Abstract
Background
Substance use disorders (SUDs), which encompass alcohol and drug use disorders (AUDs, DUDs), constitute a major public health challenge among US veterans. SUDs are among the most common and costly of all health conditions among veterans.
Objectives
This study sought to examine the epidemiology of SUDs among US veterans, compare the prevalence of SUDs in studies using diagnostic and administrative criteria assessment methods, and summarize trends in the prevalence of SUDs reported in studies sampling US veterans over time.
Methods
Comprehensive electronic database searches were conducted. A total of 3,490 studies were identified. We analyzed studies sampling US veterans and reporting prevalence, distribution, and examining AUDs and DUDs.
Results
Of the studies identified, 72 met inclusion criteria. The studies were published between 1995 and 2013. Studies using diagnostic criteria reported higher prevalence of AUDs (32% vs. 10%) and DUDs (20% vs. 5%) than administrative criteria, respectively. Regardless of assessment method, both the lifetime and past year prevalence of AUDs in studies sampling US veterans has declined gradually over time.
Conclusion
The prevalence of SUDs reported in studies sampling US veterans are affected by assessment method. Given the significant public health problems of SUDs among US veterans, improved guidelines for clinical screening using validated diagnostic criteria to assess AUDs and DUDs in US veteran populations are needed.
Scientific Significance
These findings may inform VA and other healthcare systems in prevention, diagnosis, and intervention for SUDs among US veterans.
INTRODUCTION
Substance use disorders (SUDs), which encompass alcohol and drug use disorders (AUDs, DUDs) constitute a major public health challenge among US veterans.1,2 SUDs are among the most common and costly of all health conditions among veterans.3,4 As one of the worlds’ largest providers of mental health care, the US Department of Veterans Affairs (VA) treats over 1.1 million patients diagnosed with psychiatric disorders or SUDs annually.5 Over one-third of VA inpatients screen positive for psychiatric disorders or SUDs.3,6 In 2007 alone, over 375,000 patients in the VA system were diagnosed with an SUD.7 The number of veterans treated for an SUD in an outpatient setting increased by 52.7% between 2005 and 2012, and there was a rise in the number of veterans diagnosed with opioid dependence from 2003 to 2005.8
Of late, there is considerable concern that veterans from more recent conflicts (ie, Operation Iraqi Freedom [OIF] and Operation Enduring Freedom [OEF]), particularly those who have psychiatric conditions including post-traumatic stress disorder (PTSD), are disproportionally affected by SUDs.2 Notably, increasing numbers of deployments to Iraq and Afghanistan, in addition to combat experience, have been associated with higher rates of both alcohol and other substance abuse among OIF/OEF veterans.9,10
Analyzes of VA administrative data and clinical diagnostic methods have been used to examine the occurrence of SUDs among US veterans. Given the various screening instruments that have been used to examine the prevalence of SUDs reported in studies sampling US veterans, it is important to systematically review the available research to analyze and understand whether different assessment methods produce different SUD estimates. Two systematic reviews have recently been published that summarize the epidemiology of SUDs in US veterans.11,12 One study provided a review of literature examining substance misuse, abuse, and dependence among women veterans, and the other study specifically examined whether alcohol or other SUDs were more common in Gulf War, Afghanistan, and Iraq War veterans compared to non-deployed military groups (eg, reserves). As noted in one of the previous systematic reviews,11 most studies rely on VA medical records data, and there is evidence that theses methods underestimate the true prevalence. Therefore, this study complements the other systematic reviews by providing a direct comparison of SUD prevalence using diagnostic assessment and administrative methods, and also evaluates trends in SUD prevalence over time. Although the Institute of Medicine recently published a comprehensive review of prevention, screening, diagnosis, and treatment modalities for SUDs among active members of the US Armed Forces,13 to our knowledge, no study has systematically reviewed the published epidemiology of SUDs using different assessments (ie, diagnostic or administrative methods) among US veterans.
The purpose of this study was to conduct a systematic review to compare and contrast the prevalence of SUDs reported in studies sampling US veterans using either clinical diagnostic or administrative assessment; in addition, this study aimed to summarize the trend in the prevalence of SUDs reported in studies sampling US veterans in the past two decades. The findings of this review may help to achieve more effective prevention and treatment efforts by shaping the content of targeted screening, and informing prioritization of resources to identify and reach those US veterans most affected by SUDs.
METHODS
Search Strategy
Studies were retrieved from several electronic databases (PsycINFO®, The Cochrane Library, CINAHL, Web of Science™, and MEDLINE/PubMed) using a Boolean search strategy.14 The searches consisted of the following broad terms: (i) veterans, and (ii) substance use disorders. Search terms were modified using individual database search guidelines, as needed, for each electronic database searched. For example, the search terms used in the PubMed search were as follows: veteran* AND substance use OR substance-related disorders [MeSH] OR (substance related AND disorder*) OR substance-related disorders OR addict* OR drug dependence OR drug dependence [MeSH] OR drug addiction [MeSH] OR substance use disorder [MeSH] OR substance dependence OR drug use OR substance abuse [MeSH] OR drug abuse [MeSH] OR substance addiction [MeSH] OR drug use disorder [MeSH] OR binge drinking OR ((binge AND (alcohol OR ethanol)) OR alcohol abuse OR alcoholic OR alcohol abuse [MeSH] OR alcoholism OR alcoholism [MeSH] OR alcohol use disorder* OR alcohol-related disorders [MeSH] OR alcoholic intoxication [MeSH] OR intoxicat*. As a second step, reference sections of relevant reviews (including published reviews obtained through the electronic database search) and included studies were reviewed by hand.
Inclusion Criteria
Studies were included in this systematic review if they: (i) sampled US veterans or reported on US veterans as a separate analytic group; (ii) assessed AUDs or DUDs using established DSM or World Health Organization International Classification of Diseases (ICD) diagnostic criteria; (iii) reported on the prevalence, distribution, or correlate(s) of SUD(s) in a US veterans sample; and were published in English. Diagnostic assessment defined AUDs or DUDs using validated diagnostic instruments, including the DSM and others described below, while administrative assessment defined AUDs or DUDs using ICD-9 codes (eg, 305.00–305.03 for alcohol abuse and 305.20–305.93 for drug abuse). In order to minimize misclassification of SUDs and other measurement errors, we restricted our review to studies that utilized previously validated diagnostic instruments, such as the Diagnostic Interview Schedule (DIS),15 the Structured Clinical Interview for DSM-IV (SCID),16 the Composite International Diagnostic Interview (CIDI-2),17 the Psychiatric Research Interview for Substance and Mental Disorders (PRISM),18 and the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) (19) or operationalize diagnostic criteria.
Exclusion Criteria
Due to our intention to summarize evidence regarding the prevalence of SUD diagnoses in studies sampling US veterans, we excluded studies that only used screening (rather than diagnostic) tools to identify problematic substance use behaviors (eg, the Alcohol Use Disorder Identification Test [AUDIT], the CAGE substance abuse screening tool, and the Drug Abuse Screening Tool [DAST]). Consistent with the selection criteria and overall review objectives, we excluded studies that sampled veterans entirely from substance abuse treatment programs and studies that only reported on substance use patterns or frequency (rather than disorders), and did not assess SUDs using established measures (as described above).
We further excluded studies published prior to 1987, as this year coincides with the publication and adoption of DSM-IIIR, in which significant changes were made to the classification of alcohol and substance abuse/dependence. Studies published during or after 1987 but that used DSM-III or earlier criteria were also excluded. Although DSM-V aligns nicotine dependence with other SUDs, we did not include studies exclusively assessing tobacco use disorders to be consistent with most previously published literature in this area.
Finally, we excluded case reports, case series, editorials, commentaries, and previously published narrative reviews. Given that the focus of this review was on the epidemiology of SUDs and not on substance abuse treatment interventions per se, we only included randomized controlled trials if pretreatment baseline data on the distribution or correlates of SUDs were reported. Although “grey literature,” including reports from the Substance Abuse and Mental Health Services Administration (SAMHSA), the Department of Defense, the VA, and other governmental organizations were reviewed and informed the objectives and context of the systematic review, we chose to focus our study on the synthesis of results published in the scientific, peer-reviewed literature.
Screening and Extraction Procedures
The primary author (C.W.L.) screened the titles and abstracts of each record and excluded studies that did not meet the inclusion criteria. Full-text articles were retrieved for all studies for which eligibility was unclear. Full-text versions of the remaining articles were then screened independently by two authors (C.W.L. and B.D.L.M.). Based upon the inclusion criteria, studies were categorized as “potentially relevant” or “irrelevant” by each author. Classifications were then compared for each record and any discrepancies were discussed until a consensus was reached.
Studies that fulfilled the above-mentioned selection criteria and were available and published by January 1st, 2014 were included. Comprehensive electronic searches identified 3,490 unique and potentially relevant reports. In a first stage of screening, 3,228 were excluded on the basis of their titles and abstracts because they did not meet inclusion criteria. Of the 262 full-text articles screened for eligibility, 190 were excluded in the second stage of screening because they: (i) did not provide SUD measures using established DSM or ICD diagnostic criteria, (ii) only sampled participants with AUD or SUD (ie, a treatment sample), or (iii) used DSM-III diagnostic criteria (see details in Fig. 1). We included 72 studies in the final analysis. We based our synthesis on all 72 eligible studies.
FIGURE 1.
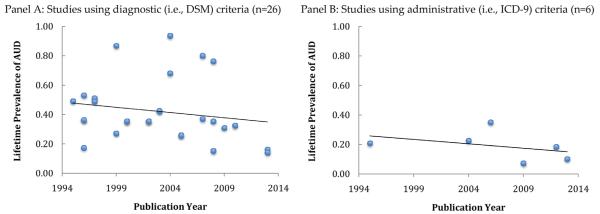
Prevalence of lifetime alcohol use disorders (AUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend lines, calculated using weighted least squares regression. Note: Some of the data points overlap with each other since they had the same or very similar data point. DSM, Diagnostic and Statistical Manual of Mental Disorders; DUD, drug use disorder; ICD-9, international classification of diseases.
Data extraction was conducted to obtain study information, including sample characteristics (eg, gender, marital status, ethnicity) and primary results. First, studies were stratified into two categories: (i) studies that used diagnostic criteria; and (ii) analyses using administrative records that defined SUDs using ICD-9 codes. Second, the prevalence of AUDs and DUDs in studies sampling US veterans were pooled from each category of studies, and were analyzed separately. We also extracted and pooled the reported prevalence of PTSD among the subset of studies that reported this information. Third, we analyzed the temporal trends of AUDs and DUDs prevalence from each category by plotting the prevalence estimates from each study by publication year. Least squares regressions were weighted by sample size and the trend line for each outcome for each study category. Finally, we conducted three sensitivity analyses, the first to examine the effect of different timeframes (ie, lifetime vs. past-year SUD) on observed trends in AUD and DUD prevalence over time. In a second sub-analysis, we also determined whether the year of earliest data collection (rather than publication year) affected the results. Finally, given that some studies focused on populations of specific clinical interest (eg, homeless veterans, HIV-infected veterans), we conducted a third sensitivity analysis, excluding studies with samples of veterans who may be at particularly high risk for SUDs. Specifically, we included in this sub-analysis only those studies that were representative (eg, relied on a random sampling frame), or derived samples based on access to VA health services, wartime era, or service period alone.
RESULTS
Overview
Across both types of study designs, the 72 eligible studies were published between 1995 and 2013. The earliest date of data collection was 1987. Of the 43 studies that reported on age distributions, the mean age was 52 years. A total of 40 studies reported the prevalence of PTSD. The 72 studies sampled a total of 18,466,328 US veterans, and of these participants, 91% were men.19–54
Prevalence of SUDs in Studies Sampling US Veterans Using Diagnostic Criteria
The 37 studies employing diagnostic criteria were published between 1995 and 2013. The earliest date of data collection was 1987. The 37 studies sampled a total of 123,885 US veterans.20–23,25–56 Of the 123,885 participants sampled, 97% were men, with a mean age of 46 years. Of the 36 studies that differentiated between AUDs and DUDs, 32% of participants with diagnosed with an AUD, and 20% with diagnosed with a DUD. Of the 22 studies that reported on PTSD, the pooled prevalence was 19%. Table 1 provides additional sample details for the 37 studies using diagnostic criteria.
TABLE 1.
Studies using diagnostic criteria to examine SUDs among US veterans (n=37)
| Study population |
SUDs |
|||||||
|---|---|---|---|---|---|---|---|---|
| Author, Year | Era or years sampled |
Total no. |
% Women |
Sample | AUD (%) |
DUD (%) |
Assessment period |
Principal findings |
| Balan (2013) | Vietnam | 642 | 0 | Combat veterans deployed to Vietnam |
16 | 8 | Lifetime | 12% reported PTSD. Prevalence of DUDs declined from 29.8% in 1972 to 8.3% in 1996. |
| Black (2004) | Gulf war | 132 | 12 | Population-based survey of military personnel |
68 | — | Lifetime | Lifetime SUDs were significantly more frequent in deployed than non-deployed veterans (70% vs. 52%), particularly AUDs (68% vs. 52%). |
| Callaghan (1996) | 1994 | 97 | 0 | Veterans with spinal cord injuries |
40 | Lifetime | Prescription of benzodiazepines was not significantly greater in veterans with a spinal cord injury and diagnosed with SUDs than those without SUDs. |
|
| Crawford (2013) | After 2001 |
1,775 | 2 | Anyone with military service after September 11, 2001 |
9 | — | Past year | Significance gender difference in AUDs prevalence were observed: the rate of any AUDs was higher among men (10%) compared to women (6%). |
| David (1999) | Vietnam | 53 | 0 | Personnel diagnosed with combat-related PTSD |
87 | 64 | Lifetime | Veterans with PTSD were sampled. No association was found between psychotic symptoms and a lifetime history of AUDs or DUDs. |
| David (2004) | 1997– 1999 |
93 | 0 | Male veterans admitted to rehabilitation for PTSD |
94 | — | Lifetime | 59% PTSD. Association between alcohol dependence and certain medical conditions is likely mediated by adverse health behaviors. |
| Dickerson (2009) | 1999– 2001 |
480 | 0 | Community-based survey of American Indian male veterans |
31 | 13 | Lifetime | 12% PTSD. Substantial co-morbidity exists between nicotine dependence and other substance abuse. |
| Ditre (2005) | 2003 | 124 | — | Veterans with spinal cord injury |
26 | 11 | Lifetime | Intoxication at injury does not necessarily substantiate the existence of an underlying substance misuse problem. |
| Fiedler (2006) | Gulf war | 967 | 10 | Random sample from all US troops |
5 | 1 | Past year | 3% PTSD. Gulf War veterans had significantly higher prevalence of psychiatric diagnosis, with twice the prevalence of anxiety disorders and depression. |
| Fu (2002) | Vietnam | 6,720 | 0 | Veterans served in Vietnam Era |
35 | — | Lifetime | Genetic effects on antisocial personality disorder are a major determinant of risk of SUDs. |
| Fu (2002) | Vietnam | 7,369 | 0 | Veterans served in Vietnam Era |
35 | 10 | Lifetime | 10% PTSD. There may be a genetic susceptibility specific to both suicidal ideation and suicide attempt in men. |
| Gale (2008) | Vietnam | 3,258 | 0 | Random sampling from veterans served in Vietnam |
32 | 10 | Past year | 10% PTSD. Lower cognitive ability was associated with an increased risk of depression, AUDs and PTSD. |
| Golub (2013) | OEF/OIF | 3,826 | 18 | National Survey on Drug Use and Health |
15 | 5 | Past year | 18% has any SUDs. The prevalence of untreated SUDs among veterans was twice as high as untreated serious psychological distress. |
| Grand (2007) | 2005 | 231 | 0 | Nicotine Dependent veterans |
80 | 58 | Lifetime | 22% PTSD. Lower quit rates among smokers with AUDs and suggests that specialized treatment is needed for this population of smokers. |
| Grant (2010) | Vietnam | 6,362 | 0 | Male veterans served between 1939–1957 |
32 | 9 | Lifetime | The analyses indicate that cannabis initiation, whether early or late, confer risk for other substance use and SUDs that is independent of familial influences. |
| Grossman (1997) | 1992– 1993 |
62 | 50 | Hospitalized female veterans |
56 | Lifetime | More men were diagnosed with PTSD or SUDs than women. | |
| Hamner (1997) | Vietnam | 25 | 0 | Veterans with PTSD | 51 | 29 | Lifetime | Psychotic phenomena occur in association with chronic PTSD in a Vietnam combat veteran population. |
| Hamner (1999) | Vietnam | 45 | 0 | Veterans with PTSD but no primary psychotic disorder |
27 | — | Lifetime | The occurrence of psychotic features in PTSD is not necessarily due to a primary psychotic disorder. |
| Herrmann (1996) | WWII | 76 | — | Veterans with PTSD | 53 | — | Lifetime | There was a significant correlation between the severity of combat stress and subsequent alcohol abuse. |
| Humphreys (2012) | Vietnam | 926 | 0 | Veterans with PTSD | 21 | — | Past year | Antisocial personality disorder comorbidities in reduced physiological reactivity to trauma reminders are present in some individuals with PTSD. |
| Joseph (1995) | 1991– 1993 |
117 | 3 | Residents of VA nursing home |
49 | — | Lifetime | The prevalence of AUDs was high in the sample. CAGE and MAST-G test are both sensitive to AUDs in the setting. |
| Kasprow (1998) | 50% Vietnam Era |
36,928 | 2 | Homeless Native American veterans |
57 | 40 | Past year | Native Americans veterans reported more current AUDs and they have more severe alcohol problems than other minority groups but fewer psychiatric problems. |
| Kausch (2003) | 2000– 2001 |
114 | 9 | Veterans treated for pathological gambling |
42 | 30 | Lifetime | 5% PTSD. Impulsivity score of gamblers with both AUDs and DUDs who had suicide attempts was higher than those without. |
| Kilbourne (2005) | 1997– 2000 |
330 | 9 | Patients with bipolar disorder |
26 | 7 | Lifetime | Minorities with bipolar disorder may be a more vulnerable population because of high rates of SUDs. |
| Miller (2008) | Vietnam | 1,325 | 0 | Veterans with PTSD | 76 | — | Lifetime | 72% PTSD. 58% of the sample was diagnosed with lifetime SUDs. |
| Miller (2011) | 49% Vietnam |
555 | 11 | Veterans who used health service at VA |
42 | Lifetime | Greater comorbidity of SUD among those who met PTSD criteria. | |
| Miller (2013) | 2011 | 242 | 1 | Veterans with history of exposure to a traumatic event |
14 | 9 | Lifetime | 43% PTSD. 17% SUD; partner alcohol and drug use explained more variance in veterans’ alcohol and drug use. |
| Morton (1996) | 1994 | 120 | 0 | 64 or older veterans | 36 | — | Lifetime | The MAST-G and the CAGE outperformed the AUDIT for detecting AUDs. |
| O’Toole (2003) | Vietnam & Gulf war |
127 | 0 | Homeless veterans | 80 | Past year | 18% PTSD. Homeless veterans reported greater percentage of SUDs and continue to have substantial health issues that need improved access to VA services. |
|
| Orsillo (1996) | Vietnam | 311 | 0 | Veterans experienced war zone-related trauma |
17 | 10 | Lifetime | 63% PTSD. Veterans with PTSD had significantly higher rates of AUDs, major depression, and panic disorder. |
| Ouimette (1996) | Vietnam | 47 | 1 | Female veterans served during Vietnam Era |
36 | — | Lifetime | 53% PTSD. Women with PTSD and AUDs reported more childhood sexual abuse and victimization during wartime. |
| Sajatovic (2006) | 1997– 2000 |
184 | 9 | Veterans with bipolar disorder |
38 | — | Past year | Having current SUDs was associated with medication non- adherence. |
| Wagner (2007) | 2000– 2003 |
12,072 | 10 | National Survey on Drug Use and Health |
6 | 2 | Past year | Veterans and comparable nonveterans reported similar rates of AUDs and DUDs in the last year. |
| Westermeyer (2008) | 1999– 2001 |
417 | 14 | American Indian veterans |
15 | — | Lifetime | 8% PTSD. Those with DUDs showed trends for an association with gambling while AUDs was not associated with gambling. |
| White (2011) | 2008 | 17,641 | 0 | National Survey on Drug Use and Health |
7 | Past year | Military status was not differentially associated with past year AUDs or DUDs. |
|
| Xian (2000) | Vietnam | 6,608 | 0 | Population registry | 35 | 10 | Lifetime | 10% PTSD. The liability for PTSD was partially due to a 15% genetic contribution common to AUDs and DUDs. |
| Yovtcheva (2001) | 1991– 2000 |
306 | 3 | Hepatitis C-positive patients |
86 | 39 | Past year | Participants with AUDs have hepatitis C sero-positivity rates higher than the general population. 19% reported PTSD. |
SUD, substance use disorder; AUD, alcohol use disorder; DUD, drug use disorder; PTSD, posttraumatic stress disorder; NSDUH, National Survey on Drug Use and Health.
Several eligible studies used data from the NSDUH to examine the prevalence of SUDs in probability-based samples of veterans. For example, a study conducted by Golub et al.32 used data from the 2004 to 2010 NSDUH cycles, and found that even though 75% of veterans reported having consumed alcohol in the past month, 18% of the sample met the DSM-IV criteria for an AUD.
Prevalence of SUDs in Studies Sampling US Veterans Using Administrative Criteria
Among the 72 eligible studies, 35 studies used administrative data and sampled a total of 18,342,443 US veterans.5,57–90 Table 2 provides sample details for the 35 studies that used VA administrative data (SUD ICD-9 diagnostic codes) to examine the prevalence of SUDs reported in studies sampling US veterans accessing VA care. These studies were published between 1995 and 2013. The earliest date of data collection was 1993. Of these participants, 91% were men, with a mean of 52 years of age. Overall the pooled prevalence of SUDs reported in studies sampling US veterans was 11%, and of the studies differentiating between AUDs and DUDs, the prevalence was 10% and 5%, respectively. In one notable nationwide study by Seal et al.,84 the prevalence of current AUD diagnoses in OEF/OIF veterans in VA healthcare was observed to be 11% for men and 5% for women. Of the 18 studies that reported on PTSD, the pooled prevalence was 10%.
TABLE 2.
Studies using administrative data to examine SUDs among US veterans (n=35)
| Study Population |
SUDs |
|||||||
|---|---|---|---|---|---|---|---|---|
| Author, Year |
Era or years sampled |
Total | % Women |
Study setting | AUD (%) |
DUD (%) |
Assessment period |
Principal findings |
| Anderson (1995) | 29% Vietnam |
125,267 | 3 | Veterans diagnosed with suicide attempt compared with non-suicidal |
21 | 7 | Lifetime | Substance-abusing suicidal inpatients received nearly twice as many SUDs diagnosis. 4% reported PTSD. |
| Andersen (2010) | OEF/OIF | 4,416 | 11 | Veterans served between 2001 to 2007 |
10 | Lifetime | Physical health effects are associated with PTSD in the early years post deployment among OEF/OIF veterans. 6% reported PTSD. |
|
| Banerjea (2009) | 1999– 2002 |
8,338 | 2 | Veterans with spinal cord injury |
9 | 8 | Past year | 26% any SUDs; 46% VHA users with spinal cord injuries had either a MI or SUDs. 6% reported PTSD. |
| Banerjea (2009) | 1999– 2000 |
16,368 | 1 | Veterans with diabetes | 4 | 3 | Past year | 13% SUDs; 45% had a mental illness (MI), SUDs, or both; SUDs rates were high among those with serious MI. |
| Bohnert (2013) | 2005– 2007 |
272, 509 | 6 | Veterans with PTSD | 19 | Past year | 19% SUDs among the PTSD cohort. | |
| Bohnert (2012) | 2000– 2006 |
3,291,891 | 10 | Patients who use VA services in 1999 |
9 | 6 | Past year | 10% SUDs; death from accidental overdose was found to be associated with psychiatric and SUDs. 6% reported PTSD. |
| Butt (2007) | 1999– 2003 |
253,942 | 3 | HCV-infected and uninfected veterans |
24 | 19 | Past year | The association of between HCV and psychiatric diagnosis is at partially attributable to AUDs and DUDs. 11% reported PTSD. |
| Butt (2009) | 2001– 2006 |
171,665 | 3 | HCV-infected veteran receiving care at VA |
28 | 21 | Past year | HCV-infected subjects were more likely to abuse alcohol and drugs. |
| Butt (2010) | 1998– 2003 |
16,043 | 4 | VA National Patient Care database |
27 | Past year | Non-completers for HCV treatment were more likely to have SUDs. |
|
| Chermack (2012) | 2001– 2007 |
3,942,948 | 9 | All patients seen at VA in 2001 |
9 | 3 | Past year | A diagnosis of SUDs was significantly associated with death by homicide. |
| Conigliaro (2003) | 1999– 2000 |
881 | 1 | HIV-infected veteran | 27 | — | Past year | Among HIV-infected cohort, alcohol diagnosis was common and associated with HIV disease progression. |
| Copeland (2012) | 2002 | 254,051 | 5 | Obese primary care patients |
3 | Past year | VHA efforts to help obese patients manage their weight appeared more common for patients with psychiatric diagnoses. 6% PTSD. |
|
| Crothers (2006) | 2001– 2002 |
1,727 | 0 | HIV-positive and negative male veteran |
22 | — | Past year | HIV-positive subjects were more likely to have received a diagnosis of AUDs. |
| Edelman (2013) | 2006 | 78, 748 | 3 | Receiving care at VA in 2006 |
10 | 11 | Past year | 9% PTSD; patients receiving opioids had a greater prevalence of AUDs, DUDs, and major depression. |
| Edens (2012) | 8% OEF/OIF |
1,102,846 | 9 | VA data in 2009 | 18 | 15 | Lifetime | DUDs had no significant independent association with pathological gambling. 38% PTSD. |
| Freiberg (2010) | 2002– 2006 |
4,743 | 0 | HIV-infected and uninfected veterans |
23 | — | Past year | Among HIV-infected men, AUDs was associated with higher prevalence of cardiovascular diseases |
| Green (2010) | 61% Vietnam |
6,351 | 5 | Veteran Aging Cohort in 2002 |
21 | 25 | Past year | Non-drug users were most prevalent among HIV uninfected. 10% PTSD. |
| Hoblyn (2009) | 2004 | 2,963 | 14 | Bipolar disorder Diagnoses |
20 | 10 | Past year | Patients diagnosed as having both an AUDs and DUDs and who were also separated from their partner had 100% risk of psychiatric hospitalization |
| Howard (1996) | 1993 | 536,244 | 2 | American Indian veterans | 20 | 6 | Past year | 23% of the sample had SUDs. Native American veterans with SUDs were more likely to be diagnosed with AUDs and PTSD and less likely with DUDs. 2% PTSD. |
| Justice (2006) | 1999– 2000 |
866 | 1 | Veterans with HIV | 35 | — | Lifetime, past year |
Past and current use of alcohol is common among those with HIV. |
| Justice (2004) | 2001– 2002 |
1,803 | — | Veteran with and without HIV |
23 | 23 | Lifetime | Older HIV-positive veterans demonstrate greater prevalence of AUDs and DUDs. |
| Kalman (2004) | 1999 | 127,308 | 4 | Veterans enrolled in VA in 1999 |
5 | — | Past year | 22% PTSD; respondents with history of AUDs had lower HRQoL. |
| Kilbourne (2004) | 2001 | 4,310 | 10 | Diagnosed with bipolar disorder |
25 | — | Past year | Individuals with bipolar disorder possess a substantial burden of general medical comorbidity, including AUDs. |
| Kilbourne (2004) | 2000 | 813 | 11 | Veterans with bipolar disorder |
30 | 14 | Past year | Older African American patients with bipolar disorder are more likely to receive diagnoses of mutually exclusive conditions such as schizophrenia. 14% PTSD. |
| McGinnis (2006) | 1997– 2004 |
42,054 | 0 | Male veterans with first HIV diagnosis between 1997–2004 |
27 | — | Past year | HIV-positive veterans have higher incidence of hepatocellular carcinoma and this association appears to be largely explained by higher prevalence of AUDs. |
| Pavao (2013) | 2010 | 126,598 | 7 | Homeless veterans | 3 | Past year | Of homeless veterans, 40% of females and 3% of males experienced military sexual trauma. |
|
| Petrakis (2011) | 58% VET |
1,001 | 11 | Veterans with PTSD | 21 | Past year | 41% PTSD. Post-VET were more likely to be dually diagnosed than veterans from other eras. |
|
| Rosen (2008) | Vietnam Era |
169,051 | 0 | VA psychiatric patients | 13 | 5 | Past year | The risk-adjusted probability of dying was 55% higher among psychiatric patients with co-occurring SUDs than those without. 47% PTSD. |
| Seal (2011) | OEF/OIF | 456, 502 | 12 | Veterans in OEF/OIF, 2001-2010 |
10 | 5 | Past year | 3% for both AUDs and DUDs; 26% PTSD. |
| Shi (2012) | 2005– 2008 |
878 | 28 | Veteran with major depressive symptoms |
37 | Past year | Veterans with major depressive disorder treated with duloxetine were associated with lower risks of opioid use and SUDs. |
|
| Sloan (2006) | 1999 | 914,225 | 5 | VA National Patient Care Database |
16 | 6 | Past year | 18% PTSD. Conditions like DUDs had higher outpatient utilization of care. |
| Smith (2011) | 1999– 2000 |
29,997 | 3 | VA nursing home resident | 21 | Past year | Adults aged 45+ were included in the study. Those with SUDs aged 75 to 84 years had significantly higher total costs of care than those aged 85 and above. |
|
| Striegel-Moore (1999) | 1996 | 196 | 0 | Inpatient veteran in 1996 | 21 | 11 | Past year | High rate of comorbid SUDs and mood disorder for men with eating disorders. |
| Tiwari (2008) | 1998– 1999 |
3,953 | 4 | Veteran with diabetes and major depressive disorder |
18 | Past year | 15% PTSD. African Americans, older veterans, and those with SUDs were less likely to have guideline-consistent antidepressant treatment. |
|
| VanCott (2010) | 1999– 2004 |
832 | 3 | VA patients 66 and older | 21 | Past year | Strongest predictor of suicide-related behaviors for older patients was a previous diagnosis of affective disorder. |
|
SUDs, substance use disorders; AUDs, alcohol use disorders; DUDs, drug use disorders; HRQoL, health-related quality of life.
Comparing SUDs in Studies Using Diagnostic and Administrative Criteria
The findings show that the prevalence of SUDs reported in studies sampling US veterans between the two groups of studies are different: studies using diagnostic criteria reported higher rates of SUDs overall (15% vs. 11%), as well as among studies that differentiated between AUDs (32% vs. 10%) and DUDs (20% vs. 5%) specifically. Of note, the samples were predominantly white (72%), yet studies using administrative data tended to have a higher proportion of African Americans than studies using clinical diagnostic criteria (28% vs. 18%), with a similar proportion of Hispanics (6% vs. 8%).
Trend of SUDs in Studies Using Diagnostic and Administrative Criteria
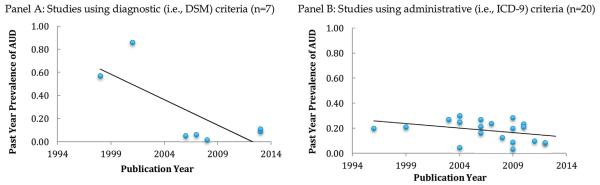
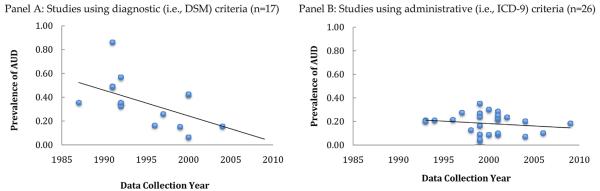
Studies using diagnostic and administrative criteria have both shown a gradual decline in the reported prevalence of AUDs in sampled US veterans over the past 20 years (Figs. 1 and 2). A similar gradual decline was observed when the analyses were stratified by timeframe (lifetime and past year, Figs. 1 and 2, respectively). Notably, from 1994 to 2014, there was wide variability in the estimates of lifetime AUDs prevalence in studies using diagnostic criteria (Fig. 1, Panel A). We observed less variability in the prevalence of lifetime and past year AUDs in studies using administrative records over the past two decades (Figs. 1 and 2, Panel B).
FIGURE 2.
Prevalence of past year alcohol use disorders (AUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend lines, calculated using weighted least squares regression. Note: Some of the data points overlap with each other since they had the same or very similar data point. AUD, alcohol use disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD-9, international classification of diseases.
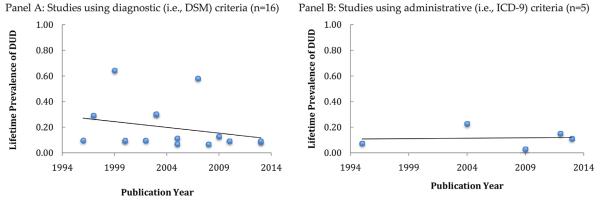
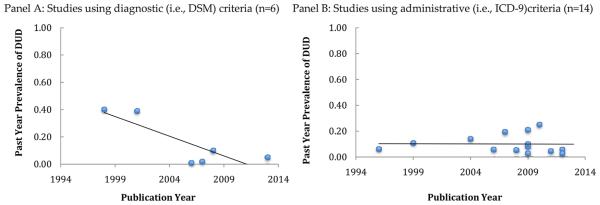
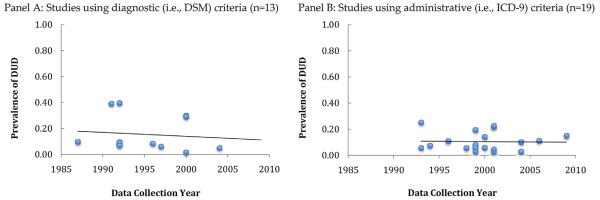
Studies using diagnostic criteria have shown a gradual decline in the reported prevalence of DUDs in studies sampling US veterans over the past 20 years (Fig. 3, Panel A). In contrast, DUD prevalence has been approximately stable in studies using administrative criteria (Fig. 3, Panel B). Similar results were observed when the analyses were stratified by lifetime and past year timeframes (see Figs. 3 and 4, respectively).
FIGURE 3.
Prevalence of lifetime drug use disorders (DUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend lines, calculated using weighted least squares regression. Note: Some of the data points overlap with each other since they had the same or very similar data point. AUD, alcohol use disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD-9, international classification of diseases.
FIGURE 4.
Prevalence of past year drug use disorders (DUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend line, calculated using weighted least squares regression. Note: Some of the data points overlap with each other since they had the same or very similar data point. AUD, alcohol use disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD-9, international classification of diseases.
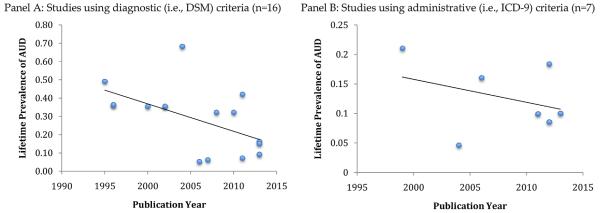
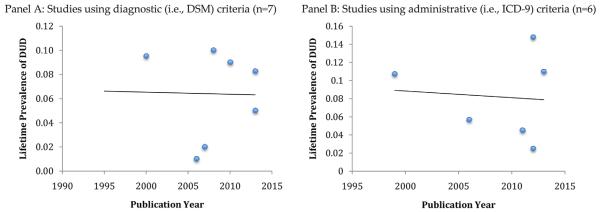
We conducted a second sub-analysis in which publication year was replaced by the earliest date of data collection in the weighted regression analysis. Of the 43 studies that reported dates of data collection for AUD prevalence, we observed a greater representation of administrative studies in more recent years (see Fig. 5). A similar pattern was observed among the 32 studies that reported the dates of data collection for DUD prevalence (see Fig. 6). As shown in Figures 5 and 6, the observed difference in AUD and DUD prevalence reported in diagnostic versus administrative studies has diminished in more recent years of data collection.
FIGURE 5.
Prevalence of alcohol use disorders (AUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by earliest data collection year. Note: black solid lines represent trend line, calculated using weighted least squares regression. Note: 18 studies are not presented in Panel A due lack of report on the year of data collection. DSM, Diagnostic and Statistical Manual of Mental Disorders; DUD, drug use disorder; ICD-9, international classification of diseases.
FIGURE 6.
Prevalence of drug use disorders (DUDs) among US veterans reported by studies using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by earliest data collection year. Note: black solid lines represent trend line, calculated using weighted least squares regression. Note: 9 studies are not presented in Panel A due lack of report on the year of data collection. DSM, Diagnostic and Statistical Manual of Mental Disorders; DUD, drug use disorder; ICD-9, international classification of diseases.
We conducted a third sub-analysis that included only studies that were representative (eg, relied on a random sampling frame) or consisted of general VA samples. Of the 23 studies included in the analysis, studies using diagnostic and administrative criteria have both shown a gradual decline in the reported prevalence of AUDs in sampled US veterans over the past 20 years (Fig. 7). In contrast, DUD prevalence has been approximately stable in these studies using both diagnostic and administrative criteria (Fig. 8).
FIGURE 7.
Prevalence of alcohol use disorders (AUDs) among US veterans reported by studies with representative sampling methods using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend lines, calculated using weighted least squares regression. Note: Some of the data points overlap with each other since they had the same or very similar data point. DSM, Diagnostic and Statistical Manual of Mental Disorders; DUD, drug use disorder; ICD-9, international classification of diseases.
FIGURE 8.
Prevalence of drug use disorders (DUDs) among US veterans reported by studies with representative sampling methods using diagnostic (ie, DSM) criteria (Panel A) and administrative (ie, ICD-9) criteria (Panel B), by publication year. Note: black solid lines represent trend lines, calculated using weighted least squares regression. AUD, alcohol use disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ICD-9, international classification of diseases.
DISCUSSION
Summary
The results of this systematic review suggest that the prevalence of AUDs and DUDs reported in studies sampling US veterans using diagnostic criteria are generally higher than studies using administrative records abstraction, although differences have diminished over time. It is important to note that diagnoses of AUDs using either assessment method have shown a gradual decline in the past 20 years, although the decline is greater in studies using diagnostic criteria than those using administrative criteria. A similar trend was also observed in the sub-analysis that only included the studies that were representative or were general VA samples. Among studies assessing DUDs, those using diagnostic criteria have shown a gradual decrease in the prevalence of DUDs. Notably, this decline in DUD prevalence was not observed in the sub-analysis that only included the studies that were representative or had general VA samples. Studies using administrative criteria suggest that the prevalence of DUDs has been largely stable. Research to further investigate DUD prevalence by assessment method, including for example studies specifying the type of drug abuse among US veterans with DUDs, may be informative.
The decline of reported AUDs in studies sampling US veterans may be attributed to targeted interventions and increased awareness of alcohol use among the veteran populations. However, relatively high rates of AUDs and DUDs among studies sampling US veterans remain a significant public health concern. The observed prevalence of AUD and DUD diagnoses in the sample of veterans were higher than civilians. Notably, rates of AUD diagnoses (10.5% for men and 4.5% for women) for OEF/OIF veterans reported by Seal et al.,84 were higher than civilian AUD prevalence, which generally range from 3.1% to 8.5%.91 In the study, 4.5% of the veterans received a DUD diagnosis, which is higher than DUD prevalence estimates among civilians, which have been reported to be approximately, 1.4–2.0%.92–94 Overall, the results of this systematic review are broadly consistent with the results of a DoD and VA survey of returning veterans from the current conflicts (ie, OEF/OIF/OND), suggesting that SUDs continue to affect large numbers of veterans.7
High rates of PTSD comorbidity with SUDs, particularly among veterans with other mental health problems, have also been reported.62,83 The average prevalence of post-traumatic stress disorder (PTSD) was found to be different across the two types of assessments (19% among studies using diagnostic criteria and 10% among studies using administrative criteria). A recent study found that, of those with co-occurring AUD and DUD, 75% received a comorbid PTSD diagnosis.84 Several studies have hypothesized that self-medication of mental health symptoms, such as PTSD, may drive comorbidity with SUDs.95,96 With an increasing prevalence of PTSD among OEF/OIF veterans who are mostly under age 45, the continued development of interventions to target this population to address co-morbid psychiatric and SUDs are needed. Further research is needed to analyze the temporal trends of PTSD prevalence in studies sampling US veterans, and within sub-groups of particularly high-risk veterans, to identify the need for and potential benefits of targeted interventions addressing SUD and PTSD comorbidity. Some studies have shown that interventions to reduce stigma, encourage utilization of confidential treatment programs, and eliminate other social and systematic barriers to care may be effective at decreasing the likelihood of chronic SUDs, relapse, or initiation among veterans with mental health problems, including PTSD.97,98 Dual-track PTSD-SUD treatment and coordinated SUD and PTSD care may help reduce morbidity and mortality among those with comorbid SUDs and PTSD.62
Study Implications
It has been estimated that only one-third of all eligible veterans utilize Department of Human Assistance (DHA) health care facilities and mental health services,99 and many of those in need of mental health services seek non-VA primary care clinics.100 Therefore, continued improvements in access to care and increased VA healthcare service utilization, particularly for SUDs, are needed. There is also a strong need to increase awareness of veterans’ issues regarding mental health and substance use disorders in primary health care settings, particularly in light of the many challenges that may arise when veterans reintegrate into families. Several interventions hold promise. For example, the American Academy of Family Physicians and other primary care physician organizations developed the patient-centered medical home (PCMH) as a comprehensive model of care for children, youth, and adults, with a focus on family centered care to promote the overall health and care of the patient.101 This model has been adopted by the VA and tailored for veterans, named the Patient Aligned Care Teams (PACT). This approach emphasizes team-based care, offers multiple ways to access health care, and seeks to meet individualized health goals. In addition, the Substance Use Disorder QUERI Strategic Plan works in partnership with the VA Office of Mental Health Services (OMHS), with the goal of improving accessibility, quality, effectiveness, and efficiency of SUD specialty treatment, treatment within VA medical settings, and improve integrated treatment of SUD and co-morbidities.102 Research is needed to identify whether such programs result in improved recognition and treatment of US veterans with alcohol and drug use disorders.
These findings may be helpful in designing programs to meet the psychiatric needs of veterans, including those from different war eras. The data suggest that there is a need to expand the use of SUD screening tools, in addition to the screening and social media campaigns that have been recently implemented by the US Armed Forces to address high-risk drinking and reduce alcohol-related problems among military personnel.84 Currently, the VA does not recommend universal screening for non-alcohol substance use disorders, given the relatively lower rate of DUD diagnoses among veterans accessing VA health care compared to AUD.7 This likely reflects the unclear value of screening and brief interventions for DUD in general healthcare settings.103–105 However, our findings suggest that the true prevalence of DUDs may be higher than that indicated by administrative data, particularly among veterans with co-morbid mental health problems. Notably, veterans with dual diagnoses of SUDs and mental disorders such as PTSD often have more severe symptoms and poorer treatment outcomes than individuals with single, non-substance use mental health disorders.106–109 Furthermore, previous studies have shown that there are unmet SUDs treatment needs among veterans.32,110 Therefore, research on developing more effective strategies to identify and address SUDs in veterans, particularly for those with previous mental health diagnoses, is needed. Finally, further research is needed to evaluate and improve the reliability of clinical diagnoses for DUDs against “gold standard” diagnostic assessments among US veterans.
Given that a considerable proportion of US veterans do not use VA health care,111 these findings also have implications for non-VA health care providers. Clinicians treating veterans in non-VA settings (assisted living facilities, nursing homes, and general clinics serving veterans) should consider assessing patients and clients for both alcohol and drug use disorders. The provision of psycho-education has been recommended as a method to destigmatize problem drug use, manage craving to use, and improve care for veterans with DUDs.84,112 Healthcare outside of VA should utilize appropriate diagnostic screening tools to assess SUDs in veterans.
These study findings indicate that there has been a gradual decrease in AUD prevalence reported in both the studies using diagnostic and those using administrative criteria sampling US veterans over the past 20 years. It is important to note, however, that the majority of the studies report data collection in the 1990s, with a few in the early 2000s, and only one study collected data until 2010. Therefore, few studies reflect the experiences of more recent OEF/OIF veterans. In contrast, data from the recent National Survey on Drug Use and Health (NSDUH) suggests that the prevalence of persons with any substance use disorder (including AUDs) in the general US population has been stable since at least 2010 (ranging from 20.6 to 22.7 million Americans).93 The differences in SUD trends between the general population and US veterans could be attributed to the variations in the age structure between the two populations. Specifically, the gradual decline of AUD prevalence among studies sampling US veterans could be a result of the continuing trend of the aging veteran population. For example, between 1992 and 2013, the percentages of veterans under the age of 45 decreased (32% vs. 21%), while the proportion above the age of 65 increased (38% vs. 26%).113 However, further studies are needed to examine more current trends in the prevalence of SUDs among US veterans, particularly veterans of more recent conflicts.
Limitations
The findings of this study should be interpreted with caution and in the context of several potential limitations. First, since one of our goals was to compare administrative and diagnostic criteria, we did not include studies that reported prevalence based on screening efforts alone. Second, administrative data reflect diagnoses assigned by clinicians to patients during their episodes of inpatient and outpatient care. In these settings, patients with less severe SUDs may go undiagnosed. Several studies have suggested that clinicians within the VHA routinely under-diagnose SUDs.84,114 Since the majority of the studies did not report the specific ICD-9 codes used to identify AUDs and DUDs, we were unable to compare and contrast the similarities and differences between the codes utilized in administrative data. Despite this potential limitation, the use of VA administrative data provides important information from all veterans treated in facilities throughout the country, and offers the benefits of examining the prevalence and correlates of SUDs in a large national cohort of US veterans with the caveat of differential access to medical care.
Third, we note that some of the studies using both administrative data and diagnostic criteria sampled veterans who may have a significantly elevated rate of SUDs compared to the general veterans population. These include, for example, HIV-infected veterans, homeless veterans, veterans with PTSD, and those sampled from inpatient clinical settings. Differences in sampling design and other study methods likely account for some of the observed variation in SUD prevalence, even among studies using similar assessment methodology and recruiting veterans from the same era. To reduce variability, we excluded studies that sampled veterans entirely from substance abuse treatment programs. In sensitivity analyses, we excluded studies sampling veterans of specific clinical interest (eg, those with spinal cord injuries, homeless veterans, and veterans with PTSD), and found that trends did not differ substantially in this sub-group.
Fourth, the differences in study design, survey, and screening methodologies among the eligible studies may have limited the implications of this review, particularly the assessment of trends in prevalence over time. For example, variation in the assessment periods for the studies included in the final analyses may have accounted for some of the observed changes in SUD prevalence over time, and may not be representative of the true trends in prevalence of SUDs among larger US veteran populations. Notably, the studies included in this analysis have significant heterogeneity in terms of the timeframe for assessment and the population studied. The majority (70%) of the 37 studies using diagnostic criteria measured lifetime SUDs, whereas only 14% of the 35 studies using administrative assessment method reported lifetime prevalence. The sub-analyses for lifetime and past year AUDs and DUDs show that the two assessment methods suggest similar time trends for AUDS but differ in DUDs. Therefore, some of the observed differences in pooled SUD prevalence across the two assessment methods and trends over time may have been due to variations in the recall periods (ie, lifetime prevalence versus past-year). The findings point to the need to collect and report consistent assessment periods in order to improve comparability of the prevalence of SUDs across studies and also over time.
Fifth, we note that assessing the temporal trends by the year of data collection (rather than publication year) may have provided a more accurate characterization of the changes in SUD prevalence over time. However, we were unable to do so with all the eligible studies, as many of them did not report the years of data collection (more than half of the studies using clinical diagnosis criteria and more than one-fifth of the studies using administrative criteria), reported only the era from which the veterans were sampled (eg, Vietnam), or only provided a broad time frame during which the data was collected. Therefore, we were only able to conduct a sub-analysis among 17 studies using clinical diagnostic criteria and 26 studies using administrative criteria that reported these dates. The findings show similar time trends as in the main analyses using publication dates; however, we did observe that administrative studies are more common in recent years of data collection. We also acknowledge that, due to OEF and OIF, there is an important shift in the characteristics of veterans after 2001, and this analysis may be limited in identifying specific changes in SUD prevalence among OEF/OIF veterans over the past decade.
Sixth, even though meta-analytic techniques offer a more rigorous evaluation of prevalence and other effect estimates, we did not conduct a meta-analysis due to the fact that our target population has changed substantially over time. Instead of pooling these data together to produce one summary effect, we were interested in identifying long-term trends in SUD prevalence reported in the studies sampling US veterans and in determining the qualitative differences between administrative and diagnostic assessments. Seventh, even though the definition of substance abuse/dependence in DSM-V was recently updated in May 2013, this study still reports on substance abuse/dependence using DSM-IV and DSM-III-R diagnostic criteria due to the fact that the majority of the eligible studies still assessed substance abuse/dependence in this manner. Further research is needed to identify the differences between various diagnostic tools and its impact on estimating the prevalence of SUD among US veterans. Additionally, DUDs assessed in the sampled studies may have included a variety of single substance or polysubstance use disorders, and may not adequately capture a particular drug of abuse in the sampled population. Finally, we note that our results are based primarily on the selected studies and may not be generalizable to all US veterans from all eras.
CONCLUSIONS
In summary, the findings show that studies using diagnostic criteria reported higher rates of SUDs (including both AUDs and DUDs) compared to studies using administrative criteria, although the differences have diminished over time. These findings have particularly important implications for research assessment and prevalence estimates of SUDs among US veterans. Specifically, the data show that resources and programs to expand SUDs screening in US veterans populations are needed, given the higher prevalence of SUDs reported in the studies sampling US veterans using diagnostic criteria. The military now conducts universal screening for high-risk alcohol use.7 Yet, neither VA nor the military conducts universal screening for non-alcohol substance misuse.84 Given the significant public health problems of SUDs among US veterans, this population should receive increased clinical attention. There is potential merit in universal SUDs screening and the guideline for universal SUDs screening should be reconsidered for this population. In summary, these findings may inform VA and other healthcare systems in improved clinical diagnosis, prevention, and intervention for SUDs among US veterans.
Acknowledgments
This work was supported in part by grant U24-AA022000 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Dr. Edelman is funded by the Yale Drug Abuse, Addiction and HIV Research Scholars (DAHRS) Program (K12-DA-33312-03). Dr. Maisto is supported by grant K05-AA16928 (NIAAA). Dr. Marshall is supported by a Richard B. Salomon Faculty Research Award from Brown University.
The funders of this study had no further role in its design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- 1.National Institutes on Drug Abuse (NIDA) [last accessed 24 Mar, 2014];Substance Abuse among the Military, Veterans, and their Families—April 2011; Topics in Brief. NIDA. Available from: http://www.drugabuse.gov/publications/topics-in-brief/substance-abuse-among-military-veterans-their-families.
- 2.Institute of Medicine (IOM) Substance use disorders in the US Armed Forces. The National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- 3.Hawkins EJ, Grossbard J, Benbow J, et al. Evidence-based screening, diagnosis, and treatment of substance use disorders among veterans and military service personnel. Mil Med. 2012;177:29–38. doi: 10.7205/milmed-d-12-00125. [DOI] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration (SAMSHA) The NSDUH Report: Serious Psychological Distress and Substance Use Disorder among Veterans. Office of Applied Studies, SAMHSA; Rockville, MD: 2007. [Google Scholar]
- 5.Rosen CS, Kuhn E, Greenbaum MA, et al. Substance abuse-related mortality among middle-aged male VA psychiatric patients. Psychiatr Serv. 2008;59:290–296. doi: 10.1176/ps.2008.59.3.290. [DOI] [PubMed] [Google Scholar]
- 6.Davis TM, Bush KR, Kivlahan DR, et al. Screening for substance abuse and psychiatric disorders among women patients in a VA Health Care System. Psychiatr Serv. 2003;54:214–218. doi: 10.1176/appi.ps.54.2.214. [DOI] [PubMed] [Google Scholar]
- 7.Department of Veterans Affairs . VA/DoD Clincial Practice Guideline For Management of Substance Use Disorders (SUD) Department of Veterans Affairs and Department of Defense; Washington, DC: 2009. [Google Scholar]
- 8.Gordon AJ, Trafton JA, Saxon AJ, et al. Implementation of buprenorphine in the Veterans Health Administration: Results of the first 3 years. Drug Alcohol Depend. 2007;90:292–296. doi: 10.1016/j.drugalcdep.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Calhoun PS, Elter JR, Jones ERJ, et al. Hazardous alcohol use and receipt of risk-reduction counseling among US veterans of the wars in Iraq and Afghanistan. J Clin Psychiatry. 2008;69:1686–1693. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- 10.Jakupcak M, Luterek J, Hunt S, et al. Post-traumatic stress and its relationship to physical health functioning in a sample of Iraq and Afghanistan War veterans seeking postdeployment VA health care. J Nerv Ment Dis. 2008;196:425–428. doi: 10.1097/NMD.0b013e31817108ed. [DOI] [PubMed] [Google Scholar]
- 11.Hoggatt KJ, Jamison AL, Lehavot K, et al. Alcohol and drug misuse, abuse, and dependence in women veterans. Epidemiol Rev. 2015;37:23–37. doi: 10.1093/epirev/mxu010. [DOI] [PubMed] [Google Scholar]
- 12.Kelsall HL, Wijesinghe MS, Creamer MC, et al. Alcohol use and substance use disorders in Gulf War, Afghanistan, and Iraq War veterans compared with nondeployed military personnel. Epidemiol Rev. 2015;37:38–54. doi: 10.1093/epirev/mxu014. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine (IOM) Returning home from Iraq and Afghanistan: Assessment of readjustment needs of veterans, service members, and their families. The National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- 14.Boole G. The Mathematical Analysis of Logic: Philosophical Library. 1847.
- 15.Robins LN, Helzer JE, Croughan J, et al. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 16.First MB, Sptizer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- 17.Robins LN, Wing J, Wittchen HU, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 18.Hasin DS, Trautman KD, Miele GM, et al. Psychiatric Research Interview for Substance and Mental Disorders (PRISM): Reliability for substance abusers. Am J Psychiatry. 1996;153:1195–1201. doi: 10.1176/ajp.153.9.1195. [DOI] [PubMed] [Google Scholar]
- 19.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 20.Balan S, Widner G, Shroff M, et al. Drug use disorders and post-traumatic stress disorder over 25 adult years: Role of psychopathology in relational networks. Drug Alcohol Depend. 2013;133:228–234. doi: 10.1016/j.drugalcdep.2013.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Black DW, Carney CP, Forman-Hoffman VL, et al. Depression in veterans of the first Gulf War and comparable military controls. Ann Clin Psychiatry. 2004;16:53–61. doi: 10.1080/10401230490452645. [DOI] [PubMed] [Google Scholar]
- 22.Callaghan EH, Radnitz CL, Tirch DD, et al. Is benzodiazepine use related to substance misuse history in veterans with SCI? SCI Psychosocial Process. 1996;9:103–106. [Google Scholar]
- 23.Crawford EF, Fulton JJ, Swinkels CM, et al. Diagnostic efficiency of the AUDIT-C in US veterans with military service since September 11, 2001. Drug Alcohol Depend. 2013;132:101–106. doi: 10.1016/j.drugalcdep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 24.David D, Kutcher GS, Jackson EI, et al. Psychotic symptoms in combat-related post-traumatic stress disorder. J Clin Psychiatry. 1999;60:29–32. doi: 10.4088/jcp.v60n0106. [DOI] [PubMed] [Google Scholar]
- 25.David D, Woodward C, Esquenazi J, et al. Comparison of comorbid physical illnesses among veterans with PTSD and veterans with alcohol dependence. Psychiatr Serv. 2004;55:82–85. doi: 10.1176/appi.ps.55.1.82. [DOI] [PubMed] [Google Scholar]
- 26.Dickerson DL, O’Malley SS, Canive J, et al. Nicotine dependence and psychiatric and substance use comorbidities in a sample of American Indian male veterans. Drug Alcohol Depend. 2009;99:169–175. doi: 10.1016/j.drugalcdep.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ditre JW, Radnitz CL. Pre- and postinjury substance misuse among veterans with spinal cord injury. Rehab Psychol. 2005;50:142–148. [Google Scholar]
- 28.Fiedler N, Ozakinci G, Hallman W, et al. Military deployment to the Gulf War as a risk factor for psychiatric illness among US troops. Br J Psychiatry. 2006;188:453–459. doi: 10.1192/bjp.188.5.453. [DOI] [PubMed] [Google Scholar]
- 29.Fu Q, Heath AC, Bucholz KK, et al. Shared genetic risk of major depression, alcohol dependence, and marijuana dependence: Contribution of antisocial personality disorder in men. Arch Gen Psychiatry. 2002;59:1125–1132. doi: 10.1001/archpsyc.59.12.1125. [DOI] [PubMed] [Google Scholar]
- 30.Fu Q, Heath AC, Bucholz KK, et al. A twin study of genetic and environmental influences on suicidality in men. Psychol Med. 2002;32:11–24. doi: 10.1017/s0033291701004846. [DOI] [PubMed] [Google Scholar]
- 31.Gale CR, Deary IJ, Boyle SH, et al. Cognitive ability in early adulthood and risk of 5 specific psychiatric disorders in middle age: The Vietnam experience study. Arch Gen Psychiatry. 2008;65:1410–1418. doi: 10.1001/archpsyc.65.12.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Golub A, Vazan P, Bennett AS, et al. Unmet need for treatment of substance use disorders and serious psychological distress among veterans: A nationwide analysis using the NSDUH. Mil Med. 2013;178:107–114. doi: 10.7205/milmed-d-12-00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grand RBG, Hwang S, Han J, et al. Short-term naturalistic treatment outcomes in cigarette smokers with substance abuse and/or mental illness. J Clin Psychiatry. 2007;68:892–898. doi: 10.4088/jcp.v68n0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grossman LS, Willer JK, Stovall JG, et al. Underdiagnosis of PTSD and substance use disorders in hospitalized female veterans. Psychiatr Serv. 1997;48:393–395. doi: 10.1176/ps.48.3.393. [DOI] [PubMed] [Google Scholar]
- 35.Hamner MB. Psychotic features and combat-associated PTSD. Depress Anxiety. 1997;5:34–38. doi: 10.1002/(sici)1520-6394(1997)5:1<34::aid-da6>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 36.Hamner MB, Frueh BC, Ulmer HG, et al. Psychotic features and illness severity in combat veterans with chronic post-traumatic stress disorder. Biol Psychiatry. 1999;45:846–852. doi: 10.1016/s0006-3223(98)00301-1. [DOI] [PubMed] [Google Scholar]
- 37.Herrmann N, Eryavec G. Lifetime alcohol abuse in institutionalized World War II veterans. Am J Geriatr Psychiatry. 1996;4:39–45. doi: 10.1097/00019442-199624410-00005. [DOI] [PubMed] [Google Scholar]
- 38.Humphreys KL, Foley KM, Feinstein BA, et al. The influence of externalizing comorbidity on psychophysiological reactivity among veterans with post-traumatic stress disorder. Psychol Trauma. 2012;4:145–151. [Google Scholar]
- 39.Joseph CL, Ganzini L, Atkinson RM. Screening for alcohol use disorders in the nursing home. J Am Geriatr Soc. 1995;43:368–373. doi: 10.1111/j.1532-5415.1995.tb05809.x. [DOI] [PubMed] [Google Scholar]
- 40.Kasprow WJ, Rosenheck R. Substance use and psychiatric problems of homeless Native American veterans. Psychiatr Serv. 1998;49:345–350. doi: 10.1176/ps.49.3.345. [DOI] [PubMed] [Google Scholar]
- 41.Kausch O. Suicide attempts among veterans seeking treatment for pathological gambling. J Clin Psychiatry. 2003;64:1031–1038. doi: 10.4088/jcp.v64n0908. [DOI] [PubMed] [Google Scholar]
- 42.Kilbourne AM, Bauer MS, Pincus H, et al. Clinical, psychosocial, and treatment differences in minority patients with bipolar disorder. Bipolar Disord. 2005;7:89–97. doi: 10.1111/j.1399-5618.2004.00161.x. [DOI] [PubMed] [Google Scholar]
- 43.Miller LN, Chard KM, Schumm JA, et al. The impact of endorsing Spitzer’s proposed criteria for PTSD in the forthcoming DSM-Von male and female Veterans. J Anxiety Disord. 2011;25:639–644. doi: 10.1016/j.janxdis.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Miller MW, Fogler JM, Wolf EJ, et al. The internalizing and externalizing structure of psychiatric comorbidity in combat veterans. J Trauma Stress. 2008;21:58–65. doi: 10.1002/jts.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller MW, Reardon AF, Wolf EJ, et al. Alcohol and drug abuse among US veterans: Comparing associations with intimate partner substance abuse and veteran psychopathology. J Trauma Stress. 2013;26:71–76. doi: 10.1002/jts.21773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morton JL, Jones TV, Manganaro MA. Performance of alcoholism screening questionnaires in elderly veterans. Am J Med. 1996;101:153–159. doi: 10.1016/s0002-9343(96)80069-6. [DOI] [PubMed] [Google Scholar]
- 47.O’Toole TP, Conde-Martel A, Gibbon JL, et al. Health care of homeless veterans. J Gen Intern Med. 2003;18:929–933. doi: 10.1046/j.1525-1497.2003.21209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Orsillo SM, Weathers FW, Litz BT, et al. Current and lifetime psychiatric disorders among veterans with war zone-related post-traumatic stress disorder. J Nerv Ment Dis. 1996;184:307–313. doi: 10.1097/00005053-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 49.Ouimette PC, Wolfe J, Chrestman KR. Characteristics of post-traumatic stress disorder-alcohol abuse comorbidity in women. J Subst Abuse. 1996;8:335–346. doi: 10.1016/s0899-3289(96)90188-1. [DOI] [PubMed] [Google Scholar]
- 50.Sajatovic M, Bauer MS, Kilbourne AM, et al. Self-report medication treatment adherence among veterans with bipolar disorder. Psychiatr Serv. 2006;57:56–62. doi: 10.1176/appi.ps.57.1.56. [DOI] [PubMed] [Google Scholar]
- 51.Wagner TH, Harris KM, Federman B, et al. Prevalence of substance use disorders among veterans and comparable nonveterans from the National Survey on Drug Use and Health. Psychol Serv. 2007;4:149–157. [Google Scholar]
- 52.Westermeyer J, Canive J, Thuras P, et al. Mental health of non-gamblers versus “normal” gamblers among American Indian veterans: A community survey. J Gambl Stud. 2008;24:193–205. doi: 10.1007/s10899-007-9084-2. [DOI] [PubMed] [Google Scholar]
- 53.White R, Barber C, Azrael D, et al. History of military service and the risk of suicidal ideation: Findings from the 2008 national survey on drug use and health. Suicide Life Threat Behav. 2011;41:554–561. doi: 10.1111/j.1943-278X.2011.00053.x. [DOI] [PubMed] [Google Scholar]
- 54.Yovtcheva SP, Rifai MA, Moles JK, et al. Psychiatric comorbidity among hepatitis C-positive patients. Psychosomatics. 2001;42:411–415. doi: 10.1176/appi.psy.42.5.411. [DOI] [PubMed] [Google Scholar]
- 55.Grant JD, Lynskey MT, Scherrer JF, et al. A cotwin-control analysis of drug use and abuse/dependence risk associated with early onset cannabis use. Addict Behav. 2010;35:35–41. doi: 10.1016/j.addbeh.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xian H, Chantarujikapong SI, Scherrer JF, et al. Genetic and environmental influences on post-traumatic stress disorder, alcohol and drug dependence in twin pairs. Drug Alcohol Depend. 2000;61:95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]
- 57.Andersen J, Wade M, Possemato K, et al. Association between post-traumatic stress disorder and primary care provider-diagnosed disease among Iraq and Afghanistan veterans. Psychosom Med. 2010;72:498–504. doi: 10.1097/PSY.0b013e3181d969a1. [DOI] [PubMed] [Google Scholar]
- 58.Anderson BA, Howard MO, Walker RD, et al. Characteristics of substance-abusing veterans attempting suicide: A national study. Psychol Rep. 1995;77:1231–1242. doi: 10.2466/pr0.1995.77.3f.1231. [DOI] [PubMed] [Google Scholar]
- 59.Banerjea R, Findley PA, Smith B, et al. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord. 2009;47:789–795. doi: 10.1038/sc.2009.42. [DOI] [PubMed] [Google Scholar]
- 60.Banerjea R, Pogach LM, Smelson D, et al. Mental illness and substance use disorders among women veterans with diabetes. Womens Health Issues. 2009;19:446–456. doi: 10.1016/j.whi.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 61.Bohnert AS, Ilgen MA, Ignacio RV, et al. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169:64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- 62.Bohnert KM, Ilgen MA, Rosen CS, et al. The association between substance use disorders and mortality among a cohort of Veterans with post-traumatic stress disorder: Variation by age cohort and mortality type. Drug Alcohol Depend. 2013;128:98–103. doi: 10.1016/j.drugalcdep.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 63.Butt AA, Khan UA, McGinnis KA, et al. Co-morbid medical and psychiatric illness and substance abuse in HCV-infected and uninfected veterans. J Viral Hepat. 2007;14:890–896. doi: 10.1111/j.1365-2893.2007.00885.x. [DOI] [PubMed] [Google Scholar]
- 64.Butt AA, McGinnis KA, Skanderson M, et al. Hepatitis C treatment completion rates in routine clinical care. Liver Int. 2010;30:240–250. doi: 10.1111/j.1478-3231.2009.02156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Butt AA, Xiaoqiang W, Budoff M, et al. Hepatitis C virus infection and the risk of coronary disease. Clin Infect Dis. 2009;49:225–232. doi: 10.1086/599371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chermack ST, Bohnert AS, Price AM, et al. Substance use disorders and homicide death in Veterans. J Stud Alcohol Drugs. 2012;73:10–14. doi: 10.15288/jsad.2012.73.10. [DOI] [PubMed] [Google Scholar]
- 67.Conigliaro J, Gordon AJ, McGinnis KA, et al. How harmful is hazardous alcohol use and abuse in HIV infection: Do health care providers know who is at risk? J Acquir Immune Defic Syndr. 2003;33:521–525. doi: 10.1097/00126334-200308010-00014. [DOI] [PubMed] [Google Scholar]
- 68.Copeland LA, Pugh MJ, Hicks PB, et al. Use of obesity-related care by psychiatric patients. Psychiatr Serv. 2012;63:230–236. doi: 10.1176/appi.ps.201100221. [DOI] [PubMed] [Google Scholar]
- 69.Crothers K, Butt AA, Gibert CL, et al. Increased COPD among HIV-positive compared to HIV-negative veterans. Chest. 2006;130:1326–1333. doi: 10.1378/chest.130.5.1326. [DOI] [PubMed] [Google Scholar]
- 70.Edelman EJ, Gordon K, Becker WC, et al. Receipt of opioid analgesics by HIV-infected and uninfected patients. J Gen Intern Med. 2013;28:82–90. doi: 10.1007/s11606-012-2189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Edens EL, Rosenheck RA. Rates and correlates of pathological gambling among VA mental health service users. J Gambl Stud. 2012;28:1–11. doi: 10.1007/s10899-011-9239-z. [DOI] [PubMed] [Google Scholar]
- 72.Freiberg MS, McGinnis KA, Kraemer K, et al. The association between alcohol consumption and prevalent cardiovascular diseases among HIV-infected and HIV-uninfected men. J Acquir Immune Defic Syndr. 2010;53:247–253. doi: 10.1097/QAI.0b013e3181c6c4b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Green TC, Kershaw T, Lin H, et al. Patterns of drug use and abuse among aging adults with and without HIV: A latent class analysis of a US Veteran cohort. Drug Alcohol Depend. 2010;110:208–220. doi: 10.1016/j.drugalcdep.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoblyn JC, Balt SL, Woodard SA, et al. Substance use disorders as risk factors for psychiatric hospitalization in bipolar disorder. Psychiatr Serv. 2009;60:50–55. doi: 10.1176/ps.2009.60.1.50. [DOI] [PubMed] [Google Scholar]
- 75.Howard MO, Walker RD, Suchinsky RT, et al. Substance-use and psychiatric disorders among American Indian veterans. Subst Use Misuse. 1996;31:581–598. doi: 10.3109/10826089609045828. [DOI] [PubMed] [Google Scholar]
- 76.Justice AC, Lasky E, McGinnis KA, et al. Medical disease and alcohol use among veterans with human immunodeficiency infection: A comparison of disease measurement strategies. Med Care. 2006;44:S52–S60. doi: 10.1097/01.mlr.0000228003.08925.8c. [DOI] [PubMed] [Google Scholar]
- 77.Justice AC, McGinnis KA, Atkinson JH, et al. Psychiatric and neurocognitive disorders among HIV-positive and negative veterans in care: Veterans aging cohort five-site study. AIDS. 2004;18:S49–S59. [PubMed] [Google Scholar]
- 78.Kalman D, Lee A, Chan E, et al. Alcohol dependence, other psychiatric disorders, and health-related quality of life: A replication study in a large random sample of enrollees in the Veterans Health Administration. Am J Drug Alcohol Abuse. 2004;30:473–487. doi: 10.1081/ada-120037389. [DOI] [PubMed] [Google Scholar]
- 79.Kilbourne AM, Cornelius JR, Han XY, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord. 2004;6:368–373. doi: 10.1111/j.1399-5618.2004.00138.x. [DOI] [PubMed] [Google Scholar]
- 80.Kilbourne AM, Haas GL, Mulsant BH, et al. Concurrent psychiatric diagnoses by age and race among persons with bipolar disorder. Psychiatr Serv. 2004;55:931–933. doi: 10.1176/appi.ps.55.8.931. [DOI] [PubMed] [Google Scholar]
- 81.McGinnis KA, Fultz SL, Skanderson M, et al. Hepatocellular carcinoma and non-Hodgkin’s lymphoma: The roles of HIV, hepatitis C infection, and alcohol abuse. J Clin Oncol. 2006;24:5005–5009. doi: 10.1200/JCO.2006.05.7984. [DOI] [PubMed] [Google Scholar]
- 82.Pavao J, Turchik JA, Hyun JK, et al. Military sexual trauma among homeless veterans. J Gen Intern Med. 2013;28:S536–S541. doi: 10.1007/s11606-013-2341-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Petrakis IL, Rosenheck R, Desai R. Substance use comorbidity among veterans with post-traumatic stress disorder and other psychiatric illness. Am J Addict. 2011;20:185–189. doi: 10.1111/j.1521-0391.2011.00126.x. [DOI] [PubMed] [Google Scholar]
- 84.Seal KH, Cohen G, Waldrop A, et al. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 85.Shi L, Liu J, Zhao Y. Comparative effectiveness in pain-related outcomes and health care utilizations between veterans with major depressive disorder treated with duloxetine and other antidepressants: A retrospective propensity score-matched comparison. Pain Pract. 2012;12:374–381. doi: 10.1111/j.1533-2500.2011.00495.x. [DOI] [PubMed] [Google Scholar]
- 86.Sloan KL, Montez-Rath ME, Spiro A, 3rd, et al. Development and validation of a psychiatric case-mix system. Med Care. 2006;44:568–580. doi: 10.1097/01.mlr.0000215819.76050.a1. [DOI] [PubMed] [Google Scholar]
- 87.Smith MW, Lemke S, Schaefer J. Substance use disorders and health care costs among veterans affairs nursing home residents. Med Care. 2011;49:538–544. doi: 10.1097/MLR.0b013e318207f257. [DOI] [PubMed] [Google Scholar]
- 88.Striegel-Moore RH, Garvin V, Dohm FA, et al. Psychiatric comorbidity of eating disorders in men: A national study of hospitalized veterans. Int J Eat Disord. 1999;25:399–404. doi: 10.1002/(sici)1098-108x(199905)25:4<399::aid-eat4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 89.Tiwari A, Rajan M, Miller D, et al. Guideline-consistent antidepressant treatment patterns among veterans with diabetes and major depressive disorder. Psychiatr Serv. 2008;59:1139–1147. doi: 10.1176/ps.2008.59.10.1139. [DOI] [PubMed] [Google Scholar]
- 90.VanCott AC, Cramer JA, Copeland LA, et al. Suicide-related behaviors in older patients with new anti-epileptic drug use: Data from the VA hospital system. BMC Med. 2010;8:7. doi: 10.1186/1741-7015-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Compton WM, Thomas YF, Stinson FS, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 93.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 95.Breslau N, Davis GC, Schultz LR. Post-traumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- 96.Chilcoat HD, Breslau N. Post-traumatic stress disorder and drug disorders: Testing causal pathways. Arch Gen Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- 97.Kersting K. Men and depression: Battling stigma through public education. Monitor Psychol. 2005;36 [Google Scholar]
- 98.Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. Am Psychol. 1999;54:765–776. doi: 10.1037//0003-066x.54.9.765. [DOI] [PubMed] [Google Scholar]
- 99.Veterans Health Affairs . Analysis of VA healthcare utilization among US Southwest Asian war veterans: Operation Iraqi Freedom, Operation Enduring Freedom. Office of Public Health and Environmental Hazrads; Washington, DC: 2006. [Google Scholar]
- 100.Engel AG, Aquilino CA. Combat duty in Iraq and Afghanistan and mental health problems. N Engl J Med. 2004;351:1798–1800. [PubMed] [Google Scholar]
- 101.Strenger RJ, DeVoe JE. Policy challenges in building the medical home: Do we have a shared blueprint? J Am Board Fam Med. 2010;23:384–392. doi: 10.3122/jabfm.2010.03.090140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sox-Harris A, Gifford E, Hagedorn H, et al. Substance Use Disorder QUERI Strategic Plan Palo Alto, CA, VA Palo Alto Health Care System. 2011.
- 103.Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: The ASPIRE randomized clinical trial. JAMA. 2014;312:502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA. 2014;312:492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kessler RC, Nelson CB, McGonagle KA, et al. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J Orthopsychiat. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- 107.Ouimette PC, Ahrens C, Moos RH, et al. Post-traumatic stress disorder in substance abuse patients: Relationship to 1-year posttreatment outcomes. Psychol Addict Behav. 1997;11:34–47. [Google Scholar]
- 108.Ouimette PC, Ahrens C, Moos RH, et al. During treatment changes in substance abuse patients with post-traumatic stress disorder. The influence of specific interventions and program environments. J Subst Abuse Treat. 1998;15:555–564. doi: 10.1016/s0740-5472(97)00315-2. [DOI] [PubMed] [Google Scholar]
- 109.Watkins KE, Burnam A, Kung FY, et al. A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatr Serv. 2001;52:1062–1068. doi: 10.1176/appi.ps.52.8.1062. [DOI] [PubMed] [Google Scholar]
- 110.Maust DT, Mavandadi S, Klaus J, et al. Missed oppportunities: Fewer service referrals after positive alcohol misuse screens in VA primary care. Psychiatr Serv. 2014;62:310–312. doi: 10.1176/ps.62.3.pss6203_0310. [DOI] [PubMed] [Google Scholar]
- 111.Bagalman E. The number of veterans that use VA Health Care Services: A Fact Sheet. Vol. R43579. Congressional Research Service; Washington, DC: 2014. [Google Scholar]
- 112.Back SE, Killeen TK, Teer AP, et al. Substance use disorders and PTSD: An exploratory study of treatment preferences among military veterans. Addict Behav. 2014;39:369–373. doi: 10.1016/j.addbeh.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.United States Department of Veterans Affairs . National Survey of Veterans. National Center for Veterans Analysis and Statistics; Washington, DC: 2010. 2011. [Google Scholar]
- 114.Vazan P, Golub A, Bennett AS. Substance use and other mental health disorders among veterans returning to the inner city: Prevalence, correlates, and rates of unmet treatment need. Subst Use Misuse. 2013;48:880–893. doi: 10.3109/10826084.2013.796989. [DOI] [PMC free article] [PubMed] [Google Scholar]