Abstract
Medical errors are the third leading cause of death in the USA, resulting in over 440,000 deaths/year. Although over a decade has passed since the first Institute of Medicine study that documented such horrific statistics and despite significant safety improvement efforts, serious progress has yet to be achieved. It is estimated that 80% of medical errors result from miscommunication among health care providers and between providers and patients. There is preliminary research evidence that communication skills programs can improve safety outcomes, but a systematic theoretical framework for such programs has not been identified. Because of the connection between emotional intelligence (EI) ability and communication effectiveness, EI has been called by some “one of the largest drivers of patient safety.” Little literature has explored this relationship. The purpose of this article was to present a theoretical model for the relationship between EI, communication and patient safety, with conceptual and clinical illustrations used to describe such a relationship.
Keywords: Nursing, patient safety, emotional Intelligence, communication
Introduction
Over a decade has passed since the first Institute of Medicine study documented that medical errors caused over 100,000 patient deaths per year. Since that time similar studies report that medical errors are now the third leading cause of death in the United states, with as many as 440,000 patient deaths per year.[1] Root cause analysis of medical errors provide the surprising data that as much as 80% of medical errors stem from breakdown in communication between care providers, and between providers and patients.[2] One contributor to the lack of a systematic approach to this problem is the lack of a theoretical framework that addresses communication capabilities and patient risk.[3,4] Emotional intelligence ability has been anecdotally referred to as “one of the largest drivers of patient safety.” Emotional intelligence (EI) ability and communication effectiveness are clearly linked, but little literature has explored this relationship.[5] A theoretical model for the relationship between emotional intelligence, communication and patient safety is described in this article, with conceptual and clinical illustrations used to describe the relationship among these three critical factors.
Theoretical Framework: Communication
The theoretical framework for communication that will be used is Berlo's communication model [Figure 1]. This model conceptualizes both the source and recipient of communication as influenced by their communication skills, attitudes, knowledge, social station, and culture. Berlo theorizes that these elements affect the communication process. All these elements are also affected by emotions, emotional capabilities, and other, both positive and negative emotional factors. The messages exchanged between sources and recipients are made up of content, elements, treatment, structure, and code, factors also greatly influenced by emotions. Finally, messages transferred between sources and recipients through hearing, seeing, touching, smelling, and tasting, also have strong emotional perception and recognition factors. The entire communication system that Berlo describes is affected by emotional perceptions and emotional skills.[6]
Figure 1.
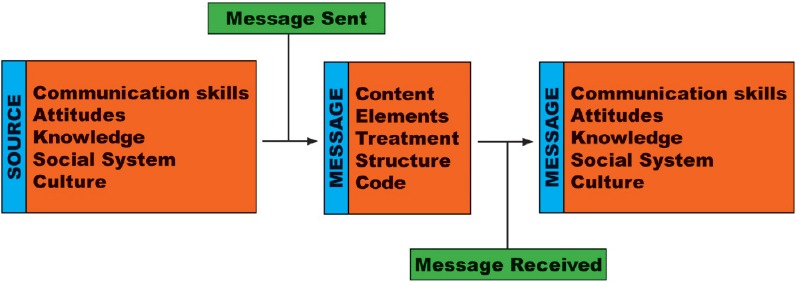
Berlo's model of communication[6]
Theoretical Framework: Breaches in Patient Safety
A commonly used model for safety performance is Reason's “Swiss cheese” model [Figure 2]. This model conceptualizes the event flow from hazard to patient harm as a vector that permeates system safety controls through holes in the system created by design flaws, active system failures, and latent conditions.[7] The more holes there are or the bigger the holes are, the greater the risk that an adverse event will occur. This model is particularly relevant to the discussion of EI and patient safety, as both latent conditions and active system failures are often related to miscommunication. Because of the influence EI skills have on communication, patient safety may be directly influenced by EI abilities. This article posits that EI ability could serve as a mediating factor to influence both latent conditions and active system failure risk.
Figure 2.

Reason's “Swiss cheese” model
Theoretical Framework: Emotional Intelligence
Emotional intelligence is a relatively new concept that has emerged in the past two decades. For this discussion, Mayer, Salovey, and Caruso's ability model of EI will be utilized. According to this model, EI is comprised of the following four abilities: 1. The ability to correctly identify emotions in self and in others, 2. The ability to use emotions in the reasoning process, 3. The ability to understand emotions, and 4. The ability to manage emotions in one's self and in emotional situations.[8]
Integration of the Three Models
This article posits that the three models just presented can be integrated in a way that suggests a novel approach to patient safety and mediating communication risk factors. This integrated model suggests that the four EI abilities serve as a mediating factor between communication and patient safety. Use of the four EI abilities may serve to both decrease the risk that latent conditions present and also reduce the incidence of active system failure. It is further posited that both these risk reduction strategies occur through improvements in communication and emotional management [Figure 3].
Figure 3.
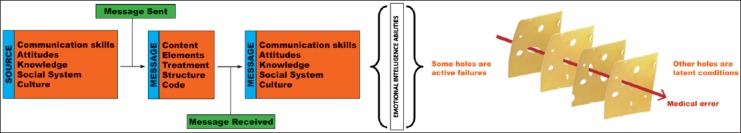
Integrated model of emotional intelligence, communication, and error conditions[6,8]
Mayer and Sparrowe suggest several means for integrating two or more theories in novel ways approach questions or important issues such as those addressed in this article. One such integration is illustrated in the model above, where two different but related phenomena (communication and conditions that lead to patient error) draw on a common set of possible explanatory factors (in this case EI abilities).[9] In this approach, effective communication, as a sum of all its constituent parts, combined with EI abilities, change the risk potential in the clinical environment. In addition, the model suggests that improved communication may also enhance EI skills, which similarly reduce risk and improve patient safety. The end result in both cases is improved communication and a decrease in both risk posed by latent conditions and active system failures.
The model can be further described using several illustrations. If there are disruptions in a communication system (right hand side of the diagram), EI abilities (correctly identifying and understanding emotions, for example), can improve the communication and prevent compromised safety (latent conditions and system failures, left-hand side of the diagram). The mediating effect of EI can be further described through illustration of the four EI abilities Mayer, Salovey and Caruso describe. Each of the abilities’ influence on communication and operational relationships will be discussed while exploring their influence on latent unsafe conditions and active system safety errors.
Emotional Intelligence Ability No. 1: Correct Identification of Emotions in Self and Others
Description of the ability
Correctly identifying emotion involves identifying feelings expressed through words, sounds, facial expression, and body language. Both expression and perception of emotions are greatly influenced by culture and social systems. This first of the EI abilities sounds simple, but is isn’t! It is a significant cause of miscommunication between care providers, and between care providers and patients, particularly in high-stress environments.
Illustration of the ability
Correct identification of emotions necessitates a differentiation between emotions that may look or sound similar. Consider a patient or co-worker who appears to be angry. There are many emotions that look and sound like anger but are not! A parent who finally locates a child they thought was lost may look and act angry but what they are actually feeling is desperate relief! A patient who cries after discussing their diagnosis with a physician could be experiencing anger, relief, fear, joy, or any other number of other emotions.
Correct identification of emotions necessitates a clarification of the patient's feelings so that the correct plan of care can be formulated. Misidentification of the patient's emotions or making assumptions about what the patient is feeling can create miscommunication, inappropriate care planning, and potentially a negative patient safety outcome. At best an inappropriate plan of care does not address actual patient problems, potentially prolongs the length of stay, and may increase compilation risk. This is a good example of a latent condition that can create patient risk. At worst, an inappropriate plan of care actually destabilizes the patient and makes their condition worse. In this case, an active system failure has occurred.
Use of this ability to influence communication and patient safety
A patient who is hostile, raging, and behaviorally inappropriate may indeed be angry. The plan of care would include helping the patient identify the reasons for their anger, the help they need to deal with these causes and a contract with the patient for more constructive behavior. However, sometimes a patient with this same behavior is actually terrified, frustrated or feeling helpless. In this case, a very different plan of care may be needed. A care plan made up of limit setting and behavior modification would be inappropriate and could result in loss of trust and foster ineffective communication. These additional “Swiss cheese holes” could increase the risk for error and adverse events for this patient.
This important EI ability influences patient safety in several other important ways. For example, emotionally aware and perceptive nurses are more apt to notice a patient's subtle emotional changes that may be the first sign of a clinical crisis. If this early warning sign is missed or ignored, the crisis could progress unnoticed into an acute crisis. A nurse's ability to identify their own emotions are important as well. How many times have you heard a nurse say “I just don’t feel good about my patient”? Experienced nurses know this “feeling without a name.” It is that anxious, nagging sense that something just isn’t right. A nurse who identifies this emotion and understands its potential importance then looks for causative factors and increases surveillance. This is an example of an active system success! The patient is safer.
Another example is patients’ emotional safety. Research evidence shows a correlation between measured nurse EI and patients’ perception that they are “cared for.” This perception creates trust in the caregiver. It may also influence strength of the therapeutic relationship, improve patient compliance with the care regimen and increase the overall effectiveness of the care plan.
Finally, there is clear research evidence that measured EI correlates with team performance. Emotionally intelligent teams can “read” each other more effectively and thus communicate better, reducing the incidence of miscommunication. Effective collaborative relationships increase the protective layers Reason's model depicts. Both these factors decrease both latent risk and opportunity for adverse events.
Emotional Intelligence Ability No. 2: Using Emotions in the Reasoning Process
Description of the ability
There are several myths about emotions and reasoning. One is that emotions are a weakness and have no place in the reasoning process. Another is that emotions contaminate reasoning and to be an objective one must be unemotional. When a nurse uses emotions in the reasoning process, thinking and feeling are integrated. Howard Gardner's theory of multiple intelligences, a foundational theory for EI, has a different premise. Gardner submits that all the forms of intelligence inform and enrich each other, resulting in integrated reasoning that enhances performance.[10] Indeed, EI as a concept grew out of the observation from cognitive researchers that individuals who integrated thinking and feeling performed better in the workplace. When emotions are used in the reasoning process, thinking, and feeling are integrated. Thinking becomes more a part of emotional processes and emotions become more a part of thinking processes. Emotional information from one's self, other people, and emotional situations is treated as data. When these data are combined with other kinds of “reasoning” data, a different kind of problem-solving is possible.
Illustration of the ability
Consider the situation of an angry staff member confronting their manager: “I can’t believe you switched my weekend this month. You bureaucrats are all alike.” A manager using emotions in the reason process holds back their own angry response. Instead, they acknowledge the fight or flight physiological reaction they are experiencing in response to the angry employee. In the moment of reflection, they remember that this employee has never before behaved this way. There is a root cause that needs to be identified so instead of an angry retort, the manager says, “This isn’t like you-what's going on?” In this situation, integrating emotions and reason in a highly charged emotional situation helped get to the real problem.
Use of this ability to influence communication and patient safety
A classic example of the importance of emotionally integrated reasoning is a patient in the ER for chest pain who reports with great anxiety that they feel like they are going to die. The cardiac rhythm is normal, vital signs are stable and labs are within acceptable parameters. A nurse who “objectively” removes emotions from reasoning may dismiss this complaint (“the patient is just anxious”). The emotionally intelligent nurse regards the “sense of impending doom” as data and incorporates it into both assessment and planning. They move the resuscitation cart a little closer and increase the frequency of rounds. Integration of thinking and feeling result in a safer environment for the patient.
When thinking and feeling are carefully integrated, there is a greater chance of balance between them. There can be better awareness of both “over/underthinking” and “over/under feeling.” Consistently “under feeling” is one of the early signs of burnout, for example. The clinical skill known as “sense of urgency” requires both sufficient emotional reactivity to respond to subtle critical indicators, but also the modulating effect of self-awareness (my patient last week died of a heart attack; I need to make sure I don’t overreact as a result).
Emotional Intelligence Ability No. 3: Understanding Emotions
Description of the ability
Emotions are like spices. They have characteristics and qualities that must be considered when “cooking” with them. This ability involves understanding the causes, effects, and characteristics of emotions. For example, fear and anger cause secretion of adrenalin! For this reason, these emotions “feel like an emergency.” As illustrated above, the physiological “fight or flight” can result in hyperreactivity, a raised voice, and other behaviors that undermine effective management of anger and fear. It is also important to understand the way that emotions evolve and change over time, and the ways in which they can be confused with other emotions. Anger can “masquerade” as several other emotions. Depression can be confused with fatigue, etc.
Illustration of the ability
A great example of this is a grief. Dr. Elizabeth Kobler-Ross identified both the stages of grief and an understanding of how the stages work. Grief is not linear. Grieving people cycle through stages of grief over and over again.[11] This understanding changes a care giver's response to a grieving person who was angry yesterday and back in denial today! Similarly, there are things to understand about fear, loss, resistance, anxiety, and other emotions that affect patients’ experiences and their compliance with care plans. When nurses understand the emotions of their patients, themselves and among care team members, the patient care environment is safer and risk is reduced.
Use of this ability to influence communication and patient safety
A good example of how understanding emotions influences patient safety is a patient's compliance with the care plan. Noncompliance is a behavior pattern that can result from emotional causes: Denial, fear, avoidance, resignation, mistrust or frustration. A nurse who understands this can look past the “problem” of noncompliance to a possible emotional root cause. This root cause and its emotional factors can then be addressed in the plan of care. If instead the patient is labeled “noncompliant,” as if it is a problem without a cause, the nurse may instead respond negatively to the “noncompliant” patient, distancing and disengaging themselves from the patient. This patient is “abandoned” in their noncompliance. If the cause of the noncompliance is an emotional factor, such abandonment may reinforce the root cause. A latent condition then exists where there is a very high risk for miscommunication between the care team and the patient. The patient may not receive the right care and an active system failure, albeit a silent one has occurred.
Understanding the way emotions work can also keep caregivers from errors of protocol. Fear, for example, is an emotion that can self-justify variation in recommended procedures. In the recent Ebola outbreak, for example, fear caused some nurses to triple glove even though recommended protocol was to double glove. Later, safety analysis concluded that the awkwardness this created during doffing actually increased caregiver risk of contamination. The procedural variation was caused by fear and instead of decreasing risk they actually increased it. This illustrates that when nurses understand how fear can influence clinical behavior, care is safer.
Managing Emotions in One's Self and in Emotional Situations
Description of the ability
Managing emotions does not mean repressing, over-controlling or denying them. Management of emotions within the context of health care safety has a goal of constructively working with the emotions present in a clinical situation to ensure that they support, not obstruct, patient safety. In emotional self-management and management of emotional situations, emotions are correctly identified and brought into the reasoning process. The plan of care uses this foundation and an understanding of the emotions involved to develop a plan of care that is effective and safe. This is hard work that benefits from peer coaching and a team approach.
Illustration of using this ability to improve communication and patient safety
Although there is no one right approach to managing emotions, the following may be helpful additions to a nurses personal “menu” of ways to effectively manage both their own emotions and difficult emotional situations.
Emotions are personal but not to be taken personally
Emotions are among the experiences most personal to us so “taking them personally” is a natural response. However, when working with patients and peers, it is important to remember that their charged emotional states are not directed at us. By taking a step back, slowing the situation down and refocusing on a root cause, the nurse can depersonalize their response, focusing on the problem solving. The resulting emotional de-escalation results in better problem-solving and a safer environment.
Assumptions about emotions are risky
Emotional reactions to clinical situations are frequently predictable (postpartum blues, grieving postamputation, etc.), but patient's emotional reactions are more varied that we think. A nurse who makes a habit of reviewing emotional data with patients and peers prevents incorrect assumptions avoids judgments and expands their understanding of root causes.
Emotions are not an emergency
Some of the emotions that have the most impact on patient safety are ones that are physiologically regulated by adrenalin. This can increase the risk for miscommunication, emotional escalation, physical hazard, and impulsive actions. In these cases, slowing down communication is important. Saying, “This is really important to me and I would like to think about it for a few minutes and get back to you,” slows down the pace of the emotional exchange and buys time to review the situation carefully.
Adopt “the pause.”
Many nurses use the “4 P's” to guide each interaction with a patient (address pain, position, personal needs, etc.). Adding a 5th P, “Pause” before starting the clinical encounter offers the nurse a moment to stop, look, think, and feel. This “check in” moment with themselves and their patient may be the most important EI habit of all.
Conclusion
Emotional intelligence is an important skill set for maintaining safety in the healthcare environment. The four EI abilities, identifying emotions in self and others, using emotions to reason, understanding emotions and managing them, not only enhance patient care but enhance patient safety. In addition, the cultivation of EI abilities may have a mediating effect on the role of communication in patient safety and the decrease of risk from environmental latent conditions and active system errors.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9:122–8. doi: 10.1097/PTS.0b013e3182948a69. [DOI] [PubMed] [Google Scholar]
- 2.Joint Commission Center for Transforming Healthcare releases targeted solutions tool for hand-off communications. Jt Comm Perspect. 2012;32:1–3. [PubMed] [Google Scholar]
- 3.Wiegand DM. Exploring the role of emotional intelligence in behavior-based safety coaching. J Safety Res. 2007;38:391–8. doi: 10.1016/j.jsr.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Sunindijo RY, Hadikusumo BH, Ogunlana S. Emotional intelligence and leadership styles in construction project management. J Manage Eng. 2014;23:166–70. [Google Scholar]
- 5.Himmer R. Emotional Intelligence in Health Care; 2014 [Google Scholar]
- 6.Berlo DK. New York: Holt, Rinehart, and Winston; 1960. The Process of Communication. [Google Scholar]
- 7.Reason J. Human error: Models and management. BMJ. 2000;320:768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer JD, Salovey P, Caruso DR. Emotional intelligence: New ability or eclectic traits? Am Psychol. 2008;63:503–17. doi: 10.1037/0003-066X.63.6.503. [DOI] [PubMed] [Google Scholar]
- 9.Mayer KJ, Sparrowe RT. Integrating theories in AMJ articles. Acad Manage Rev. 2013;56:917–22. [Google Scholar]
- 10.Gardner H. New York: Basic Books; 1993. Frames of Mind: The Theory of Multiple Intelligences. [Google Scholar]
- 11.Kübler-Ross E. NY: Simon and Schuster Ltd; 2005. On Grief and Grieving: Finding the Meaning of Grief through the Five Stages of Loss. [Google Scholar]


