Abstract
Objective:
The administration of chemotherapy forms a major part of the clinical role of oncology nurses. When a mistake is made during chemotherapy administration, admitting and reporting the error timely could save the lives of cancer patients. The main objective of this study was to assess the perceptions of oncology nurses about why chemotherapy administration errors are not reported.
Methods:
This is a descriptive study that surveyed a convenient sample of 128 oncology nurses currently practicing in the Ogun State University Teaching Hospital, Nigeria. The tool for data collection was a structured questionnaire that consisted of two sections. The first section was for the demographic data of participants and the second section consisted of questions constructed based on the Medication Administration Error (MAE) reporting survey developed by Wakefield and his team.
Results:
Findings showed that majority of the nurses (89.8%) have made at least one MAE in the course of their professional practice. Fear (mean = 3.63) and managerial response (mean = 2.87) were the two major barriers to MAE reporting perceived among oncology nurses.
Conclusion:
Critically analyzing why medication errors are not reported among oncology nurses is crucial to identifying strategic interventions that would promote reporting of all errors, especially those related to chemotherapy administration. It is therefore recommended that nurse managers and health care administrators should create a favorable atmosphere that does not only prevent medication errors but also supports nurses’ voluntary reporting of MAEs. Education, information and communication strategies should also be put in place to train nurses on the need to report, if possible prevent, all medication errors.
Keywords: Chemotherapy administration error, cancer, oncology nurse
Introduction
Health care organizations rely on nurses as front-line staff to recognize and report medication errors, irrespective of whether the nurse is the source of the error, a contributor or an observer. Irrespective of the reporting system mechanisms or policies that may be in place, reporting medication errors depends on the nurse's ability to detect errors and make a decision to report the medication errors discovered. Although errors can involve any drug, chemotherapy presents a special and untold danger to cancer patients because many of the agents involved have a relatively narrow therapeutic index and could be very toxic even at therapeutic dosages.[1]
The administration of chemotherapy forms a major part of the clinical roles of oncology nurses. Medication administration is an aspect of a process that also involves the physicians as well as the pharmacists.[2] Proper care is required during chemotherapy administration because chemotherapy regimens are highly complex, making cancer patients highly vulnerable and less tolerant.[3] Some mistakes during chemotherapy occur due to human tendencies while others could be attributed to the nature of the health care system that gives rooms to certain errors. According to Reason,[4] human errors among health care workers arise primarily from aberrant mental processes such as forgetfulness, inattention, poor motivation, carelessness, negligence and recklessness. On the other hand, human beings are fallible and susceptible to errors; therefore, it may be unrealistic to expect that medication errors would not occur at all. In fact, errors are serious and inevitable threats to patients’ safety.[5] Errors such as Medication Administration Errors (MAE) are prevalent everywhere. An incidence of MAEs in the developing countries has been reported.[6]
Statistics show that the number of in-patients who suffer from treatment-related adverse effects has risen from 2.9% to 16.6% in America.[7] An exploratory study conducted among 160 members of the Oncology Nursing Society and 26 non-members confirmed that 63% of all oncology nurses have witnessed MAE at one point or the other during their professional practice, but only 3% of the errors were reported.[8] Patients’ safety has been given so much attention in the health care setting and has been identified as an indication of quality health care delivery. MAE has been observed to be one of the major causes of patients’ death.[9] According to a European study, about 19%-28% of hospitalized patients encounter MAE.[10] Oncology nurses are the group of the health care team who are chiefly saddled with a major responsibility of administering chemotherapy to cancer patients. Consequently, they are to be adequately trained for this purpose. According to the Canadian Adverse Events Study, 7.5% of patients admitted to acute care hospitals in Canada during 2000 experienced an adverse event, with 36.9% of those errors being highly preventable.[11] In their review of the literature, Baker et al.[11] concluded that the situation in Canada is roughly equivalent to that in many other industrialized nations. A study conducted in the University of Pennsylvania reported that 30% of the nurses had committed at least one MAE during the 28 days of the study.[12]
A considerable body of evidence points to medication errors as an important problem. Importantly, however, most of the studies originate from Western nations. There are few relevant data on medication errors in developing countries. A handful of studies have examined the issue in Latin America,[13] the Middle East[14] and Asia,[15] although there is a notable lack of evidence from Africa. There is a pressing need for more studies from these regions where they experience different challenges compared with the Western nations, where the majority of large, high-quality studies have been based.
Efforts to decrease errors in health care are directed at prevention rather than at managing a situation when a mistake has occurred. Consequently, nurses and other health care providers may not know how to respond properly and may lack sufficient support to make a healthy recovery from the emotional response often accompanying making mistakes.[5] Reporting of medication error by oncology nurses should be incorporated in their training. Many institutions prescribe that MAEs be reported through the institutional reporting system such as incidence report.[16] Reporting of chemotherapy administration error appropriately will help prevent any harm that the cancer patient might possibly experience as well as serve as an important source of information that could help prevent similar occurrences. However, health care organizations should establish a culture that recognizes the imperfection of human performance and solicit the assistance of team members in order to recognize and prevent errors.[17]
In a study conducted among Iranian pediatric nurses, it was revealed that 73.9% of participants felt that MAEs occur due to nurses’ inability to properly check medicinal orders, while 64% felt that MAEs occur due to errors in the administration of medication.[18]
It was also reported that 95% of MAEs are not reported due to nurses’ fear of possible consequences.[19,20] In the same vein, 15.8% of the nurses in a study were unsure as to the exact situation that could be described as MAE and 14% were unsure of when to report the errors.[20] Studies have reported that lack of knowledge about the patients and/or patients’ diagnosis, the name, and purpose and correct method of administration of a medication are the common reasons why nurses make an MAE.[20,21]
Nursing students, because of their limited clinical experience, are likely to inadvertently make errors during medication administration. In a 3-year retrospective study conducted by Harding and Petrick,[22] 77 medication errors were reviewed. Findings revealed that rights violations, system factor and knowledge and understanding were major contributory factors to medication error among nursing students. Similarly, a study conducted among nursing students by another researcher revealed that the two major reasons why MEAs are not reported were due to administrative barriers such as its negative consequences and the fear of being tagged as an incompetent nurse.[23] Other studies have reported that the most important barriers to MAE reporting were blaming the individual instead of the system[24] and poor management practice and professional cultures that punish an individual when errors are reported.[25] Because the reporting of MAEs has been linked to reduction of similar errors and improved quality of nursing care, it is therefore very imperative for nurses to always report such incidences.
Elnitsky, Nicholas and Palmer carried out a survey among 424 nurses; 14% did not believe that future occurrences of MAE could be prevented through incidence report, 14% did not believe that reports were valid and reliable and 25% reported that their supervisors or the management would punish them using the incidence report.[26] Wakefield and colleagues reported in their studies that the major reasons why nurses underreport MAEs are: Errors are not recognized, recognized errors are viewed to be harmless, fear of implication and system factor that mounts discouragement of MAE reporting.[27,28,29] This is also similar to the findings of a qualitative study conducted by Sanghera[30] and team exploring the attitudes and beliefs of healthcare professionals toward the cause of MAE underreporting. The study reported that the chief factors were not being aware that an error had occurred, detailed paper work in the process of reporting, perception that reporting is of no benefit and fear of loss of professional license. Studies have shown that between 63% and 84% of nurses did not report MAEs due to fear of negative manager and peer responses.[20,31] However, in another study, pediatric and adult nurses reported that 67% and 56% of all MAEs in their units were reported.[32] Recognition of reasons why medication errors are not reported is crucial to finding the intervention that supports reporting of all errors, especially those related to the administration of chemotherapy.
When a mistake is made during chemotherapy administration, admitting and reporting the error early could save the lives of cancer patients while refusing to report a chemotherapy error can be dangerous and have significant adverse consequences on patients. Currently in Nigeria, the system established to monitor medication errors in the oncology units as well as other hospital wards is by maintaining the incidence report records. This is also similar with other developing countries. Data from these records are not significantly reviewed for the purpose of improving healthcare delivery services. The records do not actually portray the exact situation with regard to the occurrence of medication errors as many nurses no longer have the courage to report their errors due to the traditional culture of blame and punishment that still prevails among supervisors and hospital managers in Nigeria. Some managers go to the extent of dismissing the concerned nurses because their errors were reported.
In the oncology units, chemotherapy administration errors seem to be underreported; hence, the need to find out why nurses refuse to report errors associated with the administration of chemotherapy. Findings from this study will help hospital managers and administrators to plan and establish favorable systems that will promote accurate reporting of chemotherapy errors among nurses. Thus, a quality management process that is perceived by nurses as designed to promote patient's safety as opposed to discover mistakes will be demonstrated. Although many studies have focused on nurses’ barriers to reporting general MAEs, no study has been conducted to assess why chemotherapy administration errors are not reported by oncology nurses in Nigeria.
Materials and methods
This descriptive study was conducted to assess the opinions of oncology nurses about why chemotherapy administration errors are not reported. A convenient sampling technique was used to select 128 nurses who where providing direct care to cancer patients in the Ogun State University Teaching Hospital, a tertiary health institution located in South-West Nigeria. The sampling criterion was nurses who were directly involved in chemotherapy administration. After obtaining the required permission and ethical approval from the ethical review committee of the Hospital, the nurses were verbally informed about the aim of the study, confidentiality of information and their right to withdraw from the study at any time. Participants signed the consent form to indicate their voluntary acceptance to be included in the study. The tool for data collection was a structured questionnaire that consisted of two sections. The first section was for the demographic data of participants and the second section consisted of questions constructed based on the MAE reporting survey developed by Wakefield and his team.[28] This section contained 15 items categorized under four subscales, namely: Disagreement over definition (four items), reporting efforts (two items), fear (five items) and administrative response (four Items). All items in each of the subscales were graded on a five-point Likert scale. Data collected were analyzed with SPSS (Version 16.0) at an alpha level of 0.05. Descriptive statistics included mean and standard deviation while the inferential statistics used was the independent t-test.
Results
Demographic information of the study participants is presented in Table 1. A total of 128 nurses participated in this study (29 males and 99 females). Majority of the participants were married (61.7%), having 4-6 years of professional experience (40.6%) and had made at least one medication error during their practice.
Table 1.
Frequency distribution table of participants’ demographic data (n = 128)
| Variable | Frequency (%) |
|---|---|
| Gender | |
| Male | 29 (22.7) |
| Female | 99 (77.3) |
| Marital status | |
| Single/unmarried | 31 (24.2) |
| Married/partnered | 79 (61.7) |
| Divorced/separated | 8 (6.3) |
| Widowed | 10 (7.8) |
| Years of working experience in cancer care | |
| 1-3 | 35 (27.3) |
| 4-6 | 52 (40.6) |
| 7-9 | 29 (22.7) |
| 10 and above | 12 (9.4) |
| Ever made medication administration errors | |
| Yes | 115 (89.8) |
| No | 13 (10.2) |
Majority of the participants reported that they had made MAEs at one point or the other during their professional practice. Based on their years of experience, all the participants who had 7-9 years of experience (n = 29) and those who had 10 or more years of experience (n = 12) had ever made at least one medication error, while 92.3% (n = 52) of those having 4-6 years of experience and 74.3% of those having 1-3 years of experience (n = 35) had also made at least one medication error [Figure 1].
Figure 1.
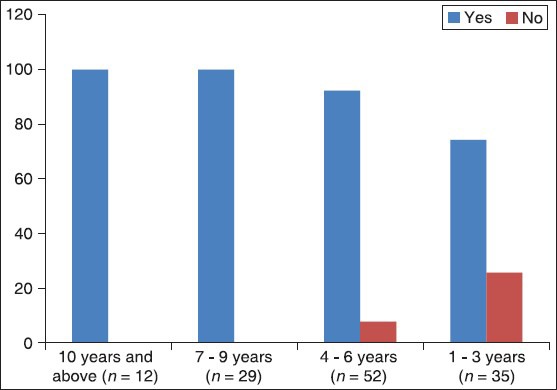
Percentage of participants who had ever made medication administration errors according to their years of working experience in cancer care (Note: Vertical axis is represented in percentage)
Table 2 shows the mean and standard deviation of reasons why medication errors are not reported by nurses. Seven of 15 items have a mean over 3.0. Item 11 has the highest mean of 3.73 and SD of 0.92, indicating the most important barrier, inferring that nurses fear that they could be blamed if something happens to the patients as a result of the medication error. Other important barriers were “the patient or family might develop a negative attitude towards the nurse or may sue the nurse if a medication error is reported,” “nurses fear adverse consequences from reporting medication errors,” “nurses are afraid the physician or supervisors would reprimand them for the medication error” and “the response by nursing administration/supervisors does not match the severity of the error.” Item 2 (mean = 1.62) and Item 4 (mean =1.76) were the only two items that ranked below 2.0.
Table 2.
Barriers to medication administration error reporting
| Item | All | Females | Males | P |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Nurses do not agree with the hospital’s definition of medication error | 2.29±0.88 | 2.68±0.84 | 2.19±0.86 | 0.000* |
| Nurses do not recognize when an error occurs | 1.62±0.91 | 2.02±1.13 | 1.52±0.81 | 0.002* |
| Medication error is not clearly defined | 2.36±1.14 | 2.68±1.12 | 2.27±1.13 | 0.023* |
| Nurses may not think the error is important to be reported | 1.76±1.21 | 1.99±0.99 | 2.10±1.11 | 0.091 |
| Filling out an incidence report for medication error takes too much time | 2.83±1.20 | 3.20±1.21 | 2.73±1.18 | 0.023* |
| Contacting the physician about a medication error takes too much time | 2.55±1.32 | 3.28±1.54 | 2.36±1.18 | 0.000* |
| Nurses believe that other nurses will think they are incompetent if they report a medication error | 3.49±0.98 | 3.75±0.82 | 3.43±1.01 | 0.040* |
| The patient or family might develop a negative attitude toward the nurse or may sue the nurse if a medication error is reported | 3.68±1.63 | 4.24±2.11 | 3.56±1.45 | 0.061 |
| Nurses are afraid the physician or supervisors would reprimand them for the medication error | 3.52±0.89 | 3.71±1.11 | 3.45±0.97 | 0.061 |
| Nurses fear adverse consequences from reporting medication errors | 3.65±1.16 | 3.66±1.24 | 3.65±1.15 | 0.851 |
| Nurses could be blamed if something happens to the patients as a result of the medication error | 3.76±0.92 | 3.84±0.79 | 3.74±0.95 | 0.658 |
| No positive feedback is given for passing medication correctly | 2.79±1.16 | 2.53±0.91 | 2.99±0.66 | 0.076 |
| Too much emphasis is placed on medication errors as a measure of the quality of nursing care | 2.06±1.19 | 2.22±1.31 | 2.02±1.16 | 0.380 |
| When medication errors occur, nursing administration focuses on the individual rather than looking at the system as a potential cause of the error | 3.21±1.12 | 3.44±0.99 | 3.31±1.01 | 0.077 |
| The response by nursing administration/supervisors does not match the severity of the error | 3.41±1.01 | 3.72±0.98 | 3.32±1.00 | 0.009* |
*P < 0.05
Table 3 shows the rankings of the subscales. The most significant subscale as perceived by nurses was fear and the least important barrier was disagreement over the definition of medication error.
Table 3.
Rank of subscales as perceived by the participants
| Subgroups | Total mean (divided by number of items in each subgroup) | Rank |
|---|---|---|
| Disagreement over definition | 2.01 | 4 |
| Reporting efforts | 2.69 | 3 |
| Fear | 3.62 | 1 |
| Administrative response | 2.87 | 2 |
Discussion
The best option to reduce chemotherapy errors and possibly promote the reporting of errors is to identify the major barriers that prevent oncology nurses from reporting errors. Findings from this study revealed that majority (89.8%) of the participants had made some MAEs at one point or the other in the course of their professional career. To compare with another study among pediatric nurses in Nigeria, which reported that 64% of the nurses had committed at least one medication error over the course of their career.[33] There seems to be a higher rate of MAE among the participants in the present study. This rate is also higher in comparison with the finding of a research conducted in Jordan that reported that 42.1% of the nurses had made at least one medication error in their career.[4] In Taiwan, a study reported that 66.9% of the nurses had experienced MAEs.[34] Another study reported that the mean rate of MAEs among nurses in Iran was 19.5%.[35] The average number of MAEs reported by nurses in a study conducted in Jordan was 2.2.[6] In a systemic review of the literature on medication errors in 10 Middle East countries, MAE rate was found to vary from 9.4% to 80%.[36] A study conducted at a chemotherapy administration setting in Iran reported that 32.5% errors were detected in the chemotherapy administered to cancer patients, with majority occurring during the preparation of chemotherapy agents.[37] There seems to be a lower rate in a study conducted in another developing country to assess the rate and type of chemotherapy errors in children with acute lymphoblastic leukemia, which reported that 12.5% of the chemotherapy errors occurred in prescription while 7.3% occurred during chemotherapy administration. However, 63% of nurses were reported to have made some errors during chemotherapy in a study published about 15 years ago.[8] The difference in the rates reported in these studies could be as a result of the different settings and methodologies adopted.[38] MAE was observed in the present study to be common among nurses who had worked for more than 6 years in an oncology setting. This can be related to the fact that MAEs may not be totally prevented and the number of errors increases with longer years of professional experience. This does not indicate that more experienced nurses commit most medication errors. The truth of this matter is that the highly experienced nurses are more exposed to various critical situations than the less-experienced nurses. But, making an incidence report whenever MAEs occur could help in reducing its occurrence as well as minimizing harm to the patients.
When comparing the nurses’ perception with their gender, a gender difference was observed in their perceptions of seven barriers. There was a significant difference in the male and female nurses’ perceptions of at least one item in each of the subscales. There seems to be no literature to support the existence of a significant difference between nurses’ perception of MAE reporting barriers and their gender. However, Mrayyan et al.[6] found gender to be the only predictor of medication errors in Jordan.
Why are medication errors not reported?
Compared with the standardized mean of each subscale, fear barrier (mean = 3.62) was considered to be a major barrier [Table 3], of which fear that “nurses could be blamed if something happens to the patients as a result of the medication error” was the factor with the highest mean of 3.76 [Table 2]. One possible explanation for perceiving fear as the most important barrier in the current study is the existence of a punitive approach of addressing medication errors in developing countries. The next barrier under the “fear” subscale was that the patient or family might develop a negative attitude toward the nurse or may sue the nurse if a medication error is reported, followed by the barrier of fear of adverse consequences from reporting medication errors. This finding is in accordance with another study that reported that 95% of MAEs are not reported due to nurses’ fear of possible consequences,[19,20] unlike the findings of Mohammadkarim et al.[25] who reported that “fear” and managerial response were given the same importance. Considering the new trends that are emerging, patients are becoming aware of their rights and nurses are becoming conscious that they could be litigated by patients due to possible and unwanted medical errors. Nurses tend to avoid reporting of medication errors to avoid potential consequences. These excuses were also reported in a similar study conducted in Nigeria.[33] Even in the Western world, fear of legal liability, job threat, economic adverse effect, face-saving concern and adverse consequences of reporting have been identified as the most important barriers to error reporting.[39]
In contrast to this finding, studies conducted in Saudi Arabia reported that fear was not a major reason why MAEs are not reported.[40,41] This discrepancy in the result could be due to the difference in sample size and methodologies. From Table 3, it was observed that administrative response was the next important barrier identified by the nurses. This is similar to a study that reported administrative barriers such as its negative consequences and the fear of being tagged as an incompetent nurse as the two major reasons why MEAs were not reported.[23] However, some researchers identified managerial response as the most important.[25] Blaming the individual instead of the system, which is an item under the administrative response, was observed by another research to be a major barrier.[24] Another study reported that fear and management responses had the same mean and were perceived to be of equal importance.[25] Shratton et al.[32] also reported that managerial response was an important barrier that hindered the voluntary reporting of medication errors.
One of the most difficult aspects of the caregiver-patient relationship in health care is the difficulty of reporting one's own error to the manager or patient. Whereas the principles of ethics demand that any error in patients’ care be reported, actually doing so can be difficult. The managers and even patients in settings where a “no blame” policy does not exist are most likely to take action against the nurse who makes a mistake. On the basis of this, the nurses perceived reporting MAEs as a means to being punished or dismissed. Is it right then for the health personnel to cover up their errors as, without reporting, the management and patients may never be aware of the errors, especially in developing countries where medication error tracking systems are not in place? How would the patient or their relatives receive the information that the illness they were trying to relieve has been aggravated or that their relative may have died due to human errors? These are weighty questions that raise ethical considerations and place the nurses, patients and health care organizations in a dilemma. Mayo and Duncan also reported in their study that the major reasons why nurses do not report MAEs included fear of manager and peer reactions.[42] There has been reported evidence of underreporting of medication error in the developing countries. In Iran, Joolaaee et al.[43] reported a high incidence of MAE with a low reporting rate. The situation in better in Taiwan, with a reporting rate of 52.4%[44] and an 87.7% willingness to report MAEs.[34]
Evidence has shown that underreporting of medication errors may also be observed among physicians. Woolf et al.[45] reported that physicians do not like to reveal or disclose their errors and that when they choose to report, such reports are hardly complete, accurate, free of bias or representative of all errors in health care. Primarily, Woolf and colleagues noted that physicians attempt to cover up their errors for fear that their regulatory bodies may sanction them and because of litigation from the patients or their relations. Reporting medical errors may be viewed by health personnel as a way of calling their competence into question. The fear that their peers or professional bodies may devalue them if it became public knowledge that they were sued for medical error may be a strong factor in the decision not to report. This corroborates the findings of a study conducted in a tertiary referral hospital in central Nigeria, which reported lack of error reporting among doctors.[46]
Nurses and other health care professionals have expressed how they fear the consequences of reporting a medication error because of the disciplinary and professional implications.[47] In an oncology setting, nurses are expected to take responsibility for most chemotherapy administration as well as monitor the prescribing practices of other health professionals in cancer care settings. This can leave the nurses vulnerable and, therefore, their chemotherapy administration practices may be motivated by factors such as fear and professional liability, instead of client safety. It has been advocated by some researchers that chemotherapy safety could be improved through voluntary incidence reporting.[48] However, this can only be achieved in an environment that encourages the same.
Regarding administrative response, many oncology nurses reported that the response by nursing administration/supervisors does not match the severity of the error (mean = 3.41). Although this was not perceived to be a major barrier, it, however, has strong implications, especially when voluntary MAE reporting is being advocated. The least barrier subscale was “disagreement over definition of medication” [Table 3]. Table 1 shows that majority of the nurses admitted to have made at least one medication error, implying that nurses are able to identify when errors occur irrespective of whether they were reported or not. Reporting effort was observed to be the third important barrier subscale primarily due to too much time required to fill out an incidence form (mean = 2.83). This finding shows that if the reporting process requires a significant amount of time and effort, it is less likely to promote voluntary reporting of MAEs, especially when the error is minor.
In studies published about 15 years ago, researchers have assessed occurrences of medication errors and the rate of error reporting among nurses mostly in western countries.[8,16,19,26,27,28,29] Improvements have been recorded in some developed countries with the establishment of a reliable reporting system and elimination of blame culture.[48,49,50] A national and local survey conducted to identify the existence of medical error reporting systems in 16 different countries found that 11 countries had at least one national or local reporting system, while five countries had none in existence.[51] The common features of the reporting systems were confidentiality of the information reported and providing feedback to those involved in the reporting. Unlike the developed countries where advanced systems are in place for detection and reporting of medication errors, many developing countries still lack a credible and valid strategy in this regard.
Conclusion
Critically analyzing why medication errors are not reported among oncology nurses is crucial to identifying strategic interventions that would promote reporting of all errors, especially those related to the administration of chemotherapy. This study found out that fear and managerial response were the two major barriers. If medication errors are used as yardsticks to measure individuals’ performance, then most nurses may be reluctant to report their errors. Some managers focus more on the disciplinary aspect of reporting the medication error rather than identifying measures to normalize the system. The issue of medication error is likely to be even larger from a global perspective. Given the magnitude of the problem, it is imperative to establish systems that consistently disclose potential errors, reduce risks and alleviate the effects of errors.
Implications for nursing practice
This study has indicated that there is a need to create a conducive environment that would support reporting of all errors. Managerial understanding and support will enhance accurate medication error reporting. Attempts to promote medication error reporting among oncology nurses must take into consideration several factors that are present in the organizational and individual levels. Patients’ safety is an important yardstick to measure quality of care. Reporting of medication errors is as important as preventing its occurrence. Although expecting that oncology nurses will report all chemotherapy medication errors may be unrealistic in Nigeria, achieving an optimum level of MAE reporting may be desirable.
Recommendations
Based on the findings of this study, it is therefore recommended that:
Education, information and communication strategies be put in place to train oncology nurses on the need to report all errors involving chemotherapy and other medications.
Accurate and effective feedback should be provided to the oncology nurses regarding how medication error reporting has improved the quality of healthcare and has benefited the organization.
Administrators should focus on the quality of care rather than capitalizing on punishment. This would invariably reduce fear among nurses and promote accurate MAE reporting.
Establish alternative methods that would facilitate voluntary reporting whenever an error occurs during medication administration, taking time required for reporting into consideration.
Multidisciplinary analysis of errors at the system level would be useful to examine errors and eliminate blames and fear.
Limitations
This study was limited by the small sample size selected, which is a small group of all nurses working in oncology settings in Nigeria. Moreover, conducting a study on only one hospital reduces the generalizability of the findings. It is therefore suggested that similar studies should be conducted among a larger sample size and in other settings.
Acknowledgment
The author would like to express his hearty gratitude to all the participants who devoted their time for this study. He would also like to appreciate Mrs. PE Ahuchuba who gave her support. He is whole heartedly thankful to the leadership of the health institutions utilized for this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Schwappach DLB, Hochreutener M, Wernli M. Oncology nurses perception about involving patients in the prevention of chemotherapy Administration error. Oncol Nurs Forum. 2010;37:E84–91. doi: 10.1188/10.ONF.E84-E91. [DOI] [PubMed] [Google Scholar]
- 2.Betz RP, Levy HB. An interdisciplinary method of classifying medication error. Am J Hosp Pharm. 1985;42:1724–32. [PubMed] [Google Scholar]
- 3.Müller T. Typical medication errors in oncology: Analysis and prevention strategies. Onkologie. 2003;26:539–44. doi: 10.1159/000074148. [DOI] [PubMed] [Google Scholar]
- 4.Reason J. Human error: Models and management. BMJ. 2000;320:768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crigger NJ. Always having to say you’re sorry: An ethical response to making mistakes in professional practice. Nurs Ethics. 2004;11:568–76. doi: 10.1191/0969733004ne739oa. [DOI] [PubMed] [Google Scholar]
- 6.Mryyan MT, Shishani K, Al-Faour I. Rate, causes and reporting of medication errors in Jordan: Nurses’ perspective. J Nurs Mang. 2007;15:659–70. doi: 10.1111/j.1365-2834.2007.00724.x. [DOI] [PubMed] [Google Scholar]
- 7.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical Practice Study I. 1991. Qual Saf Health Care. 2004;13:145–51. doi: 10.1136/qshc.2002.003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schulmeister L. Chemotherapy Medication error: Descriptions, severity and contributing factors. Oncol Nurs Forum. 1999;26:1033–42. [PubMed] [Google Scholar]
- 9.Milstein A, Galvin RS, Delbanco SF, Salber P, Buck CR., Jr Improving the safety of health care: The leapfrog initiative. Eff Clin Pract. 2000;3:313–6. [PubMed] [Google Scholar]
- 10.Johnstone MJ, Kanitsaki O. The ethics and practical importance of defining, distinguishing and disclosing nursing errors: A discussion paper. Int J Nurs Stud. 2006;43:367–76. doi: 10.1016/j.ijnurstu.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 11.Baker, GR, Jeffs L, Law M, Norton PG. Improving the safety and quality of health care in Canada. In: MacKinnon NJ, editor. Safe and Effective. The eight essential elements of an optimal medication-use system. Ottawa, ON: Canadian Pharmacists Association; 2007. [Google Scholar]
- 12.Hashemi F. Ethical response to nursing error. J Med Ethics Hist Med. 2008;1:31–45. [Google Scholar]
- 13.Mendonça JM, Lyra DP Jr, Rabelo JS, Siqueira JS, Balisa-Rocha BJ, Gimenes FR, et al. Analysis and detection of dental prescribing errors at primary health care units in Brazil. Pharm World Sci. 2010;32:30–5. doi: 10.1007/s11096-009-9335-7. [DOI] [PubMed] [Google Scholar]
- 14.Khoja T, Neyaz Y, Qureshi NA, Magzoub MA, Haycox A, Walley T. Medication errors in primary care in Riyadh City, Saudi Arabia. East Mediterr Health J. 2011;17:156–9. [PubMed] [Google Scholar]
- 15.Khoo EM, Lee WK, Sararaks S, Abdul Samad A, Liew SM, Cheong AT, et al. Medical errors in primary care clinics — a cross sectional study. BMC Fam Pract. 2012;13:127. doi: 10.1186/1471-2296-13-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wakefield DS, Wakefield BJ, Uden-Holman T, Blegen MA. Perceived barriers in reporting medication errors. Best Pract Benchmarking Healthc. 1996;1:191–7. [PubMed] [Google Scholar]
- 17.Dennison RD. Creating an organizational culture for medication safety. Nurs Clin North Am. 2005;40:1–23. doi: 10.1016/j.cnur.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Seidi M, Zardosht R. Survey of Nurses view points on causes of medicinal error and barriers to reporting in pediatric units in Hospitals of Mashhad University of Medical Sciences. J Fasa Univ Med Sci. 2012;3:142–7. [Google Scholar]
- 19.Gladstone J. Drug administration errors: A study into the factors underlying the occurrence and reporting of drug errors in a district general Hospital. J Adv Nurs. 1995;22:628–37. doi: 10.1046/j.1365-2648.1995.22040628.x. [DOI] [PubMed] [Google Scholar]
- 20.Osborne J, Blais K, Hayes JS. Nurses perception: When is it a medication error? J Nurs Adm. 1999;29:33–8. doi: 10.1097/00005110-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Armitage G, Knapman H. Adverse events in drug administration: A literature review. J Nurs Manag. 2003;11:130–40. doi: 10.1046/j.1365-2834.2003.00359.x. [DOI] [PubMed] [Google Scholar]
- 22.Harding L, Petrick T. Nursing student medication errors: A retrospective review. J Nurs Educ. 2008;47:43–7. doi: 10.3928/01484834-20080101-05. [DOI] [PubMed] [Google Scholar]
- 23.Koohestani HR, Baghcheghi N. Barriers to the reporting of Medication error among nursing students. Aus J Adv Nurs. 2009;27:66–74. [Google Scholar]
- 24.Bayazidi S, Zarezadeh Y, Zamanzadeh V, Parvan K. Medication error reporting rate and its barriers and facilitators among nurses. J Caring Sci. 2012;1:231–6. doi: 10.5681/jcs.2012.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahadori M, Ravangard R, Aghili A, Sadeghifar J, Gharsi Manshadi M, Smaeilnejad J. Factors affecting the refusal of reporting on medication Errors from the nurses Viewpoints: A case study in a Hospital in Iran. ISRN Nurs 2013. 2013 doi: 10.1155/2013/876563. 876563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elnitsky C, Nicholas B, Palmer K. Are Hospital Incidents being reported? J Nurs Adm. 1997;27:40–6. doi: 10.1097/00005110-199711000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Wakefield BJ, Wakefield DS, Uden-Holman T, Blegen MA. Nurses perception of why Medication Administration errors occur. Medsurg Nurs. 1998;7:39–44. [PubMed] [Google Scholar]
- 28.Wakefield DS, Wakefield BJ, Uden-Holman T, Borders T, Blegen M, Vaughn T. Understanding why medication administration errors may not be reported. Am J Med Qual. 1999;14:81–8. doi: 10.1177/106286069901400203. [DOI] [PubMed] [Google Scholar]
- 29.Wakefield BJ, Blegen MA, Uden-Holman T, Vaughn T, Chrichilles E, Wakefield DS. Organizational culture, continous quality quality improvements and medication administration error reporting. Am J Med Qual. 1999;14:73–80. [Google Scholar]
- 30.Sanghera IS, Franklin BD, Dhillon S. The attitudes and beliefs of health care professionals on the causes and reporting of medication errors in a UK intensive care unit. Anaesthesia. 2007;62:53–61. doi: 10.1111/j.1365-2044.2006.04858.x. [DOI] [PubMed] [Google Scholar]
- 31.Karadeniz G, Cakmakci A. Nurses’ perception of Medication errors. Int J Clin Pharm Res. 2007;22:28–33. [PubMed] [Google Scholar]
- 32.Stratton KM, Blegen MA, Pepper G, Vaughn T. Reporting of medication errors by paediatric nurses. J Pediatr Nurs. 2004;19:385–92. doi: 10.1016/j.pedn.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 33.Oshikoya KA, Oreagba IA, Ogunleye OO, Senbanjo IO, MacEbong GL, Olayemi SO. Medication administration errors among paediatric nurses in Lagos public hospitals: An opinion survey. Int J Risk Saf Med. 2013;25:67–78. doi: 10.3233/JRS-130585. [DOI] [PubMed] [Google Scholar]
- 34.Lin YH, Ma SM. Willingness of nurses to report medication administration errors in Southern Taiwan: A cross-sectional survey. Worldviews Evid Based Nurs. 2009;6:237–45. doi: 10.1111/j.1741-6787.2009.00169.x. [DOI] [PubMed] [Google Scholar]
- 35.Jolayi S, Hajibabaei F, Peyrovi H, Haghani H. Review and report the occurrence of errors and their association with the working conditions of nurses working in hospitals of Iran University of medical sciences. Iran J Med Ethics Hist Med [cited May 30] (Persian) 2009. Available from: http://journals.iums.ac.ir_files/pdf/_14785.pdf .
- 36.Alsulami Z, Conroy S, Choonara I. Medication errors in the Middle East countries: A systematic review of the literature. Eur J Clin Pharmacol. 2013;69:995–1008. doi: 10.1007/s00228-012-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tavakoli-Ardakania M, Omidi S, Eshraghi A, Salamzadeh J. Medication errors in administration of chemotherapeutic agents: An observational study. Iranian J Pharm Sci. 2013;9:1–11. Available from: http://www.ijps.ir/article_5713_459.html . [Google Scholar]
- 38.Oberoi S, Trehan A, Marwaha RK. Medication errors on oral chemotherapy in children with acute lymphoblastic leukemia in a developing country. Pediatr Blood Cancer. 2014;61:2218–22. doi: 10.1002/pbc.25203. [DOI] [PubMed] [Google Scholar]
- 39.Travaglia JF, Westbrook MT, Braithwaite J. Implementation of a patient safety incident management system as viewed by doctors, nurses and Allied Health professionals. Health (London) 2009;13:277–96. doi: 10.1177/1363459308101804. [DOI] [PubMed] [Google Scholar]
- 40.Aboshaiqah AE. Barriers in reporting medi cation administration errors as perceived by nurses in Saudi Arabia. Middle-East J Sci Res. 2013;17:130–6. Available from: http://www.idosi.org/mejsr/mejsr17(2)13/1.pdf . [Google Scholar]
- 41.Almutary HH, Lewis PA. Nurses’ willingness to report medication administration errors in Saudi Arabia. Qual Manag Health Care. 2012;21:119–26. doi: 10.1097/QMH.0b013e31825e86c8. [DOI] [PubMed] [Google Scholar]
- 42.Mayo AM, Duncan D. Nurse perceptions of medication errors: What we need to know for patient safety. J Nurs Care Qual. 2004;19:209–17. doi: 10.1097/00001786-200407000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Joolaaee S, Hajibabaee F, Peyravi H, Haghani H. The incidence and report rate of medication errors in Iran. J Med Ethics History Med. 2010;3:65–76. [Google Scholar]
- 44.Chiang HY, Lin SY, Hsu SC, Ma SC. Factors determining hospital nurses’ failures in reporting medication errors in Taiwan. Nurs Outlook. 2010;58:17–25. doi: 10.1016/j.outlook.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 45.Woolf SH, Kuzel AJ, Dovey SM, Phillips RL., Jr A string of mistakes: The importance of cascade analysis in describing, counting and preventing medical errors. Ann Fam Med. 2004;2:317–26. doi: 10.1370/afm.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ajemigbitse AA, Omole MK, Osi-Ogbu OF, Erhun WO. A qualitative study of causes of prescribing errors among junior medical doctors in a Nigeria in-patient setting. Ann Afr Med. 2013;12:223–31. doi: 10.4103/1596-3519.122691. [DOI] [PubMed] [Google Scholar]
- 47.Vincent C. Understanding and responding to adverse events. N Engl J Med. 2003;348:1051–6. doi: 10.1056/NEJMhpr020760. [DOI] [PubMed] [Google Scholar]
- 48.France DJ, Cartwright J, Jones V, Thomson V, Whitelock JA. Improving pediatric chemotherapy safety through voluntary incident reporting: Lessons from the field. J Pediatr Oncol Nurs. 2004;21:200–6. doi: 10.1177/1043454204265907. [DOI] [PubMed] [Google Scholar]
- 49.Stump LS. Re-engineering the medication error reporting process: Removing the blame and improving the system. Am J Health Syst Pharm. 2000;57(Suppl 4):S10–7. doi: 10.1093/ajhp/57.suppl_4.S10. [DOI] [PubMed] [Google Scholar]
- 50.Lehmann DF, Page N, Kirschman K, Sedore A, Guharoy R, Medicis J, et al. Every error is a treasure: Improving medication use with a nonpunitive reporting system. Jt Comm J Qual Patient Saf. 2007;33:401–7. doi: 10.1016/s1553-7250(07)33046-8. [DOI] [PubMed] [Google Scholar]
- 51.Holmström AR, Airaksinen M, Weiss M, Wuliji T, Chan XH, Laaksonen R. National and local medication error reporting systems: A survey of practices in 16 countries. J Patient Saf. 2012;8:165–76. doi: 10.1097/PTS.0b013e3182676cf3. [DOI] [PubMed] [Google Scholar]


