Abstract
Objectives
To compare the safety and efficacy of bipolar transurethral plasma vaporisation (B-TUVP) as an alternative to the ‘gold standard’ monopolar transurethral resection of the prostate (M-TURP) for the treatment of benign prostatic hyperplasia (BPH) in a prospective randomised controlled study.
Patients and methods
In all, 82 patients indicated for prostatectomy were assigned to two groups, group I (40 patients) underwent B-TUVP and group II (42 patients) underwent M-TURP. The safety of both techniques was evaluated by reporting perioperative changes in serum Na+, serum K+, haematocrit (packed cell volume), and any perioperative complications. For the efficacy assessment, patients were evaluated subjectively by comparing the improvement in International Prostate Symptom Score and objectively by measuring the maximum urinary flow rate (Qmax) and post-void residual urine volume (PVR) before and after the procedures.
Results
In group II, there was a significant perioperative drop in serum Na+ (from 137.5 to 129.4 mmol/L) and haematocrit (from 42.9% to 38.2%) (both P < 0.001). Moreover, one patient in group II had TUR syndrome. The remote postoperative complication rate was (15%) in group I and comprised of stress urinary incontinence (5%), bladder outlet obstruction (5%), and residual adenoma (5%). In group II, the remote postoperative complication rate was (4.8%), as two patients developed urethral stricture. There were statistically significant improvements in micturition variables postoperatively in both arms, but the magnitude of improvement was statistically more significant in group II.
Conclusion
B-TUPV seems to be safer than M-TURP; however, the lack of a tissue specimen and the relatively high retreatment rate are major disadvantages of the B-TUVP technique. Moreover, M-TURP appears to be more effective than B-TUPV and its safety can be improved by careful case selection and adequate haemostasis.
Abbreviations: BNO, bladder neck obstruction; PVR, post-void residual urine volume; Qmax, maximum urinary flow rate
Keywords: Benign prostatic hyperplasia (BPH), Bladder outlet obstruction (BOO), Transurethral resection of prostate (TURP), Lower urinary tract symptoms (LUTS), International Prostate Symptom Score (IPSS)
Introduction
BPH can be associated with bothersome LUTS that can affect quality of life [1]. It is the most frequent tumour requiring surgical treatment in ageing men [2]. When active intervention becomes mandatory, i.e. prostatectomy, TURP is the most widely available option in most clinical centres [3].
New strategies intend to achieve clinical efficacy comparable to that of conventional TURP with lower intraoperative and postoperative morbidity [2]. The general morbidity of TURP has been estimated at 18% and the overall mortality rate is 0.17–0.77% [4]. One of these new strategies is bipolar vaporisation of the prostate. The supporters of this technique claim that it has the advantage of less blood loss, lesser morbidity from the effects of water absorption and TUR syndrome, and a shorter learning curve than other prostatectomy techniques. Conversely, others report that bipolar vaporisation of the prostate results in less debulking of the gland, lesser improvements in micturition parameters, and more postoperative dysuria [5], [6].
In the shadow of this argument, we decided to compare the outcomes of bipolar transurethral vaporisation of the prostate (B-TUVP) to the standard monopolar TURP (M-TURP).
Patients and methods
After approval by our local ethics committee, this study was conducted on patients admitted to the Urology Department in Tanta University Hospital in Egypt from 1 April 2010 to the 1 January 2012 and indicated for prostatectomy.
Inclusion criteria were: patients with LUTS secondary to BOO with an IPSS of ⩾8, low maximum urinary flow rate (Qmax) < 15 m/s, not responding to medical treatment, and/or BPH complications such as refractory retention or recurrent haematuria, and prostate size <80 mL. Patients unfit for surgery and those suspected of prostatic carcinoma were excluded from the study.
All patients were evaluated preoperatively with a full clinical assessment including IPSS, uroflowmetry and ultrasonography with post-void residual urine volume (PVR) measurement.
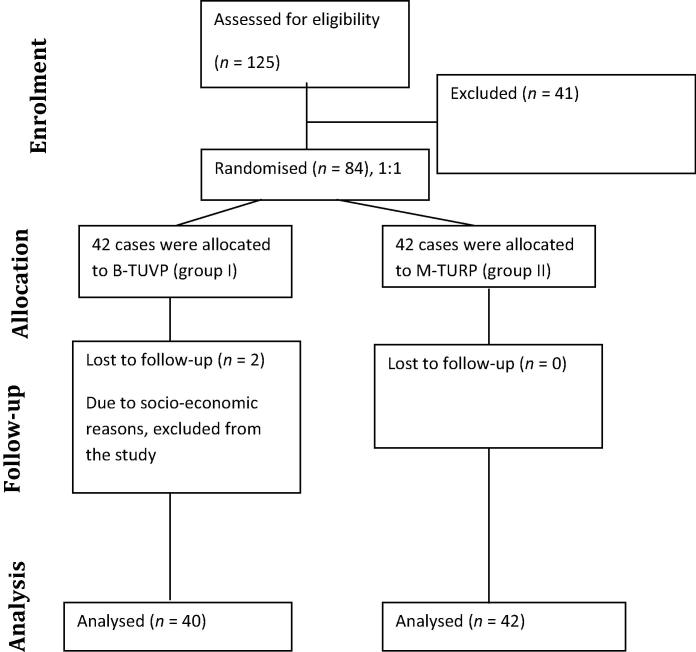
In all, 84 patients were initially enrolled in this study and were divided into two groups by 1:1 block randomisation. Group I included 42 patients who underwent B-TUVP, Group II also included 42 patients who underwent M-TURP. However, two patients in group I were lost during follow-up and excluded from the study (Fig. 1).
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flowchart of study cases.
B-TUVP/M-TURP techniques
Plasma vaporisation requires a bipolar high-frequency generator, a vaportrode and a continuous flow setup to ensure excellent visibility and sufficient elimination of vaporisation bubbles. Saline 0.9% was used as the irrigant fluid. Vaporisation was performed in a near-contact technique (hovering technique) leaving a TUR-like cavity at the end.
The monopolar generator for M-TURP was of the Berchtold type and glycine 1.5% was the irrigant fluid used. The procedures were performed using a 26-F continuous-flow resectoscope using the same surgical technique (Mauermayer technique). All procedures were performed by a single senior surgeon with extensive experience in both techniques and under spinal anaesthesia.
The primary endpoint was assessment of changes in IPSS, Qmax and PVR to evaluate the efficacy of both techniques. Safety was also evaluated by assessing perioperative changes in serum Na+, K+ and haematocrit (packed cell volume). These were measured before and immediately after the procedures. Intraoperative and early postoperative complications were reported as well. Moreover, patients attended a routine follow-up 1 week later and they were also evaluated at 3 and 6 months postoperatively for the evaluation of long-term improvement in micturition parameters and any remote postoperative complications.
Statistical analysis
Statistical analysis was conducted using the mean, standard error, t-test and Fisher’s exact test by SPSS (Statistical Package for the Social Sciences) for Windows V12. Statistically significant differences were considered at P < 0.05.
Results
Indications for intervention were: LUTS that were not responding to medical treatment, in acute urine retention, and haematuria in 73 (89%), three (3.7%) and six (7.3%) patients, respectively.
Both groups had no statistically significant differences in baseline characteristics including the patients’ age, prostate size, preoperative micturition and laboratory parameters, and operative time (Table 1).
Table 1.
Preoperative data.
| Variable, mean (SEM) | B-TUVP | M-TURP | P |
|---|---|---|---|
| Age, years | 56.9 (1.2) | 55.6 (3.1) | 0.147 |
| Prostate size, mL | 50.9 (5.3) | 53.8 (8.1) | 0.064 |
| IPSS | 24.3 (5.3) | 24.2 (4.4) | 0.978 |
| Qmax, mL/s | 7.5 (3.1) | 6.5 (2.7) | 0.268 |
| PVR, mL | 215 (7.3) | 202.1 (63.1) | 0.565 |
| Na+, mmol/L | 139.3 (5.20) | 137.5 (5.45) | 0.154 |
| K+, mmol/L | 4.9 (0.47) | 4.8 (0.50) | 0.587 |
| Haematocrit,% | 42.9 (2.51) | 42.9 (2.3) | 0.871 |
There were no cases of perioperative mortality. There was no significant difference in the complication rate between the groups. The intraoperative complications were bleeding requiring transfusion and TUR syndrome. Early postoperative complications were minor in nature e.g. UTI, clot retention and re-catheterisation. As the long-term follow-up of patients should extend to ⩾6 months, we tried to record the remote postoperative complications e.g. bladder neck obstruction (BNO), urethral stricture, and residual adenoma. Table 3 shows the details of the reported complications in both groups.
Table 3.
Complications and secondary intervention.
| B-TUVP (n = 40), n (%) | M-TURP (n = 42), n (%) | P | |
|---|---|---|---|
| Total complications | 16 (40) | 11 (26.2) | 0.241 |
| Bladder perforation | 2 (5) | 0 | 0.235 |
| Clot retention | 2 (5) | 2 (4.8) | 1 |
| Re-catheterisation | 4 (10) | 2 (4.8) | 0.427 |
| UTI | 2 (5) | 2 (4.8) | 1 |
| SUI | 2 (5) | 0 | 0.235 |
| BNO | 2 (5) | 0 | 0.235 |
| Residual adenoma | 2 (5) | 0 | 0.235 |
| Bleeding necessitating transfusion | 0 | 2 (4.8) | 0.494 |
| TUR syndrome | 0 | 1 (2.4) | 1 |
| Stricture urethra | 0 | 2 (4.8) | 0.494 |
| Modified Clavien System | |||
| Grade I | 8 (20) | 4 (9.5) | 0.221 |
| Grade II | 4 (10) | 4 (9.5) | 1 |
| Grade III | 4 (10) | 2 (4.8) | 0.427 |
| Grade IV | 0 | 1 (2.4) | 1 |
| Grade V | 0 | 0 | |
| Secondary intervention | 4 (10) | 2 (4.8) | 0.427 |
For the safety of both techniques, we measured the perioperative changes in serum Na+, serum K+ and haematocrit (Table 2).
Table 2.
Perioperative data.
| Variable, mean (SEM) | B-TUVP | M-TURP | P | |
|---|---|---|---|---|
| Operative time, min | 48.6 (5.0) | 51.2 (11.2) | 0.626 | |
| Amount of intraoperative irrigation, L | 11.1 (4.2) | 12.6 (2.0) | 0.267 | |
| Amount of postoperative irrigation, L | 14.861 (2.62) | 18.741 (2.05) | <0.001⁎ | |
| Duration of postoperative irrigation, h | 12.227 (4.66) | 24.537 (6.24) | <0.001⁎ | |
| Duration of catheterisation, h | 36.900 (4.024) | 48.283 (6.61) | <0.001⁎ | |
| Na+, mmol/L | 138 (7) | 129.4 (6.60) | <0.001⁎ | |
| P value (pre- and postoperative) | 0.511 | <0.001⁎ | ||
| K+, mmol/L | 4.8 (0.483) | 4.3 (0.42) | 0.576 | |
| P value (pre- and postoperative) | 0.524 | 0.304 | ||
| Haematocrit,% | 42.7 (2.04) | 38.2 (1.90) | <0.001⁎ | |
| P value (pre- and postoperative) | 0.824 | <0.001⁎ | ||
| IPSS | 3 months | 15.2 (1.8) | 7.8 (1.8) | <0.001⁎ |
| 6 months | 12.2 (1.0) | 7.1 (1.9) | <0.001⁎ | |
| P value preoperative vs 6 months postoperative | <0.001⁎ | <0.001⁎ | ||
| Qmax, mL/s | 3 months | 16.6 (2.2) | 18.8 (2.0) | 0.002⁎ |
| 6 months | 16.7 (1.5) | 19.5 (1.6) | <0.001⁎ | |
| P value preoperative vs 6 months postoperative | <0.001⁎ | <0.001⁎ | ||
| PVR, mL | 3 months | 65.4 (10.8) | 34.9 (10) | <0.001⁎ |
| 6 months | 60.2 (9.4) | 33.5 (2.3) | <0.001⁎ | |
| P value preoperative vs 6 months postoperative | <0.001⁎ | <0.001⁎ | ||
Statistically significant P < 0.05.
There was a statistically significant decrease in the postoperative values of serum Na+ in the patients in group II (8 mmol/L drop). Similarly and in the same group, there was a statistically significant decrease in the postoperative haematocrit (4.7% drop). Whilst, there was no statistically significant change in the perioperative serum K+ values.
Considering the duration and amount of postoperative catheter irrigation were used as an additional indirect indicator for the assessment of haemostasis or haemorrhagic complications. The mean amount and duration of irrigation was significantly higher in group II at 18.7 L and 24.5 h vs 14.9 L and 12.2 h for group I patients. Also, the mean duration of catheterisation was significantly longer in group II at 48.3 h vs 36.9 h in group I patients (Table 2).
As shown in Table 2, there were statistically significant improvements in the IPSS and Qmax accompanied by significant reductions in the PVR for both groups after 6 and 12 months, especially in group II. For the magnitude of improvement, it was statistically more evident in group II and this improvement was more evident in the Qmax than the IPSS and PVR (Fig. 2).
Figure 2.
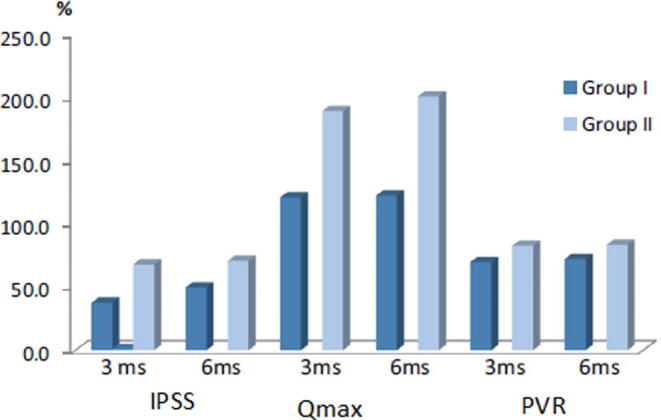
Magnitude of improvement in micturition parameters.
Secondary intervention was required in four patients (10%) in group I vs two in group II (4.8%). In group I (B-TUVP arm), re-treatment comprised bladder neck incision in two patients with BNO and re-TURP for another two patients with residual adenoma. Whilst in group II (M-TURP arm), two patients developed bulbomembranous urethral strictures and visual internal urethrotomy was required.
Discussion
Treatment of BPH varies from watchful waiting to open prostatectomy. Whenever active invention becomes mandatory (prostatectomy), TURP is the most widely available option in most clinical centres [4].
In recent years, TURP has been challenged by the development of several minimally invasive procedures. The advent of bipolar technology is the latest modification of the standard TURP technique [6], [7].
In the present study, we compared B-TUPV to M-TURP in two comparable groups of patients with BPH/benign prostatic obstruction-related LUTS, patients were randomly assigned to active treatment with B-TUVP (group I) and M-TURP (group II).
After a Medline search, we found a paucity of well-designed studies evaluating bipolar vaporisation; only four randomised studies evaluating the bipolar vaporisation technique were reported. Ahyai et al. [8] 2010 reported that there was no statistically significant difference in the safety of both techniques. Whilst, the study of Kaya et al. [9] agreed with our present study that both techniques have similar complication rates, but that B-TUVP has a higher secondary intervention rate (12% vs 6.6%).
Early experience with TURP showed that the procedure was highly morbid, with overall morbidity and mortality rates approaching 18% [4] and 2.5% [10], respectively. There is no doubt that recent technological advances and progression in the learning curve have transformed TURP from a morbid operation to a routine safe procedure with rapid convalescence and a marked reduction in the mortality of the procedure down to 0.1% and 11% overall morbidity [11].
There were no perioperative mortalities in our present study. Table 3 shows the complications encountered in both groups and classifies them according to the modified Clavien–Dindo system. Despite B-TUVP having better electrolyte stability, less postoperative irrigation, and less postoperative catheterisation time, this did not translate into statistical superiority in terms of procedure safety. However, postoperative dysuria was virtually a constant feature of all B-TUVP cases, but no alteration of postoperative care was required except in four patients who failed to void after catheter removal necessitating re-catheterisation (10%). Whilst in group II, re-catheterisation was required in two patients (4.8%) due to clot retention.
In early standard TURP series, the transfusion rates approached 20% [12], in recent series this rate has dramatically dropped to 2.9% [11]. Recently, several ex vivo studies have confirmed the superior capability of bipolar current to achieve better haemostasis through deeper coagulation and through the so called ‘cut-and-seal’ effect of plasma produced by bipolar current [13], [14], [15].
In our present series, complications related to blood loss were generally few. None of the patients treated with B-TUVP had either significant operative bleeding or required a transfusion, whilst two patients treated with M-TURP had intraoperative bleeding mandating transfusion (4.8%).
Perioperative changes in haematocrit were significant in group II (4.7% drop) vs 0.2% drop in group I. Also, the duration and amount of postoperative catheter irrigation were considered additional indirect parameters for assessment of haemostasis or haemorrhagic complications. M-TURP patients required larger amounts of irrigation fluid (mean 18.7 L) and also had a longer duration of postoperative catheter irrigation (mean 24.5 h) until the urine became clear, in addition, two patients, in group II, had frequent clot retention and required catheter exchange.
TUR syndrome is another critical issue, which is commonly referred to in arguments against TURP. Only one patient in the M-TURP arm developed TUR syndrome and was managed with diuretics and recovered smoothly. In earlier monopolar TUR series, TUR syndrome was reported in 2% [16] to 2.8% [17]. There has been a remarkable decline in more recent series, down to 0% to 0.8% [18]. Generally speaking, the incidence of TUR syndrome increases with a gland size of >45 g and resection times of >90 min.
A common agreement amongst individual studies comparing bipolar to monopolar current is the occurrence of TUR syndrome in the monopolar TURP arms vs none in the bipolar arms, although the difference was statistically insignificant in our present study and other studies, when data were pooled into a systemic meta-analysis, the overall difference was significant [8]. A secondary benefit of bipolar technology application is to extend the safe resection or vaporisation time, which in turn allows coping with larger glands without compromising safety of the patient.
The safety of the bipolar vaporisation technique is further confirmed by laboratory monitoring of perioperative changes in serum Na+. Falahatkar et al. [19] found that the mean (SD) perioperative drop in serum Na+ was 1.7 (0.19) mmol/L. In our present series, we were unfortunately confronted with a single case of TUR syndrome in group II (2.38%) vs none in group I. Retrospective analysis of the operative notes of this patient showed a prolonged resection time and subsequent over use of irrigation fluid, both of which occurred during pursuing a bleeding prostatic sinus. Similar to published data, biochemical monitoring of perioperative changes in serum Na+ showed that these changes were significant in M-TURP patients when compared to those treated with B-TUVP; an ∼8 mmol/L drop in the mean serum Na+ level occurred in group II patients.
It should be noted that different centres use variable protocols for removal of the catheter after a transurethral procedure, thus it is usually difficult to compare catheter removal with other studies. We removed catheters 24 h after the urine became clear. The mean period of catheterisation in our present series was 36.9 h and 48.3 h in groups I and II, respectively. Re-catheterisation was required in six patients, four in group I (10%) and two in group II (4.8%).
For effectiveness, B-TUVP was comparable to M-TURP, which was maintained at the 3- and at 6-month follow-up visits.
For measurable outcome parameters, M-TURP can produce up to 10 mL/s or 165% improvement in the Qmax, a 70% reduction in the IPSS, and another 70% improvement in the quality-of life scores compared with preoperative levels [8].
In the present study, both techniques were statistically effective with a marginal superiority of M-TURP over B-TUVP. At the 3-month follow-up, group II patients had a greater reduction in the symptom score at 67.8% vs 37.4% for group I. In the subsequent 6-month follow-up visit, group II patients still had a greater overall reduction in the IPSS (70.6% vs 49.7% in group I), all differences were statistically significant in comparison to the preoperative levels.
Similarly, group II patients had a greater reduction in the PVR at the 3-month follow-up visit (82.7%) than group I patients (69.6%). This improvement was maintained at the 6-month follow-up visit.
The 3-month, improvement of Qmax was 121% and 189.3% in groups I and II, respectively. At 6 months postoperatively, the Qmax improvement was 122.4% vs 201% in groups I and II, respectively.
Contrary to our present results, Zhang et al. [20] concluded that B-TUVP is superior to M-TURP in terms of efficacy parameters. Conversely, a meta-analysis study evaluating B-TUVP found that its efficacy is comparable to M-TURP for IPSS and PVR improvement, whilst M-TURP is marginally superior for Qmax changes [8].
Data taken from a nationwide analysis from Austria comparing the morbidity of TURP to open prostatectomy confirms that re-operation and secondary interventional procedures for correction of long-term TURP complications (mainly bladder neck stenosis, urethral stricture and prostatic re-growth) are relatively high, approaching 2.9%, 5.8% and 7.4% at 1, 5 and 8 years, respectively. The overall incidence of a secondary endourological procedure (TURP, internal urethrotomy, bladder neck incision) within 8 years after the initial TURP is 14.7% following the initial TURP procedure [21].
It seems that urethral stricture is a common sequela to any transurethral procedure. The urethral stricture rates following M-TURP and B-TUVP are 4% and 2%, respectively [8]. As these figures are nearly comparable, we believe that factors other than the type of the current used are responsible, for instance; the overall manoeuvre time, the size, and the insulation of the working instruments. On the other hand, a complication such as bladder neck stenosis is probably related to excessive cauterisation and dissemination of heat. Bladder neck stenosis after M-TURP and B-TUVP occur in 2% and 0.5%, respectively. Surprisingly, the risk of bladder neck stenosis is more than double (5%) after treatment with a potassium titanyl phosphate (KTP) laser [8].
The longest published follow-up period after bipolar vaporisation does not extend beyond 3 years [22]. The re-treatment and secondary intervention rate after B-TUVP is 2.4% [23].
In our present series, the follow-up of our patients extended up to 6 months after the initial procedure. The successful results reported at the 3-month visit were also maintained at 6 months.
The long-term complications and secondary intervention rates were 10% and 4.76% in groups I and II, respectively, which was not statistically significant.
Another point that should be considered is that B-TUVP does not provide a tissue specimen for histopathology, which can mean that prostate cancer is missed in 1.4% of cases [24], [25].
Limitations of the present study are a lack of long-term reporting (>6 months) and financial assessment. Also, sexual function, postoperative prostate volume, and PSA level reduction should have been evaluated. Post hoc analysis showed a relatively low study power (60%), thus further well-designed studies are needed to consolidate our present results.
Conclusion
In the present study, B-TUVP did not prove to be superior to standard M-TURP, with both techniques having comparable safety and efficacy. However, the lack of a tissue specimen and postoperative irritative LUTS are clear disadvantages of the B-TUVP technique. B-TUVP is a safe and effective alternative, but M-TURP can still defend its position.
Conflicts of interest
None.
Source of funding
None.
Prostatic Disorders
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.McNeal J.E. Origin and evolution of benign prostatic enlargement. Invest Urol. 1978;15:340–345. [PubMed] [Google Scholar]
- 2.Donnell R.F. Changes in medicare reimbursement: impact on therapy for benign prostatic hyperplasia. Curr Urol Rep. 2002;3:280–284. doi: 10.1007/s11934-002-0049-9. [DOI] [PubMed] [Google Scholar]
- 3.Black L., Naslund M.J., Gilbert T.D., Jr, Davis E.A., Ollendorf D.A. An examination of treatment patterns and costs of care among patients with benign prostatic hyperplasia. Am J Manag Care. 2006;12(Suppl. 1):S99–110. [PubMed] [Google Scholar]
- 4.Mebust W.K., Holtgrewe H.L., Cockett A.T., Peters P.C. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 2002;167:999–1003. [PubMed] [Google Scholar]
- 5.Mamoulakis C., Trompetter M., de la Rosette J. Bipolar transurethral resection of the prostate, the golden standard reclaims its leading position. Curr Opin Urol. 2009;19:26–32. doi: 10.1097/MOU.0b013e32831e44da. [DOI] [PubMed] [Google Scholar]
- 6.Gilleran J.P., Thaly R.K., Chernoff A.M. Rapid communication: bipolar PlasmaKinetic transurethral resection of the prostate: reliable training vehicle for today’s urology residents. J Endourol. 2006;20:683–687. doi: 10.1089/end.2006.20.683. [DOI] [PubMed] [Google Scholar]
- 7.Issa M.M. Technological advances in transurethral resection of the prostate: bipolar versus monopolar TURP. J Endourol. 2008;22:1587–1595. doi: 10.1089/end.2008.0192. [DOI] [PubMed] [Google Scholar]
- 8.Ahyai S.A., Gilling P., Kaplan S.A., Kuntz R.M., Madersbacher S., Montorsi F. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010;58:384–397. doi: 10.1016/j.eururo.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Kaya C., Ilktac A., Gokmen E., Ozturk M., Karaman M.I. The long-term results of transurethral vaporization of the prostate using plasmakinetic energy. BJU Int. 2007;99:845–848. doi: 10.1111/j.1464-410X.2006.06683.x. [DOI] [PubMed] [Google Scholar]
- 10.Roos N.P., Wennberg J.E., Malenka D.J., Fisher E.S., McPherson K., Andersen T.F. Mortality and reoperation after open and transurethral resection of the prostate for benign prostatic hyperplasia. N Engl J Med. 1989;320:1120–1124. doi: 10.1056/NEJM198904273201705. [DOI] [PubMed] [Google Scholar]
- 11.Reich O., Gratzke C., Bachmann A., Seitz M., Schlenker B., Hermanek P. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180:246–249. doi: 10.1016/j.juro.2008.03.058. [DOI] [PubMed] [Google Scholar]
- 12.Doll H.A., Black N.A., McPherson K., Flood A.B., Williams G.B., Smith J.C. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992;147:1566–1573. doi: 10.1016/s0022-5347(17)37628-0. [DOI] [PubMed] [Google Scholar]
- 13.Wendt-Nordahl G., Häcker A., Reich O., Djavan B., Alken P., Michel M.S. The Vista system: a new bipolar resection device for endourological procedures: comparison with conventional resectoscope. Eur Urol. 2004;46:586–590. doi: 10.1016/j.eururo.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Wendt-Nordahl G., Häcker A., Fastenmeier K., Knoll T., Reich O., Alken P. New bipolar resection device for transurethral resection of the prostate: first ex-vivo and in-vivo evaluation. J Endourol. 2005;19:1203–1209. doi: 10.1089/end.2005.19.1203. [DOI] [PubMed] [Google Scholar]
- 15.Qu L., Wang X., Huang X., Zhang Y., Zeng X. The hemostatic properties of transurethral plasmakinetic resection of the prostate: comparison with conventional resectoscope in an ex vivo study. Urol Int. 2008;80:292–295. doi: 10.1159/000127344. [DOI] [PubMed] [Google Scholar]
- 16.Wilkinson A.G., Wild S.R. Survey of urological centres and review of current practice in the pre-operative assessment of prostatism. Br J Urol. 1992;70:43–45. doi: 10.1111/j.1464-410x.1992.tb15662.x. [DOI] [PubMed] [Google Scholar]
- 17.Horninger W., Unterlechner H., Strasser H., Bartsch G. Transurethral prostatectomy: mortality and morbitidy. Prostate. 1996;28:195–198. doi: 10.1002/(SICI)1097-0045(199603)28:3<195::AID-PROS6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 18.Kallenberg F., Hossack T.A., Woo H.H. Long-term followup after electrocautery transurethral resection of the prostate for benign prostatic hyperplasia. Adv Urol. 2011;2011:359478. doi: 10.1155/2011/359478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falahatkar S., Mokhtari G., Moghaddam K., Asadollahzade A., Farzan A., Shahab E. Bipolar transurethral vaporization: a superior procedure in benign prostatic hyperplasia: a prospective randomized comparison with bipolar TURP. Int Braz J Urol. 2014;40:346–355. doi: 10.1590/S1677-5538.IBJU.2014.03.08. [DOI] [PubMed] [Google Scholar]
- 20.Zhang S.Y., Hu H., Zhang X.P., Wang D., Xu K.X., Na Y.Q. Efficacy and safety of bipolar plasma vaporization of the prostate with “button-type” electrode compared with transurethral resection of prostate for benign prostatic hyperplasia. Chin Med J (Engl) 2012;125:3811–3814. [PubMed] [Google Scholar]
- 21.Madersbacher S., Haidinger G., Struhal G. Prostate Study Group of the Austrian Society of Urology. Management of lower urinary tract symptoms of elderly men in Austria. Eur Urol. 2001;39:145–150. doi: 10.1159/000052429. [DOI] [PubMed] [Google Scholar]
- 22.Autorino R., De Sio M., D’Armiento M. Bipolar plasmakinetic technology for the treatment of symptomatic benign prostatic hyperplasia: evidence beyond marketing hype? BJU Int. 2007;100:983–985. doi: 10.1111/j.1464-410X.2007.07042.x. [DOI] [PubMed] [Google Scholar]
- 23.De Sio M., Autorino R., Quarto G., Damiano R., Perdonà S., di Lorenzo G. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. 2006;67:69–72. doi: 10.1016/j.urology.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 24.Tefekli A., Muslumanoglu A.Y., Baykal M., Binbay M., Tas A., Altunrende F. A hybrid technique using bipolar energy in transurethral prostate surgery: a prospective, randomized comparison. J Urol. 2005;174:1339–1343. doi: 10.1097/01.ju.0000173075.62504.73. [DOI] [PubMed] [Google Scholar]
- 25.Hon N.H., Brathwaite D., Hussain Z., Ghiblawi S., Brace H., Hayne D. A prospective, randomized trial comparing conventional transurethral prostate resection with plasmakinetic vaporization of the prostate: physiological changes, early complications and long-term followup. J Urol. 2006;176:205–209. doi: 10.1016/S0022-5347(06)00492-7. [DOI] [PubMed] [Google Scholar]