Abstract
Objective:
The aim of the study was to introduce and evaluate the compliance to documentation of situation, background, assessment, recommendation (SBAR) form.
Methods:
Twenty nurses involved in active bedside care were selected by simple random sampling. Use of SBAR was illustrated thru self-instructional module (SIM). Content validity and reliability were established. The situation, background, assessment, recommendation (SBAR) form was disseminated for use in a clinical setting during shift handover. A retrospective audit was undertaken at 1st week (A1) and 16th week (A2), post introduction of SIM. Nurse's opinion about the SBAR form was also captured.
Results:
Majority of nurses were females (65%) in the age group 21-30 years (80%). There was a significant association (P = 0.019) between overall audit scores and graduate nurses. Significant improvement (P = 0.043) seen in overall scores between A1 (mean: 23.20) and A2 (mean: 24.26) and also in “Situation” domain (P = 0.045) as compared to other domains. There was only a marginal improvement in documentation related to patient's allergies and relevant past history (7%) while identifying comorbidities decreased by 40%. Only 70% of nurses had documented plan of care. Most (76%) of nurses expressed that SBAR form was useful, but 24% nurses felt SBAR documentation was time-consuming. The assessment was easy (53%) to document while recommendation was the difficult (53%) part.
Conclusions:
SBAR technique has helped nurses to have a focused and easy communication during transition of care during handover. Importance and relevance of capturing information need to be reinforced. An audit to look for reduced number of incidents related to communication failures is essential for long-term evaluation of patient outcomes. Use of standardized SBAR in nursing practice for bedside shift handover will improve communication between nurses and thus ensure patient safety.
Keywords: Nurses, situation, background, assessment, recommendation, shift handover

Introduction
All patients have a right to effective care at all times. Patients admitted to health care setting are treated by a number of health care personnels. Communication between health care personnel accounts for a major part of the information flow in health care, and growing evidence indicates that errors in communication give rise to substantial clinical morbidity and mortality.[1] One of the risk factors leading to communication breakdowns during transition of care is a lack of standardized procedures in conducting successful handoffs, for example, use of the situation, background, assessment, recommendation (SBAR).[2] Studies indicate that use of structured handoffs will improve the quality of patient handover.[3,4,5] Hands off is the transfer of responsibility and accountability of a patient, from one nurse to another[6] either during shift handover or transfers of the patient from one department to the other.
SBAR was introduced by rapid response teams at Kaiser Permanente in Colorado in 2002, to investigate patient safety. It is an acronym for SBAR; a technique that can be used to facilitate prompt and appropriate communication. This communication model has gained popularity in healthcare settings, especially among professionals such as nursing staff. It is a way for health care professionals to communicate effectively with one another, and also allows for important information to be transferred accurately. The format of SBAR allows for the short, organized and predictable flow of information between professionals.[7] The main purpose of SBAR technique is to improve the effectiveness of communication through standardization of communication process.
Nurses often take more of a narrative and descriptive approach to explain a situation, while physicians usually want to hear only main aspects of a situation. The SBAR technique closes the gap between these two approaches allowing communicators to understand each other better. It includes a summary of the patient's current medical status, recent changes in condition, potential changes to watch for, resuscitation status, recent laboratory values, allergies, problem list, and a to-do list for the incoming nurse. It is specially used for communication between a physician and a nurse when there is a change in patient condition or between a nurse and nurse during patients shift to a new department or during shift change. It is a technique used to deliver quality patient care. It is a skill that can be learned.[8]
Published evidence shows that SBAR provides effective and efficient communication, thereby promoting better patient outcomes.[9] SBAR communication method is an evidence-based strategy for improving not only interprofessional communication, but all communication[10] especially when combined with good assessment skills, clinical judgment, and critical-thinking skills. Nursing documentation must describe patient's ongoing status from shift to shift with records of all nursing interventions.[9] In India, no such data was available. Therefore, the aim of this study was to introduce and evaluate the compliance to effective use of SBAR form during nurses’ handover in a tertiary care cancer center.
Methods
Data for this study were drawn from a larger research study. Ethical approval for the study was granted by the institutional review board. Of the 113 nurses in the larger study, 20 nurses involved in active bedside care were selected by simple random sampling using research randomizer software. A self-instructional module (SIM) on clinical communication skill for nurses (used in the larger study) incorporated the SBAR format in which information and use of SBAR was illustrated. The content validity of the format was established by giving it to clinical and nursing experts. The SBAR form was disseminated for use in clinical setting for hands off during shift handover.
Inter-rater reliability of the audit checklist was established using the kappa statistic to determine consistency among raters (κ = 0.91, P < 0.001). A retrospective audit was undertaken at 1st week (referred to as A1) and 16th week (referred to as A2) respectively, post introduction of SIM. Items in the audit checklist were scored as “1” for yes and “0” for no and “9” if not applicable. Though 100% compliance would be considered as excellent, a benchmark of 80% and above was considered as acceptable. The audit checklist had 29 items in four areas. The number of items under each domain was a situation (10), background (7), assessment (7), and recommendation (5). The content of the SBAR format was verified with clinical record of the patient. Nurses opinion about the SBAR form was captured using a three point (i.e., not at all, somewhat and very much) Likert scale having seven items and three multiple choice questions. The data were analyzed using descriptive (frequency and percentage) and inferential statistics (nonparametric test: Wilcoxon signed rank test).
Results
The study included 20 nurses in the first audit and 19 nurses in the second audit. The survey on nurse's opinion was completed by 17 nurses.
Demographic variables
There were 6 (30%) males and 14 (70%) female nurses. Majority (80%) of nurses were in age group 21-30 years. There was an equal representation of qualifications, i.e., nurses who had a diploma or a degree in nursing. Nearly, two-third (60%) of them had <5 years of experience. SBAR score was correlated with demographic variables. A statistically significant association (P = 0.019) was seen between overall audit scores and education/qualification. Nurses who were certified with a graduate degree showed a better score as compared to nurses who held a diploma in nursing [Table 1].
Table 1.
Demographic variables of nurses
| Demographic variable | Frequency (%) |
|---|---|
| Gender | |
| Male | 6 (30) |
| Female | 14 (70) |
| Age in years | |
| 21-30 | 16 (80) |
| 31-40 | 4 (20) |
| Education | |
| Diploma in nursing | 10 (50) |
| Degree in nursing | 10 (50) |
| Experience in years | |
| 0-5 | 12 (60) |
| 6-10 | 6 (30) |
| 11-15 | 1 (5) |
| 16-20 | 1 (5) |
Audit findings
Compliance to SBAR documentation was audited at 2 times points A1 (first audit in 1st week) and A2 (second audit in 16th week). There was an absolute difference of 4% between A1 and A2, valid percent score was A1 (mean: 82, range: 61-96) and A2 (mean: 86, range: 70-96). There was a significant improvement (P = 0.043) in overall scores between A1 (mean: 23.20, standard deviation [SD]: 2.96) and A2 (mean: 24.26, SD: 2.20). This difference may be due to the routine use of the form. When analyzed further into different domains of SBAR, a significant improvement was seen in “Situation” domain (P = 0.045) as compared to other domains. The difference can be attributed to simplicity and objectivity of the content in situation domain.
Analysis on compliance to the four domains of situation, background, assessment, recommendation
There was an overall improvement in all sections of SBAR [Figure 1] from first observation to second observation.
Figure 1.
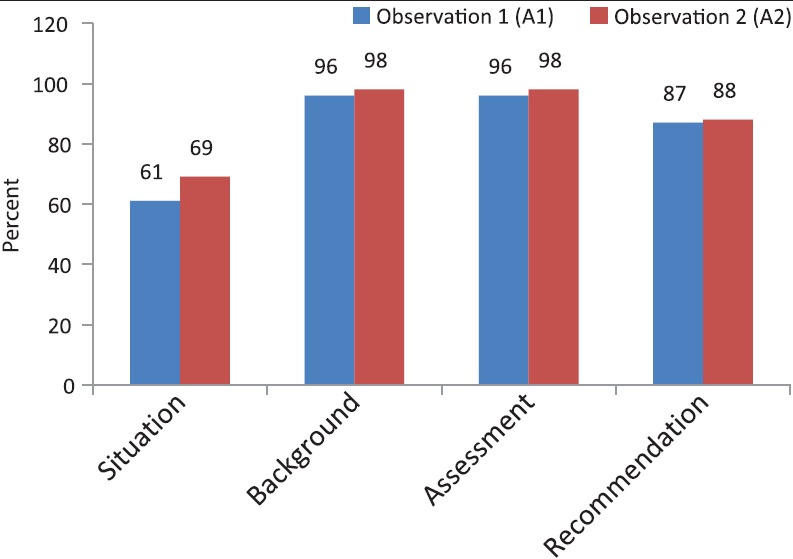
Section wise distribution of observation scores-situation, background, assessment, recommendation
Situation
During A1, only 45% (n = 20) of the nurses in the study group had documented the age of patient while it was 79% (n = 19) in A2. Item, wise comparison of A1 and A2, was carried out using McNemar test. Out of seven items in this domain, there was a significant difference in one item only, i.e., documentation of age (P = 0.039). There was only a marginal improvement (A1-40%, A2-47%) in documentation related to patient's allergies and relevant past history while identifying comorbidities decreased from 45% in A1 to 5% in A2 [Table 2].
Table 2.
Distribution of nurses based on observation of situation component of situation, background, assessment, recommendation
| Items | A1 (n = 20) (%) | A2 (n = 19) (%) |
|---|---|---|
| Patients name | 20 (100) | 19 (100) |
| Unit | 17 (85) | 18 (95) |
| Age | 9 (45) | 15 (79) |
| Register number | 17 (85) | 19 (100) |
| Date of admission | 9 (45) | 10 (53) |
| Diagnosis | 16 (80) | 15 (79) |
| Surgery* | 8 (73) | 11 (100) |
| Allergies | 8 (40) | 9 (47) |
| Relevant past history | 4 (20) | 8 (42) |
| Comorbidities | 9 (45) | 1 (5) |
*Valid percentage is calculated (n = 11)
Background
Though 95% compliance was seen in most of the items under “Situation” in both audits, important information like the current treatment of patient (e.g., antiepileptic, or withhold tablet amlodipine, injection 5 fluorouracil is on continuous infusion and patient is on injection clexane) was not documented. Injection clexane is a high alert drug and requires nursing assessment and observation for bleeding, petechiae, hematuria, and black tarry stools. Transmission of this information is essential for patient care and safety [Table 3].
Table 3.
Distribution of nurses based on observation of background component of situation, background, assessment, recommendation
| Items | A1 (n = 20) (%) | A2 (n = 19) (%) |
|---|---|---|
| Medications, blood products | 19 (95) | 18 (95) |
| Urine | 19 (95) | 19 (100) |
| Bowel | 19 (95) | 18 (95) |
| Mobility | 19 (95) | 19 (100) |
| Diet | 19 (95) | 19 (100) |
| Lines | 19 (95) | 19 (100) |
| Intravenous fluids on flow | 19 (95) | 18 (95) |
Assessment
There was almost 100% compliance in most of the items under the “Assessment” category in both audits. An area that needed to be focused on in A1 was pain score, Glasgow coma scale (GCS) score and fall risk as the compliance was 85%. Pain is considered to be a fifth vital sign and as a routine 4 hourly assessments is carried out. The area where nurses do not pay much attention is on GCS and fall risk assessment. Both these areas are important especially in an oncology unit, where patients may have neurological problems, are in older age group and are on medications for comorbidities, and thereby prone to electrolyte imbalance or have gastrointestinal disturbances. In A2, the compliance was 100% [Table 4].
Table 4.
Distribution of nurses based on observation of assessment component of situation, background, assessment, recommendation
| Items | A1 (n = 20) (%) | A2 (n = 19) (%) |
|---|---|---|
| Airway | 20 (100) | 19 (100) |
| Breathing | 20 (100) | 19 (100) |
| Skin | 20 (100) | 19 (100) |
| Vital signs | 20 (100) | 17 (89) |
| Difficulty in communication | 19 (95) | 19 (100) |
| Is there a drains | 11 (92) | 10 (91) |
| Pain score/Glasgow coma scale score/fall risk | 17 (85) | 19 (100) |
Recommendation
Compliance was around 90% in most of the area of recommendation. Though there was around 85-95% compliance related to investigation and reports, in some of the patient files that were sampled, the information related to pending reports such as those pertaining to serum electrolytes, calcium, or urine was not documented. Referrals for physiotherapy, psychiatry, and dietician reference were also not captured in approximately 90% of forms. One area which needed improvement was in plan of care. Only about 70% of the nurses had documented the plan of care. Information related to 4 hourly mouth care, watch for the motor deficit, neurological monitoring, incentive spirometry, observation for bleeding, discharge plan, care of tracheostomy tube, pressure points, and use of thromboembolic deterrent stocking was not incorporated in plan of care. This may be due to lack of clarity about information to be documented [Table 5].
Table 5.
Distribution of nurses based on observation of recommendation component of situation, background, assessment, recommendation
| Items | A1 (n = 20) (%) | A2 (n = 19) (%) |
|---|---|---|
| Any investigation/reports pending | 17 (85) | 18 (95) |
| Have the critical results intimated | 20 (100) | 19 (100) |
| Any referrals | 19 (95) | 17 (89) |
| Any special orders | 17 (85) | 16 (84) |
| Plan of care | 14 (70) | 14 (74) |
Nurses opinion about situation, background, assessment, recommendation
Most (79%) of the nurses expressed that they found the SBAR form for shift handover very useful. This was consistent with a study by Velji et al. nurses reported use of SBAR helped them to “organize their thinking” and streamline data.[4]
They also opined that all information relevant to patient care was only somewhat (68%) captured, and 63% of nurses felt that it will improve patient safety. The contents were not at all difficult for 74% of nurses. Only 53% of nurses felt that patient involvement in documenting information in SBAR was very much necessary [Figure 2].
Figure 2.
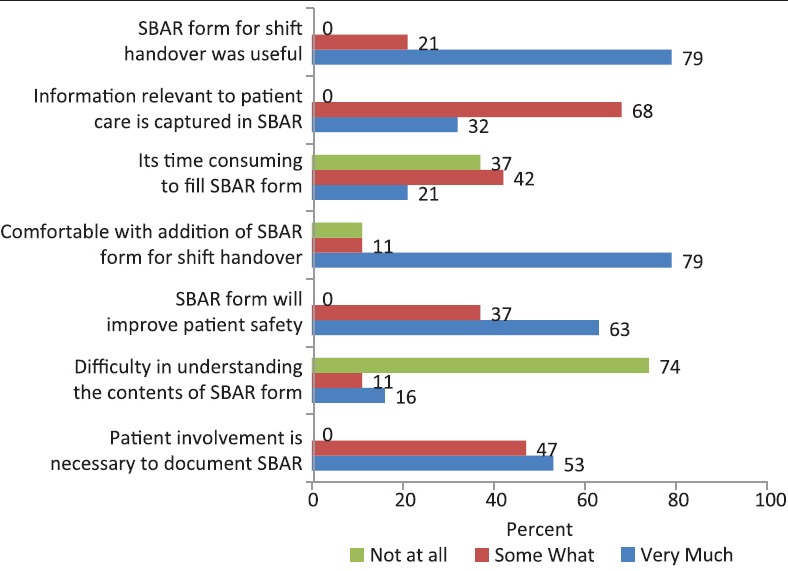
Item wise distribution of nurse's opinion about situation, background, assessment, recommendation
It was interesting to note that though majority (68%) of the nurses expressed that they completed the documentation in 5-10 min, 21% nurses felt filling SBAR form was very much time consuming, while 42-37% expressed somewhat and not at all, respectively. They also opined that Assessment was easy (47%) to document while recommendation was the difficult (47%) part [Figure 3].
Figure 3.
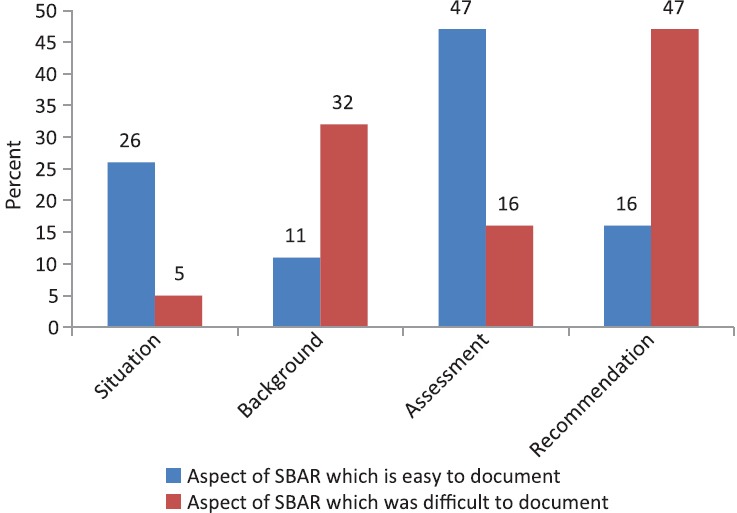
Situation, background, assessment, recommendation — Level of difficulty
Discussion
This study aimed to examine the introduction of SBAR into nursing practice using a self-instructional method. Currently, use of SBAR is not prevalent in hospitals across India. With the advent to accreditation concept in India, where the focus is on patient safety, it has become essential for nurses to excel in the work they undertake. Handover of the patient being an important area where information of the patient is transferred from one shift to another. The SBAR has been tested in Western countries and have been a part of standard care. It was unclear whether or not the SBAR tool would be commensurate with the needs of Indian nurses.
The findings suggest that introduction of a standardized handover tool like SBAR helped nurses to capture all relevant information pertaining to the patient. It is noted that in many instances important clinical findings were not documented. Laws and Amato, in his review, found reports of inconsistency between information provided and the actual status of the patient.[11] Miller et al., in his study also suggested that nurses need to recognize and identify important clinical cues and act promptly to ensure patient safety.[12] Around 21% nurses felt SBAR form documentation as time-consuming. This was also brought forth by Renz et al. where 28% of nurses responded that SBAR tool was time-consuming.[13] It can be seen that only 53% of nurses felt patient involvement in documenting information and plan of care was necessary.
Patient's involvement is crucial as it provides them with an opportunity to ask questions, clarify, and share information which makes them less anxious, more compliant with the plan of care and more satisfied because they know what things are being monitored throughout the shift.[11] One area which needs improvement is in the documenting plan of care.
Limitations
The SBAR format was a self-report tool and some nurses might have had difficulty in understanding the contents required for documentation, and therefore, the accuracy of entry of SBAR data were questionable:
Content analysis of all the SBAR forms was not done.
The sample size was small and hence cannot be generalized.
Patient care outcomes in terms of average length of stay were not evaluated but are important considerations for future research.
Conclusion
Nurses have a vital role in ensuring successful team performance by transferring relevant and critical information. SBAR technique helps in focused and easy communication between nurses especially during transition of patient care from one nurse to another. SBAR communication has become a standard, across disciplines as a mode of hands off communication.[9] Use of standardized hands off communication during bedside shift handover is essential for patient safety, as the benefits for patients outweigh the risks and cost of implementation.[14] The patient, who is the focus of all interaction, should be involved in decision-making and updated with information relevant to them, which in turn will help in reducing errors and create a sense of well-being and satisfaction.
The results suggest that individual and team training in various aspects of SBAR need to be initiated to bring about an impact by use of SBAR form. Importance and relevance of capturing information related allergies, comorbidities, assessment of pain, neurological monitoring, and aspects to be documented under the plan of care need to be incorporated as a regular part of continuing education program. An audit to look for reduced number of incidents related to communication failures is essential for long-term evaluation of patient outcomes[3] and thus, provide safe and quality care to patients.
Implications
SBAR form modified to organizational requirement can play an important role in transferring of information from one nurse to next during bedside shift handoff. SBAR can play an important role in communication between nurse and physician, especially when the doctor is not available in the premises and vital information regarding patient status need to be communicated. Though SBAR is regularly used in Western world and has been found to be effective, it is time that Indian nurses understand the importance of a standardized approach to bedside shift handoff and implement in their clinical practice to bring about a positive outcome for patients and thus play an important role in ensuring patient safety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was written on the basis of a presentation given at the AONS 2015 Conference held in Seoul Korea by the Asian Oncology Nursing Society.
References
- 1.Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joint Commission. “Joint Commission Center for Transforming Healthcare.” Joint Commission Resources Hot topics in health care — transitions of care: the need for a more effective approach to continuing patient care. [Updated (2012)]. http://www. jointcommission. org/assets/1/18/Hot_Topics_Transitions_of_Care. pdf .
- 3.Clark E, Squire S, Heyme A, Mickle ME, Petrie E. The PACT project: Improving communication at handover. Med J Aust. 2009;190(11 Suppl):S125–7. doi: 10.5694/j.1326-5377.2009.tb02618.x. [DOI] [PubMed] [Google Scholar]
- 4.Velji K, Baker GR, Fancott C, Andreoli A, Boaro N, Tardif G, et al. Effectiveness of an adapted SBAR communication tool for a rehabilitation setting. Healthc Q. 2008;11:72–9. doi: 10.12927/hcq.2008.19653. [DOI] [PubMed] [Google Scholar]
- 5.Wayne JD, Tyagi R, Reinhardt G, Rooney D, Makoul G, Chopra S, et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65:476–85. doi: 10.1016/j.jsurg.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Griffin T. Bringing change-of-shift report to the bedside: A patient-and family-centered approach. J Perinat Neonatal Nurs. 2010;24:348–53. doi: 10.1097/JPN.0b013e3181f8a6c8. [DOI] [PubMed] [Google Scholar]
- 7.Thomas CM, Bertram E, Johnson D. The SBAR communication technique: Teaching nursing students professional communication skills. Nurse Educ. 2009;34:176–80. doi: 10.1097/NNE.0b013e3181aaba54. [DOI] [PubMed] [Google Scholar]
- 8.Organizations JCoAoH. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety: Joint Commission. 2013 [Google Scholar]
- 9.Narayan MC. Using SBAR communications in efforts to prevent patient rehospitalizations. Home Healthc Nurse. 2013;31:504–15. doi: 10.1097/NHH.0b013e3182a87711. [DOI] [PubMed] [Google Scholar]
- 10.Coiera E, Tombs V. Communication behaviours in a hospital setting: An observational study. BMJ. 1998;316:673–6. doi: 10.1136/bmj.316.7132.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laws D, Amato S. Incorporating bedside reporting into change-of-shift report. Rehabil Nurs. 2010;35:70–4. doi: 10.1002/j.2048-7940.2010.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 12.Miller K, Riley W, Davis S. Identifying key nursing and team behaviours to achieve high reliability. J Nurs Manag. 2009;17:247–55. doi: 10.1111/j.1365-2834.2009.00978.x. [DOI] [PubMed] [Google Scholar]
- 13.Renz SM, Boltz MP, Wagner LM, Capezuti EA, Lawrence TE. Examining the feasibility and utility of an SBAR protocol in long-term care. Geriatr Nurs. 2013;34:295–301. doi: 10.1016/j.gerinurse.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Novak K, Fairchild R. Bedside reporting and SBAR: Improving patient communication and satisfaction. J Pediatr Nurs. 2012;27:760–2. doi: 10.1016/j.pedn.2012.09.001. [DOI] [PubMed] [Google Scholar]


