Abstract
Thailand has a universal multi-payer system with two main types of health insurance: National Health Security Office or public health insurance and private insurance. National health insurance is designed for people who are not eligible to be members of any employment-based health insurance program. Although private health insurance is also available, all Thai citizens are required to be enrolled in either national health insurance or employees’ health insurance. There are many differences between the public health insurance and private insurance. Public health insurance, therefore, initiates programs that offer many sets of benefit packages for high-cost care. For cancer care, cover screening, curative treatment such as surgery, chemotherapy, radiation together with supportive and palliative care.
Keywords: Cancer care, health insurance, Thailand

Introduction
Thailand is a country in Southeast Asia that encompasses 514,000 km2 with a population of 67 million and borders with Myanmar, Laos, Cambodia, and Malaysia. The official national language, spoken and written by almost 100% of the population, is Thai. Buddhism is the professed faith of 94.6% of the population. Islam is embraced by 4.6% of the Thai people while the rest of the population practices Christianity, Hinduism, and other religions. The economy has performed well in recent years with an average annual Gross National Income (GNI) growth rate of 5.2% between 2000 and 2008. Upgraded to an upper-middle-in come country by the World Bank in 2011, Thailand's GNI/capita, US$ 4210 in 2010, is lower than the average of US$ 5884 for this income group. The economy is export-led, with exports accounting for more than two-third of gross domestic product. The unemployment rate is low: 1.4% of the total labor force in 2008. Of the 35 million employed, 51% are in work categories associated with the informal economy, namely self-employed workers (31%) and unpaid family labor (20%).
Economic growth and social policies that include a national social protection floor have resulted in significant poverty reduction, from 49.7% of the population in 1988 to 8.1% in 2009. However, income inequality as measured by the Gini index (the degree of inequality in the distribution of household income in a country) has not reduced from its level of 42.5 reached in 2004.
Thailand's human development index was 0.682 in 2010, ranking it 103rd out of 187 countries with comparable data. This index represents a broader definition of well-being and provides a composite measure of three basic dimensions of human development: Health, education, and income. In 2010, the adult literacy rate was 94% (the youth literacy rate was 98.1% in 2005) and life expectancy at birth was 74.1 years.[1]
Thailand achieved the health millennium development goals in the early 2000s, well in advance of the 2015 targets. The total fertility rate dropped from 2.0 in 1992 to 1.6 in 2009, below replacement level, as a result of a high contraceptive prevalence rate (81%). In 2009, antenatal care and skilled birth attendant coverage were 99-100%, the maternal mortality ratio was 48/100,000 live births, and the under-five mortality rate was 14/1,000 live births. Life expectancy at birth women/men 78/71 years top 10 causes of death in Thailand (1) cancer 19%, (2) ischemic heart disease 12%, (3) stroke 10%, (4) lower respiratory infections 9%, (5) chronic obstructive pulmonary disease, (6) diabetes 4%, (7) road injuries 4%, and (8) cirrhosis 2% (http://viz., healthmetricsandevaluation.org/gbd-compare).[2]
Cancer Care in Thailand
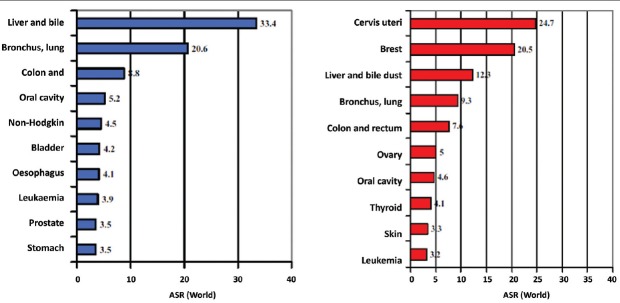
In 2002, 4.2 million new cancer cases-39% of new cases worldwide — Were diagnosed among 3.2 billion persons (48% of the world population) living in the 15 most highly developed in South, East, and Southeast Asia: Japan, Taiwan, Singapore, South Korea, Malaysia, Thailand, China, Philippines, Sri Lanka, Vietnam, Indonesia, Mongolia, India, Laos, and Cambodia [Figure 1].[3]
Figure 1.
Incidence rate for total cancers by gender and country
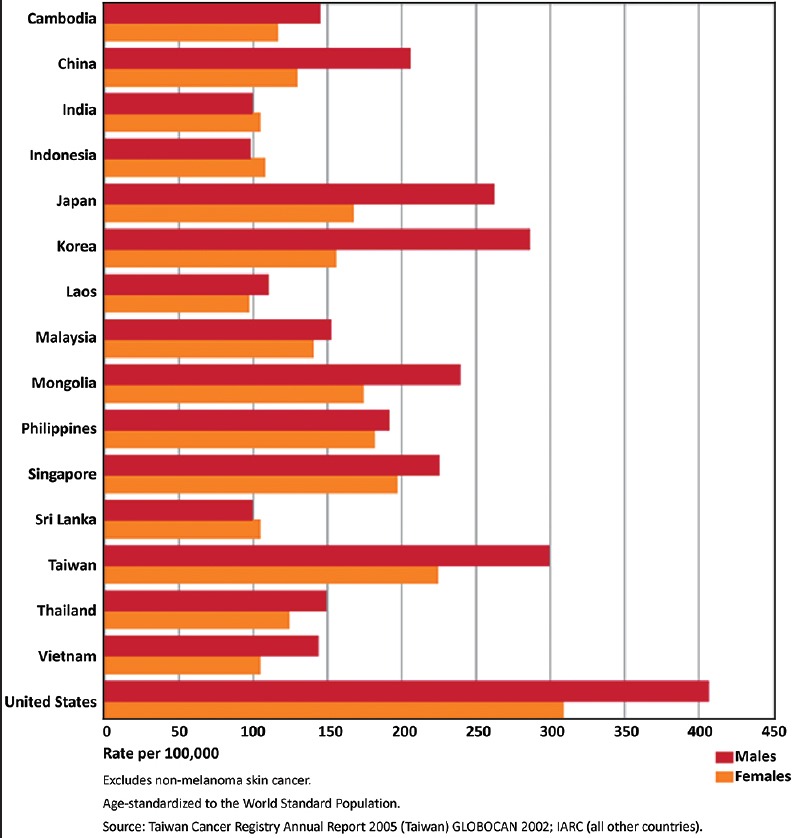
Cancer in Thailand is becoming a significant health problem. The estimated numbers of new cancer cases in Thailand in the year 1999 was 31,582 in men and 33,678 in women. These correspond to age-standardized rates (ASR) of 127.7/100 000 for men and 125.5/100 000 in women. The national estimates of the 10 leading cancers in men and women are shown as age-standardized rates and as a number of cases [Figure 2].
Figure 2.
Leading Cancers in Thailand, 1998-2000
Liver and bile duct cancer are the most common cancer in men (ASR = 33.4), followed by lung cancer (ASR = 20.6), colon and rectum cancer (ASR = 8.8), and oral cancer (ASR = 5.2). In women, cervix cancer is the most common (ASR = 24.7), followed by breast cancer (ASR = 20.5), liver and bile duct cancer (ASR = 12.3), and lung cancer (ASR = 9.3).
The very high incidence of liver cancer in the North Eastern region means that liver and bile duct cancer is the major cancer of men in the whole country, with an estimated 8 298 new cases in 1999. Lung cancer is second in importance (4947 new cases); taken together, these two sites are responsible for 41.9% of all cancer in men.
In women, cervix cancer is the most important (6954 new cases), followed by breast cancer (5854 new cases), liver and bile duct cancer (3094 new cases), and lung cancer (2344 new cases), these four sites being responsible for 54.2% of all cancers in women.[4]
When Thai people get cancer, a significant consideration is medical treatment expenses, which depend on the type of cancer, a hospital used and treatment approaches such as an operation, a radiation treatment, a hormone medical treatment and chemotherapy, including the duration of treatment. Though some kinds of cancer can be completely cured, a cancer patient has to take into account expenses for continuous taking care of his/her health, including a reserve fund in case he/she has to stop working for a long period, which inevitably affects his/her, incomes. It is estimated that a large sum of money has to be spent for a cancer treatment.
Health Insurance for Cancer in Thailand
Thailand introduced universal coverage reforms in 2001, becoming one of only a handful of lower-middle income countries to do so. Means-tested health care for low-income households was replaced by a new and more comprehensive insurance scheme, originally known as the 30 baht project, in line with the small co-payment charged for treatment. People joining the scheme receive a gold card which allows them to access services in their health district, and if necessary, be referred for specialist treatment elsewhere. A universal multi-payer system with two main types of health insurance: National Health Security Office (NHSO) or public health insurance and private insurance.[5]
National health insurance is designed for people who are not eligible to be members of any employment-based health insurance program. Although private health insurance is also available, all Thai citizens are required to be enrolled in either national health insurance or employees’ health insurance. There are many differences between the public health insurance and private insurance. National health insurance is designed for people who are not eligible to be members of any employment-based health insurance program. Although private health insurance is also available, all Thai citizens are required to be enrolled in either national health insurance or employees’ health insurance which cover cancer care such as screening, curative treatment such as surgery, chemotherapy, radiation together with supportive and palliative care.
Conclusion
Provision of medical services under the universal coverage has been changed from fragmented service to the new integrated “Continuum of Care” design. The NHSO introduce an active manage approach to both providers and beneficiaries. Therefore, the NHSO together with the Social Security Scheme (SSS) and the Comptroller General's Department (CGD), Ministry of Finance, Thailand have already implemented the new periodic health examination as a risk stratification tools. The goal of this screening and evaluation program is to prevent the onset of disease or the warning of an existing disease. A further goal of the periodic health examination is to educate patients about behavioral patterns or environmental exposures that pose risks for future diseases. Then risked group will be informed and encourage them to join the risk modification program and appropriate treatment under standard care map where national health insurance is designed to cover screening, curative treatment such as surgery, chemotherapy, radiation together with supportive, and palliative in cancer care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was written on the basis of a presentation given at the AONS 2015 Conference held in Seoul Korea by the Asian Oncology Nursing Society.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global Cancer Statistics, 2002. CA Cancer J Clin. 2005:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Sakunphanit T, Eungpoonsawat W, Sornchumni C, Ruangdej S, Rassiri J, Bhakeecheep S, et al. National Health Security Office Annual Report. 2008 [Google Scholar]
- 3.McManus T. Nonthaburi, Thailand: Health Insurance System Research Office; 2012. Thailand's Universal Coverage Scheme: Achievements and Challenges. An Independent Assessment of the First 10 Years (2001-2010) [Google Scholar]
- 4.Sakunphanit T. Thailand: Universal Health Care Coverage Through Pluralistic Approaches. International Labour Organization. 2015 [Google Scholar]
- 5.Khuhaprema T. Current cancer situation in Thailand. Thai J Toxicol. 2008;23:60–1. [Google Scholar]