Abstract
Objective:
Sleep disorder and fatigue are among a few major concerns of breast cancer survivors across the survivorship trajectory. The purpose of this pilot study was to examine feasibility and trends in multiple outcomes after a 6-week Qigong exercise program in breast cancer survivors.
Methods:
Eight female adults (mean age 55.4 ± 9.4 years, mean time after the completion of cancer treatment 3.9 ± 5.7 years) who had a diagnosis of breast cancer and were at least 3 months postcompletion of primary cancer treatment prior to participation in this study. Baseline evaluation was administered using subjective questionnaires on sleep quality, insomnia, fatigue, and quality of life. All subjects participated in two training sessions to learn the “Six Healing Sound” Qigong exercise and attended group Qigong sessions once per week in the following 6 weeks. In addition to the group sessions, subjects were asked to perform the Qigong exercises twice at home right before going to bed in the evening and immediately after getting up in the morning. Following the 6-week intervention, subjects were re-assessed using the same questionnaires. Pre- and post-intervention scores were analyzed for statistical significance.
Results:
Compliance rate was 89.6% for group sessions and 78.5% (ranging from 65.6% to 90.7%) for daily home Qigong exercises. No participant reported any adverse event or side effect during the study. All participants indicated in the end-intervention questionnaire that they would highly recommend the intervention to others. Significant improvements were observed in sleeping quality score (from 10.3 ± 3.6 to 5.4 ± 2.3, P < 0.01), insomnia index score (from 16.2 ± 3.2 to 6.8 ± 4.8, P < 0.01), fatigue score (from 60.3 ± 9.4 to 49.1 ± 8.6, P < 0.01), and SF-36 score (from 66.8 ± 7.7 to 80.9 ± 3.9, P < 0.01).
Conclusions:
Results of this single arm pilot study showed the feasibility and potential of “Six Healing Sounds” Qigong exercise for improving sleep and other symptoms in breast cancer survivors.
Keywords: Breast cancer, fatigue, sleep disorder, survivors, Qigong
Introduction
Worldwide, breast cancer is the most common cancer among women and one of the leading causes of morbidity and mortality for women;[1,2] and almost 1.7 million new cases and 521,900 breast cancer deaths were estimated in 2012.[3] Breast cancer survivors make up a large proportion of cancer survivors. Their numbers have prompted a concerted effort to address and meet the needs of this ever-growing population. Concerns related to difficulty in sleep, fatigue, distress, and sexual dysfunction are among ones that significantly impact the quality of life (QOL).[4,5,6] Sleep disorder has been reported before, during, and after cancer treatment.[4,5,6,7] Chronic sleep disorder is common among breast cancer survivors with the reported prevalence ranging from 30% to 90%.[6,7,8,9,10] Individuals with sleep disorder suffer from difficulty falling sleep, difficulty staying asleep, nonrestorative sleep, frequent nighttime awakenings, and/or excessive daytime napping. Insomnia is particularly frequent in those with breast cancer relative to other cancer types.[11] Persistent sleep disorder can increase morbidity and mortality in cancer patients/survivors.[12,13,14,15,16,17] Treatment options for problems in sleep include the use of sedatives and hypnotics, cognitive-behavioral therapy (CBT), and lifestyle interventions. Despite various treatment options, sleep disorder and fatigue are listed consistently among a few major concerns by breast cancer survivors across the survivorship trajectory[18,19,20] and are often not successfully treated.[5,11,14]
Qigong is an ancient form of mind-body self-management approach that may potentially help people with sleep difficulties. Past controlled trials of healthy adults and people with chronic conditions have shown that Qigong exercise was associated with improvement in psychological and musculoskeletal problems including pain, fatigue, sleep disorder, and mental distress.[21,22,23,24,25,26] Past studies of breast cancer patients showed improvement in white blood cell counts, platelets, and overall severity of symptoms after Qigong exercise compared to a control group.[27,28,29] Although the mechanism of Qigong exercise has not been elucidated, past research findings indicate two possible pathways involved: Qigong exercise focusing on meditation and deep breathing may increase melatonin,[30,31] and may also affect stress response pathway.[32,33] Other complementary approaches, such as Yoga or tai chi, may also benefit breast cancer survivors. A recent clinical trial in breast cancer survivors reported significant improvement in sleep quality using Yoga intervention.[34] A recent randomized clinical trial of tai chi reported improvement in breast cancer survivors in physical function, mental health, and biomarkers of inflammation, but not in sleep and fatigue.[35] Some formats of Qigong exercise are easy to learn and require less physical capacity to practice when compared to Yoga or Tai Chi, thus making it more desirable to patients who are less physically capable.
The purpose of this pilot study was to examine trends in outcomes of a Qigong exercise program in breast cancer survivors. Specifically, we are interested in changes in sleep quality and insomnia severity following the 6-week Qigong exercise program. In addition, outcome measurements included fatigue and QOL.
Methods
The current pilot study used a single arm with pre- and post-intervention comparison. The inclusion criteria included women at age of 18 years or older, at least 3 months postcompletion of primary cancer treatment for stages I, II, or III breast cancer and with no further anticancer therapy planned; and meet the criteria for insomnia as indicated by the score of Insomnia Severity Index (ISI) (>8). Participants should have no obvious cognitive impairment and no current evidence of cancer or any other diseases, such as severe depression or other psychiatric disorder, any illness affecting the immune system, etc. Participants should not be involved in other mind-body interventions during the study period. Women who used a stable dosage of hypnotic medication were not excluded from the study, provided that they met all criteria. The participants were instructed to maintain their regular exercise activities, but not to participate in any new exercise program during the study period.
Participants of the current study were 8 women (mean age 55.4 ± 9.4 years) with a diagnosis of stages I (n = 3), II (n = 4) or III (n = 1) breast cancer [Table 1]. They were on average 46.4 ± 68.5 months postcompletion of primary cancer treatment (surgery, chemotherapy, and radiation therapy) with no further anticancer therapy planned (excepting adjuvant hormone therapy). All participants had surgical intervention for breast cancer; all but one had radiation therapy; and all but two had chemotherapy. On average, the height, weight, and body mass index (BMI) of participants were (165.3 ± 5.4) cm, (75.0 ± 14.1) kg, and 27.3 ± 3.9, respectively with only one individual falling into obesity category based on her BMI. All participants were concerned about their sleep and feeling of fatigue with an average insomnia index score of 14.8 ± 2.1 at phone screen.
Table 1.
Study participants’ background information and clinical characteristics
| Subject # | Ethnicity/race | Age | Education (year) | Marital status | Employment | Cancer stage | Cancer treatment | Post-treatment | Height (cm) | Weight (kg) | BMI | IIS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | W/nonH | 70.6 | 15 | Married | Retired | 1 | s/r | 105 | 167.6 | 70.4 | 25.0 | 12 |
| 3 | W/nonH | 48.7 | 15 | Married | Unemployed | 2 | s/c | 17 | 162.6 | 77.2 | 29.2 | 17 |
| 4 | W/nonH | 67.1 | 13 | Married | Self-employed | 3 | s/r/c | 8 | 157.5 | 65.8 | 26.5 | 16 |
| 5 | W/nonH | 48.1 | 15 | Married | Full-time | 2 | s/r/c | 22 | 170.2 | 86.3 | 29.8 | 17 |
| 7 | W/nonH | 55.1 | 18 | Single | Full-time | 1 | s/r | 195 | 171.5 | 103.5 | 35.2 | 15 |
| 8 | W/nonH | 50.2 | 15 | Married | Part-time | 2 | s/r/c | 8 | 157.5 | 59.0 | 23.8 | 13 |
| 9 | W/nonH | 58.8 | 15 | Married | Part-time | 1 | s/r/c | 6.5 | 167.6 | 68.1 | 24.2 | 12 |
| 10 | B | 44.6 | 18 | Single | Full-time | 2 | s/r/c | 10 | 167.6 | 69.5 | 24.7 | 16 |
| Mean | 55.4 | 15.5 | 46.4 | 165.3 | 75.0 | 27.3 | 14.8 |
W/nonH: White or Caucasian, not Hispanic, B: Black or Africa American, s/r: Surgery and radiotherapy, s/c: Surgery and chemotherapy, s/r/c: Surgery, radiotherapy, and chemotherapy, BMI: Body mass index, IIS: Insomnia Index score
Study participants were recruited from patients who received their cancer treatment in KU Hospital. Potential candidates received the study information when they come to the clinic for clinical follow-up. If they were interested in the study, a researcher would contact them to conduct a phone screen. They were recruited sequentially in two small groups with four members in each group. Prior to their participation, all participants signed an informed consent approved by the institutional IRB. All participants went through the same 12-week intervention program that consists of a 2-week baseline (pre-intervention) period, 6-week intervention period, and 4-week end-intervention period. The 4-week end-intervention period is needed to obtain accurate information for sleep questionnaire.
A specific format of Qigong exercise, the “Six Healing Sound” Qigong exercise (see a webpage in Wikipedia for more details: http://en.wikipedia.org/wiki/Liu_Zi_Jue), was used in the study because it was considered easy to learn and practice. An experienced instructor conducted two subject training sessions. During the first training session, the subject learned to perform the Qigong exercise in standing or sitting posture. The standing position required the subject to stand with knees slightly bent and feet approximately shoulder width apart. The sitting position required the subject to maintain good upright posture. The subject should feel relaxed and comfortable with the body having a general sense of ease. The standing position was preferred; however, the subjects could choose to practice Qigong exercise in whichever posture was most comfortable for them. The subjects were then trained to control deep breathing through a diaphragmatic breathing technique and to pronounce each of the six healing sounds. A diaphragmatic breathing would minimize the role of upper chest and neck muscles and rely mainly on the contraction and relaxation of muscles in lower belly including diaphragm. When pronouncing a healing sound, the subject was instructed to exhale while quietly chanting the sound. In a complete session of “Six Healing Sound” Qigong exercise, the subject repeated six times on each of six healing sounds.
In the second training session, the subjects were taught body movements associated with each of the six healing sounds. The subjects were instructed to breathe slowly and coordinate deep breath with smooth arm movements while trying to clear their minds by concentrating on the feeling of diaphragmatic contraction during exhalation and expansion during inhalation. This is based on an assumption that self-healing begins with a quiet and empty state of mind. The body movements involved only upper extremity including arm/hand moving up/down and extending to the front and then back toward the body, except for the fifth sound during which a squat with limited knee flexion is involved (not required when performing the exercise in a sitting posture). Throughout the training sessions, the subjects were instructed to calm their mind into a mind emptiness status. They were instructed not to feel bad if thoughts or feelings intrude. Just simply say to themselves “Oh well” and return to their practice. Throughout the training sessions, the subjects learned to breathe slowly, to synchronize their breathing with the smooth arm movements and to clear their minds by concentrating on the feeling of lower belly contraction and expansion.
After the training sessions, the subjects were instructed to continue the Qigong exercise in their homes every day, at least twice per day in the morning immediately after getting up and in the evening right before going to bed. Each session of the Qigong exercise takes about 15-20 min. Participants were instructed to not eat any food within half hour before the Qigong exercise to avoid mild stomach discomfort. Each participant was given a diary to record the home Qigong exercise sessions (compliance measure) during the last day. The subject and her family member(s) were educated on the importance of adherence to Qigong exercise.
During the following 6-week intervention period, the participants met weekly with an instructor and a subgroup of 4 members for group exercise sessions. During the group exercise, the instructor evaluated and corrected the performance of each participant, answered her questions, and discussed relevant issues. The subjects turned in their Qigong exercise compliance diary that recorded their daily Qigong exercise in the previous 7 days. A discussion was triggered if the adherence rate was <70%.
During the last 4-week post-intervention period, there were no group exercise sessions within these 4 weeks. The subjects were instructed to continue their Qigong exercise at home and maintain their Qigong exercise diary. The end-study evaluation was conducted for each subject.
Subjects’ demographic data and medical history were collected immediately after they signed the informed consents. During the first meeting in the baseline period, participants were asked to fill out questionnaires regarding their insomnia severity, sleep quality, fatigue, and QOL. The same information from each subject was collected again at the end-study period. Information related to study feasibility was collected including compliance rates of participants for group and daily home sessions, adverse event or side effect, and attitude of participants toward the intervention. The compliance rate for group sessions was based on the attendance rate in a total of 8 group sessions (2 training and 6 intervention sessions). Participants were asked to start their daily two sessions of Qigong exercise after the first training session for a total of 7 weeks. The compliance rate for daily home exercise sessions was based on the rate of practiced homes sessions as recorded in daily exercise diary against a total of 98 expected sessions (two sessions daily in 7 weeks). Any adverse event or side effect, if occurred, would be documented. In an end-intervention questionnaire, all participants were asked whether they would recommend the intervention to others.
Instrument/measure
The evaluation of sleep primarily used data from subjective questionnaires because insomnia is a condition that is defined primarily by a subjective complaint of poor sleep and by a subjective dissatisfaction with sleep that are better accounted by sleep diaries and questionnaires.[36] Sleeping quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI)[37] which was developed to measure sleep quality during the previous month and to discriminate between good and poor sleepers. Sleep quality is a complex phenomenon that involves several dimensions, each of which is covered by the PSQI. The covered domains include:
Sleep duration,
Sleep disturbances,
Sleep latency,
Daytime dysfunction,
Sleep efficiency,
Sleep quality, and
Use of sleep medications.
The PSQI is composed of 19 self-rated questions and 5 questions rated by a bed partner or roommate (only the self-rated items are used in scoring the scale). The PSQI has been reported to be a stable measure of sleep quality,[38] with high test–retest reliability and construct validity.[39,40,41] The ISI[42] was also used to evaluate insomnia severity on the basis of difficulties falling asleep, night-time awakenings, early morning awakenings, impairment of daytime functioning due to sleep problems, noticeability of impairments, distress or worry caused by sleep difficulties, and dissatisfaction with sleep. Each item is rated using a five-point Likert scale ranging from 0 (not at all satisfied) to 4 (very much satisfied), for a total score ranging from 0 to 28. Its reliability and validity have been reported in general population and cancer patients.[43,44]
A commonly used instrument in assessing fatigue in cancer patients and survivors is Multidimensional Fatigue Inventory (MFI-20).[45] This 20-item questionnaire, specifically designed for cancer patients, is a self-report instrument consisting of five subscales including general fatigue, physical fatigue, reduced activity, reduced motivation, and mental fatigue. Each subscale consists of 4 items and the score for each subscale is calculated as the sum of the scores of the 4 items. It was validated for use in cancer in a subsequent study of 275 patients undergoing radiotherapy.[46] Function and QOL were measured by the MOS short-form 36 (SF-36) distributed by RAND, Santa Monica, CA, USA a multi-item scale that includes the following eight health concepts:
Physical functioning,
Role limitations due to physical health,
Role limitations due to emotional problems,
Energy/fatigue,
Emotional well-being,
Social functioning,
Bodily pain, and
General health.[47] Higher scores (possible 0-100) indicate higher QOL.
Internal consistency reliability estimates for the MOS SF-36 have been reported with an α coefficient of 0.83.[47] Normal scores for the general population are available.[48]
Statistical analysis
Multivariate analysis of variance (MANOVA) was used to determine whether a significant difference existed in mean values of four primary variables before and after the intervention program. If a significance was shown, a paired t-test with a Bonferroni adjustment for alpha level at (0.05/4 = 0.0125) was used in the post-hoc analysis to identify which variable(s) had significant difference before and after the intervention. Additional data analyses were conducted for each item of PSQI and each subcategory of SF-36. The MANOVA was used to analyze significant change in each of 7 items of PSQI. If a significance was shown between baseline and end-study evaluations, an independent t-test with an alpha level at (0.05/7 = 0.0071) was used in post-hoc analysis to identify which item had significantly changed after the intervention. Similarly, the MANOVA was used to analyze significant change in each of eight subcategories of SF-36. If a significance was shown between baseline and end-study evaluations, an independent t-test with an alpha level at (0.05/8 = 0.0063) was used in post-hoc analysis to identify which subcategory had significantly changed after the intervention.
Results
Compliance rate of the participants was 89.6% for group sessions and 78.5% (ranging from 65.6% to 90.7%) for daily home Qigong exercises. No participant reported any adverse event or side effect during the study. All participants indicated in the end-intervention questionnaire that they would highly recommend the intervention to others.
Significant improvements were observed in PSQI total score (from 10.3 ± 3.6 to 5.4 ± 2.3, P < 0.01) and Insomnia Index score (from 16.2 ± 3.2 to 6.8 ± 4.8, P < 0.01) [Figure 1]. Itemized details of PSQI scores [Table 2], however, revealed variance in changes of 7 items in PSQI. Two items, sleep quality and daytime dysfunction, improved significantly (P < 0.007) after intervention. Three items showed the pre-post changes approaching significance, including sleep disturbances (P = 0.040), sleep latency (P = 0.024), and sleep efficiency (P = 0.024). Two items that seemed no significant changes before and after the intervention were sleep duration (P = 0.099) and use of sleep medicine (P = 0.175).
Figure 1.
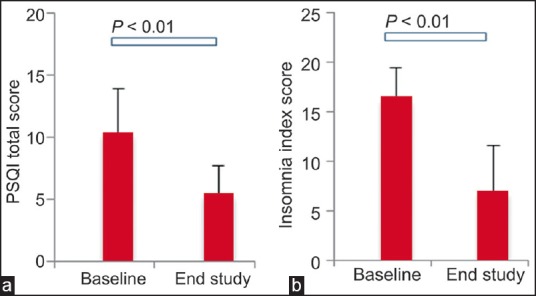
Group means (standard deviation) between baseline and end-study measurements were significantly different in (a) Pittsburgh Sleep Quality Index total score (P < 0.01); and (b) insomnia index score (P < 0.01)
Table 2.
Mean score (SD) of the group for each specific item in PSQI pre (baseline) and post the intervention. For each item, the score ranged from 0 to 3, representing no problem to severe problem
| PSQI item | Pre | Post | Percentage of change | P |
|---|---|---|---|---|
| Sleep duration | 1.50 (0.39) | 1.13 (0.83) | 25.0 | 0.099 |
| Sleep disturbances | 1.75 (0.46) | 1.38 (0.52) | 21.4 | 0.040 |
| Sleep latency | 1.00 (0.93) | 0.25 (0.46) | 75.0 | 0.024 |
| Daytime dysfunction | 1.75 (0.89) | 0.63 (0.74) | 64.3 | 0.007 |
| Sleep efficiency | 1.38 (1.30) | 0.63 (0.92) | 54.5 | 0.024 |
| Sleep quality | 2.00 (0.76) | 0.63 (0.92) | 68.8 | 0.000 |
| Use of sleep medicine | 1.00 (1.41) | 0.75 (1.16) | 25.0 | 0.175 |
SD: Standard deviation, PSQI: Pittsburgh Sleep Quality Index
Changes in MFI-20 score (from 60.3 ± 9.4 to 49.1 ± 8.6, P < 0.01) and SF-36 score (from 66.8 ± 7.7 to 80.9 ± 3.9, P < 0.01) were also significant after the intervention [Figure 2]. An examination of all sub-categories of SF-36 revealed again different patterns of change after the intervention [Table 3]. Significant changes were found in subcategories of role limitations due to physical health (P < 0.006). Changes approaching significance were found in physical function (P = 0.014), role limitations due to emotional problems (P = 0.009), energy/fatigue (P = 0.014), social functioning (P = 0.070), and general health (P = 0.009). There was no significant changes in emotional well-being (P = 0.279); and bodily pain (P = 0.237).
Figure 2.
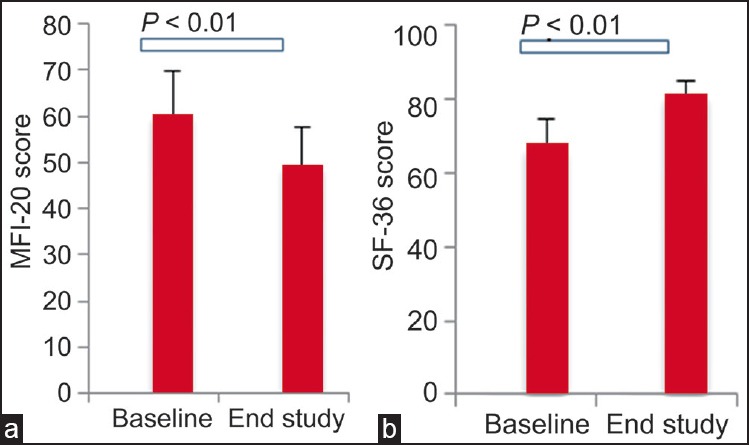
Group means (standard deviation) between baseline and end-study measurements were significantly different in (a) Multidimensional Fatigue Inventory-20 score (P < 0.01); and (b) short-form 36 score (P < 0.01)
Table 3.
Mean score (SD) of the group for each specific subcategory in SF-36 pre (baseline) and post the intervention. For each item, the score ranged from 0 to 100, representing the worst to best
| SF-36 subcategory | Pre | Post | Percentage of change | P |
|---|---|---|---|---|
| Physical functioning | 77.5 (11.6) | 84.4 (8.6) | 8.9 | 0.014 |
| Role limitations due to physical health | 59.4 (26.5) | 100.0 (0.0) | 68.4 | 0.002 |
| Role limitations due to emotional problems | 58.3 (38.8) | 91.7 (15.4) | 57.1 | 0.009 |
| Energy/fatigue | 44.4 (12.7) | 63.1 (11.3) | 42.3 | 0.014 |
| Emotional wellbeing | 71.0 (14.0) | 75.0 (12.6) | 5.6 | 0.279 |
| Social functioning | 70.3 (17.6) | 85.9 (23.6) | 22.2 | 0.070 |
| Bodily pain | 73.1 (19.8) | 77.5 (18.2) | 6.0 | 0.237 |
| General health | 63.1 (18.3) | 72.5 (16.3) | 14.9 | 0.009 |
SD: Standard deviation, SF-36: Short-form 36
Discussion
In this pilot study, we demonstrated the feasibility of a specific format of Qigong exercise, i.e., six healing sound Qigong, in breast cancer survivors. The compliance rates for either group exercise sessions or daily home exercise sessions were acceptable. On average, every participant practiced the Qigong exercise at home more than one session per day, as indicated by the lowest compliance rate of 65.6%. There was no adverse event or side effect reported by any participant. All participants would highly recommend the intervention to others.
Compared to the baseline evaluation, we observed significant improvements after the Qigong exercise in sleep, fatigue, and QOL in a group of breast cancer survivors who complained initially of sleep disorder. This result is in agreement with a recent study[49] that reported significant improvement in sleep in a comparison to baseline assessment in both the Qigong exercise group and a sham Qigong exercise group. However, they found no difference between two groups in terms of sleep measurement. A few other studies of Qigong exercise reported beneficial results focusing on fatigue in breast cancer patients/survivors but did not include a measure of sleep quality.[50,51] Sleep disorder is an important concern in many breast cancer survivors, and current treatments had only limited success.[5,11,14,18,19,20] There is an urgent need to develop more effective interventions, especially self-management approaches to help those who suffer from sleep disorder after breast cancer treatment. More randomized controlled trials are needed to further examine the effect of Qigong exercise for sleep disorder in breast cancer survivors.
CBT has been recommended most commonly by health professionals for sleep disorder in cancer survivors. A comparison of outcomes of past CBT trials with the results of the current study revealed interesting areas for future research. First, the Qigong exercise in the current study showed a level of improvement in sleep measurements comparable to findings reported in CBT studies. For instance, compared to a recent study of CBT in breast cancer survivors, changes recorded from sleep diary were 18% in sleep efficacy, 55% in sleep latency, 4% in sleep duration.[52] In contrast, our results showed changes in those three measurements by 54.5%, 75.0%, and 21.4%, respectively. Second, it appeared that the Qigong exercise in the current study produced more prominent changes in sleep quality and day-time dysfunction than other aspects of sleep including sleep latency and sleep efficiency. In contrary, studies of CBT intervention showed the major benefits in sleep latency and sleep efficiency. Past studies of CBT trials reported either no results on sleep quality,[52,53] or small changes (e.g., 8%) in the measure of sleep quality.[54] Future trails will be desired to compare two types of interventions through a randomized design and confirm whether such observation can be further confirmed.
In the current study, we have also observed improvements of participants in fatigue and QOL. A further examination of subcategories of PSQI and SF-36 measurements indicated potential improvements in daytime dysfunction, physical function, role limitation due to physical health, role limitations due to emotional problems, energy/fatigue, social functioning, and general health. We speculate that the significant improvement in sleep measurements might partially contribute to reduced fatigue and improvement in physical function that in turn led to reduced role limitation due to emotional problems. It has been repeatedly reported in literature that fatigue is strongly correlated with insomnia in breast cancer survivors.[5,7,9,55,56,57] A recent study indicated that insomnia predicted higher levels of fatigue and treatment focusing on sleeping problems might be beneficial for fatigue symptom in those women.[58] Future research may reveal more insight of the importance of a good sleep on multiple symptoms in breast cancer survivors.
Limitations of the current pilot study include lack of a randomized control group, small sample size without blinding of study personal or subjects. Nevertheless, the current study demonstrated the feasibility of a specific Qigong exercise in breast cancer survivors. Furthermore, results of outcome measurements indicated potential beneficial effects of the Qigong exercise in sleep disorder, fatigue, and QOL. The specific format of Qigong exercise used in the current study was easy to learn and practice. Future research is required to determine whether the significant improvement in sleep quality and other outcome measures can be achieved through a rigorous randomized controlled trial.
Financial support and sponsorship
This project is internally support by University of Kansas Medical Center.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Toriola AT, Colditz GA. Trends in breast cancer incidence and mortality in the United States: Implications for prevention. Breast Cancer Res Treat. 2013;138:665–73. doi: 10.1007/s10549-013-2500-7. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. Lyon, France: International Agency for Research on Cancer; 2013. [last accessed in October 20 th, 2015]. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Available from: http://www.globocan.iarc.fr/Default.aspx . [Google Scholar]
- 3.DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2015;24:1495–506. doi: 10.1158/1055-9965.EPI-15-0535. [DOI] [PubMed] [Google Scholar]
- 4.Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL. Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum. 2004;31:591–5598. doi: 10.1188/04.onf.591-598. [DOI] [PubMed] [Google Scholar]
- 5.Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH. Sleep and quality of life in breast cancer patients. J Pain Symptom Manage. 2002;24:471–80. doi: 10.1016/s0885-3924(02)00500-6. [DOI] [PubMed] [Google Scholar]
- 6.Savard J, Simard S, Blanchet J, Ivers H, Morin CM. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583–90. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 7.Ancoli-Israel S, Liu L, Marler MR, Parker BA, Jones V, Sadler GR, et al. Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer. 2006;14:201–9. doi: 10.1007/s00520-005-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berger AM, Farr LA, Kuhn BR, Fischer P, Agrawal S. Values of sleep/wake, activity/rest, circadian rhythms, and fatigue prior to adjuvant breast cancer chemotherapy. J Pain Symptom Manage. 2007;33:398–409. doi: 10.1016/j.jpainsymman.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, et al. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol. 2010;28:292–8. doi: 10.1200/JCO.2009.22.5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schultz PN, Klein MJ, Beck ML, Stava C, Sellin RV. Breast cancer: Relationship between menopausal symptoms, physiologic health effects of cancer treatment and physical constraints on quality of life in long-term survivors. J Clin Nurs. 2005;14:204–11. doi: 10.1111/j.1365-2702.2004.01030.x. [DOI] [PubMed] [Google Scholar]
- 11.Davidson JR, MacLean AW, Brundage MD, Schulze K. Sleep disturbance in cancer patients. Soc Sci Med. 2002;54:1309–21. doi: 10.1016/s0277-9536(01)00043-0. [DOI] [PubMed] [Google Scholar]
- 12.Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–7. doi: 10.1093/sleep/32.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ancoli-Israel S. Recognition and treatment of sleep disturbances in cancer. J Clin Oncol. 2009;27:5864–6. doi: 10.1200/JCO.2009.24.5993. [DOI] [PubMed] [Google Scholar]
- 14.Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural course of insomnia comorbid with cancer: An 18-month longitudinal study. J Clin Oncol. 2011;29:3580–6. doi: 10.1200/JCO.2010.33.2247. [DOI] [PubMed] [Google Scholar]
- 15.Lehrer S, Green S, Ramanathan L, Rosenzweig KE. Obesity and deranged sleep are independently associated with increased cancer mortality in 50 US states and the District of Columbia. Sleep Breath. 2013;17:1117–8. doi: 10.1007/s11325-013-0811-x. [DOI] [PubMed] [Google Scholar]
- 16.Miller YE, Karoor V, Dempsey EC, Fagan KA. Sleep-disordered breathing, hypoxemia, and cancer mortality. Am J Respir Crit Care Med. 2013;187:330–1. doi: 10.1164/ajrccm.187.3.330. [DOI] [PubMed] [Google Scholar]
- 17.Østhus AA, Aarstad AK, Olofsson J, Aarstad HJ. Prediction of survival by pretreatment health-related quality-of-life scores in a prospective cohort of patients with head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2013;139:14–20. doi: 10.1001/jamaoto.2013.1056. [DOI] [PubMed] [Google Scholar]
- 18.Baker F, Denniston M, Smith T, West MM. Adult cancer survivors: How are they faring? Cancer. 2005;104(11 Suppl):2565–76. doi: 10.1002/cncr.21488. [DOI] [PubMed] [Google Scholar]
- 19.Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M. It's not over when it's over: Long-term symptoms in cancer survivors – a systematic review. Int J Psychiatry Med. 2010;40:163–81. doi: 10.2190/PM.40.2.c. [DOI] [PubMed] [Google Scholar]
- 20.Ness S, Kokal J, Fee-Schroeder K, Novotny P, Satele D, Barton D. Concerns across the survivorship trajectory: Results from a survey of cancer survivors. Oncol Nurs Forum. 2013;40:35–42. doi: 10.1188/13.ONF.35-42. [DOI] [PubMed] [Google Scholar]
- 21.Cheung BM, Lo JL, Fong DY, Chan MY, Wong SH, Wong VC, et al. Randomised controlled trial of Qigong in the treatment of mild essential hypertension. J Hum Hypertens. 2005;19:697–704. doi: 10.1038/sj.jhh.1001884. [DOI] [PubMed] [Google Scholar]
- 22.Tsang HW, Fung KM, Chan AS, Lee G, Chan F. Effect of a Qigong exercise programme on elderly with depression. Int J Geriatr Psychiatry. 2006;21:890–7. doi: 10.1002/gps.1582. [DOI] [PubMed] [Google Scholar]
- 23.Tsang HW, Mok CK, Au Yeung YT, Chan SY. The effect of Qigong on general and psychosocial health of elderly with chronic physical illnesses: A randomized clinical trial. Int J Geriatr Psychiatry. 2003;18:441–9. doi: 10.1002/gps.861. [DOI] [PubMed] [Google Scholar]
- 24.Hui PN, Wan M, Chan WK, Yung PM. An evaluation of two behavioral rehabilitation programs, Qigong versus progressive relaxation, in improving the quality of life in cardiac patients. J Altern Complement Med. 2006;12:373–8. doi: 10.1089/acm.2006.12.373. [DOI] [PubMed] [Google Scholar]
- 25.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–74. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 26.Griffith JM, Hasley JP, Liu H, Severn DG, Conner LH, Adler LE. Qigong stress reduction in hospital staff. J Altern Complement Med. 2008;14:939–45. doi: 10.1089/acm.2007.0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee TI, Chen HH, Yeh ML. Effects of chan-chuang Qigong on improving symptom and psychological distress in chemotherapy patients. Am J Chin Med. 2006;34:37–46. doi: 10.1142/S0192415X06003618. [DOI] [PubMed] [Google Scholar]
- 28.Yeh ML, Lee TI, Chen HH, Chao TY. The influences of chan-chuang qi-gong therapy on complete blood cell counts in breast cancer patients treated with chemotherapy. Cancer Nurs. 2006;29:149–55. doi: 10.1097/00002820-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Chen Z, Meng Z, Milbury K, Bei W, Zhang Y, Thornton B, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: Results of a randomized controlled trial. Cancer. 2013;119:1690–8. doi: 10.1002/cncr.27904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martarelli D, Cocchioni M, Scuri S, Pompei P. Diaphragmatic breathing reduces exercise-induced oxidative stress. Evid Based Complement Alternat Med 2011. 2011:932430. doi: 10.1093/ecam/nep169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim DH, Moon YS, Kim HS, Jung JS, Park HM, Suh HW, et al. Effect of zen meditation on serum nitric oxide activity and lipid peroxidation. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:327–31. doi: 10.1016/j.pnpbp.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 32.Lee MS, Lee MS, Kim HJ, Moon SR. Qigong reduced blood pressure and catecholamine levels of patients with essential hypertension. Int J Neurosci. 2003;113:1691–701. doi: 10.1080/00207450390245306. [DOI] [PubMed] [Google Scholar]
- 33.Jones BM. Changes in cytokine production in healthy subjects practicing Guolin Qigong: A pilot study. BMC Complement Altern Med. 2001;1:8. doi: 10.1186/1472-6882-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mustian KM, Sprod LK, Janelsins M, Peppone LJ, Palesh OG, Chandwani K, et al. Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors. J Clin Oncol. 2013;31:3233–41. doi: 10.1200/JCO.2012.43.7707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sprod LK, Janelsins MC, Palesh OG, Carroll JK, Heckler CE, Peppone LJ, et al. Health-related quality of life and biomarkers in breast cancer survivors participating in tai chi chuan. J Cancer Surviv. 2012;6:146–54. doi: 10.1007/s11764-011-0205-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krystal AD. The changing perspective on chronic insomnia management. J Clin Psychiatry. 2004;65(Suppl 8):20–5. [PubMed] [Google Scholar]
- 37.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 38.Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166:1768–74. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 39.Gentili A, Weiner DK, Kuchibhatla M, Edinger JD. Test-retest reliability of the Pittsburgh Sleep Quality Index in nursing home residents. J Am Geriatr Soc. 1995;43:1317–8. doi: 10.1111/j.1532-5415.1995.tb07415.x. [DOI] [PubMed] [Google Scholar]
- 40.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 41.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 42.Morin CM. New York: The Guilford Press; 1993. Insomnia: Psychological Assessment and Management. [Google Scholar]
- 43.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 44.Smith S, Trinder J. Detecting insomnia: Comparison of four self-report measures of sleep in a young adult population. J Sleep Res. 2001;10:229–35. doi: 10.1046/j.1365-2869.2001.00262.x. [DOI] [PubMed] [Google Scholar]
- 45.Smets EM, Garssen B, Bonke B, De Haes JC. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39:315–25. doi: 10.1016/0022-3999(94)00125-o. [DOI] [PubMed] [Google Scholar]
- 46.Smets EM, Garssen B, Cull A, de Haes JC. Application of the multidimensional fatigue inventory (MFI-20) in cancer patients receiving radiotherapy. Br J Cancer. 1996;73:241–5. doi: 10.1038/bjc.1996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 48.van der Zee K, Sanderman R. The Netherlands: University of Groningen; 1993. RAND-36.Groningen: Northern Centre for Health Care Research. [Google Scholar]
- 49.Larkey LK, Roe DJ, Weihs KL, Jahnke R, Lopez AM, Rogers CE, et al. Randomized controlled trial of Qigong/tai chi easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med. 2015;49:165–76. doi: 10.1007/s12160-014-9645-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oh B, Butow P, Mullan B, Clarke S, Beale P, Pavlakis N, et al. Impact of medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: A randomized controlled trial. Ann Oncol. 2010;21:608–14. doi: 10.1093/annonc/mdp479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Campo RA, Agarwal N, LaStayo PC, O’Connor K, Pappas L, Boucher KM, et al. Levels of fatigue and distress in senior prostate cancer survivors enrolled in a 12-week randomized controlled trial of Qigong. J Cancer Surviv. 2014;8:60–9. doi: 10.1007/s11764-013-0315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. J Clin Oncol. 2005;23:6083–96. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- 53.Espie CA, Fleming L, Cassidy J, Samuel L, Taylor LM, White CA, et al. Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin Oncol. 2008;26:4651–8. doi: 10.1200/JCO.2007.13.9006. [DOI] [PubMed] [Google Scholar]
- 54.Epstein DR, Dirksen SR. Randomized trial of a cognitive-behavioral intervention for insomnia in breast cancer survivors. Oncol Nurs Forum. 2007;34:E51–9. doi: 10.1188/07.ONF.E51-E59. [DOI] [PubMed] [Google Scholar]
- 55.Roscoe JA, Kaufman ME, Matteson-Rusby SE, Palesh OG, Ryan JL, Kohli S, et al. Cancer-related fatigue and sleep disorders. Oncologist. 2007;12(Suppl 1):35–42. doi: 10.1634/theoncologist.12-S1-35. [DOI] [PubMed] [Google Scholar]
- 56.Anderson KO, Getto CJ, Mendoza TR, Palmer SN, Wang XS, Reyes-Gibby CC, et al. Fatigue and sleep disturbance in patients with cancer, patients with clinical depression, and community-dwelling adults. J Pain Symptom Manage. 2003;25:307–18. doi: 10.1016/s0885-3924(02)00682-6. [DOI] [PubMed] [Google Scholar]
- 57.Kim SH, Son BH, Hwang SY, Han W, Yang JH, Lee S, et al. Fatigue and depression in disease-free breast cancer survivors: Prevalence, correlates, and association with quality of life. J Pain Symptom Manage. 2008;35:644–55. doi: 10.1016/j.jpainsymman.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 58.Schultz SL, Dalton SO, Christensen J, Carlsen K, Ross L, Johansen C. Factors correlated with fatigue in breast cancer survivors undergoing a rehabilitation course, Denmark, 2002-2005. Psychooncology. 2011;20:352–60. doi: 10.1002/pon.1739. [DOI] [PubMed] [Google Scholar]


