Abstract
Purpose
The 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol management guidelines advocate the use of statin treatment for prevention of cardiovascular disease. We aimed to assess the usefulness of coronary artery calcium (CAC) for stratifying potential candidates of statin use among asymptomatic Korean individuals.
Materials and Methods
A total of 31375 subjects who underwent CAC scoring as part of a general health examination were enrolled in the current study. Statin eligibility was categorized as statin recommended (SR), considered (SC), and not recommended (SN) according to ACC/AHA guidelines. Cox regression analysis was employed to estimate hazard ratios (HR) with 95% confidential intervals (CI) after stratifying the subjects according to CAC scores of 0, 1–100, and >100. Number needed to treat (NNT) to prevent one mortality event during study follow up was calculated for each group.
Results
Mean age was 54.4±7.5 years, and 76.3% were male. During a 5-year median follow-up (interquartile range; 3–7), there were 251 (0.8%) deaths from all-causes. A CAC >100 was independently associated with mortality across each statin group after adjusting for cardiac risk factors (e.g., SR: HR, 1.60; 95% CI, 1.07–2.38; SC: HR, 2.98; 95% CI, 1.09–8.13, and SN: HR, 3.14; 95% CI, 1.08–9.17). Notably, patients with CAC >100 displayed a lower NNT in comparison to the absence of CAC or CAC 1–100 in SC and SN groups.
Conclusion
In Korean asymptomatic individuals, CAC scoring might prove useful for reclassifying patient eligibility for receiving statin therapy based on updated 2013 ACC/AHA guidelines.
Keywords: Coronary artery disease, risk assessment, calcium, hydroxymethylglutaryl-CoA reductase inhibitor
INTRODUCTION
Statin treatment has persistently demonstrated a significant benefit in diminishing cardiovascular disease (CVD) risk, especially in primary prevention settings.1,2 Recently, the American College of Cardiology (ACC) and American Heart Association (AHA) reported extensively on cholesterol management guidelines, focusing on the use of statin therapy for prevention of CVD, based on a new pooled cohort risk equation designed to predict 10-year risk of atherosclerotic cardiovascular disease (ASCVD).3 Although these updated guidelines increased the eligibility of patients for statin treatment, they also led to an overestimation of CVD risk in several particularistic populations.4,5,6
Coronary artery calcium (CAC) score is determined using cardiac computed tomography and acts a robust marker of coronary artery calcification. Prior studies have reported that CAC score is closely associated with increased coronary atherosclerotic burden, as well as future onset of adverse cardiac events.7,8,9,10 Current guidelines for assessing CVD recommend that CAC screening should be considered for primary risk assessment in asymptomatic populations.11 Furthermore, more recent studies have documented that reclassification of populations according to CAC score may facilitate treatment decision-making in clinical settings.12,13,14
Cardiovascular disease burden tends to differ according to ethnicity. Indeed, Asians often present with a low risk for CVD.15,16 Accordingly, assessing the efficacy of statin treatment according to the recently updated 2013 ACC/AHA guidelines in these individuals is warranted. Using a large multicenter registry of asymptomatic Korean adults, we sought to explore whether CAC scoring could reclassify individuals recommended for statin treatment according to the recently updated 2013 ACC/AHA cholesterol management guidelines.
MATERIALS AND METHODS
Study design and population
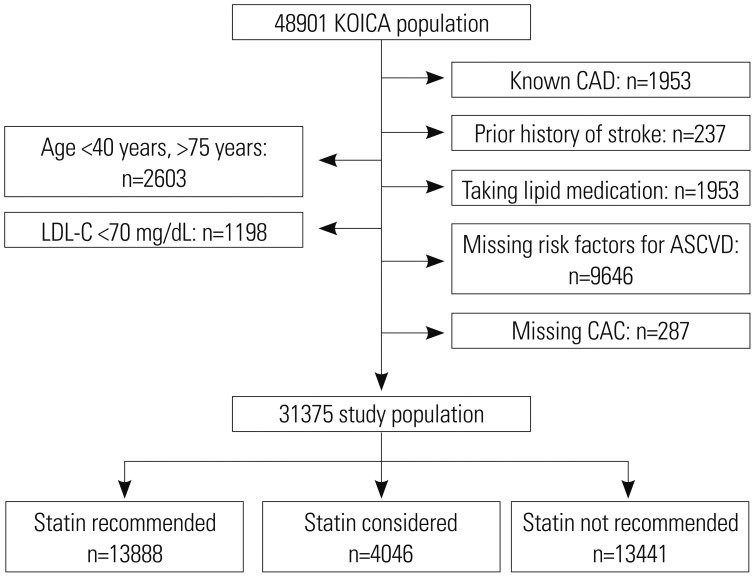
This study population belonged to the KOrea Initiative on Coronary Artery calcification (KOICA) registry. The KOICA registry is a single ethnicity, multicenter, observational registry of self-referred individuals who underwent a health check-up at one of three healthcare centers in South Korea (i.e., Severance Check-up Healthcare Center; Seoul National University Healthcare System, Gangnam Center; and Samsung Medical Center in Seoul, South Korea). A total of 48903 individuals were recruited between December 2002 and July 2014. For the purposes of this study, subjects were deemed eligible for study inclusion if they were of an age between 40 to 75 years and had no known CVD at baseline. Otherwise, individuals were excluded from the study if they were prescribed any lipid-lowering medication or were missing any values related to risk factors used for calculating 10-year ASCVD risk or CAC score. Hence, after applying the inclusion and exclusion criteria, 31375 individuals were subsequently enrolled in the current analysis (Fig. 1). The appropriate institutional review board committees at all centers approved the study protocol.
Fig. 1. Study flow chart of participant groups. KOICA, KOrea Initiative on Coronary Artery calcification; CAD, coronary artery disease; ASCVD, atherosclerotic cardiovascular disease; LDL-C, low-density lipoprotein cholesterol; CAC, coronary artery calcium.
Acquisition of clinical factors
Baseline demographic and risk factors were collected at the time of each initial visit to the healthcare centers. Age, gender, body mass index, and systolic and diastolic blood pressure were measured as baseline demographic profiles. A self-reported medical questionnaire was used to obtain information on past medical history. Presence of hypertension was defined as a history of being diagnosed with hypertension or taking antihypertensive medications. Presence of diabetes mellitus was defined as a history of being diagnosed with diabetes or receiving medication for diabetes. Current smoking was defined as active smoking status. Total, high-density lipoprotein, and low-density lipoprotein (LDL) cholesterol were obtained after participants had fasted for a minimum 8 h. CACS was measured using a >16-slice CT scanner. Specific CT scanner types used within each center included the Philips Brilliance 256 iCT, Philips Brilliance 40 channel multi-detector CT (Philips Healthcare, Cleveland, OH, USA), Siemens 16-slice Sensation (Siemens AG, Forchheim, Germany), and GE 64-slice Lightspeed (GE Healthcare, Milwaukee, WI, USA). A calcium scan was performed using standard prospective or retrospective methods with a 225 to 400 ms gantry rotation time. Image data were reconstructed with a 2.5- to 3-mm slice thickness. Calcium score analysis was performed using dedicated workstations (AW Volume Share 5 workstation, GE Healthcare; Rapidia 3D, Infinitt Co., Seoul, Korea; EBW workspace version 3.5, Philips Healthcare) and analysis software (Smart Score 4.0, GE Healthcare; Rapidia3D, Infinitt Co.; HeartBeat CS, Philips Healthcare). Estimated radiation doses for CACS ranged between 0.7–1.5 mSv. CAC score was calculated based on the Agatston scoring method,17 and subjects were categorized according to the presence any of CAC (CAC>0), as well as CAC 0, 1–100, and >100 based on the background of CAC.18,19
Statin candidate groups
In this study population, we calculated 10-year ASCVD risk, based on that for Caucasians, and subsequently categorized participants according to 2013 ACC/AHA cholesterol management guidelines using the following groups: statin recommended (SR), statin considered (SC), and statin not recommended (SN) (Table 1).3 Specifically, the SR group was defined as either: 1) those with LDL cholesterol levels ≥190 mg/dL, 2) those aged 40 to 75 years with diabetes and LDL cholesterol levels ranging from 70 to 189 mg/dL, or 3) individuals without diabetes, but with an estimated 10-year ASCVD risk of 7.5% or higher. The SC and SN groups were defined as individuals without diabetes or ASCVD events and with a 10-year ASCVD risk of between 5% to 7.5%, and <5%, respectively.
Table 1. Statin Eligibility in Study Population.
| Classification | Number (%) |
|---|---|
| SR | |
| LDL-C≥190 | 2883 (9.2) |
| DM with LDL 70–189 | 4797 (15.3) |
| ASCD risk≥7.5% | 6208 (19.8) |
| SC | |
| ASCVD risk 5–7.5% | 4046 (12.9) |
| SN | |
| ASCVD risk <5% | 13441 (42.8) |
SR, statin recommend; SC, statin considered; SN, statin not recommended; LDL-C, low-density lipoprotein cholesterol; DM, diabetes mellitus; ASCVD, atherosclerotic cardiovascular disease.
Study outcome
The primary outcome of the KOICA registry is all-cause mortality (ACM). Ascertainment of ACM events was determined by querying the Ministry of Security and Public Administration up until December 2014 for two centers and until September 2014 in the remaining center.
Statistical methods
Continuous variables are reported as means with standard deviations, and categorical variables are reported as counts with proportions. A one-way analysis of variance (ANOVA) was used for the comparison of continuous variables across statin groups, and Pearson’s Chi-squared test was employed for comparison of categorical variables between statin groups. Cumulative mortality events over time according to CAC categories and statin candidate groups were calculated by use of the Kaplan-Meier method and compared using the log rank test. Time to mortality event was assessed using incidence rates per 1000 person years. Further, Cox regression analysis was used to estimate the risk of ACM according to CAC categories across statin candidate groups, reporting adjusted hazard ratios (HR) with 95 % confidence intervals [95% confidential interval (CI)]. Models were adjusted for age, gender, BMI, hypertension, and current smoking. We calculated number needed to treat (NNT) to prevent one mortality event by applying the mortality risk associated with statin treatment in primary prevention on the basis of a Cochrane meta analysis.20 The results from 18 randomized control trials showed that the incidence of ACM is lowered by 14% according to statin treatment (odds ratio: 0.86, 95% CI: 0.79 to 0.94). The 5-year NNT was calculated as the reciprocal of the absolute risk difference at 5-year follow up based on Kaplan-Meier estimates, according to the Altman and Andersen21 method, in each CAC category across statin candidate groups. A two-tailed p value <0.05 was considered statistically significant. All statistical analyses were performed using STATA Version 13 (StataCorp LP, College Station, TX, USA).
RESULTS
Baseline characteristics
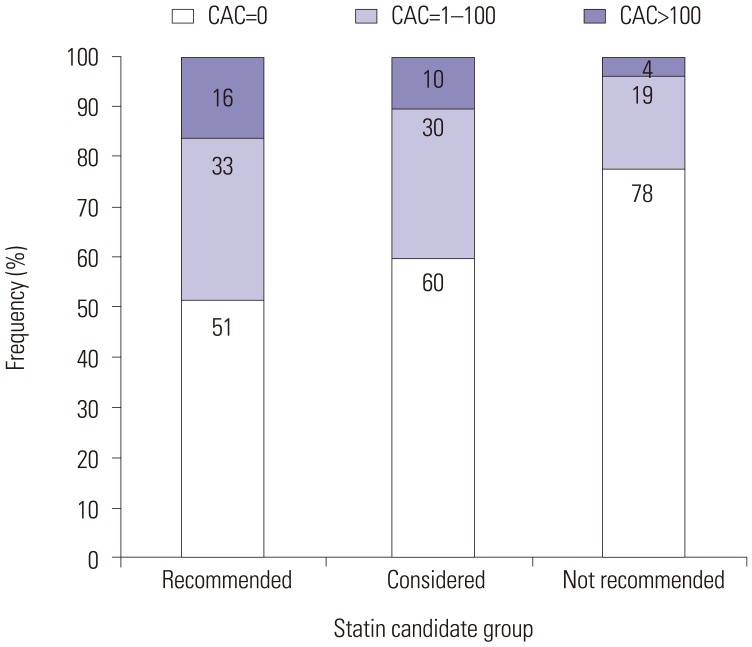
Mean age of the study participants was 54.4±7.5 years, and 23923 (76.3) were male. Baseline characteristics according to the statin candidate groups are shown in Table 2. Demographic variables and lipid profiles differed among the three statin candidate groups. CAC distribution according to statin eligibility is displayed in Fig. 2. The proportion of zero CAC was more than 50% across all statin candidate groups, while the proportion of a CAC score >100 tended to increase within the SR group (16%), as compared with the SC (10%) and SN groups (4%), respectively.
Table 2. Baseline Characteristics among Statin Candidate Groups.
| SR group (n=13888) | SC group (n=4046) | SN group (n=13441) | p value | |
|---|---|---|---|---|
| Age | 58.2±7.7 | 55.0±5.5 | 50.2±5.2 | <0.001 |
| Male | 11394 (82.0) | 3457 (85.4) | 9072 (67.5) | <0.001 |
| SBP | 124.4±15.7 | 121.7±14.5 | 116.1±13.9 | <0.001 |
| DBP | 78.9±10.8 | 78.9±10.3 | 74.9±10.7 | <0.001 |
| BMI | 24.7±2.8 | 24.8±2.6 | 24.0±2.9 | <0.001 |
| Hypertension | 7305 (52.8) | 1735 (43.6) | 4524 (33.9) | <0.001 |
| Current smoker | 4718 (34.0) | 1342 (33.2) | 1662 (12.4) | <0.001 |
| TC | 201.5±35.0 | 201.0±29.4 | 196.3±29.7 | <0.001 |
| HDL-C | 50.6±12.0 | 50.6±129.7 | 55.1±13.0 | <0.001 |
| LDL-C | 130.5±32.0 | 129.7±25.9 | 124.1±26.0 | <0.001 |
SR, statin recommended; SC, statin considered; SN, statin not recommended; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Fig. 2. Distribution of coronary artery calcium scores according to statin candidate groups. CAC, coronary artery calcium.
All-cause mortality and CAC across statin candidate groups
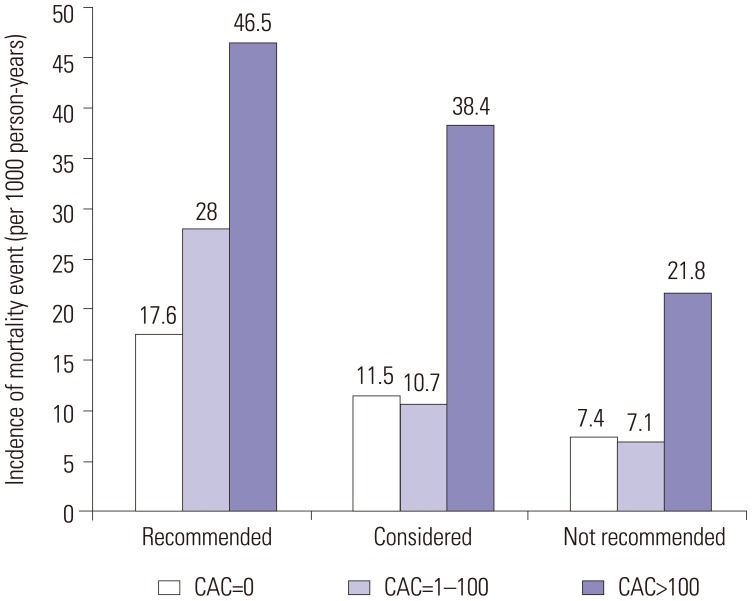
During a median follow-up of 5 years (25–75th percentile: 3–7 years), 251 mortality events occurred among 31375 subjects. Fig. 3 shows the incidence of mortality per 1000 person-years for each CAC category by statin candidate group. Notably, mortality events tended to be higher among subjects with a CAC score >100, compared with the other CAC groups. In Cox regression analysis, a CAC score >100 was independently associated with ACM in all three statin candidate groups, even after adjusting for numerous cardiac risk factors (Table 3). In particular, in the SN group, the adjusted risk of death for those with a CAC score >100 increased by more than three-fold (HR, 3.14; 95% CI, 1.08–9.17; p value, 0.036), compared with those in the SN group with a CAC=0.
Fig. 3. Incident mortality (per 1000 person-years) according to coronary artery calcium scores, and stratified by statin candidate groups. CAC, coronary artery calcium.
Table 3. Risk of All-Cause Mortality by CAC Burden Across Statin Candidate Groups.
| Unadjusted | Adjusted* | ||||||
|---|---|---|---|---|---|---|---|
| Event | HR | 95% CI | p value | HR | 95% CI | p value | |
| SR group | |||||||
| CAC=0 | 68 | Ref | Ref | ||||
| CAC=1–100 | 63 | 1.62 | 1.15–2.29 | 0.006 | 1.14 | 0.80–1.63 | 0.461 |
| CAC>100 | 47 | 2.82 | 1.94–4.10 | <0.001 | 1.60 | 1.07–2.38 | 0.022 |
| Any CAC | 110 | 1.98 | 1.46–2.68 | <0.001 | 1.29 | 0.93–1.77 | 0.124 |
| SC group | |||||||
| CAC=0 | 13 | Ref | Ref | ||||
| CAC=1–100 | 6 | 0.92 | 0.35–2.41 | 0.860 | 0.76 | 0.28–2.02 | 0.579 |
| CAC>100 | 6 | 3.66 | 1.38–9.71 | 0.009 | 2.98 | 1.09–8.13 | 0.033 |
| Any CAC | 12 | 1.46 | 0.67–3.21 | 0.342 | 1.19 | 0.53–2.66 | 0.667 |
| SN group | |||||||
| CAC=0 | 36 | Ref | Ref | ||||
| CAC=1–100 | 8 | 0.96 | 0.45–2.07 | 0.920 | 0.93 | 0.43–2.06 | 0.867 |
| CAC>100 | 4 | 3.13 | 1.11–8.84 | 0.031 | 3.14 | 1.08–9.17 | 0.036 |
| Any CAC | 12 | 1.25 | 0.65–2.40 | 0.505 | 1.21 | 0.61–2.39 | 0.584 |
CAC, coronary artery calcium; SR, statin recommended; SC, statin considered; SN, statin not recommended; HR, hazard ratio; CI, confidential interval.
*Adjusted by age, gender, body mass index, study site, hypertension, current smoking.
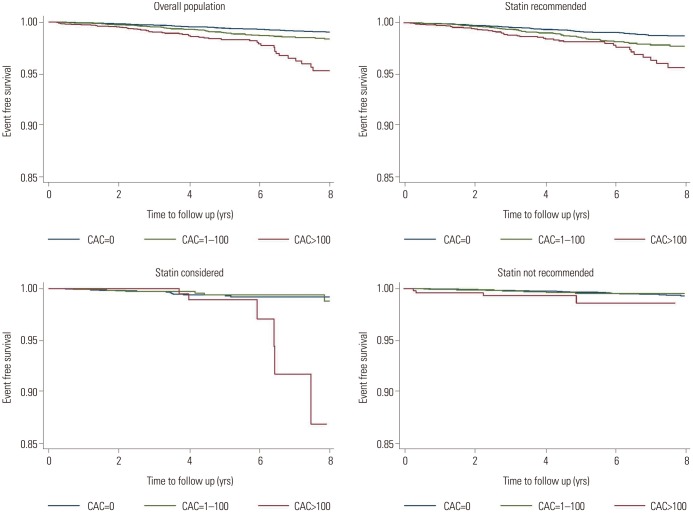
Number needed to treatment
In Fig. 4, Kaplan-Meier survival curves revealed that increasing CAC score categories were associated with a concurrent rise in mortality across each of the statin candidate groups (Log rank p values were <0.01 in overall, SR, and SC groups, and p value= 0.07 in SN group). Based on Kaplan-Meier estimates, the 5-year NNTs to prevent one ACM event was 834, 1250, and 2000 for CAC score 0; 500, 1250, and 1429 for CAC scores 1–100; and 385, 667, and 500 for CAC scores more than 100 in the SR, SC, and SN groups, respectively (Table 4). Foremost, subjects with a CAC score >100 demonstrated the lowest NNT across all statin candidate groups.
Fig. 4. Kaplan-Meier survival curves according to coronary artery calcium scores and statin candidate groups. CAC, coronary artery calcium.
Table 4. NNT According CAC Categories Across Statin Candidate Group.
| Number | NNT for ACM (14% RR*) | |
|---|---|---|
| SR group | ||
| CAC=0 | 7092 | 834 |
| CAC=1–100 | 4518 | 500 |
| CAC>100 | 2278 | 385 |
| Any CAC | 6796 | 0455 |
| SC group | ||
| CAC=0 | 2422 | 1250 |
| CAC=1–100 | 1227 | 1250 |
| CAC>100 | 397 | 667 |
| Any CAC | 1624 | 1000 |
| SN group | ||
| CAC=0 | 10454 | 2000 |
| CAC=1–100 | 2494 | 1429 |
| CAC>100 | 493 | 500 |
| Any CAC | 2948 | 1112 |
NNT, number needed to treat; CAC, coronary artery calcium; ACM, all-cause mortality; SR, statin recommended; SC, statin considered; SN, statin not recommended; RR, risk reduction.
*Based on a 14% relative reduction of ACM from a Cochran meta analysis.20
DISCUSSION
In this multicenter observational study, we assessed the impact of CAC for reclassifying statin candidates according to the 2013 ACC/AHA cholesterol management guidelines for primary prevention. The results of the present study showed that CAC is closely related to a greater risk of ACM. Specifically, a CAC score >100 independently increased the risk of ACM across all statin candidate groups, while the NNT for preventing one mortality event during the current study period was lower among subjects with a CAC score >100 in the SC and SN groups. The 2013 ACC/AHA guidelines for the assessment of cardiovascular risk recommend that CAC screening should be considered only among cases in which treatment decisions remain uncertain following quantitative risk assessment.11 Nevertheless, the results of the current investigation indicated that CAC screening may be of use in guiding initiation of statin treatment in asymptomatic individuals.
In 2014, the ACC/AHA reported new cholesterol management guidelines that were based on 10-year ASCVD risk.3 In comparison with previous scores, such as the Third Report of the National Cholesterol Education Program (NCEP ATP-III) guidelines,22 in this study, the statin-eligible population was significantly increased when applying the new guidelines. Further still, Pencina, et al.6 reported that the more recent guidelines would increase the number of candidates for statin treatment by 11.1% or 12.8 million, especially in primary prevention settings, using data from the United States National Health Survey. Although the use of statins could have a large public health benefit,23 statins cannot be recommended purely on the basis of high risk, given concerns for efficacy, potential side effects, and health-related costs.24,25 Therefore, the implication of the new cholesterol management guidelines should be carefully assessed.
In prior research, statin therapy exhibited different effects between Western and Asian populations. For example, the initiation of statin therapy in Asian populations usually begins with a lower dose, compared to Western populations, as the pharmacokinetics and metabolites of statins differ substantially by ethnicity.26 Moreover, the Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese (MEGA) study reported that the low dosage statin prescribed therein was half the dose often utilized in European and U.S. populations and could significantly lower the risk of coronary heart disease in Japanese patients.27 A recent meta-analysis evaluating the effect of statin therapy on coronary plaque also documented a different effect of statins for modifying LDL-cholesterol levels, as well as the regression of coronary atherosclerotic plaque, among ethnic groups.28
In this study, we employed CAC as a marker for reclassification of statin treatment. It is well known that CAC score has added benefit towards cardiovascular risk prediction over conventional risk tools.29,30 An additional strength is that CAC can be employed to better define target populations who require preventive treatment through prescribing cardiovascular medications. Indeed, Miedema, et al.13 investigated aspirin use for primary prevention of CHD in the Multi-Ethnic Study of Atherosclerosis (MESA). In that study, participants with a CAC score >100 showed favorable risk/benefit estimation on the background of aspirin use. Similarly, Blaha, et al.12 showed that CAC might have benefit for defining rosuvastatin eligible participants according to the Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial.31 The results of the latter study demonstrated that the absence of CAC was related to an extremely lower CVD event rate in statin eligible participants.
Recently, Nasir, et al.18 reported the implications of CAC testing among statin candidates according to 2013 ACC/AHA cholesterol management guidelines in the MESA population. In that study, ASCVD risk appeared to be heterogeneous among statin candidate groups, while CAC appeared to reclassify this population. To this end, the absence of CAC reclassified half of the candidates as not suitable for statin treatment. Our data supports those results in that CAC scoring also appeared to be effective in determining a target population among Asians who might benefit from statin therapy. Nevertheless, some disparity exists between these studies: Our study showed that a CAC >100 is closely associated with mortality events and can perhaps identify participants who may be eligible for statin treatment. However, the absence of CAC did not prove useful for predicting incident mortality or NNT when compared with the presence of CAC in our study population. It bears mentioning however, that the clinical outcomes differed between both studies, whereby ASCVD events included both ACM and non-fatal CVD events in the MESA population while in the present study, only ACM events were included. In addition, the burden of CVD is lower in Korean populations than Western populations (i.e., MESA participants) that consist mainly of Caucasians.15,32 Thus, the onset of adverse clinical events may only occur on the background of a higher level of CAC in Korean populations, particularly when compared with previous study cohorts, such as MESA.
Although, in this study, CAC scanning displayed some added benefit for reclassifying patient eligibility to receive statin therapy, the latter purpose of CAC scanning and its subsequent benefits are somewhat offset in light of the anticipated rise in healthcare costs, as well as the burden of additional radiation exposure. Though, a recent investigation from MESA study showed that CAC screening is likely to incur cost savings, compared with guideline based risk assessment strategies.33 Moreover, the radiation dose administered for CAC screening is continuously decreasing, with an effective median radiation dose comparable to mammograms.34
Limitations
The KOICA registry was designed retrospectively and observationally in nature. Thus, The KOICA population comprised only a self-referred population, and was predominantly male. Hence, our findings should be interpreted with caution when extrapolated to other populations. In light of the retrospective nature of this study and given treatment strategies for atherosclerotic disease have likely evolved since initial enrollment in 2002 through 2014, persons enrolled later into the study might have received different treatment strategies, compared to those enrolled earlier, which could have offset the risk of the study outcome. While we selected individuals who did not receive any lipid-lowering medications at baseline, we were unable to assess medication use that may have been initiated during the study follow-up period. Hence, another limitation of this study was not being able to ascertain the prevalence of statin therapy beyond CAC examination. While the new cholesterol management guidelines were based on a 10-year risk of ASCVD, information regarding ASCVD events was unavailable, as only ACM were ascertained in the KOICA registry. Therefore, further studies are needed to assess CAC and statin eligibility according to ASCVD events. Despite this, ACM is considered a useful clinical outcome as it lowers the potential for bias as opposed to utilizing a cause specific endpoint, particularly in a retrospectively designed study.35 Also, when estimating NNT, it is perhaps feasible to consider the likelihood for some uncertainty with regards to the application of reduction in risk of ACM on the background of Cochran’s meta-analysis. As such, our study’s NNT findings should be considered hypothesis generating only and interpreted with caution.
Conclusion
In a large sample of asymptomatic Koreans, CAC scoring further reclassified individuals for eligibility of statin treatment according to the recently updated 2013 ACC/AHA cholesterol management guidelines. Assessment of CAC scoring may prove useful for guiding treatment decision-making for initiating statins among Korean adults in a primary prevention setting.
ACKNOWLEDGEMENTS
This work was supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2012027176) and funded in part by a generous gift from the Dalio Institute of Cardiovascular Imaging and the Michael Wolk Foundation.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 2.Cholesterol Treatment Trialists’ (CTT) Collaboration. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382:1762–1765. doi: 10.1016/S0140-6736(13)62388-0. [DOI] [PubMed] [Google Scholar]
- 5.Vaucher J, Marques-Vidal P, Preisig M, Waeber G, Vollenweider P. Population and economic impact of the 2013 ACC/AHA guidelines compared with European guidelines to prevent cardiovascular disease. Eur Heart J. 2014;35:958–959. doi: 10.1093/eurheartj/ehu064. [DOI] [PubMed] [Google Scholar]
- 6.Pencina MJ, Navar-Boggan AM, D’Agostino RB, Sr, Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422–1431. doi: 10.1056/NEJMoa1315665. [DOI] [PubMed] [Google Scholar]
- 7.Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31:126–133. doi: 10.1016/s0735-1097(97)00443-9. [DOI] [PubMed] [Google Scholar]
- 8.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 9.Han D, Ó Hartaigh B, Gransar H, Yoon JH, Kim KJ, Kim MK, et al. Incremental benefit of coronary artery calcium score above traditional risk factors for all-cause mortality in asymptomatic Korean adults. Circ J. 2015;79:2445–2451. doi: 10.1253/circj.CJ-15-0651. [DOI] [PubMed] [Google Scholar]
- 10.Park JK, Kim JY, Kwon HM, Kim TH, Oh SJ, Hong BK, et al. Multidetector computed tomography for the evaluation of coronary artery disease; the diagnostic accuracy in calcified coronary arteries, comparing with IVUS imaging. Yonsei Med J. 2014;55:599–605. doi: 10.3349/ymj.2014.55.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 12.Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378:684–692. doi: 10.1016/S0140-6736(11)60784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7:453–460. doi: 10.1161/CIRCOUTCOMES.113.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bittencourt MS, Blaha MJ, Blankstein R, Budoff M, Vargas JD, Blumenthal RS, et al. Polypill therapy, subclinical atherosclerosis, and cardiovascular events-implications for the use of preventive pharmacotherapy: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2014;63:434–443. doi: 10.1016/j.jacc.2013.08.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jee SH, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014;4:e005025. doi: 10.1136/bmjopen-2014-005025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J, Hong Y, D’Agostino RB, Sr, Wu Z, Wang W, Sun J, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 17.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 18.Nasir K, Bittencourt MS, Blaha MJ, Blankstein R, Agatson AS, Rivera JJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2015;66:1657–1668. doi: 10.1016/j.jacc.2015.07.066. [DOI] [PubMed] [Google Scholar]
- 19.Cho I, Chang HJ, Ó Hartaigh B, Shin S, Sung JM, Lin FY, et al. Incremental prognostic utility of coronary CT angiography for asymptomatic patients based upon extent and severity of coronary artery calcium: results from the COronary CT Angiography EvaluatioN For Clinical Outcomes InteRnational Multicenter (CONFIRM) study. Eur Heart J. 2015;36:501–508. doi: 10.1093/eurheartj/ehu358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):CD004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altman DG, Andersen PK. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ. 1999;319:1492–1495. doi: 10.1136/bmj.319.7223.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 23.Pletcher MJ, Lazar L, Bibbins-Domingo K, Moran A, Rodondi N, Coxson P, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150:243–254. doi: 10.7326/0003-4819-150-4-200902170-00005. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton VH, Racicot FE, Zowall H, Coupal L, Grover SA. The cost-effectiveness of HMG-CoA reductase inhibitors to prevent coronary heart disease. Estimating the benefits of increasing HDL-C. JAMA. 1995;273:1032–1038. [PubMed] [Google Scholar]
- 25.Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124:146–153. doi: 10.1161/CIRCULATIONAHA.110.986349. [DOI] [PubMed] [Google Scholar]
- 26.Birmingham BK, Bujac SR, Elsby R, Azumaya CT, Zalikowski J, Chen Y, et al. Rosuvastatin pharmacokinetics and pharmacogenetics in Caucasian and Asian subjects residing in the United States. Eur J Clin Pharmacol. 2015;71:329–340. doi: 10.1007/s00228-014-1800-0. [DOI] [PubMed] [Google Scholar]
- 27.Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet. 2006;368:1155–1163. doi: 10.1016/S0140-6736(06)69472-5. [DOI] [PubMed] [Google Scholar]
- 28.Li YF, Feng QZ, Gao WQ, Zhang XJ, Huang Y, Chen YD. The difference between Asian and Western in the effect of LDL-C lowering therapy on coronary atherosclerotic plaque: a meta-analysis report. BMC Cardiovasc Disord. 2015;15:6. doi: 10.1186/1471-2261-15-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 30.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 32.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 33.Roberts ET, Horne A, Martin SS, Blaha MJ, Blankstein R, Budoff MJ, et al. Cost-effectiveness of coronary artery calcium testing for coronary heart and cardiovascular disease risk prediction to guide statin allocation: the Multi-Ethnic Study of Atherosclerosis (MESA) PLoS One. 2015;10:e0116377. doi: 10.1371/journal.pone.0116377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim KP, Einstein AJ, Berrington de González A. Coronary artery calcification screening: estimated radiation dose and cancer risk. Arch Intern Med. 2009;169:1188–1194. doi: 10.1001/archinternmed.2009.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: time for a reassessment? J Am Coll Cardiol. 1999;34:618–620. doi: 10.1016/s0735-1097(99)00250-8. [DOI] [PubMed] [Google Scholar]