Abstract
The purpose of this study was to present three cases of Saturday night retinopathy. The study design was observational case series. We described three cases who presented to our centre with acute visual loss following intravenous drug abuse and stupor leading to continuous pressure on the orbit while asleep. All cases presented with acute vision loss and had funduscopic evidence of ophthalmic or central retinal artery occlusion. Two of the cases presented with ophthalmoplegia and proptosis. One of the cases had significantly increased intraocular pressure with corneal oedema. All cases had fixed and non-reactive pupils with significant relative afferent pupillary defect. One case also had accompanying peroneal nerve damage. All three cases had poor visual outcomes. Saturday night retinopathy is a blinding condition with either central retinal or ophthalmic artery occlusion, which may present with transient orbital congestion and ophthalmoplegia. It may be accompanied by other nerve damage from compression in other parts of the body and is caused by prolonged positional pressure on the orbit.
Keywords: Ophthalmoplegia, retinal artery occlusion, saturday night retinopathy
INTRODUCTION
In 1974, Jayam et al.1 reported a unique case of unilateral ischaemic retinopathy in association with peroneal palsy in the setting of stupor leading to continuous pressure on the orbit while asleep. They called it “Saturday night retinopathy,” as it had happened following heavy alcohol and possibly methadone abuse at a party. Although the pathophysiology is presumed to be similar to cases of central retinal artery occlusion from direct pressure on the eye as a complication of surgical positioning, cases with this aetiology are extremely rare. We hereby present a series of three of these rare cases, two of which had accompanying ophthalmoplegia.
methods
This is a retrospective observational case series approved by the institutional review board at New Jersey Medical School, Rutgers.
RESULTS
Case 1
An 18-year-old male was referred to our centre with 3 days of acute visual loss in his right eye. He had a history of intravenous (IV) drug abuse, and had used IV heroin just before he passed out and awoke about 12 hours later with a red, painful blind eye. He said he had fallen asleep face down and on his right side, and that he also had difficulty moving his right foot with numbness on its dorsal aspect since the incident. He had no other past ocular or medical history. Upon examination, he had acuities of no light perception (NLP) OD and 20/20 OS; Ishihara plates were all correct OS. The right pupil was 6 mm and fixed and non-reactive to either ipsilateral or contralateral light or near stimulation, with a +4 relative afferent pupillary defect (RAPD) OD. The left pupil was normally reactive. There was swelling, tenderness, and erythaema without warmth of the right eyelids with 3 mm of proptosis and chemosis. The motility of the right eye showed complete ophthalmoplegia and ptosis of the right eye; the lid and motility were normal OS. Forced ductions could not be performed due to significant eyelid tenderness and swelling. The rest of the cranial nerve examination was normal. No orbital bruit was audible. The slit-lamp examination was normal on both sides except for the chemosis of the right conjunctiva. Intraocular pressure (IOP) was 19 mm Hg in the right eye and 13 mm Hg in the left eye. The fundus examination of the right eye revealed significant pallor of the retina, most notable in the posterior pole, with a cherry-red spot, engorgement of veins and perfused, albeit attenuated arteries, and very mild hyperaemia of the optic disc (Figure 1). Fluorescein angiography confirmed the presence of ophthalmic artery occlusion, with significantly delayed and decreased perfusion of the choroid and retinal circulation (Figure 2). Optical coherence tomography (OCT) of the retina confirmed significant swelling of the entire retina (Figure 3). Magnetic resonance imaging (MRI) revealed engorgement of the right extraocular muscles and lacrimal gland, normal optic nerve, superior ophthalmic vein, and intact cavernous sinus (Figure 4). The diagnosis of Saturday night retinopathy with orbitopathy and complete ophthalmoplegia was made. The patient underwent evaluation for carotid, cardiac, or hypercoagulable aetiologies for the occlusions, all of which were negative. He did not return for follow-up; but upon further telephone follow-up 2 weeks later, he stated that the eyelid swelling and tenderness had significantly improved, along with some limited eye movement, but he was still NLP. Of note, the right foot paresis had completely resolved.
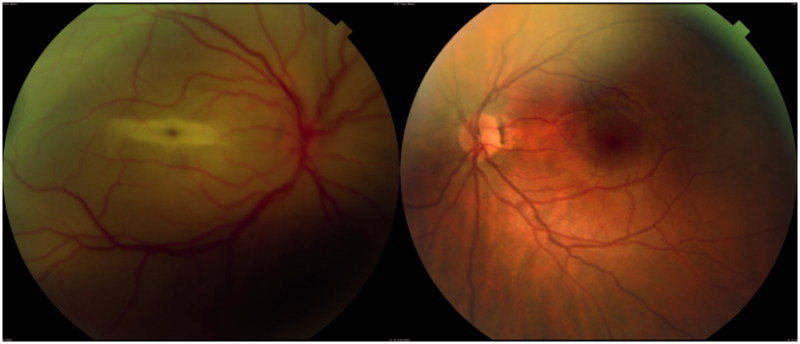
FIGURE 1.
Case 1—3 days after visual loss. (Left) Fundus examination of the right eye revealed significant pallor of the fundus, most notable in the posterior pole, cherry-red spot, engorgement of veins and attenuation of arteries, and slight hyperaemia of the optic disc. (Right) Normal left eye.
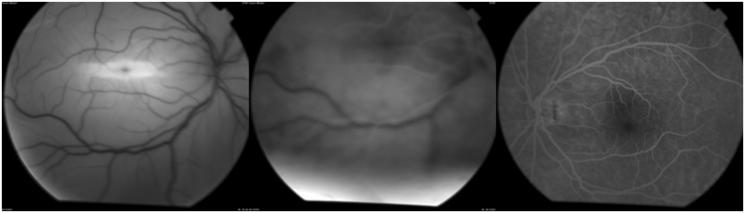
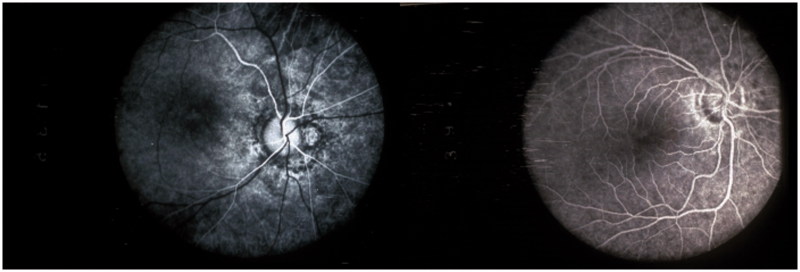
FIGURE 2.
Case 1—3 days after visual loss. (Left) Red free fundus photo, right eye. (Middle) Fluorescein angiography of the right eye at approximately 45 seconds following dye injection confirmed the presence of what had been complete ophthalmic artery occlusion, with significantly delayed and decreased perfusion of the choroid and retinal circulation. (Right) Normal left eye.
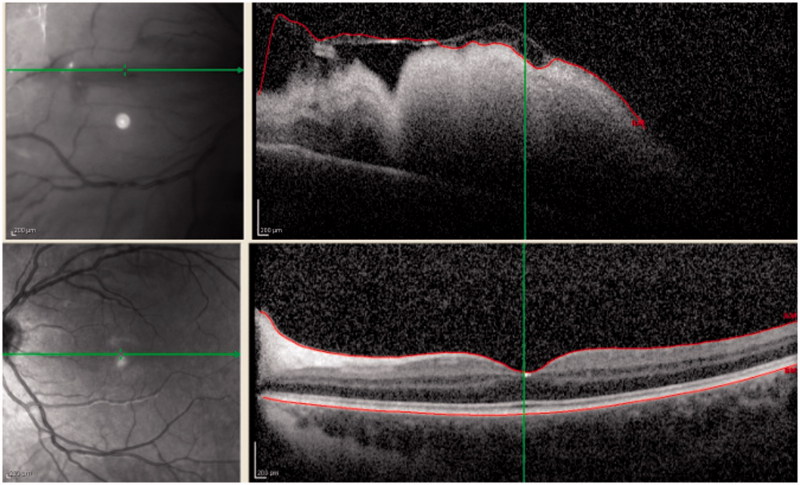
FIGURE 3.
Case 1—3 days after visual loss. OCT of the retina confirmed significant swelling of entire retinal thickness in the right eye extrafoveally (top); normal left eye in the macular area (bottom).
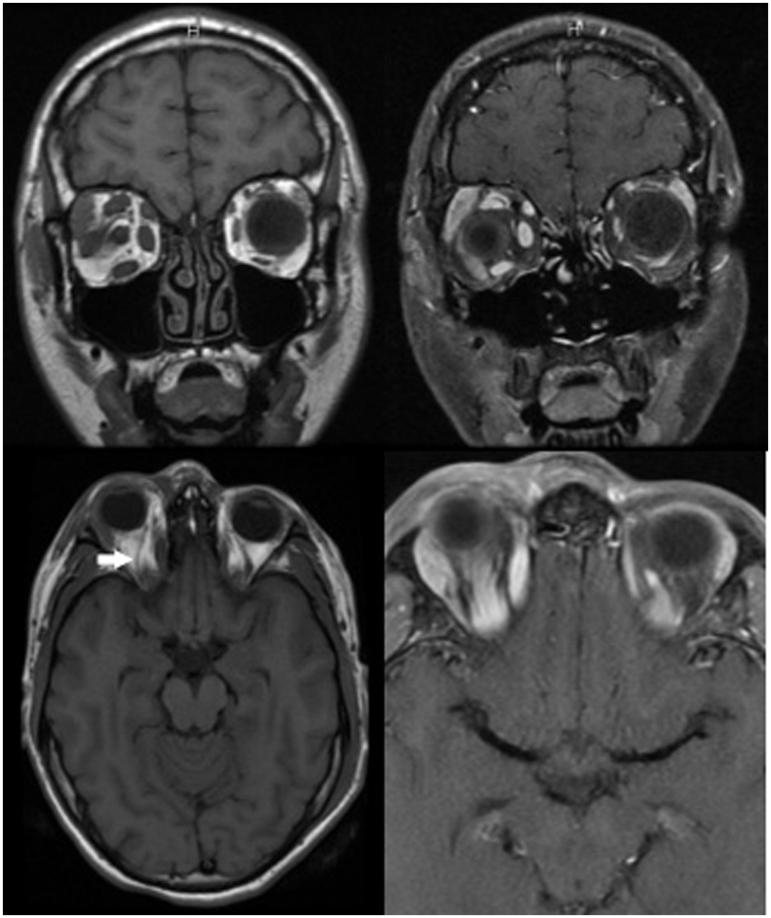
FIGURE 4.
Case 1—3 days after visual loss. MRI of orbit revealed engorgement of right extraocular muscles and lacrimal gland. (Top left) Coronal T1. (Top right) Coronal T1 with contrast. (Bottom left) Axial T1. Note normal size of right superior ophthalmic vein (arrow). (Botton right) Axial T1 with contrast.
Case 2
A 32-year-old woman was referred with a history of 4 days of loss of vision OD. She had a history of manic depressive illness and IV drug abuse; she had been tested for human immunodeficiency virus (HIV) 4 weeks before and was negative. She said she last injected drugs 5 days before, passed out, and awoke blind in the right eye. She said that she had fallen asleep on the edge of her kitchen sink, with her right eye down. There was no other ocular history, and she thought that her vision had only slightly improved over the 4 days since her symptoms started. Her examination showed acuities of hand motion (HM) OD, 20/30 OS, with Ishihara plates 0/10 OD, 10/10 OS. The pupils were 4/4, sluggish OD, with a +3 RAPD OD. There was a 3 mm of proptosis OD with normal retropulsion. The motility showed 2+ underaction (UA) of right medial rectus and lateral rectus OD, 4+ UA in upgaze, trace UA in downgaze; the OS was normal (Figure 5). There was no restriction on forced duction. The rest of the cranial nerves were normal. The slit-lamp examination was normal (no conjunctival injection or chemosis), and no bruits were audible. The fundus was normal OS, the right eye showed the residua of a cherry-red spot, with pallid oedema in the maculopapillary bundle; the disc and retina were perfused. The MRI was normal; the electroretinogram (ERG) was flat OD, indicating ophthalmic artery occlusion, supporting the diagnosis of Saturday night retinopathy with ophthalmoplegia. Fluorescein angiography revealed significantly delayed and decreased perfusion of the choroid and retina (Figure 6). Upon follow-up a month later, the patient had developed the characteristic retinal pigment epithelium changes of ophthalmic artery occlusion (Figure 7).
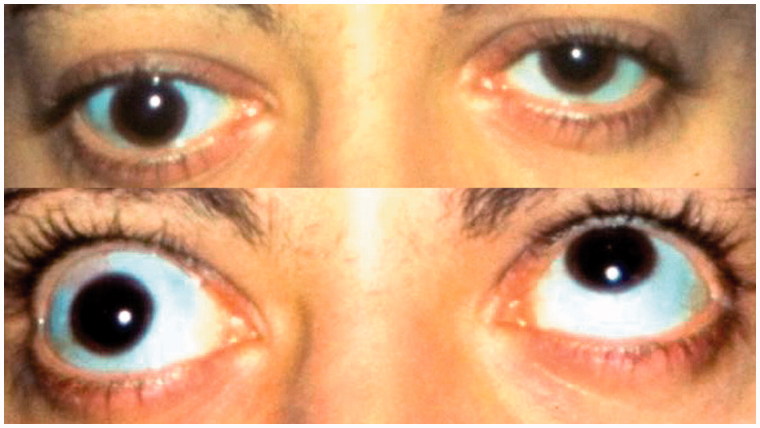
FIGURE 5.
External photograph of patient (case 2) showing proptosis and 4+ underaction in upgaze, OD; OS was normal. Four days after visual loss. (Top) Primary gaze. (Bottom) Upgaze.
FIGURE 6.
Case 2—4 days after visual loss. Fluorescein angiography of right eye reveals the presence of ophthalmic artery occlusion, with significantly delayed and decreased perfusion of the choroid and retinal circulation.
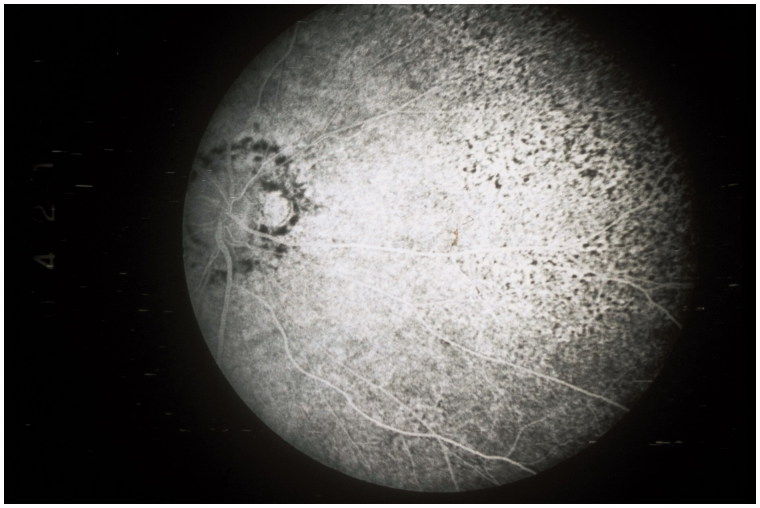
FIGURE 7.
Case 2. Retinal pigment epithelial changes seen 1 month after presentation in the nasal periphery of the fundus further indicate that the ophthalmic artery was involved.
Case 3
A 33-year-old male with a history of IV drug abuse presented with a 3-hour history of acute visual loss and pain and redness in the right eye. He had used IV heroin in the morning and had fallen sleep in a prone position in bed for about 12 hours, and woke up with painful visual loss OD. He did not have any other medical or ocular history. Upon examination about an hour after arrival at the emergency room, he had acuities of light perception (LP) OD and 20/20 OS; Ishihara plates were 0/10 OD, 10/10 OS. The right pupil was 6 mm and fixed and non-reactive to either ipsilateral or contralateral stimulation, with a +3 RAPD OD. The left pupil was normally reactive. The external eye examination and ocular motility were entirely normal in both eyes. The slit-lamp examination revealed moderate right conjunctival injection without chemosis and corneal epithelial oedema, and was normal in the left eye. IOP was >60 mm Hg OD and 15 mm Hg OS. Gonioscopy of both eyes showed grade IV open angles in both eyes, although the view was mildly hazy in the right eye due to the presence of corneal oedema. The fundus examination of the right eye revealed a pale non-perfused retina, most notable in the posterior pole, with a cherry-red spot without emboli. The left fundus was normal. The patient was immediately started on topical timolol/dorzolamide and brimonidine OD every 5 minute for three times OD) and was given IV acetazolamide (250 mg once) for the elevated pressure. He was offered anterior chamber paracentesis, but declined. About 45 minutes later, his IOP had dropped to 42 mm Hg, and his vision had improved to hand motion (HM). At this point he became verbally aggressive with the emergency staff and left the hospital against the medical advice, and he was lost to follow-up.
DISCUSSION
Jayam et al.1 reported a 17-year-old male who had ingested an unknown quantity of methadone along with approximately a pint and half of wine at a birthday party, leading to stupor. He was put on a bed, from which he fell off and was unresponsive for 6–7 hours. He presented with “total blindness” of the left eye, pain, proptosis, ophthalmoplegia, and diffuse retinal oedema along with left peroneal nerve palsy. The ERG was extinguished, showing no response under either light- or dark-adapted conditions. Orbital venogram showed bilateral normal ophthalmic veins, and carotid studies and ophthalmodynamometry were normal bilaterally. The pain and tenderness of the orbit, proptosis, and left peroneal palsy improved significantly in the next couple of weeks, but he remained blind. They called the entity “Saturday night retinopathy.”1
Our first and second cases are similar to their original case. Our first case had blindness, proptosis, and ophthalmoplegia, with extraocular muscle and lacrimal gland enlargement, presumably from venous congestion, on MRI following heroin use. As did Jayam et al.’s case, our patient also had peroneal nerve palsy ipsilateral to the involved eye.1 Our second case had loss of vision from ophthalmic artery occlusion, with proptosis and ophthalmoplegia while in an inebriated state and sleeping on the eye. Jayam et al.1 proposed that these findings were caused by an acute rise in orbital cavity pressure caused by direct compression of the orbit for a prolonged period when the patient falls sleep on it in a stuporous state. This can lead to venous stasis, decreased perfusion pressure, and ultimately closure of ophthalmic artery. Orbital tissues may become oedematous, swollen, and tender, leading to painful proptosis, and intraorbital cranial nerves may be damaged. That these cases were ophthalmic rather than central retinal artery occlusion (CRAO) is evidenced by that the vision was worse than is typically seen in a CRAO, by the fluorescein angiography findings, which acutely show decreased perfusion to the choroid in addition to the retina. Further support includes that the ERG showed involvement of both a and b waves, indicative of both inner and outer retinal involvement as opposed to in CRAO, where the a wave is spared, indicative of photoreceptor sparing. Furthermore, case 1 showed more diffuse retinal swelling on OCT, and case 2 showed the development of retinal pigment epithelial abnormalities typical of ophthalmic artery occlusion (Figure 7).
Our third case presented with an acute rise in intraocular pressure, corneal oedema, central artery occlusion, and minimal orbital findings. Unfortunately, the patient left the hospital before any diagnostic test could be performed to better identify the nature of his arterial occlusion. However, it can be postulated that direct continuous pressure on the eye caused intraocular pressure to continuously exceed central retinal artery perfusion pressure and thus CRAO. As the pressure is relieved and intraocular pressure decreases, the retinal perfusion improves (allowing for the mild improvement of vision in our case), but the retinal tolerance time for irreversible functional loss after a period of hypoxia (around 100 minutes) was most likely exceeded.2 The lack of orbital symptoms (e.g., proptosis and ophthalmoplegia) in our third case can be explained by his moving and thereby relieving the orbital compression after a shorter period of time than in the other two cases. The congestion in this syndrome may be explained by either the mechanism of direct compression and congestion, or, as Hollenhorst et al. described, that both orbital veins and arteries may be occluded by external pressure,3 and with release of the pressure, the orbital veins and arteries decompress, resulting in orbital oedema, proptosis, and ophthalmoplegia. This process may take a few hours, so if the patient is seen in the early hours after awakening with release of external pressure, the orbital oedema may not manifest.
Different clinical entities with components of pathophysiology similar to this diagnosis have been well documented in the literature.3–9 Intraoperative loss of vision may be due to CRAO or ophthalmic artery occlusion from direct pressure on the globe such as may be caused by a headrest.10 Perioperative visual loss, typically an ischaemic optic neuropathy, may have attendant orbital congestion and has prolonged prone positioning without direct pressure on the eye as a major risk factor, and may be a compartment syndrome. Saturday night retinopathy, however, happens out of the hospital, and there is no realistic preventive measure to be implemented in the patient population at risk, although family education can potentially be of some value. Awareness of health care professionals and emergency medical services with this entity may help them better understand this clinical scenario. Unfortunately, no treatment has proven to be of significant clinical benefit.11–14
Saturday night retinopathy is a blinding condition with either central retinal or ophthalmic artery occlusion, which may have with transient orbital congestion and ophthalmoplegia. It may be accompanied by other nerve damage from compression in other parts of the body and is caused by prolonged positional pressure on the orbit. Prolonged periods of altered mental status inhibit spontaneous movements, which would ordinarily alleviate the focal compression during normal sleep.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Note: Figures 1, 3, 5, 6, and 7 are available in colour online at http://informahealthcare.com/oph.
References
- 1.Jayam AV, Hass WK, Carr RE, Kumar AJ. Saturday night retinopathy. J Neurol Sci 1974;22:413–418 [DOI] [PubMed] [Google Scholar]
- 2.Hayreh SS, Kolder HE, Weingeist TA. Central retinal artery occlusion and retinal tolerance time. Ophthalmology 1980;87:75–78 [DOI] [PubMed] [Google Scholar]
- 3.Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical operations. AMA Arch Ophthalmol 1954;52:819–830 [DOI] [PubMed] [Google Scholar]
- 4.Montero JA, Ruiz-Moreno JM, Galindo A, Fernandez-Munoz M. Release hallucinations and visual loss as first manifestations of postoperative unilateral blindness. Eur J Ophthalmol 2007;17:844–846 [DOI] [PubMed] [Google Scholar]
- 5.Givner I, Jaffe N. Occlusion of the central retinal artery following anesthesia. Arch Ophthalmol 1950;43:197–201 [DOI] [PubMed] [Google Scholar]
- 6.Ooi EI, Ahem A, Zahidin AZ, Bastion ML. Unilateral visual loss after spine surgery in the prone position for extradural haematoma in a healthy young man. BMJ Case Rep 2013;2013. pii: bcr2013200632. doi: 10.1136/bcr-2013-200632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossman W, Ward WT. Central retinal artery occlusion after scoliosis surgery with a horseshoe headrest. Case report and literature review. Spine 1993;18:1226–1228 [DOI] [PubMed] [Google Scholar]
- 8.Katz DA, Karlin LI. Visual field defect after posterior spine fusion. Spine 2005;30:E83–E85 [DOI] [PubMed] [Google Scholar]
- 9.Kumar N, Jivan S, Topping N, Morrell AJ. Blindness and rectus muscle damage following spinal surgery. Am J Ophthalmol 2004;138:889–891 [DOI] [PubMed] [Google Scholar]
- 10.Slocum HC, O'Neal KC, Allen CR. Neurovascular complications from malposition on the operating table. Surg Gynecol Obstet 1948;86:729–734 [PubMed] [Google Scholar]
- 11.Ahn SJ, Kim JM, Hong JH, Woo SJ. Efficacy and safety of intra-arterial thrombolysis in central retinal artery occlusion. Invest Ophthalmol Vis Sci 2013;54:7746–7755 [DOI] [PubMed] [Google Scholar]
- 12.Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond) 2013;27:688–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cugati S, Varma DD, Chen CS, Lee AW. Treatment options for central retinal artery occlusion. Curr Treat Options Neurol 2013;15:63–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy-Lavoie H, Butler F, Hagan C. Central retinal artery occlusion treated with oxygen: a literature review and treatment algorithm. Undersea Hyperb Med 2012;39:943–953 [PubMed] [Google Scholar]