ABSTRACT
A 51-year-old Caucasian male was referred to neuro-ophthalmology clinic for an evaluation of acute onset of painless visual loss in the left eye. The ocular examination revealed subtle retinal changes suspicious for chorioretinitis. Laboratory workup revealed a reactive Treponema pallidum particle agglutination assay (TP-PA), confirming the diagnosis of ocular syphilis. The patient was treated with intravenous infusion of penicillin with complete recovery of vision and resolution of retinal abnormalities.
Keywords: Autofluorescence, chorioretinitis, optical coherence tomography (OCT), syphilis, Treponema pallidum, vision loss
A 51-year-old Caucasian male presented to neuro-ophthalmology clinic with complaint of seeing a large grey spot in central vision of the left eye for 3 days, with no other visual or systemic symptoms. He reported no significant medical or ocular history, and no recent illnesses or travel. He works from home as a computer administrator for two local companies. The patient reported no use of tobacco, excessive alcohol, prescribed or over-the-counter medication.
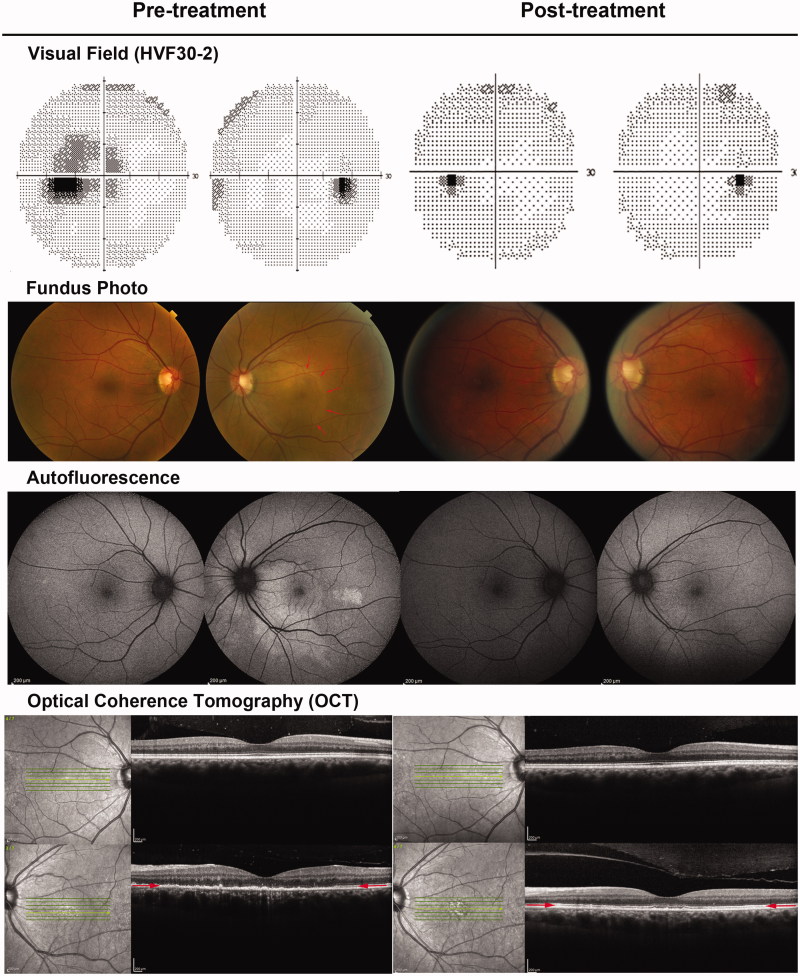
The ocular examination revealed the best-corrected visual acuity of 20/20 in the right eye and 4/200 in the left eye. He read 11/11 in the right eye and 0/11 in the left on Ishihara color plate. The pupils constricted briskly to light stimulation; there was no afferent pupil defect. A 30-2 Humphrey visual field (HVF) confirmed a large, relative central scotoma contiguous with the blind spot in the left eye (Figure 1, top row, pre-treatment). There were no cells or other signs of inflammation in the anterior chamber or vitreous cavity. On dilated fundus examination, the left fundus exhibited a faint, yellowish, well-demarcated round area of hypopigmentation in the posterior pole including the macula and the optic nerve head (Figure 1, second row, pre-treatment, red arrows). The affected area demonstrated increased autofluorescence (Figure 1, third row, pre-treatment). The retinal fluorescein angiography showed mild late-stage patchy hyperfluorescence corresponding to the retinal lesion. Spectral-domain optical coherence tomography (SD-OCT; SPECTRALIS; Heidelberg Engineering, Heidelberg, Germany) of the macula of the left eye revealed disruption of the normally identifiable photoreceptor inner-outer segment (IS/OS) junction and irregular, granular hyper-reflectivity of the retinal pigment epithelium (RPE) (Figure 1, bottom row, pre-treatment, red arrows). The ocular findings were suggestive of chorioretinitis.
FIGURE 1.
Pre- and post-treatment visual fields, fundus photos, retinal autofluorescence, and OCT. On presentation, the patient had a large, relative central scotoma contiguous with the blind spot in the left eye on visual field testing (top row, pre-treatment). The dilated fundus examination revealed a faint, yellowish, well-demarcated round area of hypopigmentation in the posterior pole including the macula and the optic nerve head (second row, pre-treatment, red arrows). The affected area demonstrated increased autofluorescence (third row, pre-treatment). The OCT of the affected area revealed disruption of the normally identifiable photoreceptor inner-outer segment (IS/OS) junction and irregular, granular hyper-reflectivity of the retinal pigment epithelium (bottom row, pre-treatment, red arrows). These abnormalities all resolved after treatment (post-treatment).
Further investigation revealed an elevated antinuclear antibody (ANA) titre of 1:160 and Lyme antibody of 1.65 (0–1.2) Lyme Index Value (LIV), as well as a reactive rapid plasma regain (RPR) with titre of 1:256. The complete blood count and differential (CBCD), liver and renal functions, electrolytes, and angiotensin-converting enzyme (ACE) were within normal limits; human immunodeficiency virus (HIV 1 and 2) antibodies were non-reactive. Confirmatory testing showed a negative Smith antibody (for lupus), a negative Lyme immunoglobulin G/immunolglobulin M (IgG/IgM; Western blot), but a reactive Treponema pallidum particle agglutination assay (TP-PA), consistent with a diagnosis of ocular syphilis. A lumbar puncture revealed nucleated cells of 5/μL (55% of neutrophils, 39% of lymphocytes, 5% of macrophage), red cells of 10,400/μL, protein of 53 (15–45) mg/dL, and glucose of 57 (45–80) mg/dL. On further questioning, the patient described multiple sexual partners within the past year, both male and female.
The patient was treated for neuro-syphilis with intravenous infusion of penicillin G 24 million units once a day for 14 days, followed by one dose of intramuscular injection of benzathine penicillin 2.4 million units. The patient noted steady improvement in his vision a few days after the treatment was started. At last visit, 9.5 weeks after presentation, the patient’s best-corrected acuity in the left eye was 20/20−2; the color vision was 11/11 on Ishihara plate. The central scotoma was completely resolved (Figure 1, top row, post-treatment). The hypopigmentation lesion as well as abnormal autofluorescence on fundus examination resolved (Figure 1, second and third rows, post-treatment). Improvement was also seen on follow-up SD-OCT with visualization of the IS/OS junction, as well as resolution of the irregular, granular hyper-reflectivity of the RPE (Figure 1, bottom row, post-treatment). A repeat serology showed a reactive RPR with titre of 1:8.
Acquired syphilis is a sexually transmitted disease caused by the spirochete Treponema pallidum. Ocular syphilis is a relatively uncommon manifestation of T. pallidum infection and usually occurs in the secondary and tertiary stages of syphilis and can present as a variety of ocular pathologies, including chancre of the eyelid, conjunctivitis, scleritis, uveitis, chorioretinitis, and optic neuritis.1–6 The diagnosis of syphilis is based upon non-specific serologic tests such as Venereal Disease Research Laboratory test (VDRL) and RPR, and confirmatory treponemal tests such as the fluorescent treponemal antibody absorption (FTA-ABS) test and the microhemagglutination–T. pallidum (MHA-TA) test. Patients presenting with ocular syphilis need to have cerebrospinal fluid examination for central nervous system syphilis.2 Parenteral penicillin G is the mainstay of treatment for all stages of syphilis; duration of treatment is dictated by the stage of the disease and various host factors.7
Our patient presented with ocular findings consistent with acute syphilitic posterior placoid chorioretinopathy (ASPPC).8 ASPPC is characterized by the presence of placoid, yellowish, outer retinal lesions associated with varying degree of ocular inflammation. Visual acuity at presentation ranges from 20/20 to counting finger, with a median of 20/80. Visual loss improves shortly after antibiotic treatment to a median of 20/25.9 Retinal fluorescein angiography (FA) shows hypofluorescence in early stage and hyperfluorescence in late stage in the area corresponding to the placoid lesions.9 OCT has been increasingly used to provide additional information regarding the underlying pathologic process. Disruption of the inner/outer photoreceptor segment (IS/OS) junction, thickening and granular hyper-reflectivity of the RPE and loss of choroidal vascular detail are common OCT findings.9,10 The ophthalmoscopic, angiographic, and OCT findings in ASPPC seem to suggest a pathophysiologic process of active inflammatory reaction at the level of the choriocapillaris-RPE-retinal photoreceptor complex.
Although an exclusive retinal disorder, patients with ASPPC can present to neuro-ophthalmologists when subtle retinal changes are overlooked in their initial ophthalmologic evaluation, such as in our patient’s case. Awareness of this condition among neuro-ophthalmologists is important for prompt diagnosis and institution of antibiotic therapy, since both visual dysfunction and structural abnormalities can be reversed by appropriate treatment.
Declaration of interest. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- 1.Aldave AJ, King JA, Cunningham ET. Ocular syphilis. Curr Opin Ophthalmol 2001;12:433–441 [DOI] [PubMed] [Google Scholar]
- 2.Karunaratne I, Sharma S, Dick A, Carrington D, Horner P. Shared care approach to managing ophthalmological disease in patients with positive treponemal serology: a case series. Int J STD AIDS 2012;23:291–296 [DOI] [PubMed] [Google Scholar]
- 3.Weinstein JM, Lexow SS, Ho P, Spickards A. Acute syphilitic optic neuritis. Arch Ophthalmol 1981;99:1392–1395 [DOI] [PubMed] [Google Scholar]
- 4.Jegerlehner S, Vogel D, Tappeiner C, Leib SL. [What vision loss might bring to light]. Praxis 2012;101:419–423 [DOI] [PubMed] [Google Scholar]
- 5.Cillino S, Di Pace F, Trizzino M, Li Vecchi V, Di Carlo P. Chancre of the eyelid as manifestation of primary syphilis, and precocious chorioretinitis and uveitis in an HIV-infected patient: a case report. BMC Infect Dis 2012;12:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang SW, Kang JH, Chun JS, Seo JK, Kim HW, Lee D, Sung HS. A case of syphilitic keratoderma concurrent with syphilitic uveitis. Ann Dermatol 2009;21:399–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention 1998 guidelines for treatment of sexually transmitted diseases. MMWR Recomm Rep 1998;47:1–111 [PubMed] [Google Scholar]
- 8.Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 1990;97:1288–1297 [DOI] [PubMed] [Google Scholar]
- 9.Eandi CM, Neri P, Adelman RA, Yannuzzi LA, Cunningham ET Jr, International Syphilis Study Group Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina 2012;32:1915–1941 [DOI] [PubMed] [Google Scholar]
- 10.Pichi F, Ciardella AP, Cunningham ET Jr, Morara M, Veronese C, Jumper JM, Albini TA, Sarraf D, McCannel C, Voleti V, Choudhry N, Bertelli E, Giuliari GP, Souied E, Amer R, Regine F, Ricci F, Neri P, Nucci P. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina 2014;34:373–384 [DOI] [PubMed] [Google Scholar]