L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): an open-label randomised controlled trial. Lancet. 2016;387:1057–1065. doi: 10.1016/S0140-6736(15)01166-6. [DOI] [PubMed] [Google Scholar]
- 32.Xu B, Généreux P, Yang Y, et al. Validation and comparison of the long term prognostic capability of the SYNTAX score II among 1,528 consecutive patients who underwent left main percutaneous coronary intervention. J Am Coll Cardiol Intv. 2014;7:1128–1137. doi: 10.1016/j.jcin.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 33.Tazaki J, Shiomi H, Morimoto T, et al. Three-year outcome after percutaneous coronary intervention and coronary artery bypass grafting in patients with triple-vessel coronary artery disease: observations from the CREDO-Kyoto PCI/CABG registry cohort-2. EuroIntervention. 2013;9:437–445. doi: 10.4244/EIJV9I4A72. [DOI] [PubMed] [Google Scholar]
- 34.Garg S, Sarno G, Garcia-Garcia HM, et al. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv. 2010;3:317–326. doi: 10.1161/CIRCINTERVENTIONS.109.914051. [DOI] [PubMed] [Google Scholar]
- 35.Farooq V, Vergouwe Y, Räber L, et al. Combined anatomical and clinical factors for the long-term risk stratification of patients undergoing percutaneous coronary intervention: the Logistic Clinical SYNTAX score. Eur Heart J. 2012;33:3098–3104. doi: 10.1093/eurheartj/ehs295. [DOI] [PubMed] [Google Scholar]
- 36.Farooq V, Serruys PW, Bourantas C, et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur Heart J. 2012;33:3105–3113. doi: 10.1093/eurheartj/ehs367. [DOI] [PubMed] [Google Scholar]