ABSTRACT
Background
These trials are the first randomised controlled trials of telephone-based weight management and healthy lifestyle interventions for low back pain and knee osteoarthritis. This article describes the protocol and statistical analysis plan.
Method
These trials are parallel randomised controlled trials that investigate and compare the effect of a telephone-based weight management and healthy lifestyle intervention for improving pain intensity in overweight or obese patients with low back pain or knee osteoarthritis. The analysis plan was finalised prior to initiation of analyses. All data collected as part of the trial were reviewed, without stratification by group, and classified by baseline characteristics, process of care and trial outcomes. Trial outcomes were classified as primary and secondary outcomes. Appropriate descriptive statistics and statistical testing of between-group differences, where relevant, have been planned and described.
Conclusions
A protocol for standard analyses was developed for the results of two randomised controlled trials. This protocol describes the data, and the pre-determined statistical tests of relevant outcome measures. The plan demonstrates transparent and verifiable use of the data collected. This a priori protocol will be followed to ensure rigorous standards of data analysis are strictly adhered to.
Keywords: low back pain, knee osteoarthritis, lifestyle, telephone, randomised controlled trial, statistical analysis plan
BULLET POINTS
Lifestyle factors such as overweight and obesity are associated with low back pain and osteoarthritis. However, accessible interventions aiming to support patients with low back pain or osteoarthritis to manage lifestyle factors have not been tested in high quality trials.
The two trials determine the effectiveness of telephone-based healthy lifestyle interventions for low back pain and osteoarthritis of the knee.
This protocol comprehensively describes key trial methodology relating to data capture, management and pre-determined statistical analyses.
Such protocols are important in raising the validity of physical therapy research as they demonstrate transparent and verifiable use of the data collected and ensure rigorous standards of data analysis are strictly adhered to.
Introduction
This protocol describes the first randomised controlled trials (RCT) of telephone-based weight management and healthy lifestyle interventions for low back pain and knee osteoarthritis. Here we describe the protocol and pre-determined statistical analysis plan, for both trials (trial one: low back pain and trial two: knee osteoarthritis). The protocol and statistical analysis plan was finalised prior to analysing the data and will be adhered to in analysing the data from the trials. All study investigators signed and approved the statistical analysis plan in May 2016. Participant recruitment for both trials was completed in October 2015, and final participant follow-up was completed in May 2016. Following data integrity checks the database will be locked (June 2016). The statistical analyses specified in the statistical analysis plan will be performed in June 2016.
Study overview
Study design and setting
These trials were established as part of a cohort multiple RCT design 1 , whereby participants from our existing cohort of patients referred for an outpatient orthopaedic consultation at a public tertiary referral hospital within NSW Australia, were randomised to be offered a new clinical intervention (intervention group) or remain as part of the cohort (control group). Both trials were prospectively registered with the Australian New Zealand Clinical Trials Registry (trial one: ACTRN12615000478516, and trial two: ACTRN12615000490572) and full study protocols for each trial have been published elsewhere 2 , 3 . These trials were approved by the Hunter New England Health Human Research Ethics Committee (13/12/11/5.18), Wallsend NSW, Australia and the University of Newcastle Human Research Ethics Committee (H-2015-0043), Newcastle, Australia.
Participants and recruitment
Patients with non-specific low back pain (trial one, n=160) or knee osteoarthritis (trial two, n=120) were recruited. Participants in the intervention group of both trials were provided with brief advice and education about the benefits of weight loss and physical activity for their conditions by trained telephone interviewers. Additionally, participants in the intervention group of trial one (low back pain) were provided with an initial consultation with the study physical therapist. The consultation involved a low back pain clinical assessment and detailed low back pain education based on clinical practice guidelines. Behavioural change techniques were also utilised to support a healthy lifestyle and weight management for low back pain. There was no baseline clinical assessment for participants of trial two (knee osteoarthritis).
Following baseline data collection, participants in the intervention groups of both trials were referred to the NSW Get Healthy Information and Coaching Service (GHS). The GHS is a free, telephone-based government funded service to support individuals to modify their eating behaviours, increase their physical activity, reduce alcohol consumption and achieve or maintain a healthy weight 4 . The GHS has been shown to be effective in the general population and involves 10 individually tailored coaching calls delivered over a 6-month period by a university-qualified health professional. The support provided is based on national guidelines and utilises motivational interviewing 4 . All health coaches were provided with training by a study investigator (CW) in evidence-based management for low back pain and knee osteoarthritis.
Participants in the control group received any usual care offered to them by their treating clinician during the six month intervention period, and participated in data collection. Follow-up lasted for 26 weeks (6 months).
Inclusion/exclusion criteria
Patients were eligible for inclusion in the trials if all of the following criteria were met:
-
•
Trial one condition definition: chronic low back pain defined as pain in the lower back (i.e. between the 12th rib and buttock crease) with/without leg pain and duration of longer than 3 months since the onset of pain 5 ;
-
•
Trial two condition definition: complaint of pain in the knee due to knee osteoarthritis (as per referral) lasting longer than 3 months;
-
•
Aged 18 years or older;
-
•
Classified as overweight or obese with a self-reported body mass index (BMI) ≥27kg/m2 and <40kg/m2;
-
•
Have access to and can use a telephone; and
-
•
Have back or knee pain, for each trial respectively, severe enough to cause at least average pain intensity ≥3 of 10 on a 0–10 numerical rating scale (NRS) 6 in the last week or moderate level of interference in activities of daily living (adaptation of item 8 on SF36) 7 .
Patients were excluded if they met the following criteria:
-
•
Known or suspected serious pathology as the underlying cause of back pain or knee osteoarthritis, for each trial respectively, (e.g. fracture, cancer, infection, inflammatory arthritis, infection, cauda equine syndrome);
-
•
A previous history of obesity surgery;
-
•
Current participation in any prescribed, medically supervised or commercial weight loss program;
-
•
Back or knee surgery, for each trial respectively, in the last 6 months or booked in for surgery in the next 6 months;
-
•
Unable to walk unaided;
-
•
Unable to comply with the study protocol that requires them to, adapt meals or exercise, due to non-independent living arrangements;
-
•
Any medical or physical impairment, apart from back pain or knee osteoarthritis for each trial respectively, precluding safe participation in exercise such as uncontrolled hypertension, or morbid obesity (BMI≥40); and
-
•
Unable to speak and read English sufficiently to complete the study procedures.
Unblinding
The analysis plan was written and approved prior to analysis of data and blind to group status. Dummy coded variables representing group allocation will be used to ensure blinding of statistician(s) undertaking the analysis.
Objectives
The primary objective of both trials is to establish if:
Trial one: pain education and referral to a telephone-based weight management and healthy lifestyle intervention improves pain intensity in patients with low back pain, who are overweight or obese, compared to usual care.
Trial two: referral to a telephone-based weight management and healthy lifestyle intervention improves pain intensity in patients with knee osteoarthritis, who are overweight or obese compared to usual care.
Secondary aims of the two trials is to establish if the telephone interventions lead to reductions in disability, weight, BMI, waist circumference, alcohol consumption, and smoking prevalence, and improvement in quality of life, emotional distress, sleep quality, physical activity, diet, pain attitudes and beliefs, perceived change in condition and change in health care and medication use.
A separate analysis plan will be detailed for health economic analyses and is not included in this manuscript.
Definition of outcome variables
Participant demographics and baseline characteristics
Baseline data includes: age, gender, Aboriginal and/or Torres Strait Islander status, employment status, country of origin, highest level of education, health insurance status, other co-existing medical conditions needing medication, and pain duration (how long have you been troubled with your pain). Length of time waiting for consultation (days) and triage classification will be obtained from hospital records. In Australia, patients referred for orthopaedic consultation are categorised according to urgency of consultation: urgent – to be seen within 30 days; semi-urgent – to be seen within 90 days; and non-urgent – to be seen within 12 months 8 . See Table 1 for details.
Table 1. Demographic and baseline characteristics.
| Intervention | Control | |
|---|---|---|
| Demographic | ||
| Age (years) | mean (SD) | mean (SD) |
| Gender (male) | n/N (%) | n/N (%) |
| Aboriginal and/or Torres Strait Islander status | n/N (%) | n/N (%) |
| Employment status | ||
| Employed | n/N (%) | n/N (%) |
| Unemployed | n/N (%) | n/N (%) |
| Retired | n/N (%) | n/N (%) |
| Can’t work (health reasons) | n/N (%) | n/N (%) |
| Country of origin (Australia) | n/N (%) | n/N (%) |
| Highest level of education | ||
| >High school | n/N (%) | n/N (%) |
| Private health insurance | n/N (%) | n/N (%) |
| Other co-existing medical conditions needing medication | n/N (%) | n/N (%) |
| Length of time waiting for consultation (days) | mean (SD) | mean (SD) |
| Triage classification | ||
| Non-urgent | n/N (%) | n/N (%) |
| Semi-urgent | n/N (%) | n/N (%) |
| Baseline characteristics | ||
| Pain intensity (NRS) | mean (SD) | mean (SD) |
| Pain duration (how long have you been troubled with your pain) | mean (SD) | mean (SD) |
| Disability and function (Trial 1: RMDQ / Trial 2: WOMAC) | mean (SD) | mean (SD) |
| Subjective weight | mean (SD) | mean (SD) |
| BMI | mean (SD) | mean (SD) |
| Quality of Life (SF12.v2) | ||
| Physical component score (PCS) | mean (SD) | mean (SD) |
| Mental component score (MCS) | mean (SD) | mean (SD) |
| Emotional distress (DASS-21) | mean (SD) | mean (SD) |
| Poor sleep quality (item 6, Pittsburgh Sleep Quality Index) | n/N (%) | n/N (%) |
| Physical activity (mins MVPA/week) | mean (SD) | mean (SD) |
| Diet | ||
| Fruit (serves) | n/N (%) | n/N (%) |
| Vegetables (serves) | n/N (%) | n/N (%) |
| Discretionary foods (serves) | n/N (%) | n/N (%) |
| Alcohol consumption (AUDIT) | mean (SD) | mean (SD) |
| Smoking prevalence | n/N (%) | n/N (%) |
| Pain attitudes (SOPA) | mean (SD) | mean (SD) |
| Fear avoidance beliefs (FABQ) | mean (SD) | mean (SD) |
| Health care utilisation | ||
| Medication use for back or knee pain | n/N (%) | n/N (%) |
| Visits for back or knee pain | n/N (%) | n/N (%) |
NRS=numerical rating scale; RMDQ=Roland Morris Disability Questionnaire; WOMAC=Western Ontario and McMaster Universities Index; BMI=Body Mass Index; SF12.v2= Short Form Health Survey version 2; PCS=Physical Component Score; MCS=Mental Component Score; 21=Depression Anxiety Stress Scale; MVPA=Moderate-to-Vigorous Physical Activity; AUDIT=Alcohol Use Disorders Identification Test; SOPA=Survey of Pain Attitudes; FABQ=Fear Avoidance Beliefs Questionnaire.
Primary outcome
The primary outcomes are average weekly back pain intensity (trial one) and average weekly knee pain intensity (trial two), measured over the course of follow up.
Participants were asked to report the “average pain intensity experienced in their back (trial one) or knee (trial two) over the past week, on a 0 to 10 NRS, where 0 was ‘no pain’ and 10 was the ‘worst possible pain’” 6 . These pain intensity scores were measured at baseline, at 2, 6, 10, 14, 18, 22 and 26 weeks. Average weekly (back or knee) pain intensity is defined as the Area under the Curve (AUC) of the pain intensity trajectory, over the follow up period. The AUC for each participant will be computed using the trapezoid rule.
Secondary outcomes
The secondary outcomes include:
-
•
Physical disability and function, measured in trial one using the Roland Morris Disability Questionnaire (RMDQ) 9 0-24 scale and measured in trial two using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 0-96 scale 10 ;
-
•
Self-reported weight (kg);
-
•
Objective weight (kg) measured to the nearest 0.1kg by a trained research assistant using International Society for the Advancement of Kinanthropometry (ISAK) procedures 11 ;
-
•
BMI calculated as weight /height squared (kg/m2) 12 ;
-
•
Waist circumference measured by a trained research assistant using ISAK procedures taken at the level of the narrowest point between the inferior rib border and the iliac crest using a flexible tape measure to the nearest 0.1 cm 11 ;
-
•
Quality of life, measured using the physical and mental health component scores from the 12-item Short Form Health Survey version 2 (SF12.v2) 7 ;
-
•
Global perceived change in symptoms, measured using the Global Perceived Effect (GPE) scale (-5 ‘vastly worse’ to 5 ‘completely recovered’) 13 ;
-
•
Emotional distress, measured using the Depression Anxiety Stress Scale-21 (DASS-21) 0-63 scale 14 ;
-
•
Sleep quality, measured using item 6 from the Pittsburgh Sleep Quality Index (response options: very bad, fairly bad, fairly good, very good) 15 ;
-
•
Physical activity, measured using the Active Australia Survey 16 , reported as the average minutes spent participating in moderate-to-vigorous physical activity (MVPA) per week;
-
•
Diet, measured using a short food frequency questionnaire (FFQ) 17 , reported as serves of fruit (0-1, 2 or more), serves of vegetables (0-2, 3-4, 5 or more), serves of discretionary foods including processed meats, salty snacks, takeaway meals, sweet or savoury snacks, confectionary and sugar sweetened beverages (more than once per week, once per week or less);
-
•
Alcohol consumption measured using the Alcohol Use Disorders Identification Test (AUDIT) 0-12 scale 18 ;
-
•
Smoking prevalence (have you smoked any tobacco in the last 4 weeks? (this can include cigarettes, roll your own, pipes, cigars or any other tobacco products)) 19 ;
-
•
Attitudes and beliefs, measured using the Survey of Pain Attitudes (SOPA) 20 ; and the physical component of the Fear Avoidance Beliefs Questionnaire (FABQ) 0-24 scale 21 ; and
-
•
Health care utilisation for each trial respectively, including back or knee pain medication use (name), type of health service utilised for back or knee pain including number of sessions, and attended orthopaedic consultation or received surgery.
See Table 2 for data collection time points for secondary outcomes.
Table 2. Secondary outcome measures.
| Construct | Measurement | Time-point (weeks) |
|---|---|---|
| Disability and function | Trial one: Roland
Morris Disability Questionnaire (RMDQ)
9
Trial two: Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) 10 |
0, 6, 26 0, 6, 26 |
| Subjective weight | Self-reported weight (kg) | 0, 6, 26 |
| Objective weight | Measured to the nearest 0.1kg 11 | 0a, 26 |
| BMI | BMI calculated as weight/height squared (kg/m2) 12 | 0, 6, 26 |
| Waist circumference | Measured to the nearest 0.1cm 11 | 26 |
| Quality of life | Short Form Health Survey version 2 (SF12.v2) 7 | 0, 6, 26 |
| Perceived change in condition | Global Perceived Effect scale (–5 to 5 scale) 13 | 6, 26 |
| Emotional distress | Depression Anxiety Stress Scale-21 (DASS-21) 14 | 0, 26 |
| Sleep quality | Item 6 from the Pittsburgh Sleep Quality Index 15 | 0, 6, 26 |
| Physical activity | The Active Australia Survey 16 | 0, 6, 26 |
| Diet | Short food frequency questionnaire 17 | 0, 6, 26 |
| Alcohol consumption | Alcohol Use Disorders Identification Test (AUDIT) 18 | 0, 6, 26 |
| Smoking prevalence | Self-reported current smoking status 19 | 0, 6, 26 |
| Pain Attitudes | Survey of Pain Attitudes (SOPA) 20 | 0, 6, 26 |
| Fear avoidance beliefs | Fear Avoidance Beliefs Questionnaire (FABQ) 21 | 0, 26 |
| Health care utilisation | Medication use for back
(trial one) or knee pain (trial two) Visits for back (trial one) or knee pain (trial two) – type and number of sessions Attended orthopaedic consultation, received surgery |
0, 6, 26 0, 6, 26 26 |
Intervention group of low back pain patients (trial one) only. BMI: Body Mass Index.
Process variables
Intervention fidelity
Delivery of the intervention is assessed by the GHS, data includes; commencement, the number, length, and timing of coaching calls and achievement of identified goals.
Concomitant treatments
Participants were asked to record separately all medication and health care services used for the back or knee pain, for each trial respectively, at baseline, and weeks 6 and 26 post-randomisation. Information for each additional treatment was provided as free text often using variable terminology. These will be aggregated using a common terminology. Medications will be coded using the Anatomical Therapeutic Chemical Classification System at the third level. Other health services will be coded according to common provider types, for example specialist, hospital or emergency department presentation or admission, physical therapy, chiropractic, massage therapy, other allied health, alternative medicine, and other.
Safety
Participants were monitored for adverse events throughout the intervention period. All adverse events (AE), that is, any new medical conditions or an exacerbation of another existing condition, were recorded at 6 and 26 weeks. All AEs will be described for each group.
Design issues
General design
These trials were parallel group RCTs, established as part of a cohort multiple RCT. Patients waiting for an outpatient orthopaedic consultation at a public tertiary referral hospital within NSW were sent an information letter to invite participation in the cohort (telephone survey) and again at 12-months follow-up. At 12-month follow-up patients consenting to the telephone survey were screened for eligibility for the RCT by a trained interviewer and invited to participate if eligible for the study.
Treatment allocation
Eligible patients were randomised in a 1:1 allocation ratio, to either receive the weight management and healthy lifestyle intervention at that time (intervention group) or remain as part of the cohort and be told they will be offered clinical services in 6 months (control group). The randomisation schedule was generated a priori by an independent statistician using SAS 9.3 through the SURVEYSELECT procedure. To randomise patients, a trained interviewer opened a sealed opaque envelope containing group allocation. A staff member not involved in the study prepared the envelopes.
Sample size
The sample size for both trials was calculated using Stata sample size calculator.
For trial one a standard deviation of 2.3, a two-sided alpha of 0.025 (to account for two outcomes of interest, the primary outcome (pain) and the key secondary outcome (weight) 22 and allowing for 15% loss to follow-up was used. A sample size of 80 participants per group (n=160) has 90% power to detect a clinically meaningful difference of 1.5 points in pain intensity (pain NRS) between intervention and control groups 23 . This sample also provides power 80% to detect a 6% reduction in weight in the underlying sampling population, based on evidence from other musculoskeletal conditions this is hypothesised to lead to a clinically meaningful reduction in pain 23 .
For trial two a standard deviation of 2.7, a two-sided alpha of 0.025 (to account for two outcomes of interest, the primary outcome (pain) and the key secondary outcome (weight) 22 and allowing for 15% loss to follow up, a sample of 60 participants per group will provide 90% power to detect a clinically meaningful difference of 2 points in pain intensity (pain NRS) scores between intervention and control groups at 26 weeks. This sample also provides 80% power to detect a 6% weight reduction which is hypothesised to be lead to a clinically meaningful reduction in pain 23 .
In these calculations the increase in statistical power conferred by reducing error variance through repeated outcome measures over time and the correlations among repeated measures have been conservatively ignored.
Data collection and follow up
The different stages of data collection and follow-up for secondary outcomes are summarised in table one. The primary outcome, pain intensity score, was collected at baseline, week 2, 6, 10, 14, 18, 22 and at 26 weeks. Baseline assessment was conducted prior to randomisation.
Interim analysis
No interim analysis was conducted.
Statistical analysis
Trial profile
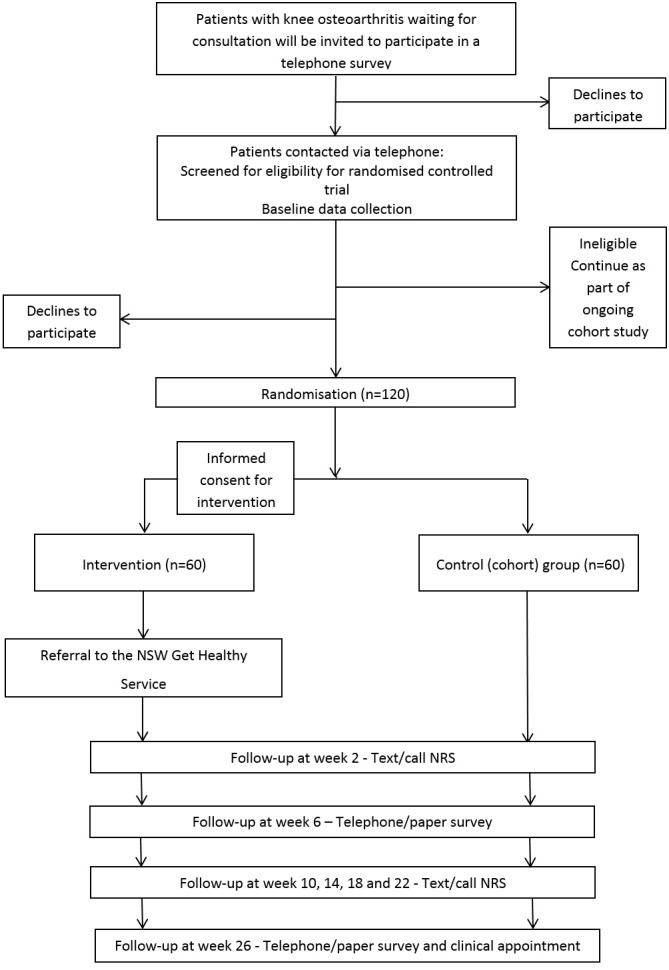
Flow of the patients through the study will be displayed in a Consolidated Standards of Reporting Trials (CONSORT) diagram for each trial. We will report the number of screened patients who met study inclusion criteria, reasons for exclusion of non-included patients, the number of participants randomised per group, and the number who completed follow-up, as shown in Figures 1A and 1B.
Figure 1A. Progress of participants through trial one (low back pain).

Figure 1B. Progress of participants through trial two (knee osteoarthritis).
Data integrity
Trial data integrity will be monitored by regularly scrutinising data files for data omissions and errors. Manually entered data (i.e. data not recorded directly by the participant) will be double entered and the source of any inconsistencies will be explored and resolved in consultation with the lead investigator (CW).
Analysis principles
Primary analyses will be conducted independently by an independent statistician who is blinded to group status.
Analyses will be conducted using SAS V9.4 (SAS Institute, Cary, North Carolina, USA). Intention-to-treat (ITT) (analysed as randomised) will be utilised. All statistical tests will be two-tailed. Treatment effect for the primary and secondary outcomes will be considered significant if p≤0.025 and p≤0.01, respectively.
Summaries of continuous variables that are symmetrically distributed will be presented as means and standard deviations (SD) or medians and inter-quartiles for skewed data, whereas categorical variables will be presented as frequencies and percentages. Large count variables will be reported as medians and interquartile ranges, low counts (max count <5) will be presented as frequencies and percentages.
Analysis population
The ITT population is defined as all randomised participants with a baseline measurement. Participants failing to record an outcome value at any follow-up period will be treated using the methods described below (see “Methods for handling missing data”).
Methods for handling missing data
The number of participants with missing observations will be reported for each outcome variable. Patterns of missing data will be investigated and compared by demographic characteristics of the participants, t-tests will be used to compare continuous variables and chi-square tests will be used to compare categorical variables. For the primary outcome variable (average weekly pain intensity score) for participants with <10% missing pain intensity values, the missing pain intensity values will be interpolated using cubic spline interpolation. For participants with 10% or greater missing data an AUC will not be computed. The primary method of dealing with missing AUC data will be through multiple imputation (assuming missing at random), where missing AUC data will be imputed using the chained equations method of generating a number of complete data sets; the imputation model will include a range of covariates believed to be associated with either the missing outcome or the outcome itself (baseline pain and duration, waiting time, BMI). Sensitivity of analysis results will be assessed by comparing results obtained various imputation models. If there is reason to suggest the data may be missing not at random, pattern mixture models will be utilised 24 .
Evaluation of demographics and baseline characteristics
The description of baseline characteristics listed below will be presented by treatment group. Categorical variables will be summarized by frequencies or denominators and percentages. Percentages will be calculated using the number of patients for whom data is available as the denominator. Denominators will be systematically reported (for example, nn/NN, %). Continuous variables will be summarised using standard measures of central tendency and dispersion, either mean and SD, or median and interquartile range.
-
-
Age at randomisation
-
-
Gender
-
-
Aboriginal and/or Torres Strait Islander
-
-
Employment status
-
-
Country of origin
-
-
Highest level of education
-
-
Private health insurance
-
-
Other co-existing medical conditions needing medication
-
-
Length of time waiting for consultation (days)
-
-
Triage classification
-
-
Pain intensity and duration
-
-
Disability and function
-
-
Subjective weight
-
-
BMI
-
-
Quality of Life
-
-
Emotional distress
-
-
Sleep quality
-
-
Physical activity
-
-
Diet
-
-
Alcohol consumption
-
-
Smoking prevalence
-
-
Pain attitudes
-
-
Fear avoidance beliefs
-
-
Health care utilisation
Process measures and concomitant treatments
When indicated, data will be summarised per group. Again continuous variables will be summarised by use of standard measures of central tendency and dispersion, either mean and SD, or median and interquartile range. Categorical variables will be summarised by frequencies or denominators and percentages.
Primary analysis
To examine between-group differences in the primary outcome (AUC – based on pain intensity score) we will use an independent sample Students t-test. The primary analysis will not adjust for known prognostic variables as covariates, but results adjusting for these will be presented as a sensitivity analysis (see below). Separate models will be estimated for each imputed dataset and the means and standard errors will be combined using Rubin’s method 25 . We will assess other model assumptions (homoscedasticity, normality) through inspecting appropriate residual plots, where serious violations are observed we will apply a rank-inverse normal transformation to the pain intensity score values. Dummy coded variables representing group allocation will be used to ensure blinding of the analyses. See Table 3 for details.
Table 3. Analyses of primary outcome.
| Analysis | Outcome | Intervention | Control | Difference |
|---|---|---|---|---|
| Primary (ITT Multiple Imputation) | Area under the pain intensity curve (AUC) | mean(95%CI) | mean(95%CI) | mean(95%CI) |
| Sensitivity | Adjusted AUC* | mean(95%CI) | mean(95%CI) | mean(95%CI) |
| Secondary | Pain intensity score | |||
| Baseline | mean(SD) | mean(SD) | ||
| Week 2, | mean(SD) | mean(SD) | ||
| Week 6 | mean(SD) | mean(SD) | ||
| Week 10 | mean(SD) | mean(SD) | ||
| Week 14 | mean(SD) | mean(SD) | ||
| Week 18 | mean(SD) | mean(SD) | ||
| Week 22 | mean(SD) | mean(SD) | ||
| Week 26 | mean(SD) | mean(SD) | ||
| Weekly trend | mean(95%CI) | mean(95%CI) | mean(95%CI) |
Adjusted for baseline pain and duration, waiting time, previous surgery; BMI: physical activity and dietary intake; ITT: Intention to treat.
Secondary analysis
Between group differences in the trajectory of pain intensities over the follow-up period will be examined using growth curve modelling. Hierarchical linear models will be used, with fixed effects for treatment group, time, and the interaction between the two. The model will include random subject-level intercepts and slopes. A linear growth trend will initially be assumed, and if not appropriate different functional forms for the trend will be applied (for example the square root transformation). If an appropriate functional form cannot be determined a flexible piecewise linear model will be used 26 . We will also investigate treatment effect heterogeneity that may exist in latent subgroups of participants through growth mixture models 27 . In these models a number of latent classes are specified that model the potential for participants to have different trajectory types, the functional forms identified from the previous growth curve analyses will inform the functional forms for this analysis. The model will include the following random effects that are all conditional trajectory class membership: intercept linear slope and quadratic slope. The random effects are influenced by the treatment group, so there will potentially be 3 lots of treatment effects (for each random effect) for each latent class.
Longitudinal generalised linear mixed models will be used to assess treatment effect on post randomisation secondary outcome measurements with random intercepts for individuals to account for correlation of repeated measures and an appropriate link function dependent on the type and distribution of the data. We will compare the adjusted mean change (continuous variables) or relative risks (dichotomous variables) in outcome from baseline to each time point between the treatment and control groups. A binomial distribution family (with log link) will be used for dichotomous outcomes (sleep quality, smoking prevalence), and a Poisson or negative-binomial distribution family (with a log link function) will be used for count outcomes (health care utilisation) based on assessment of data dispersion. T-tests will be used to test between group differences in variables collected only at 26 weeks (objective weight, BMI, waist circumference). See Table 4 for details.
Table 4. Secondary outcomes.
| Outcome | Intervention | Control | Intervention - control |
|---|---|---|---|
| Disability and function (Trial 1: RMDQ / Trial 2: WOMAC) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Subjective weight | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Objective weight | |||
| Baselinea | mean (SD) | N/A | N/A |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| BMI | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Waist circumference | |||
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Quality of life (SF12v2, PCS) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Quality of life (SF12v2, MCS) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Perceived change in condition (GPE) | |||
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Emotional distress (DASS-21) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Poor sleep quality (item 6, Pittsburgh Sleep Quality Index) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Physical activity (mins MVPA/week) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Diet (Fruit, serves) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Diet (Vegetable, serves) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Diet (Discretionary foods, serves) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Alcohol consumption (AUDIT) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Smoking prevalence | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Pain Attitudes (SOPA) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 6 | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Fear avoidance beliefs (FABQ) | |||
| Baseline | mean (SD) | mean (SD) | mean (95% CI) |
| Week 26 | mean (SD) | mean (SD) | mean (95% CI) |
| Overall | mean (SD) | mean (SD) | mean (95% CI) |
| Health care utilisation (Medication use for back or knee pain) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Health care utilisation (Visits for back or knee pain) | |||
| Baseline | n/N (%) | n/N (%) | OR (95% CI) |
| Week 6 | n/N (%) | n/N (%) | OR (95% CI) |
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Overall | n/N (%) | n/N (%) | OR (95% CI) |
| Health care utilisation (Attended orthopaedic consultation for back or knee) | |||
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
| Health care utilisation (Received surgery for back or knee) | |||
| Week 26 | n/N (%) | n/N (%) | OR (95% CI) |
Intervention group of low back pain patients (trial one) only.
RMDQ=Roland Morris Disability Questionnaire; WOMAC=Western Ontario and McMaster Universities Index; BMI=Body Mass Index; SF12.v2=Short Form Health Survey version 2; PCS=Physical Component Score; MCS=Mental Component Score; GPE=Global Perceived Effect; DASS-21=Depression Anxiety Stress Scale; MVPA=Moderate-to-Vigorous Physical Activity; AUDIT=Alcohol Use Disorders Identification Test; SOPA=Survey of Pain Attitudes; FABQ=Fear Avoidance Beliefs Questionnaire.
Sensitivity analyses
Adjusting for prognostic variables:
The following variables hypothesised to effect outcome will be assessed by their inclusion as covariates in a linear regression model for the analysis of the primary outcome (AUC): baseline pain intensity, time since onset of pain, waiting time, BMI.
Evaluation of adverse events
The Fisher exact test will be used to compare the incidence of any AEs between groups. This test will be used as the event rate of AEs is expected to be low.
Acknowledgements
This study is funded by Hunter New England Local Health District and the Hunter Medical Research Institute. The project also received support from the University of Newcastle.
Footnotes
Trial Registration: Both trials were prospectively registered with the Australian New Zealand Clinical Trials Registry (trial one: ACTRN12615000478516https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368472, and trial two: ACTRN12615000490572https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368452).
HOW TO CITE THIS ARTICLE O’Brien KM, Williams A, Wiggers J, Wolfenden L, Yoong S, Campbell E, et al. Effectiveness of a healthy lifestyle intervention for low back pain and osteoarthritis of the knee: protocol and statistical analysis plan for two randomised controlled trials. Braz J Phys Ther. 2016 Mês-Mês; 20(5):xx-xx. http://dx.doi.org/10.1590/bjpt-rbf.2014.0189
References
- 1.Relton C, Torgerson D, O’Cathain A, Nicholl J. Rethinking pragmatic randomised controlled trials: introducing the “cohort multiple randomised controlled trial” design. BMJ. 2010;340:c1066. doi: 10.1136/bmj.c1066. http://dx.doi.org/10.1136/bmj.c1066 [DOI] [PubMed] [Google Scholar]
- 2.Williams A, Wiggers J, O’Brien KM, Wolfenden L, Yoong S, Campbell E, et al. A randomised controlled trial of a lifestyle behavioural intervention for patients with low back pain, who are overweight or obese: study protocol. BMC Musculoskelet Disord. 2016;17(1):70. doi: 10.1186/s12891-016-0922-1. http://dx.doi.org/10.1186/s12891-016-0922-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Brien KM, Wiggers J, Williams A, Campbell E, Wolfenden L, Yoong S, et al. Randomised controlled trial of referral to a telephone-based weight management and healthy lifestyle programme for patients with knee osteoarthritis who are overweight or obese: a study protocol. BMJ Open. 2016;6(3):e010203. doi: 10.1136/bmjopen-2015-010203. http://dx.doi.org/10.1136/bmjopen-2015-010203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Hara B, Phongsavan P, Venugopal K, Eakin E, Eggins D, Caterson H, et al. Effectiveness of Australia’s get healthy information and coaching service: translational research with population wide impact. Prev Med. 2012;55(4):292–298. doi: 10.1016/j.ypmed.2012.07.022. http://dx.doi.org/10.1016/j.ypmed.2012.07.022 [DOI] [PubMed] [Google Scholar]
- 5.Krismer M, van Tulder M. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific) Best Pract Res Clin Rheumatol. 2007;21(1):77–91. doi: 10.1016/j.berh.2006.08.004. http://dx.doi.org/10.1016/j.berh.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 6.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83(2):157–162. doi: 10.1016/s0304-3959(99)00101-3. http://dx.doi.org/10.1016/S0304-3959(99)00101-3 [DOI] [PubMed] [Google Scholar]
- 7.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. User’s manual for the SF-12v2 health survey (with a supplement documenting SF-12 health survey) Boston: QualityMetric Incorporated; 2002. [Google Scholar]
- 8.My Hospitals . About the data: elective surgery waiting times. Australian Institute of Health and Welfare; Internet. cited 2015 Sep 15. Available from: http://www.myhospitals.gov.au/about-the-data/elective-surgery-waiting-times. [Google Scholar]
- 9.Roland M, Morris R. A study of the natural history of back pain. Part 1: development of a reliable and sensitive measure of disability in low back pain. Spine (Phila Pa 1976) 1983;8(2):141–144. doi: 10.1097/00007632-198303000-00004. http://dx.doi.org/10.1097/00007632-198303000-00004 [DOI] [PubMed] [Google Scholar]
- 10.Bellamy N. WOMAC user guide IX. Brisbane: Nicholas Bellamy; 2009. [Google Scholar]
- 11.International Society for the Advancement of Kinanthropometry – ISAK . International standards for anthropometric assessment. Underdale: ISAK; 2001. [Google Scholar]
- 12.National Institutes of Health, National Heart, Lung and Blood Institute – NHLBI . The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. Bethesda: National Institutes of Health; 2000. (NIH publication). Internet. [Google Scholar]
- 13.Kamper SJ, Ostelo RWJG, Knol DL, Maher CG, de Vet HCW, Hancock MJ. Global Perceived Effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol. 2010;63(7):760–766.e1. doi: 10.1016/j.jclinepi.2009.09.009. http://dx.doi.org/10.1016/j.jclinepi.2009.09.009 [DOI] [PubMed] [Google Scholar]
- 14.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 15.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. http://dx.doi.org/10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 16.Australian Institute of Health and Welfare – AIHW . The active Australia survey: a guide and manual for implementation, analysis and reporting. Canberra: AIHW; 2003. Cat. no. CVD 22. [Google Scholar]
- 17.Centre for Epidemiology and Research . NSW Population Health Survey. Sydney: NSW Department of Health; 2014. [Google Scholar]
- 18.Babor T, Higgins-Biddle J, Saunders J, Monteiro M. AUDIT: the alcohol use disorders identification test: guidelines for use in primary care. 2nd. Geneva: World Health Organization; 1992. [Google Scholar]
- 19.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123(1):87.e7–35. doi: 10.1016/j.amjmed.2009.05.028. http://dx.doi.org/10.1016/j.amjmed.2009.05.028 [DOI] [PubMed] [Google Scholar]
- 20.Jensen MP, Karoly P, Huger R. The development and preliminary validation of an instrument to assess patients’ attitudes toward pain. J Psychosom Res. 1987;31(3):393–400. doi: 10.1016/0022-3999(87)90060-2. http://dx.doi.org/10.1016/0022-3999(87)90060-2 [DOI] [PubMed] [Google Scholar]
- 21.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. http://dx.doi.org/10.1016/0304-3959(93)90127-B [DOI] [PubMed] [Google Scholar]
- 22.Proschan MA, Waclawiw MA. Practical guidelines for multiplicity adjustment in clinical trials. Control Clin Trials. 2000;21(6):527–539. doi: 10.1016/s0197-2456(00)00106-9. http://dx.doi.org/10.1016/S0197-2456(00)00106-9 [DOI] [PubMed] [Google Scholar]
- 23.Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta‐analysis. Ann Rheum Dis. 2007;66(4):433–439. doi: 10.1136/ard.2006.065904. http://dx.doi.org/10.1136/ard.2006.065904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molenberghs G, Kenward M. Missing data in clinical studies. New York: Wiley; 2007. [Google Scholar]
- 25.Marshall A, Altman DG, Holder RL, Royston P. Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol. 2009;9(1):57. doi: 10.1186/1471-2288-9-57. http://dx.doi.org/10.1186/1471-2288-9-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gallop R, Dimidjian S, Atkins D, Muggeo V. Quantifying treatment effects when flexibly modeling individual change in a nonlinear mixed effects model. J Data Sci. 2011;9:221–241. [Google Scholar]
- 27.Muthen B, Brown C, Hunter A, Cook I, Leuchter A. General approaches to analysis of course: applying growth mixture modeling to randomized trials of depression medication. In: Shrout P, Keyes K, Ornstein K, editors. Causality and psychopathology: finding the determinants of disorders and their cures. 1st. New York: Oxford University Press; 2011. pp. 159–178. [Google Scholar]


