Abstract
Oral cancer refers to the malignancies that occur in the oral cavity, lip and pharynx with 90% of oral cancers being squamous cell carcinomas (OSCC). OSCC has the highest mortality ratio compared to other carcinomas. Although oral cavity is easily accessible, most oral cancers are detected at a later stage leading to lower survival rates. Early detection of OSCC is a key factor in improving the prognosis and survival rate of the patient. Rapid advancement in the field of diagnosis has enabled early diagnosis of many potentially malignant conditions even before its clinical manifestations. One such diagnostic modality that has gained much relevance in the field of molecular biology has been the discovery of salivary biomarkers (DNA, RNA and protein markers). These salivary biomarkers have been shown to play a non-invasive role in the diagnosis and surveillance of oral cancer. The direct contact between the saliva and the oral cancer lesions makes it a most sensitive and specific, screening method in diagnosis, staging and follow-up. This review aims to discuss the effectiveness and the potential of salivary biomarkers as a screening tool in OSCC.
Keywords: Biomarkers, Oral squamous cell carcinoma, Saliva, Oral cancer
1. Introduction
Oral cancer ranks sixth among the cancers occurring worldwide with 90% of them being diagnosed as OSCC. However, the prognosis of OSCC is good with a survival rate of 90% in case of early detection. The gold standard for diagnosis of OSCC is biopsy followed by histopathological examination, the major drawback in this technique is delay in detection. The biomarkers which are the measurable indicators of physiological and pathological process are useful in the diagnosis and influence the prognosis of disease.
Salivary biomarkers have proven to be cost effective adjourns in diagnosis and follow-up of oral and oropharyngeal carcinoma. This review summarizes the current knowledge regarding the classification, criterias, rationale, applications, merits and demerits of salivary biomarkers in relation to oral squamous cell carcinoma.
2. Biomarkers
Biomarkers are molecular signatures that are unique to a certain disease (e.g., oral cancer), and has been defined by ‘WHO’ as any substance, structure or process that can be measured in the body or its products and influences or predicts the incidence of outcome or disease.1 Biomarkers are also defined as “a characteristic that is an objectively measured and evaluated indicator of normal biologic processes, pathogenic processes, or pharmacologic responses to therapeutic intervention” (National Institutes of Health, 1998).2 Biomarkers could be analyzed in different analytes like blood and saliva.
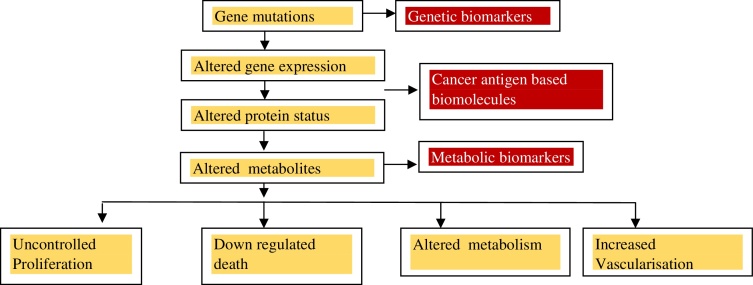
3. Classification of cancer biomarkers
Biomarkers have been classified based on biomolecules and disease states (Table 1).3
Table 1.
Classification of cancer biomarkers.3
| Based on biomolecules | Based on disease state |
|---|---|
| a. DNA biomarkers | a. Diagnostic biomarkers |
| b. RNA biomarkers | b. Prognostic biomarkers |
| c. Protein biomarkers |
3.1. Applications of biomarkers4
-
1.
Biomarkers help in predicting the preventive measures that could be formulated.
-
2.
Aids in detection of various stages of oral malignant transformation.
-
3.
Evaluates the molecular changes related to oral carcinogenesis.
-
4.
Enhances the prognosis, diagnosis, and treatment of oral carcinomas.
-
5.
Helps in manipulating the drugs used for the treatment of cancer.
4. Salivary biomarkers in the detection of oral cancer
Saliva, the readily available specimen containing large number of proteins and peptides is used as a biomarker for diagnosing various oral and systemic diseases. It is one of the most reliable tool for diagnosing oral squamous cell carcinomas because of their direct contact with oral cancer lesions. FD Shah et al. (2011) in their review on salivary genomics in oral cancer has insisted saliva as the potential biomarker for squamous cell carcinoma because of their locally expressed proteins such as alpha amylase, lactoferrins, lysozymes, proline-rich proteins, mucins, histatins, cystatins and transferrin.5 Molecular diagnosis of OSCC can be pursued in three levels. This was proved by Markopoulos et al. in their original study on salivary biomarkers for oral cancer detection.6 These include:
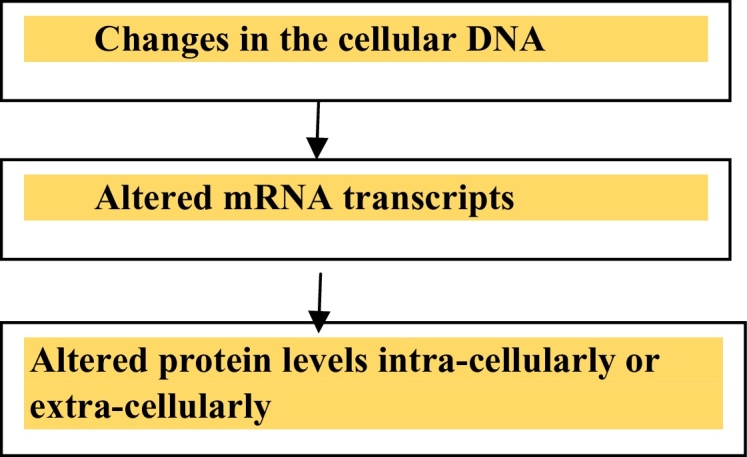
Salivary biomarkers can be a genetic marker, a protein or a metabolomic marker.1
5. Rationale behind the use of salivary biomarkers7
-
(1)
Saliva contains a wide range of compounds
-
(2)
Easily accessible
-
(3)
Patient comfort
-
(4)
Non-invasive method of disease detection
-
(5)
Safe to handle
-
(6)
Low chances of transmission compared to blood samples
-
(7)
Easy to store
-
(8)
Saliva does not clot
6. Salivary biomarkers – an update
More than 100 potential salivary biomarkers have been reported till date. Numerous analytes have been detected in saliva using various techniques (Table 2).8 Dearth of studies confirming the potential of many salivary biomarkers in detection of oral cancer is available in scientific literature (Table 3).
Table 2.
Review of salivary analytes and methods used.
| Category | Analytes | Methods used |
|---|---|---|
| Non-organic compounds | Na, Ca, F and Mg | Flame photometry, atomic absorption, and spectrophotometry |
| Peptides | Defensin-1 | High performance liquid chromatography (HPLC), Enzyme-linked immunosorbent assay (ELISA), radio-immunoassay two-dimensional gel electrophoresis (2DE), followed by mass spectrometry (MS), matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) |
| Proteins | P53, interleukin (8, 6, 1β), matrixmetalloproteinase MMP (2, 9), transforming growth factor TGF-1, cancer antigen (CA-125), statherin, CD (59, 44), carcino embryonic antigen (CEA), Ki67, cyclic D1, Cyfra 21.1, transferrin, α amylase, tumor necrosis factor – TNF-α, catalase | HPLC, ELISA, 2DE, MS, MALDI-TOF MS |
| DNA's | P53, loss of heterozygosity in the combination of markers D3S1234, D9S156, and D17S799, mitochondrial DNAs (cytochrome coxidase I and II), hypermethylation of promoters in tumor suppressor genes: DAPK, DCC, MINT-31, TIMP-31, TIMP-3, p16, MGMT, CCNA1 | Polymerase chain reaction (PCR), quantitative PCR (qPCR), microarrays followed by qPCR |
| mRNAs | DUSP1 (dual specificity phosphatase 1), IL-8, IL-1β, H3F3A (H3 histone family 3A), S100P (S100 calcium binding protein P), SAT (spermidine/spermine N1-acetyltransferase EST) | PCR, qPCR, microarrays |
| MicroRNA | miR-125a, miR-200a, miR-31 | PCR, qPCR, microarrays |
| Miscellaneous | HOTAIR, glutathione S-transferase (GST), superoxide dismutase (SOD), reactive nitrogen species (RNS) such as nitric oxide (NO), nitrites (NO2) and nitrates (NO3), glutathione | HPLC, calorimetric assays |
Adapted and modified from Cheng et al.8
Table 3.
Evidence from literature for salivary biomarkers in oral squamous cell carcinoma.
| Year | Reference | Authors | Biomarker studied | Study findings |
|---|---|---|---|---|
| 1998 | 9 | Mizukawa et al. | Defensin-1 | Higher concentrations of defensin-1 were found in OSCC patients compared to healthy controls |
| 1999 | 10 | Nagler et al. | Intermediate filament protein (Cyfra 21-1), TPS | These proteins have been detected in saliva of OSCC patients |
| 2007 | 11 | Franzmann et al. | CD44 | Increased CD44 levels in saliva (oral rinse) of OSCC patients (n = 102) compared to controls (n = 69) |
| 2004 | 12 | St John et al. | IL-8, IL-1b | Increased concentration of IL-8, IL-1b in OSCC patients |
| 2008 | 13 | Boyle et al. | P53 | p53 mutations were identified in 71% of saliva samples of OSCC patients |
| 2012 | 14 | Liu et al. | OAZ-1, SAT, IL-1b, IL-8 | Increased levels in whole unstimulated saliva in OSCC patients (n = 32) compared to controls (n = 32) |
| 2013 | 15 | Khor et al. | DUSP1 | Significantly elevated in OSCC patients |
| 2012 | 14 | Liu et al. | miR-125a, miR-200a, miR-31 | miR-125a, miR-200a levels are significantly reduced in patients with OSCC. miR-31 levels are increased in patients with OSCC compared to controls |
| 2011 | 16 | Lajer et al. | miR-31 | miR-31 was considered to be a potential biomarker to detect OSCC following microarray analysis of 51 sites from representative areas |
| 1993 | 17 | Kurakowa et al. | IAP | Increased in patients with SCC |
| 1997 | 18 | Kurakowa et al. | CA-125 | Increased concentrations detected in OSCC patients |
| 1998 | 19 | Krimmel et al. | SCC-Ag, CEA, CA 19.9, CA128 | All biomarkers were found to be elevated in patients with OSCC |
| 2008 | 20 | Hu et al. | M2BP (tumor antigen), MRP 14, CD 59, Profilm 1, catalase | Increased in whole unstimulated saliva of OSCC patients (n = 64) compared to healthy controls (n = 64). This combination of proteins provided high sensitivity (90%) and specificity (83%) in detection of OSCC |
OSCC, oral squamous cell carcinoma; TPS, tissue polypeptide specific antigen; IL, interleukin; OAZ-1, ornithine decarboxylase antizyme 1; SAT, spermidine/spermine N1-acetyltransferase; DUSP 1, dual specificity phosphatase 1; miR, microRNA; IAP, inhibitor of apoptosis; CA, carcino antigen; SCC-Ag, squamous cell carcinoma antigen; CEA, carcino embryonic antigen.
6.1. Peptides
Defensins possess antimicrobial and cytotoxic properties. The azurophil granules of polymorphonuclear leukocytes contain defensins. Studies by Mizukawa et al. have reported that OSCC can be detected even in their earlier stages by the elevated levels of salivary defensin-1 compared with healthy controls.9
6.2. Proteins
Several salivary protein markers such as interleukins (8, 6, 1β), matrix metalloproteinase (MMP 2, 9), transforming growth factor (TGF-1), Ki67, cyclic D1, Cyfra 21.1, transferrin, α amylase, tumor necrosis factor (TNF-α) and catalase have been detected in oral squamous cell carcinoma by various studies.10
Franzmann et al. reported elevated levels of CD 44 in saliva (oral rinse) of oral squamous cell carcinoma patients (n = 102) compared to controls (n = 69).11
St John et al. detected higher concentrations of IL-8 in saliva and higher concentrations of IL-6 in serum of patients with OSCC and concluded that IL-8 in saliva and IL-6 in serum are the informative biomarkers for OSCC.12
6.3. DNA
Boyle et al. in their comparative study identified p53 mutations in 71% of saliva samples from patients with OSCC by using plaque hybridization technique.13 Rosas et al. identified aberrant methylation of p16, MGMT and DAP-K in OSCC patients.
6.4. Salivary mRNAs
According to Liu et al, oral carcinogenesis can be detected by the elevation of salivary mRNAs which includes six mRNA molecules such as DUSP1, H3F3A, IL 1B, IL 8, SAT and S100.14
6.4.1. DUSP1 (dual specificity phosphatase 1)
DUSP mRNA participates in the MAPK (Mitogen Activated Protein Kinase) pathway. It is involved in protein modification, oxidative stress, and signal transduction. Molecular studies conducted by Khor et al. revealed that hypermethylation of DUSP1 gene is an important event in oral carcinogenesis.15
6.4.2. H3F3A
H3 histone family 3A, is a protein encoded by the H3F3A gene which is situated on chromosome 1. These proteins are nuclear proteins responsible for the structural integrity of chromosomal nucleosome and acts as a proliferative marker for oral cancer.
6.4.3. IL IB
Interleukin 1 beta is a member of interleukin 1 family of cytokines. It is a chemical mediator of cell proliferation, differentiation, and apoptosis. Elevated serum levels of IL IB are detected in patients with oral squamous cell carcinoma.
6.4.4. IL 8
Interleukin 8 is a pro-inflammatory cytokine, also known as neutrophil chemotactic factor. It plays an important role in tumor angiogenesis, cell adhesion, and cell cycle arrest. St John et al. by their various studies on salivary biomarkers concluded that IL 8 in saliva is the best biomarker for squamous cell carcinoma.
6.4.5. SAT
Spermidine/spermine N1-acetyltransferase 1 a protein encoded by the gene SAT, belongs to the acetyl transferase family. It participates in the catabolism of polyamines. The levels are elevated in the saliva of oral cancer patients compared to the healthy controls.
6.4.6. S100 P
S100 calcium binding protein P, a member of the S100 family is located in the cytoplasm or in the nucleus. It is responsible for cell cycle regulation and differentiation.
6.5. Salivary microRNA
MicroRNAs (miRNAs) are short RNA transcripts. Their dysregulation affects cell growth, apoptosis, differentiation, motility, and immunity. Compared to mRNA, microRNA's are significant potential biomarkers for diagnosis of oral cancer because they can accurately differentiate even poorly differentiated carcinomas. These include miR-125a, miR-200a and miR-31.
6.5.1. miR-125a
It plays an important role in cell proliferation and can affect the genes involved in MAPK metabolism. The levels of miR-125 in saliva are reduced in patients of oral cancer compared to healthy individuals.
6.5.2. miR-200a
It is involved in tumor suppression and in early metastasis. The levels of miR-200 are also reduced in the patients of oral cancer compared to healthy individuals.
6.5.3. miR-31
This is a tumor suppressor microRNA. Genetic and molecular studies conducted by Liu et al. have shown elevated miR-31 levels in all stages of squamous cell carcinoma patients and has advocated the use of miR-31 as one of the earliest biomarker to detect oral cancer.14 Lajer et al. also suggested miR-31 as one of the potential biomarker to detect oral cancer by their microarray analysis using 51 biopsies from the representative sites.16
7. Merits and demerits of salivary biomarkers
7.1. Merits
Salivary biomarkers have many advantages over serum because they are inexpensive, non-invasive, cost effective and easily accessible media and plays a vital role in diagnosis, prediction of prognosis and monitoring of patient's health. It can be used for early detection of carcinomas. It is a convenient medium for multisampling and safe for health care professionals compared to blood and is also used for detection of other types of cancers.21
7.2. Demerits22
-
1.
Lack of standardization procedures like sample collection, processing and storage.
-
2.
Variability in the levels of salivary biomarkers.
-
3.
Validation in oral inflammatory conditions.
8. Salivary biomarkers in other diseases
Salivary biomarkers are not only used for detecting oral carcinomas but evidence from several studies has proved its extensive support in diagnosing breast, lung, pancreatic and ovarian cancers (Table 4).23
Table 4.
Salivary biomarkers in carcinomas other than those involving oral cavity.
| Ovarian cancer – CA 125 |
| Breast cancer – Her2/neu, CA15, C-erb B-2 |
| Pancreatic cancer – AVP 1, ACRV1, DMXL2, DPM1 and carbonic anhydrase |
| Lung cancer – S100 |
9. Conclusion
Salivary biomarker analysis for OSCC is a major advancement in diagnosis and is a rapidly growing field of scientific research. The emergence of advanced molecular diagnostic techniques has led to the emergence of salivary biomarkers as a promising diagnostic and prognostic tool in OSCC. The use of saliva as a diagnostic medium lacks drama of blood, sincerity of sweat and emotional appeal of tears. It is convenient for multisampling and safe for health care professionals compared to blood. Salivary biomarkers can also be applied for detection of other types of cancer such as breast cancer, lung cancer, ovarian cancer and pancreatic cancer. More studies on salivary biomarkers may provide greater insight into various systemic diseases in human population.
Conflicts of interest
The authors have none to declare.
References
- 1.Bano S., David M.P., Indira A.P. Salivary biomarkers for oral squamous cell carcinoma – an overview. IJSS Case Rep Rev. 2015;1(8):39–45. [Google Scholar]
- 2.Spielmann N., Wong D.T. Saliva-diagnostics and therapeutic perspectives. Oral Dis. 2011;17(4):345–354. doi: 10.1111/j.1601-0825.2010.01773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mishra A., Verma M. Cancer biomarkers – are we ready for the prime time? Cancers (Basel) 2010;2:190–208. doi: 10.3390/cancers2010190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka T., Tanaka M., Tanaka T. Oral carcinogenesis and oral cancer chemoprevention – a review. J Pathol Res Int. 2011:1–10. doi: 10.4061/2011/431246. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Shah F.D., Begum R., Vajaria B.N. A review on salivary genomics and proteomics biomarkers in oral cancer. Indian J Clin Biochem. 2011;26(4):326–334. doi: 10.1007/s12291-011-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markopoulos A.K., Michailidou E.Z., Tzimagiorgis G. Salivary markers for oral cancer detection. Open Dent J. 2010;4:172–178. doi: 10.2174/1874210601004010172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshizawa J.M., Schafer C.A., Schafer J., Farrell J., Paster J., Wong D.T.W. Salivary biomarkers – towards future clinical and diagnostic utilities. Clin Microbiol Rev. 2014;26(4):781–791. doi: 10.1128/CMR.00021-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng Y.S., Rees T., Wright J. A review of research on salivary biomarkers for oral cancer detection. Clin Transl Med. 2014;3:1–10. doi: 10.1186/2001-1326-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mizukawa N. Defensin-1, a peptide detected in the saliva of oral squamous cell carcinoma patients. Anticancer Res. 1998;18(6B):4645–4649. [PubMed] [Google Scholar]
- 10.Nagler R.M., Barak M., Ben-Aryeh H., Peled M., Filatov M., Laufer D. Early diagnostic and treatment monitoring role of Cyfra 21-1 and TPS in oral squamous cell carcinoma. Cancer. 1999;35:101825. [PubMed] [Google Scholar]
- 11.Franzmann E.J., Reategui E.P., Pedroso F. Soluble CD44 is a potential marker for the early detection of head and neck cancer. Cancer Epidemiol Biomark Prev. 2007;16:1348–1355. doi: 10.1158/1055-9965.EPI-06-0011. [DOI] [PubMed] [Google Scholar]
- 12.St John M.A., Li Y., Zhou X. Interleukin 6 and interleukin 8 as potential biomarkers for oral cavity and oropharyngeal squamous cell carcinoma. Arch Otolaryngol Head Neck Surg. 2004;130:929–935. doi: 10.1001/archotol.130.8.929. [DOI] [PubMed] [Google Scholar]
- 13.Boyle P., Levin B. International Agency for Research on Cancer; Lyon: 2008. World Cancer Report; p. 330. [Google Scholar]
- 14.Liu J., Duan Y. Saliva – a potential media for disease diagnostics and monitoring. Oral Oncol. 2012;48:569–577. doi: 10.1016/j.oraloncology.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Khor G.H. DNA methylation profiling revealed promoter hypermethylation induced silencing of p16, DDAH2 and DUSP1 in primary oral squamous cell carcinoma. Int J Med Sci. 2013;10(12):1727–1739. doi: 10.7150/ijms.6884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lajer C.B. Different miRNA signatures of oral and pharyngeal squamous cell carcinomas a prospective translational study. Br J Cancer. 2011;104(5):830–840. doi: 10.1038/bjc.2011.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurokawa H., Tsuru S., Okada M., Nakamura T., Kajiyama M. Evaluation of tumor markers in patients with squamous cell carcinoma in the oral cavity. Int J Oral Maxillofac Surg. 1993;22:35–38. doi: 10.1016/s0901-5027(05)80353-4. [DOI] [PubMed] [Google Scholar]
- 18.Kurokawa H., Yamashita Y., Tokudome S., Kajiyama M. Combination assay for tumor markers in oral squamous cell carcinoma. J Oral Maxillofac Surg. 1997;55:964–966. doi: 10.1016/s0278-2391(97)90071-9. [DOI] [PubMed] [Google Scholar]
- 19.Krimmel M., Hoffmann J., Krimmel C., Cornelius C.P., Schwenzer N. Relevance of SCC-Ag, CEA, CA 19.9 and CA 125 for diagnosis and follow-up in oral cancer. J Craniomaxillofac Surg. 1998;26:243–248. doi: 10.1016/s1010-5182(98)80020-6. [DOI] [PubMed] [Google Scholar]
- 20.Hu S., Arellano M., Boontheung L. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res. 2008;14:6246–6252. doi: 10.1158/1078-0432.CCR-07-5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vahanwala S.P., Mukherji S. Utilisation of saliva as a diagnostic fluid in determination of oral cancer. Int J Head Neck Surg. 2014;5(1):15–20. [Google Scholar]
- 22.Bigler L.R., Streckfus C.F., Dubinsky W.P. Salivary biomarkers for the detection of malignant tumors that are remote from the oral cavity. Clin Lab Med. 2009;29(1):71–85. doi: 10.1016/j.cll.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Streckfus C., Bigler L., Tucci M., Thigpen J.T. A preliminary study of CA15-3, cerbB-2, epidermal growth factor receptor, cathepsin-D, and p53 in saliva among women with breast carcinoma. Cancer Investig. 2000;18(2):101–109. doi: 10.3109/07357900009038240. [DOI] [PubMed] [Google Scholar]