Abstract
Objective:
Scalp cooling (SC) is applied to reduce chemotherapy-induced alopecia (CIA). The aim of this study was to investigate patients’ familiarity and opinions and oncological professionals’ attitude and knowledge about SC in the Netherlands.
Methods:
Ex breast cancer patients, nurses and medical oncologists (MDs) from SC and non-SC hospitals filled out questionnaires.
Results:
The majority of MDs and nurses were satisfied with the results of SC, as were SC patients. Over 33% of MDs and nurses perceived their knowledge level insufficient to inform patients about effectiveness, which was over 43% for information about safety. MDs main reason to not apply SC was doubt about effectiveness and safety. Nurses generally offered SC to a minority of eligible patients. Patients were frequently unfamiliar with SC before diagnosis. Seventy percent of SC patients with insufficient results (20/52) reported to mind it very much. With expected success rates of 35% and 50%, respectively, 36% and 54% of patients would use SC again.
Conclusion:
Room for improvement has been shown for both patients’ familiarity and oncological professionals’ knowledge about SC. Sharing knowledge about results, safety and patients’ experiences will improve patient counseling and SC availability. The results of this survey led to the development of a national standard on CIA and SC.
Keywords: Breast cancer, chemotherapy-induced alopecia, hair loss, patient counseling, scalp cooling
Introduction
Chemotherapy-induced alopecia (CIA) is a frequently occurring side-effect. Patients perceive hair loss as one of the most distressing side-effects of cancer treatment,[1,2,3,4] and often report that they were insufficiently prepared for it.[5] CIA may have a negative impact on body image and quality of life.[2,6] Its impact is however considerably underestimated by both medical oncologists (MDs) and nurses.[7] CIA has received more attention in the literature in recent years,[8,9] including papers about guidance for nurses to inform and support patients who are facing and/or experiencing CIA.[10,11,12,13] Scalp cooling (SC) to prevent CIA has been used since the 70s, with different methods.[14,15,16,17] Today, continuous cooling devices are used most frequently worldwide, but the use varies considerably between countries [Figure 1]. Ongoing trials will be decisive for the Food and Drug Administration (FDA) to approve SC in the USA. As there are no approved agents to prevent CIA in human beings, SC is the only clinically effective method to reduce the burden of this side-effect for our patients.[18,19]
Figure 1.
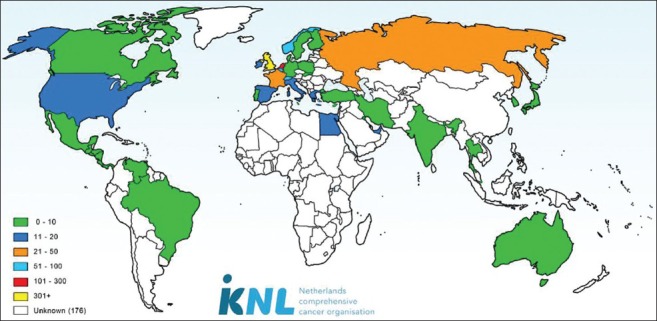
Number of scalp cooling machines worldwide (December 2014)
SC is applied nonstop from about 30 min before initiation until about 90 min after completion of chemotherapy. Cooling causes vasoconstriction in the scalp skin and decreases biochemical activity in the hair follicles, protecting them from damage by cytotoxics.[20] The reported results of SC vary considerably and are mainly determined by the type and dose of the cytotoxics.[21] For example, 8% of the patients were satisfied with the results after TAC chemotherapy (docetaxel, doxorubicine, cyclophosphamide) compared with 95% of the patients after paclitaxel treatment. SC efficacy is high for taxanes, but decreases when used in combination with anthracyclines.[17,21,22,23] Overall, 50% of the patients are satisfied with their hair preservation.[14,21]
SC can be applied during chemotherapy for all solid tumors. However, up to now, it is mainly used by breast cancer patients.[21,24] Breast cancer accounts for 14,000 newly diagnosed Dutch patients each year.[25] The majority of these patients are treated with chemotherapy, and most of them face CIA.
In the Netherlands, about 90 hospitals offer cancer treatment. The number of hospitals using SC has risen from five in 2005 to more than 80 in 2015. This increase has been achieved, among others, by the establishment of a professional Dutch SC network that initiates studies and provides information for patients and oncological professionals. An important source of information is the continuous registration of results,[21] in which the majority of Dutch SC hospitals participate nowadays. SC is however still not offered to a large group of eligible patients[25] and therefore the goal of this study was to evaluate patients’ familiarity and opinions and oncological professionals’ attitude and knowledge about SC. The second goal was to increase patients’ chances of being offered SC during chemotherapy, thereby increasing the chance for hair preservation and contributing to the quality of life of cancer patients.
Materials and methods
Recruitment of respondents
Ex breast cancer patients, nurses and MDs were asked to fill out questionnaires in the period from February to May 2010. Cancer patients were recruited through a patient panel of the Netherlands Comprehensive Cancer Organization (IKNL) in Eindhoven and through the websites of the Dutch SC group (www.geefhaareenkans.nl), the Dutch Breast Cancer Association (BVN) and the Dutch Pink Ribbon Foundation. Nurses were recruited by e-mail through the Dutch national group of specialized oncology nurses (LOOV) and the Mamma Care Nurses Working Group of IKNL. MDs were invited by e-mail via the directors of the (former) eight Comprehensive Cancer Centers of the Netherlands, comprising a complete sample of oncologists in Dutch hospitals.
Questionnaires
All questionnaires were self-developed, as there are no validated questionnaires available on the proposed topics. All questions had predefined response categories, sometimes complemented with an open-answer possibility.
Scalp-cooled (16 questions) and nonscalp-cooled (eight questions) patients were asked about their familiarity with SC prior to diagnosis, satisfaction with information provision, motives for (not) choosing SC and likeliness of choosing SC in the future. The likeliness was assessed for an expected chance for hair preservation of 35% and 50%. Besides, scalp-cooled patients were asked about the tolerance of SC, their experiences with (the probable) hair loss and SC and satisfaction with the final result.
All nurses were asked about reasons for (not) applying SC. Nurses in SC hospitals (35 questions) were also asked about their self-perceived level of knowledge, their efforts to stay up-to-date about the subject and their satisfaction with the results. Furthermore, they were asked about reasons for applying SC, the ratio of offering SC to male and female patients, the proportion of males and females choosing SC and the possible implementation problems at the day care unit. Additionally, they were asked about their need for additional education. Nurses in non-SC hospitals (13 questions) were asked if they would like to introduce SC in their hospital in the future.
All MDs were asked about reasons for (not) applying SC and their self-perceived level of knowledge about the results and safety. In SC hospitals (26 questions), MDs were asked about implementation of SC in their hospital and their satisfaction with the results. MDs in non-SC hospitals (11 questions) were additionally asked about their intention, whether or not to apply it in the future.
Results
Respondents’ characteristics
In total, 178 patients, 64 nurses and 132 MDs returned the questionnaire, but, respectively, one (0.5%), 15 (23%) and 32 (24%) only completed the demographic information and were therefore excluded from the analyses.
All 177 patients were breast cancer patients and 29% had received SC [Table 1]. More than half of the nurses (61%) and MDs (53%) were employed in a hospital where SC was available at that time. The nurses were active as oncology nurse (31%), clinical nurse specialist (18%), nurse practitioner (12%), mamma care nurse (12%) or research nurse (2%). The sub-specialization was unknown for 12 nurses (24%). Sixteen percent of the nurses and 22% of the MDs had less than 5 years of working experience. Nurses in SC hospitals reported to have minimal (27%), moderate (47%) or much (17%) experience with it (missing, n = 3). These figures were, respectively, 10%, 35% and 56% among MDs. Most MDs were employed in nonacademic hospitals [Table 1].
Table 1.
Respondents’ characteristics
| Respondents | Scalp cooling, n (%) | No scalp cooling, n (%) |
|---|---|---|
| Patients (n = 177) | 52 (29) | 125 (71) |
| Nurses (n = 49) | 30 (61) | 19 (39) |
| MDs (n = 100)* | 52 (53) | 47 (47) |
| Academic hospital | 6 (12) | 13 (28) |
| Peripheral training hospital | 7 (13) | 19 (40) |
| Peripheral non-training hospital | 39 (75) | 15 (32) |
*One MD did not know whether scalp cooling was available in the hospital.
Satisfaction with SC information and results
Before diagnosis, 73% of the patients had never heard about SC. Overall, patients were satisfied with the information provision about SC in their hospital (63%) (missing, n = 18). Of the 48 unsatisfied patients, 56% gave the reason that the MD or nurse had not mentioned SC.
In SC hospitals, the majority of MDs (77%, n = 52) and nurses (50%, n = 26) were satisfied with the hair0preservative results, as were scalp-cooled patients (60%, n = 52) (Table 2).
Table 2.
Satisfaction with the scalp cooling results
| Respondent group | Results of scalp cooling, n (%) | |||
|---|---|---|---|---|
| Insufficient | Sufficient | Good | I don’t know | |
| MDs (n = 52)* | 10 (19) | 37 (71) | 3 (6) | 2 (4) |
| Nurses (n = 26)* | 3 (12) | 12 (46) | 1 (4) | 10 (38) |
| Patients (n = 52)* | 20 (38) | 18 (35) | 13 (25) | 1 (2) |
*In scalp cooling hospitals (nurses missing, n = 4)
When SC was not successful (n = 20), 70% of these patients reported to mind it very much or moderately, two patients (10%) were neutral and two patients (10%) reported not to mind it (missing, n = 2). Patients were satisfied with the attention of nurses for hair loss despite SC (70%).
Patients’ experiences with SC
Nine patients (17%) reported SC to not be burdensome at all. Thirty-one (60%) thought it to be minimally burdensome but well tolerable and another nine (17%) patients reported it to be moderately burdensome and not always well tolerable. Two patients (4%) reported to have experienced severe tolerance problems during SC (missing, n = 1).
Half of the scalp-cooled patients reported that they were insecure about the final hair preservative result until the last chemotherapy (50%). Ten patients (19%) were only insecure at the beginning of chemotherapy and 13 patients (25%) reported not to have been insecure (missing, n = 3). Patients’ feelings about SC are displayed in Table 3. Fifty of the 52 patients (96%) would recommend SC to other breast cancer patients (missing, n = 1).
Table 3.
Patients’ feelings about scalp cooling
| Scalp cooling led to* | Patients (n = 52), n (%) |
|---|---|
| Self-esteem | 27 (52) |
| Insecurity | 5 (10) |
| Grief | 3 (6) |
| Disappointment | 14 (27) |
| Deteriorated quality of life | 0 |
| Improved quality of life | 26 (50) |
| Hope | 11 (21) |
*Multiple answers allowed
Offering, choosing and applying SC
The most important reason for patients to choose SC was their own feeling of well-being (56%) or that of their close family and friends (42%) (missing, n = 1). The main reasons why patients had not used SC (n = 125) were because it had not been offered to them (14%), it was not available in their hospital (15%), because of the potential risk of scalp skin metastases (15%), because of the necessary extra time (6%) and because patients were afraid that SC would be too burdensome due to the cold (10%). Finally, some patients had not used SC because they did not perceive hair loss as a problem (7%) or because they were not eligible for it (7%). The remaining patients were not treated with chemotherapy (10%), had other reasons or were missing (16%).
With an expected chance for hair preservation of 35%, 36% of all patients would like to use SC in case of future chemotherapy treatment. This was 54% when the expected success rate would be 50%.
The most frequently mentioned reason for starting SC for both nurses and MDs was that they perceived it as a service for their patients (Table 4a). The most important reason for MDs to not apply SC was lack of evidence about effectiveness and safety. For nurses, the reasons were logistical difficulties and the preference to refer patients to another hospital (Table 4b). Thirteen MDs (28%) and four (20%) nurses of non-SC hospitals reported not to offer it because it would be too burdensome for the patients.
Table 4a.
Reasons of oncological professionals for applying scalp cooling in their hospital
| Reasons for applying scalp cooling* | MDs (n = 52), n (%) | Nurses (n = 30), n (%) |
|---|---|---|
| As a service for patients | 36 (69) | 16 (53) |
| Many patients ask for scalp cooling | 28 (54) | 7 (23) |
| Because nurses requested it | 14 (27) | NA |
| For the image of the hospital | 10 (19) | 8 (27) |
| Patients went to other hospitals for scalp cooling | 6 (12) | 4 (13) |
| Adjacent hospitals were applying it | 4 (8) | 2 (7) |
| Because MDs requested it | NA | 5 (17) |
| I do not know/other | 11 (21) | 10 (33) |
*Multiple answers allowed, NA: Not applicable
Table 4b.
Reasons of oncological professionals for not applying scalp cooling in their hospital
| Reasons for not applying scalp cooling* | MDs (n = 47), n (%) | Nurses (n = 20), n (%) |
|---|---|---|
| Too little evidence on the effectiveness | 29 (62) | 4 (20) |
| Insufficient results | 28 (60) | 6 (30) |
| Too little evidence on the risk of scalp skin metastases in the adjuvant setting | 27 (57) | 6 (30) |
| The schedule of the outpatient clinic does not allow scalp cooling application (logistical difficulties) | 18 (38) | 10 (50) |
| Patients referred to another hospital | 15 (32) | 9 (45) |
| Patients do not ask for it | 13 (28) | 2 (10) |
| It is too burdensome for patients | 13 (28) | 4 (20) |
| Difficult to explain to patients why only a selected group is eligible for scalp cooling | 8 (17) | 2 (10) |
| It is too burdensome for nurses to apply | 6 (13) | 2 (10) |
| One or more colleagues do not want it | 6 (13) | 0 (0) |
| Hair loss can be overcome sufficiently by using wigs or head covers | 5 (11) | 1 (5) |
| Only applying scalp cooling in palliative patients is a too narrow indication | 4 (9) | 1 (5) |
| The nurses do not want it | 2 (4) | NA |
| Do not believe hair loss decreases quality of life | 2 (4) | 0 (0) |
| Afraid too many patients will ask for scalp cooling because of the increasing awareness | 0 (0) | 1 (5) |
| The MDs do not want it | NA | 8 (40) |
| Other | 7 (15) | 4 (20) |
*Multiple answers allowed, NA: Not applicable
Sixty percent of the 20 nurses employed in non-SC hospitals wanted their hospital to start offering SC in the future. In contrast, 16% of the MDs in these hospitals reported to have the intention to apply SC in the future.
Fifteen nurses answered questions about offering and choosing SC. Three of them (20%) reported to offer SC to more than 75% of eligible male patients and two (6%) offered it to 50%-75%. These percentages were higher for eligible female patients (40% and 33%). About 50% of the nurses reported to offer SC rarely (i.e., in 0-5%) to eligible men. One nurse reported to hardly offer SC to eligible female patients as well. Sixty-six percent of the nurses thought that less than 10% of the male patients who are offered SC would choose it, compared with 10% for female patients. Ten MDs (19%) always advised SC to eligible patients, 40% advised it often, 35% sometimes and 6% never.
One nurse and two MDs (4%) reported to have experienced severe problems with the implementation of SC in their hospital, 19% reported no (n = 4, n = 12) and 45% reported minimum (n = 6, n = 31) problems, and 22% did not know whether there had been any problems (n = 11, n = 7). This information was missing for eight nurses (10%).
Knowledge about SC
The percentage of nurses who perceived their knowledge about SC results and safety as sufficient (33%, 43%) was equal to the percentages among MDs (34%, 45%) (Table 5). To keep their knowledge up-to-date, nurses in SC hospitals exchanged information with colleagues (60%), read scientific articles and/or the newsletters of the Dutch SC group (50%), consulted the Dutch SC website (33%) and attended follow-up trainings from the distributor of the SC machines (7%). Four nurses (13%) reported not to make any efforts to stay informed about SC. Sixteen nurses (53%) would prefer more frequent training in applying SC.
Table 5.
Self-perceived satisfaction of oncological professionals on their knowledge about the effectiveness and safety of SC to well-informed patients
| Respondent group | Sufficient knowledge, n (%) | |||||
|---|---|---|---|---|---|---|
| About effectiveness | About safety | |||||
| Yes | No | I don’t know | Yes | No | I don’t know | |
| MDs | ||||||
| Scalp cooling (n = 52) | 27 (52) | 19 (37) | 6 (11) | 35 (67) | 13 (25) | 4 (8) |
| Nonscalp cooling (n = 47) | 16 (34) | 26 (55) | 5 (11) | 21 (45) | 20 (42) | 6 (13) |
| Nurses | ||||||
| Scalp cooling (n = 30) | 10 (33) | 17 (57) | 3 (10) | 13 (43) | 16 (53) | 1 (3) |
Conclusion
This is the first survey addressing patients’ familiarity and opinions and oncological professionals’ attitude and knowledge about SC. It has been shown that there is considerable room for improvement in dissemination of knowledge and in patient counseling. As in the Netherlands, unlike in other countries, there is a professional network for SC, one may expect that the findings of this survey will – even to a greater extent – apply in other countries as well.
Satisfaction with the results of SC was rated sufficient or good by the majority of patients and oncological professionals. This is in accordance with the results in our studies, showing that about 50% of the patients do not need to wear a wig or head cover.[21] Regardless of their own result, almost all scalp-cooled patients would recommend it to other breast cancer patients. Although patients know that hair preservation cannot be guaranteed, one-third of them would start SC when the chance for a good result is 35%. Nevertheless, SC should not be offered to patients with chemotherapy schedules in which chances of hair preservation are minimal;[21] Hair loss in spite of using SC causes an extra burden for patients and it tends to cause a deteriorated body image and quality of life.[2] Patient tolerance of SC was high and in accordance with the literature,[14,22] but it was underestimated by nurses and MDs.
The knowledge about SC proved to be insufficient among oncological professionals, even in hospitals where it was regularly applied. Effectiveness and safety were underestimated; therefore, dissemination of knowledge about these aspects should be improved, even more as they are mentioned as the main reasons for not offering and not choosing SC. Knowledge transfer is important for both MDs and nurses, as in daily practice MDs usually decide whether or not there is an indication for SC, whereas nurses provide more detailed patient information. This information and the nurses’ personal vision about SC will often be decisive for the patient.
SC was only offered to a minority of eligible patients, and it was rarely offered to men, which was also found in another study.[24] However, CIA appeared to be an important side-effect of cancer treatment for males too[3,26] and, when SC was actively offered to them, 37%[22] to 57%[23] chose it. Again, this shows the need for improved information provision.[26]
The familiarity with SC among patients proved to be very low: 73% of them had never heard about it before cancer diagnosis. The familiarity and patient information should be improved, as well-informed patients are more capable of decision making, are more in control of their situation and will have more understanding for medical decisions regarding indications for SC.[27,28]
Most of the scalp-cooled patients who experienced severe hair loss despite SC indicated that it was inconvenient, but they were satisfied with the attention of nurses when CIA had actually occurred. Extra attention should also be paid to the uncertainty about the final result of SC. Therefore, future studies should address the course of CIA during SC.
Now-a-days, most Dutch hospitals use SC. This study showed that in general no implementation problems arise, but also that introduction of SC is of more interest of nurses than MDs. However, MDs who already offer SC perceived it as a service for their patients and were satisfied with the results. Doubts about effectiveness[21,22] and safety[29,30] of SC are no longer valid reasons for not introducing the treatment in hospitals.
Based on this survey and years of personal experience, we conclude that, preferably, SC is offered to all eligible patients and that the choice is left to the well-informed patient. This will result in improved quality of care and improved quality of life for many patients undergoing chemotherapy and facing CIA. Therefore, we should conduct studies that aim at improving the results and try to improve information provision. Educational activities should include aspects like the impact of CIA, the patient's desire for hair preservation, SC (contra-) indications, effectiveness and safety. For this purpose, the Dutch SC group developed a national standard to provide both MDs and nurses with a complete document that covers all aspects of CIA and SC.
Limitations
This survey has limitations. It is likely that selection bias occurred by the recruiting method for the three respondent groups. First, the populations from which the samples have been taken are unknown. Second, the recruited MDs will probably mainly be the ones with some interest in SC, and the nurses may be the most professionally active ones, as they participated in special interest groups. Finally, it is likely that only empowered patients who are active on the Internet have participated. Furthermore, the questionnaires were self-developed and while most response categories were defined, the answers may not have covered all aspects.
Acknowledgements
This study was supported by the Dutch Pink Ribbon Foundation (Grant No. C72). The authors would like to thank all patients, nurses and medical oncologists who participated in this survey.
Footnotes
Source of Support: Pink Ribbon Foundation, grant number C72.
Conflict of Interest: None declared.
References
- 1.McGarvey EL, Baum LD, Pinkerton RC, Rogers LM. Psychological sequelae and alopecia among women with cancer. Cancer Pract. 2001;9:283–9. doi: 10.1046/j.1523-5394.2001.96007.x. [DOI] [PubMed] [Google Scholar]
- 2.van den Hurk CJ, Mols F, Vingerhoets AJ, Breed WP. Impact of alopecia and scalp cooling on the well-being of breast cancer patients. Psychooncology. 2010;19:701–9. doi: 10.1002/pon.1615. [DOI] [PubMed] [Google Scholar]
- 3.Nozawa K, Shimizu C, Kakimoto M, Mizota Y, Yamamoto S, Takahashi Y, et al. Quantitative assessment of appearance changes and related distress in cancer patients. Psychooncology. 2013;22:2140–7. doi: 10.1002/pon.3268. [DOI] [PubMed] [Google Scholar]
- 4.Jayde V, Boughton M, Blomfield P. The experience of chemotherapy-induced alopecia for Australian women with ovarian cancer. Eur J Cancer Care (Engl) 2013;22:503–12. doi: 10.1111/ecc.12056. [DOI] [PubMed] [Google Scholar]
- 5.Kim IR, Cho J, Choi EK, Kwon IG, Sung YH, Lee JE, et al. Perception, attitudes, preparedness and experience of chemotherapy-induced alopecia among breast cancer patients: A qualitative study. Asian Pac J Cancer Prev. 2012;13:1383–8. doi: 10.7314/apjcp.2012.13.4.1383. [DOI] [PubMed] [Google Scholar]
- 6.Choi EK, Kim IR, Chang O, Kang D, Nam SJ, Lee JE, et al. Impact of chemotherapy-induced alopecia distress on body image, psychosocial well-being, and depression in breast cancer patients. Psychooncology. 2014;23:1103–10. doi: 10.1002/pon.3531. [DOI] [PubMed] [Google Scholar]
- 7.Mulders M, Vingerhoets A, Breed W. The impact of cancer and chemotherapy: Perceptual similarities and differences between cancer patients, nurses and physicians. Eur J Oncol Nurs. 2008;12:97–102. doi: 10.1016/j.ejon.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Paus R, Haslam IS, Sharov AA, Botchkarev VA. Pathobiology of chemotherapy-induced hair loss. Lancet Oncol. 2013;14:e50–9. doi: 10.1016/S1470-2045(12)70553-3. [DOI] [PubMed] [Google Scholar]
- 9.Chung S, Low SK, Zembutsu H, Takahashi A, Kubo M, Sasa M, et al. A genome-wide association study of chemotherapy-induced alopecia in breast cancer patients. Breast Cancer Res. 2013;15:R81. doi: 10.1186/bcr3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frith H, Harcourt D, Fussell A. Anticipating an altered appearance: Women undergoing chemotherapy treatment for breast cancer. Eur J Oncol Nurs. 2007;11:385–91. doi: 10.1016/j.ejon.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Batchelor D. Hair and cancer chemotherapy: Consequences and nursing care-a literature study. Eur J Cancer Care (Engl) 2001;10:147–63. doi: 10.1046/j.1365-2354.2001.00272.x. [DOI] [PubMed] [Google Scholar]
- 12.Hesketh PJ, Batchelor D, Golant M, Lyman GH, Rhodes N, Yardley D. Chemotherapy-induced alopecia: Psychosocial impact and therapeutic approaches. Support Care Cancer. 2004;12:543–9. doi: 10.1007/s00520-003-0562-5. [DOI] [PubMed] [Google Scholar]
- 13.Rosman S. Cancer and stigma: Experience of patients with chemotherapy-induced alopecia. Patient Educ Couns. 2004;52:333–9. doi: 10.1016/S0738-3991(03)00040-5. [DOI] [PubMed] [Google Scholar]
- 14.Breed WP, Hurk van den CJ, Peerbooms M. Presentation, impact and prevention of chemotherapy-induced hair loss; scalp cooling potentials and limitations. Expert Rev Dermatol. 2011;6:109–25. [Google Scholar]
- 15.Kargar M, Sarvestani RS, Khojasteh HN, Heidari MT. Efficacy of penguin cap as scalp cooling system for prevention of alopecia in patients undergoing chemotherapy. J Adv Nurs. 2011;67:2473–7. doi: 10.1111/j.1365-2648.2011.05668.x. [DOI] [PubMed] [Google Scholar]
- 16.Kato M, Sakuyama A, Imai R, Kobayashi T. Evaluation of dignicap system for the prevention of chemotherapy-induced hair loss in breast cancer patient. Breast. 2011;20(Suppl 1):S80. [Google Scholar]
- 17.Betticher DC, Delmore G, Breitenstein U, Anchisi S, Zimmerli-Schwab B, Muller A, et al. Efficacy and tolerability of two scalp cooling systems for the prevention of alopecia associated with docetaxel treatment. Support Care Cancer. 2013;21:2565–73. doi: 10.1007/s00520-013-1804-9. [DOI] [PubMed] [Google Scholar]
- 18.Wang J, Lu Z, Au JL. Protection against chemotherapy-induced alopecia. Pharm Res. 2006;23:2505–14. doi: 10.1007/s11095-006-9105-3. [DOI] [PubMed] [Google Scholar]
- 19.Shin H, Jo SJ, Kim do H, Kwon O, Myung SK. Efficacy of interventions for prevention of chemotherapy-induced alopecia: A systematic review and meta-analysis. Int J Cancer. 2015;136:E442–54. doi: 10.1002/ijc.29115. [DOI] [PubMed] [Google Scholar]
- 20.Grevelman EG, Breed WP. Prevention of chemotherapy-induced hair loss by scalp cooling. Ann Oncol. 2005;16:352–8. doi: 10.1093/annonc/mdi088. [DOI] [PubMed] [Google Scholar]
- 21.Hurk van den CJ, Peerbooms M, van de Poll-Franse LV, Nortier JW, Coebergh JW, Breed WP. Scalp cooling for hair preservation and associated characteristics in 1411 chemotherapy patients - results of the Dutch Scalp Cooling Registry. Acta Oncol. 2012;51:497–504. doi: 10.3109/0284186X.2012.658966. [DOI] [PubMed] [Google Scholar]
- 22.van den Hurk CJ, Breed WP, Nortier JW. Short post-infusion scalp cooling time in the prevention of docetaxel-induced alopecia. Support Care Cancer. 2012;20:3255–60. doi: 10.1007/s00520-012-1465-0. [DOI] [PubMed] [Google Scholar]
- 23.Hurk van den C, Komen M, Nortier J, Goey H, Breed W. Short post-infusion scalp cooling still prevents docetaxel-induced alopecia. Eur J Cancer. 2013;49(Suppl 2) abstract 1317. [Google Scholar]
- 24.van den Hurk CJ, van den Akker-van Marle ME, Breed WP, van de Poll-Franse LV, Nortier JW, Coebergh JW. Cost-effectiveness analysis of scalp cooling to reduce chemotherapy-induced alopecia. Acta Oncol. 2014;53:80–7. doi: 10.3109/0284186X.2013.794955. [DOI] [PubMed] [Google Scholar]
- 25.Hurk van den CJ. Enschede: Leiden University Medical Center; 2013. Safety and effectiveness of scalp cooling in cancer patients undergoing cytotoxic treatment, in Clinical oncology; p. 212. [Google Scholar]
- 26.Can G, Demir M, Erol O, Aydiner A. A comparison of men and women's experiences of chemotherapy-induced alopecia. Eur J Oncol Nurs. 2013;17:255–60. doi: 10.1016/j.ejon.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Davies E, Yeoh KW. Internet chemotherapy information: Impact on patients and health professionals. Br J Cancer. 2012;106:651–7. doi: 10.1038/bjc.2011.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van de Poll-Franse LV, van Eenbergen MC. Internet use by cancer survivors: Current use and future wishes. Support Care Cancer. 2008;16:1189–95. doi: 10.1007/s00520-008-0419-z. [DOI] [PubMed] [Google Scholar]
- 29.van den Hurk CJ, van de Poll-Franse LV, Breed WP, Coebergh JW, Nortier JW. Scalp cooling to prevent alopecia after chemotherapy can be considered safe in patients with breast cancer. Breast. 2013;22:1001–4. doi: 10.1016/j.breast.2013.07.039. [DOI] [PubMed] [Google Scholar]
- 30.Lemieux J, Provencher L, Perron L, Brisson J, Amireault C, Blanchette C, et al. No effect of scalp cooling on survival among women with breast cancer. Breast Cancer Res Treat, Published online: 16 December. 2014 doi: 10.1007/s10549-014-3231-0. doi 10.1007/s10549-014-3231-0. [DOI] [PubMed] [Google Scholar]


