Abstract
Purpose/Objectives
To evaluate the feasibility and acceptability of a newly developed web-based, couple-oriented intervention called Prostate Cancer Education and Resources for Couples (PERC).
Design
Quantitative, qualitative, mixed-methods approach.
Setting
Oncology outpatient clinics at the University of North Carolina (UNC) Lineberger Comprehensive Cancer Center at UNC–Chapel Hill.
Sample
26 patients with localized prostate cancer (PCa) and their partners.
Methods
Pre- and postpilot quantitative assessments and a postpilot qualitative interview were conducted.
Main Research Variables
General and PCa-specific symptoms, quality of life, psychosocial factors, PERC's ease of use, and web activities.
Findings
Improvement was shown in some PCa-specific and general symptoms (small effect sizes for patients and small-to-medium effect sizes for partners), overall quality of life, and physical and social domains of quality of life for patients (small effect sizes). Web activity data indicated high PERC use. Qualitative and quantitative analyses indicated that participants found PERC easy to use and understand, as well as engaging, of high quality, and relevant. Overall, participants were satisfied with PERC and reported that PERC improved their knowledge about symptom management and communication as a couple.
Conclusions
PERC was a feasible, acceptable method of reducing the side effects of PCa treatment–related symptoms and improving quality of life.
Implications for Nursing
PERC has the potential to reduce the negative impacts of symptoms and enhance quality of life for patients with localized PCa and their partners, particularly for those who live in rural areas and have limited access to post-treatment supportive care.
Keywords: symptom management, web-based, eHealth, intervention, quality of life, couple, localized prostate cancer
The incidence of localized prostate cancer (PCa) has risen dramatically in the past several decades with the widespread use of prostate-specific antigen testing. About 70%–90% of patients with localized PCa are treated with surgery or radiation, with or without hormonal treatment; younger patients more frequently choose aggressive treatment in the form of radical prostatectomy (Cooperberg, Broering, & Carroll, 2010; Schymura et al., 2010). Potential side effects include transient or persistent bowel, hormonal, sexual, and urinary symptoms; general symptoms (e.g., fatigue, pain, sleep disturbance); and emotional distress. These symptoms reduce patients' quality of life and negatively affect their relationship with their partners (Ferrer et al., 2008; Gore, Kwan, Lee, Reiter, & Litwin, 2009; Litwin et al., 2007; Sanda et al., 2008; Song et al., 2011).
Partners are also affected by these symptoms, experiencing as much distress, decreased quality of life, and general symptoms as patients (Northouse, Mood, Montie, et al., 2007; Song et al., 2011). Partners play an integral caregiver role, influencing patients' medical decisions, symptom management, and self-care behaviors (Adams, Boulton, & Watson, 2009; Ervik, Nordøy, & Asplund, 2013). Because of this fundamental interdependence, patients with localized PCa might benefit from working with their partners to manage symptoms (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008) and to minimize the detrimental effects of PCa treatment on the quality of life of both members (Chou et al., 2011; Resnick et al., 2013).
However, to date, few couple-focused interventions have been developed to help patients and partners manage PCa treatment–related symptoms and the associated emotional stress (Badger et al., 2011; Campbell et al., 2007; Canada, Neese, Sui, & Schover, 2005; Giarelli, McCorkle, & Monturo, 2003; Manne, Babb, Pinover, Horwitz, & Ebbert, 2004; Manne et al., 2011; McCorkle, Siefert, Dowd, Robinson, & Pickett, 2007; Northouse, Mood, Schafenacker, et al., 2007; Schover et al., 2012). Multisession in-person interventions are expensive to deliver and rely on a limited supply of professionals qualified to deliver them effectively. However, eHealth interventions have emerged as an innovative and often efficacious vehicle for using the Internet as a means of delivering interventions to large numbers of people at a lower cost (Strecher, 2007).
The authors of the current article developed a couple-focused, web-based intervention for PCa symptom management called Prostate Cancer Education and Resources for Couples (PERC). PERC takes a supportive educational approach to helping couples work together to mitigate the impact of patients' symptoms after treatment for PCa, which may improve quality of life for patients and partners. This article describes the feasibility and acceptability results from initial evaluations of the PERC program in a pilot study of patients with localized PCa and their partners.
Methods
PERC was developed by a team of nurses, physicians, a psychologist, a media specialist, web designers, and programmers. It integrated two components: (a) the family involvement and symptom management modules from the FOCUS program, a theory-based, family-oriented intervention that explores family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management, and has been shown to improve quality of life among patients with PCa and their partners (Northouse, Mood, Schafenacker, et al., 2007) and (b) empirically based evidence and guidelines for symptom management (e.g., PCa survivorship care guidelines) (National Comprehensive Cancer Network [NCCN], 2014; NCCN & American Cancer Society, 2005; Skolarus et al., 2014). The resulting intervention protocol was reviewed and informed by a panel of six urologic oncologists and three nurse practitioners at a university-affiliated cancer hospital (University of North Carolina [UNC] Lineberger Comprehensive Cancer Center at UNC–Chapel Hill) and two community hospitals (Carolinas HealthCare System and Carolinas Medical Center–University). Various strategies were used to address the potential for low literacy among users. For example, PERC included audio-enhanced Microsoft PowerPoint® presentations and video clips to supplement text, and it also used plain language (Nielsen-Bohlman, Panzer, & Kindig, 2004; U.S. Department of Health and Human Services [USDHHS], 2006), following guidelines at www.plainlanguage.gov to ensure an accessible reading level (i.e., sixth- to eighth-grade level, as evaluated with the SMOG Readability Formula) (McLaughlin, 1969). In addition, content was developed with the goal of improving the information itself (Centers for Medicare and Medicaid Services, 2012) to capture readers' attention, ensuring that they find, understand, and use information of personal interest (Centers for Medicare and Medicaid Services, 2012; Nielsen-Bohlman et al., 2004).
Usability testing was conducted on the PERC prototype website to obtain feedback from three patients who had completed treatment for localized PCa and their partners. Paired-user testing involves end users in the design process, gathering information through natural discussion (Bastien, 2010; Wilson & Blostein, 1998) to yield a program that more closely meets their needs (Damodaran, 1996). Contextual interviews (USDHHS, 2015) using a think-aloud protocol (Creswell, 2013) provided qualitative data about couples' experiences with the PERC website (e.g., design, navigation scheme, graphical images) while they navigated the website. Each couple used PERC while verbalizing their actions and providing suggestions for enhancements; the couples were guided by a usability expert with extensive experience designing web-based interventions. Sessions were video recorded, and a notetaker monitored couples' interactions with the program and documented feedback and any problems with using the site. Responses guided refinement of the PERC website for this pilot study.
The PERC website included seven education modules for couples to review; two modules were mandatory, and five modules were optional. The mandatory modules provided information about how couples can work as a team (e.g., communication) and various survivorship issues (e.g., distress, relaxation, communication with healthcare team). The optional modules focused on the management of PCa-specific symptoms (i.e., bowel, hormonal, sexual, and urinary issues) and general symptoms (e.g., fatigue, pain, sleep disturbance); couples chose modules to review according to the presence of symptoms in patients or partners. The text and audio-enhanced slides contained the same information, allowing users to select their preferred medium for accessing it. Modules also included links to videos demonstrating relevant skills (e.g., Kegel exercises), and assignments were available to encourage couples to share personal experiences with symptoms and to collaboratively develop management strategies. For couples who wanted additional information, PERC also provided a Prostate Cancer Resource Center with web links to different organizations and online resources. Each module provided 10–20 minutes of information; additional time was needed to complete assignments. After each module, couples were encouraged to practice skills they learned from the module, discuss the symptoms and their positive and negative effects on their daily lives, and brainstorm strategies to minimize the negative effects. Couples were also encouraged to review modules and complete the assignments together, but they could choose to complete PERC individually. Each couple was given a maximum of eight weeks to complete the modules; they were asked to complete one module each week or to complete the modules at their own pace.
Program Evaluation and Measures
PERC feasibility and acceptability were evaluated using a mixed-methods approach. Recruitment and retention rates, pre- and postpilot assessments, and website activity data tracking (e.g., number of logins, time spent on the site) were evaluated quantitatively. Patients and partners separately completed online surveys before and after the intervention period, which ranged from three to eight weeks. The measurements used in this pilot study have been proven to be valid and reliable in previous research. The qualitative evaluation included postpilot interviews with a subset of couples in the pilot study.
Quality of life was measured using the 27-item Functional Assessment of Chronic Illness Therapy–General (FACT-G) scale (Cella et al., 1993), which measures general quality of life and quality of life in emotional, functional, physical, and social and family domains (Esper et al., 1997). Partners reported their quality of life using the spousal version of FACT-G with modified wording (Northouse et al., 2002). In the authors' previous study, the Cronbach alpha was 0.9 for patients with PCa and their partners (Song et al., 2011).
Symptom distress related to PCa-specific symptoms in patients was measured using the 26-item Expanded Prostate Cancer Index Composite (EPIC) (Wei, Dunn, Litwin, Sandler, & Sanda, 2000). Subscale scores for bowel, hormonal, sexual, and urinary (i.e., irritability and incontinence) symptoms were used. Partners completed the modified four-item EPIC intended for spouses to assess the extent to which their partner's symptoms were a problem for them (Song et al., 2011). The Cronbach alpha ranged from 0.74–0.9 in the authors' previous study of patients with PCa and their partners (Song et al., 2012). General symptoms (e.g., fatigue, pain, sleep disturbance) were measured with the 21-item symptom scale, in which patients and partners rated their own symptoms (Mood, Song, Kershaw, & Northouse, 2007). The Cronbach alpha ranged from 0.76–0.84 in the authors' previous study (Song et al., 2012).
Dyadic communication about PCa was measured using a 21-item, five-point Likert-type Mutuality and Interpersonal Sensitivity Scale (Lewis, 1996). The Cronbach alpha ranged from 0.9–0.94 in the authors' previous study (Song et al., 2012). Relationship satisfaction was measured with the Relationship Assessment Scale, a seven-item, five-point Likert-type scale measure of global relationship satisfaction. The alpha coefficients for reliability and validity ranged from 0.73–0.9 in previous studies (Hendrick, Dicke, & Hendrick, 1998).
Data about web activity (e.g., number of logins, time spent on the site) were collected through a built-in, automatic tracking system. Perceived ease of use (Brooke, 1996; Davis, 1989) was a postpilot online questionnaire. Personal factors were self-reported and included participant gender, age, race and ethnicity, education, work status, and annual household income. Health literacy was measured using the single-item literacy screener (Morris, MacLean, Chew, & Littenberg, 2006). Type of treatment was collected from patients' medical records. This information was provided to the recruiter by clinicians as part of the eligibility screening process.
The postpilot exit interviews were conducted using guidelines from www.usability.gov a semistructured interview guide was used to ask couples about their experience with PERC. Participants were interviewed first as couples to identify problems with the paired-user features, then separately to identify specific issues they individually wanted to share. Each interview was audio recorded and lasted 45–60 minutes. Two experienced qualitative researchers conducted the interviews. To ensure consistency and reduce variability, these researchers were involved in developing the interview guide. They also listened to each other's audio recordings of participants and had pre- and postinterview discussions.
Participants
To be eligible for the current study, patients had to (a) be diagnosed with localized PCa, (b) have completed initial primary treatment (surgery or radiation therapy, with or without hormonal therapy), (c) have a partner willing to participate in the study, and (d) have access to a computer and the Internet. The patient's partner had to (a) be aged 21 years or older, (b) be identified as the partner by the patient, and (c) not have been diagnosed with any cancer or been the recipient of any cancer treatment within the past 12 months (so couples could focus on managing PCa). Patients and partners needed to be able to read, speak, and write English.
A subset of couples who completed the pilot study participated in postpilot telephone interviews. These couples were selected to maximize representation of patient demographic characteristics, including type of treatment (surgery versus radiation therapy, with or without hormonal therapy), age (aged 65 years or younger versus aged older than 65 years), and race (Caucasian versus African American). The goal was to capture potentially diverse feedback and comments on PERC.
Patients were recruited from the UNC Lineberger Comprehensive Cancer Center after obtaining institutional review board approval. Partners were recruited in person with patients if they presented at the clinic or through a follow-up correspondence after the patient gave permission to contact his partner. All participants provided informed consent through an automatic online process. Weekly emails were sent to remind couples about program elements scheduled for completion. After completing the pre- or postpilot assessment and, for those who completed it, the postpilot telephone interview, participants selected and then received either a $30 check or gift card.
Data Analysis
Descriptive statistics were calculated separately for patients and partners. The small sample size provided limited power to use inferential statistics; therefore, between-group effect sizes were used to evaluate treatment effects (i.e., small, d = 0.2; medium, d = 0.5; and large, d = 0.8) (Cohen, 1988). Effect sizes were calculated using Dunlap's method, which accounts for correlation between measures (Dunlap, Cortina, Vaslow, & Burke, 1996).
A thematic qualitative analysis was performed on the postpilot telephone interviews, which were audio recorded. Two researchers independently reviewed each recording and discussed for consensus and appropriate interpretation of context. Main themes and values were summarized.
Results
Among 51 patients who were eligible, 25 were either not interested in the study or did not respond to the authors' follow-up correspondence via mail, email, or telephone calls. Therefore, 26 couples were recruited, producing a recruitment rate of 51%. Twenty-five couples (96%) completed PERC, and 22 completed the postintervention survey; the retention rate was 85%. Dropouts were because of family death (n = 1), family illness (n = 1), and loss to follow-up (n = 2). The final sample size for analysis was 22 couples. Table 1 displays the characteristics of patients and partners.
Table 1. Characteristics of Patient-Partner Dyads (N = 22).
| Patients | Partners | |||
|---|---|---|---|---|
|
|
|
|||
| Characteristic | X̄ | SD | X̄ | SD |
| Age (years) | 62.95 | 08.22 | 59.32 | 10.67 |
| Distance from home to hospital (miles) | 81.56 | 93.85 | – | – |
| Length of relationship (years) | 28.59 | 17.34 | – | – |
| Time since diagnosis (months) | 19.05 | 21.39 | – | – |
|
| ||||
| Characteristic | n | n | ||
|
| ||||
| Education | ||||
| High school or less | 07 | 06 | ||
| College | 13 | 14 | ||
| Graduate degree | 02 | 02 | ||
| Family income ($)a | ||||
| 30,000 or less | 04 | – | ||
| 30,001–50,000 | 02 | – | ||
| 50,001–75,000 | 07 | – | ||
| 75,001 or greater | 09 | – | ||
| Health literacy level | ||||
| Never had problems | 17 | 17 | ||
| Have some problems | 05 | 05 | ||
| Raceb | ||||
| Caucasian | 16 | – | ||
| African American | 6 | – | ||
| Type of treatment | ||||
| Radiation therapy | 13 | – | ||
| Surgery | 09 | – | ||
Patient- and partner-reported family incomes were the same.
Partner race was not obtained.
Quantitative Evaluation
Preintervention data (see Table 2) suggested that patients and partners reported relatively mild symptoms, good quality of life, and positive psychosocial outcomes compared to participants in previous studies (Song et al., 2011). Pre- to postintervention changes indicated improvement in urinary irritability and bowel dysfunction scores for patients (d = 0.18 and d = 0.17, respectively). Observed improvement in partners' perception of patients' PCa symptoms as problems was particularly promising (0.18 to 0.51). Small effect sizes were also observed for improvement of general symptoms for patients and partners (d = 0.21 and d = 0.38, respectively). Improvement in physical and social quality of life was promising for patients (d = 0.32). A small increase (d = 0.25) in social quality of life for partners was noted.
Table 2. Means, Standard Deviations, and Effect Sizes of Study Variables and Web Activities.
| Patients | Partners | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Pre | Post | Pre | Post | |||||||||
|
|
|
|
|
|||||||||
| Variable | na | X̄ | SD | X̄ | SD | d | na | X̄ | SD | X̄ | SD | d |
| Bowel dysfunctionb | 22 | 94.89 | 10.2 | 96.59 | 7.57 | 0.17 | 22 | 89.77 | 18.35 | 100 | – | – |
| Couple cancer communication | 22 | 45 | 6.49 | 43.73 | 3.98 | −0.23 | 22 | 42.73 | 10.17 | 43.55 | 7.97 | 0.09 |
| Current concerns | 21 | 9 | 8.14 | 8.36 | 6.69 | −0.15 | 21 | 8.76 | 7.08 | 8.95 | 7.73 | −0.01 |
| Emotional domain QOL | 22 | 21.41 | 2.24 | 21.5 | 2.2 | 0.04 | 22 | 20.36 | 3.43 | 20.45 | 4.4 | 0.02 |
| Functional domain QOL | 22 | 22.73 | 4.31 | 22.68 | 5.86 | −0.01 | 22 | 20.88 | 5.54 | 21 | 6.57 | 0.02 |
| Hormonal dysfunctionb | 22 | 89.32 | 13.83 | 90.68 | 10.83 | 0.1 | 22 | 77.27 | 26.62 | 86.36 | 22.79 | 0.28 |
| General QOL (FACT-G) | 22 | 91.15 | 11.42 | 92.91 | 13.54 | 0.14 | 22 | 88.31 | 14.94 | 87.36 | 17.36 | −0.06 |
| General symptoms | 22 | 5.95 | 5.79 | 4.82 | 4.54 | −0.21 | 22 | 7.45 | 6.1 | 5.78 | 5.84 | −0.38 |
| Physical domain QOL | 22 | 24.33 | 3.47 | 25.32 | 2.75 | 0.32 | 22 | 23.57 | 4.59 | 23.72 | 4.98 | 0.03 |
| Relationship satisfaction | 22 | 19.27 | 2.21 | 18.82 | 2.02 | −0.21 | 22 | 18.5 | 2.52 | 17.91 | 2.37 | −0.24 |
| Sexual dysfunctionb | 21 | 49.08 | 37.21 | 43.78 | 39.85 | −0.14 | 22 | 60.23 | 40.58 | 64.88 | 41.01 | 0.18 |
| Social and family domain QOL | 22 | 22.68 | 4.55 | 23.41 | 4.89 | 0.15 | 22 | 23.5 | 5.08 | 22.18 | 5.31 | −0.25 |
| Urinary incontinenceb | 22 | 68.51 | 13.67 | 68.99 | 10.61 | 0.04 | 22 | 82.95 | 24.86 | 92.86 | 14.02 | 0.51 |
| Urinary irritabilityb | 22 | 88.07 | 16.58 | 90.91 | 14.14 | 0.18 | 22 | 82.95 | 24.86 | 92.86 | 14.02 | 0.51 |
Four couples dropped out of the study. Dropouts were because of family death (n = 1), illness (n = 1), and failure to follow up (n = 2).
Symptoms are considered specific to prostate cancer and were measured using the Expanded Prostate Cancer Index Composite.
FACT-G—Functional Assessment of Chronic Illness Therapy–General; QOL—quality of life
Note. Higher scores indicate less bowel, hormonal, and sexual dysfunction, as well as less urinary incontinence and irritability. They also indicate fewer general symptoms and current concerns; better overall quality of life and quality of life in the emotional, functional, physical, and social and family domains; increased relationship satisfaction; and more couple cancer communication.
Among the 22 couples who completed pre- and postintervention assessments, eight couples always logged in jointly, five always logged in individually, and nine logged in jointly and individually. The average number of logins per couple was 3.64 (SD = 1.68). For patients, it was 2.73 (SD = 1.2); for partners, it was 2.68 (SD = 1.39). The average total time spent on PERC per couple was 56.96 minutes (SD = 39.74). Individually, patients spent an average of 41.99 minutes (SD = 26.21) on the site, as compared to the average of 43.99 minutes (SD = 43.69) spent by partners. The site's most frequently visited sections were those on sexual dysfunction (77%), fatigue (77%), and urinary dysfunction (76%). Most of the participants (83%) used audio-enhanced slides, and 94% visited the assignment and exercise section. Participants rated PERC as easy to use and understand, engaging, of high quality, and relevant (see Table 3). Overall, the couples were satisfied with PERC and reported that it improved their knowledge about symptom management and communication as a couple.
Table 3. Usability and Satisfaction of the Web-Based Intervention Among Patients and Their Partners.
| Patients (n = 22) | Partners (n = 22) | |||
|---|---|---|---|---|
|
|
|
|||
| Item | X̄ | 95% CI | X̄ | 95% CI |
| The intervention website | ||||
| Is easy to use. | 4.41 | [4.08, 4.73] | 4.59 | [4.24, 4.94] |
| Has an attractive presentation. | 4.41 | [3.98, 4.83] | 4.27 | [3.88, 4.66] |
| Is interesting and engaging. | 4.14 | [3.62, 4.65] | 4.23 | [3.82, 4.64] |
| Responds quickly. | 4.59 | [4.3, 4.89] | 4.45 | [4.13, 4.78] |
| Did not always do what I expected it to do. | 2 | [1.44, 2.56] | 1.95 | [1.43, 2.48] |
| Is unnecessarily complex. | 2 | [1.44, 2.56] | 1.77 | [1.26, 2.28] |
| The content of the website is | ||||
| Written in clear, simple language. | 4.45 | [4.1, 4.81] | 4.64 | [4.34, 4.93] |
| Easy to understand and follow. | 4.41 | [4.01, 4.81] | 4.50 | [4.12, 4.88] |
| Of high quality. | 4.32 | [3.88, 4.76] | 4.18 | [3.76, 4.61] |
| Highly relevant to me. | 4.14 | [3.68, 4.6] | 3.73 | [3.25, 4.2] |
| I found what I was looking for quickly and easily. | 4.41 | [4.03, 4.79] | 4.36 | [4.01, 4.71] |
| The organization of menus seems quite logical. | 4.23 | [3.75, 4.7] | 4.32 | [3.9, 4.74] |
| I had to click too many times to complete typical tasks. | 1.91 | [1.36, 2.45] | 1.73 | [1.31, 2.14] |
| Using the website is frustrating. | 1.36 | [1.01, 1.71] | 1.50 | [1.12, 1.88] |
| I am satisfied with the | ||||
| Amount of time given to review each week. | 2.68 | [2.29, 3.08] | 2.64 | [2.26, 3.01] |
| Information from PERC. | 3.14 | [2.79, 3.48] | 2.82 | [2.35, 3.26] |
| Quality of information. | 3.09 | [2.76, 3.42] | 2.91 | [2.46, 3.36] |
| The PERC program has | ||||
| Increased my knowledge about managing symptoms. | 3.91 | [3.33, 4.49] | 4.09 | [3.71, 4.48] |
| Improved my knowledge about how cancer has affected my partner and our relationship. | 3.86 | [3.35, 4.38] | 3.91 | [3.46, 4.36] |
| Improved my communication with my partner about sensitive topics related to prostate cancer. | 3.59 | [3, 4.18] | 3.77 | [3.32, 4.23] |
| Improved how I manage symptoms. | 3.73 | [3.13, 4.33] | 3.73 | [3.27, 4.18] |
| The weekly exercises and assignments are helpful. | 3.73 | [3.21, 4.24] | 3.64 | [3.13, 4.14] |
| My partner and I work together. | 4.45 | [4.07, 4.83] | 4.14 | [3.72, 4.55] |
CI—confidence interval; PERC—Prostate Cancer Education and Resources for Couples
Note. Items were rated on a 1–5 scale, with 5 indicating strong agreement.
Qualitative Evaluation
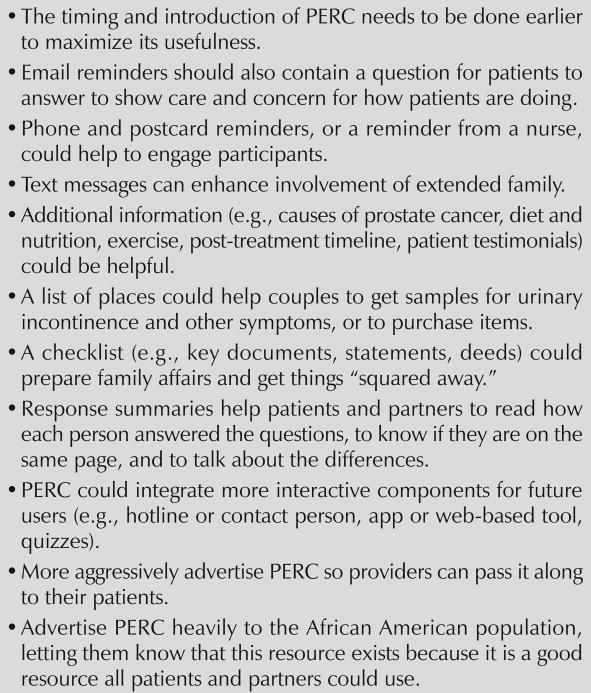
Eight couples completed postpilot interviews; three patients were African American (the rest were Caucasian), and five of the eight patients were aged 65 years or younger. Half had undergone surgery, and half had undergone radiation therapy. Participants reported no Internet connectivity issues when accessing PERC. After reviewing the website jointly (four couples) or independently (four couples), six of the eight couples reported that they had discussed what they read and completed assignments. Participants' comments and suggestions for improvement are summarized in Figure 1.
Figure 1. Participant Suggestions to Improve Prostate Cancer Education and Resources for Couples (PERC).
Participants agreed that PERC was a useful PCa resource for patients and partners, describing it as “an information cornucopia” that was “easy to use.” Other comments indicated that the content was clear, as well as that terminology and text were concise and easy to understand. Participants said finding a trustworthy source for PCa information was sometimes challenging, but that they viewed PERC as a credible source that offered them as much information as they wanted. Participants used PERC as a starting point for further online research or as an informational resource to guide follow-up discussion with their doctors. Key features of PERC that participants liked included the straightforward index to help locate specific information, the option of either watching or reading informational content, concise modules, and content about communication and various symptoms.
Other themes indicated that PERC provided a way for patients and partners to work together and strengthen their relationships during a difficult time. Regarding racial sensitivity, African American participants commented that PCa “does not discriminate” and did not think race-specific information was necessary for PERC. Participants also noted that they liked being able to visit the site at their convenience, choose what information they viewed, and spend more time on issues of primary concern to them.
Discussion
Internet use for health information and health activities is rapidly rising, particularly among older adults (Zickuhr & Madden, 2012; Zulman, Kirch, Zheng, & An, 2011). The quantitative and qualitative findings of the current study support the promise of PERC in helping to manage localized PCa treatment–related symptoms and associated distress among patients and their partners. PERC was found to be a feasible, acceptable method of reducing the side effects of PCa treatment–related symptoms and improving quality of life.
In addition, participants rated PERC as easy to use and understand, and they found it to be engaging, of high quality, and relevant. The high usage rates were encouraging, particularly because PERC targeted older adults—a population that has a relatively large proportion of people with little experience using computers and the Internet.
Several aspects of the development strategy likely were critical to the program's success, but their individual contributions would need to be evaluated with additional research. First, PERC was disseminated via an easy-to-use eHealth program. Using the Internet to disseminate proven interventions overcomes a variety of barriers that limit access to these types of interventions. This approach may be particularly beneficial to patients living far from a comprehensive cancer center or other treatment center who, therefore, have limited access to supportive care. More than half of the participants in the current study lived 50 miles or farther from the treating cancer center. In addition, participants liked that they could access credible information via PERC at their convenience.
Second, the authors adopted various strategies to lower the demand that health literacy places on an educational program. Third, involving providers during development of the intervention protocol, as well as patients with cancer and their partners, particularly those who were older, during usability testing, resulted in a number of important program modifications that improved PERC performance and accessibility. Finally, combining quantitative and qualitative evaluation provides rich data for understanding participants' responses and feedback, which will contribute to further refinement of PERC and its implementation.
Given its focus on couples, participants reported that PERC provided a way for patients and partners to work together and strengthen their relationships during a difficult time. In general, couples liked having the option to log in as a couple or separately. However, quantitative assessments showed decreases in couples' cancer communication and relationship satisfaction. Previous research has indicated that couples coping with cancer who engaged in more frequent and mutual constructive discussions about their relationship had greater marital adjustment (Badr & Taylor, 2006, 2009). Research also shows that when patients had poor erectile dysfunction, couples were more likely to avoid open couple discussions and had greater relationship distress (Badr & Taylor, 2009). In the current pilot study, the authors observed that patients' sexual dysfunction worsened over time. Worsened sexual dysfunction may be associated with poorer marital satisfaction in patients and partners, as well as with decreased couples' cancer communication, despite the PERC intervention. Future research will need to include a control group to examine this hypothesis. Participants in the current study had long-standing relationships (the average length was 29 years) and started PERC with relatively good quality of life and positive psychosocial profiles. The couple components in PERC (e.g., “working as a team,” assignments that encouraged couples to discuss the impact of cancer and brainstorm strategies to minimize its negative effects) may have introduced concepts and ideas that are different from couples' long-standing relationship and communication patterns. Couples may have experienced some difficulty adjusting to new ways of relating to each other, or difficulty talking about sensitive topics they may not have discussed before. Further research is needed to examine these possibilities. The authors plan to integrate the suggestions from participants to further strengthen the couple interaction component of PERC.
Limitations
The current pilot study was limited by several factors. Findings must be interpreted with caution because of the small sample size and low recruitment rate. Replication with larger samples in a randomized, controlled trial would help to establish PERC's promise. In addition, because of funding and time constraints, this pilot study did not include participants who lacked computer or Internet access. About 2% of eligible patients approached for recruitment did not have access to a computer or the Internet. Future research needs to explore and expand resources to ensure computer and Internet access for a broader population of patients and partners. Patients in this study, who were, on average, 19 months postdiagnosis, reported relatively mild symptoms, as well as good quality of life and psychosocial outcomes preintervention. Future research should consider changing the timing of the intervention to right after surgery or during radiation therapy, as the participants suggested, to maximize PERC's usefulness. Also, dissatisfied couples may be relatively unlikely to join couple-oriented studies. Future research is needed to understand how to address the needs of patients and partners in dissatisfied relationships. A couples approach is not relevant to nonpartnered patients. A version of PERC designed for nonpartnered patients may need to include information to help them identify and mobilize support resources, or to improve their own ability to manage their symptoms.
Implications for Nursing
Nurses are at the forefront in the promotion of self-management of symptoms and in the improvement of the health of individuals and families. Lessons learned through conducting this pilot feasibility study suggest that nurses may use technology (e.g., the Internet) to assist individuals with localized PCa—and, potentially, other illnesses—and their families to better understand their illness, enhance their self-management behaviors, and, ultimately, improve their quality of life and reduce the burden of illness. Using technology in nursing practice and research can expand nurses' work and improve access to supportive care for individuals and families who cannot or prefer not to engage in traditional face-to-face care, particularly when dealing with sensitive symptom and illness issues.
Conclusion
PERC was well received, and users reported that the current version of the program provided valuable, high-quality, and relevant content. After refining PERC and optimizing its performance based on participant feedback, critical additional work is needed to evaluate the efficacy of PERC for improving symptom management and quality of life, as well as to explore other benefits of this eHealth approach (e.g., cost effectiveness).
Knowledge Translation.
Prostate cancer and its treatment can cause myriad symptoms that affect the patient and his partner, reducing their quality of life. Patients and partners should be considered as one unit of care.
Couples often experience cancer-related communication difficulties while managing the symptoms of prostate cancer. Better management of symptoms and communication can help to improve the quality of life for patients and partners.
Most patients with cancer have unmet supportive care needs. Web-based intervention has the potential to provide this care for more patients and their families.
Acknowledgments
This study was supported, in part, by the Population Sciences Developmental Award from the UNC Lineberger Comprehensive Cancer Center, the Clinical and Translational Sciences Award (KL2TR001109 and UL1TR001111), the American Cancer Society (No. MRSG-13-154-01-CPPB), and the Urology Care Foundation and Astellas.
Contributor Information
Lixin Song, Email: lsong@unc.edu, the School of Nursing University of North Carolina (UNC)–Chapel Hill and at the UNC Lineberger Comprehensive Cancer Center.
Christine Rini, the Department of Health Behavior in the Gillings School of Global Public Health at the University of North Carolina (UNC)–Chapel Hill and at the UNC Lineberger Comprehensive Cancer Center.
Allison M. Deal, Biostatistician at the UNC Lineberger Comprehensive Cancer Center.
Matthew E. Nielsen, the Division of Urologic Oncology at the UNC Lineberger Comprehensive Cancer Center, as well as an assistant professor in the Department of Urology in the School of Medicine and an adjunct assistant professor in the Departments of Epidemiology and Health Policy and Management at the Gillings School of Global Public Health, all at UNC–Chapel Hill.
Hao Chang, UNC–Chapel Hill and an undergraduate student in the Department of Mathematics at Dartmouth College in Hanover, NH.
Patty Kinneer, the School of Nursing at UNC–Chapel Hill.
Randall Teal, Nutrition Communication for Health Applications and Interventions Core at the UNC Lineberger Comprehensive Cancer Center.
David C. Johnson, Urology resident, Department of Urology, UNC–Chapel Hill.
Mary W. Dunn, both in the Department of Urology, UNC–Chapel Hill.
Barbara Mark, Distinguished Professor in Aging, both in the School of Nursing, all at UNC–Chapel Hill.
Mary H. Palmer, the Helen W. and Thomas L. Umphlet Distinguished Professor in Aging, both in the School of Nursing, all at UNC–Chapel Hill.
References
- Adams E, Boulton M, Watson E. The information needs of partners and family members of cancer patients: A systematic literature review. Patient Education and Counseling. 2009;77:179–186. doi: 10.1016/j.pec.2009.03.027. [DOI] [PubMed] [Google Scholar]
- Badger TA, Segrin C, Figueredo AJ, Harrington J, Shep-pard K, Passalacqua S, et al. Bishop M. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Quality of Life Research. 2011;20:833–844. doi: 10.1007/s11136-010-9822-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H, Taylor CL. Social constraints and spousal communication in lung cancer. Psycho-Oncology. 2006;15:673–683. doi: 10.1002/pon.996. [DOI] [PubMed] [Google Scholar]
- Badr H, Taylor CL. Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psycho-Oncology. 2009;18:735–746. doi: 10.1002/pon.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien JMC. Usability testing: A review of some methodological and technical aspects of the method. International Journal of Medical Informatics. 2010;79:e18–23. doi: 10.1016/j.ijmedinf.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Brooke J. SUS: A ‘quick and dirty’ usability scale. In: Jordan PW, Thomas B, Weerdmeester BA, McClelland IL, editors. Usability evaluation in industry. London, England: Taylor and Francis; 1996. pp. 189–194. [Google Scholar]
- Campbell LC, Keefe FJ, Scipio C, McKee DC, Edwards CL, Herman SH, et al. Donatucci C. Facilitating research participation and improving quality of life for African American prostate cancer survivors and their intimate partners. A pilot study of telephone-based coping skills training. Cancer. 2007;109:414–424. doi: 10.1002/cncr.22355. [DOI] [PubMed] [Google Scholar]
- Canada AL, Neese LE, Sui D, Schover LR. Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer. 2005;104:2689–2700. doi: 10.1002/cncr.21537. [DOI] [PubMed] [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafan B, Linn E, Bonomi A, et al. Brannon J. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Toolkit for making written material clear and effective. 2012 Retrieved from http://www.cms.gov/Outreach-and-Education/Outreach/WrittenMaterialsToolkit/index.html.
- Chou R, Dana T, Bougatsos C, Fu R, Blazina I, Gleitsmann K, Rugge JB. Treatments for localized prostate cancer: Systematic review to update the 2002 US Preventive Services Task Force recommendation. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. Journal of Clinical Oncology. 2010;28:1117–1123. doi: 10.1200/JCO.2009.26.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW. Qualitative inquiry and research design: Choosing among five approaches. 3rd. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Damodaran L. User involvement in the systems design process: A practical guide for users. Behaviour and Information Technology. 1996;15:363–377. [Google Scholar]
- Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13:319–340. doi: 10.2307/249008. [DOI] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. doi: 10.1037/1082-989X.1.2.170. [DOI] [Google Scholar]
- Ervik B, Nordøy T, Asplund K. In the middle and on the sideline: The experience of spouses of men with prostate cancer. Cancer Nursing. 2013;36:E7–E14. doi: 10.1097/NCC.0b013e31824fe1ef. [DOI] [PubMed] [Google Scholar]
- Esper P, Mo F, Chodak G, Sinner M, Cella D, Pienta KJ. Measuring quality of life in men with prostate cancer using the Functional Assessment of Cancer Therapy-prostate instrument. Urology. 1997;50(97):920–928. 00459–7. doi: 10.1016/s0090-4295. [DOI] [PubMed] [Google Scholar]
- Ferrer M, Suárez JF, Guedea F, Fernández P, Macías V, Mariño A, et al. Aguiló F. Health-related quality of life 2 years after treatment with radical prostatectomy, prostate brachytherapy, or external beam radiotherapy in patients with clinically localized prostate cancer. International Journal of Radiation Oncology. 2008;72:421–432. doi: 10.1016/j.ijrobp.2007.12.024. [DOI] [PubMed] [Google Scholar]
- Giarelli E, McCorkle R, Monturo C. Caring for a spouse after prostate surgery: The preparedness needs of wives. Journal of Family Nursing. 2003;9:453–485. doi: 10.1177/1074840703258317. [DOI] [Google Scholar]
- Gore JL, Kwan L, Lee SP, Reiter RE, Litwin MS. Survivorship beyond convalescence: 48-month quality-of-life outcomes after treatment for localized prostate cancer. Journal of the National Cancer Institute. 2009;101:888–892. doi: 10.1093/jnci/djp114. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- Hendrick SS, Dicke A, Hendrick C. The Relationship Assessment Scale. Journal of Social and Personal Relationships. 1998;15:137–142. doi: 10.1177/0265407598151009. [DOI] [Google Scholar]
- Lewis FM. Family home visitation study final report. Bethesda, MD: National Cancer Institute, National Institutes of Health; 1996. [Google Scholar]
- Litwin MS, Gore JL, Kwan L, Brandeis JM, Lee SP, Withers HR, Reiter RE. Quality of life after surgery, external beam irradiation, or brachytherapy for early-stage prostate cancer. Cancer. 2007;109:2239–2247. doi: 10.1002/cncr.22676. [DOI] [PubMed] [Google Scholar]
- Manne S, Babb J, Pinover W, Horwitz E, Ebbert J. Psychoeducational group intervention for wives of men with prostate cancer. Psycho-Oncology. 2004;13:37–46. doi: 10.1002/pon.724. [DOI] [PubMed] [Google Scholar]
- Manne SL, Kissane DW, Nelson CJ, Mulhall JP, Winkel G, Zaider T. Intimacy-enhancing psychological intervention for men diagnosed with prostate cancer and their partners: A pilot study. Journal of Sexual Medicine. 2011;8:1197–1209. doi: 10.1111/j.1743-6109.2010.02163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCorkle R, Siefert ML, Dowd MF, Robinson JP, Pickett M. Effects of advanced practice nursing on patient and spouse depressive symptoms, sexual function, and marital interaction after radical prostatectomy. Urologic Nursing. 2007;27:65–77. discussion 78-80. [PubMed] [Google Scholar]
- McLaughlin GH. Smog Grading: A new readability formula. Journal of Reading. 1969;12:639–646. [Google Scholar]
- Mood D, Song L, Kershaw T, Northouse L. Assessing risk for distress in cancer patients and family caregivers. Oncology Nursing Forum. 2007;34:233. [Google Scholar]
- Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice. 2006;721 doi: 10.1186/1471-2296-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network, & American Cancer Society. Distress: Treatment guidelines for patients [version II] Atlanta, GA: American Cancer Society; 2005. [Google Scholar]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Survivorship [v.2.2014] 2014 Retrieved from http://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf.
- Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, et al. Decker V. Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology. 2002;20:4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M, et al. Kershaw T. Living with prostate cancer: Patients' and spouses' psychosocial status and quality of life. Journal of Clinical Oncology. 2007;25:4171–4177. doi: 10.1200/JCO.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, et al. Kershaw T. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS, et al. Penson DF. Long-term functional outcomes after treatment for localized prostate cancer. New England Journal of Medicine. 2013;368:436–445. doi: 10.1056/NEJMoa1209978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Wei JT. Quality of life and satisfaction with outcome among prostate-cancer survivors. New England Journal of Medicine. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- Schover LR, Canada AL, Yuan Y, Sui D, Neese L, Jenkins R, Rhodes MM. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer. 2012;118:500–509. doi: 10.1002/cncr.26308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schymura MJ, Kahn AR, German RR, Hsieh MC, Cress RD, Finch JL, et al. Stuckart E. Factors associated with initial treatment and survival for clinically localized prostate cancer: Results from the CDC-NPCR Patterns of Care Study (PoC1) BMC Cancer. 2010;10152 doi: 10.1186/1471-2407-10-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skolarus TA, Wolf AM, Erb NL, Brooks DD, Rivers BM, Underwood W, III, et al. Cowens-Alvarado RL. American Cancer Society prostate cancer survivorship care guidelines. CA: A Cancer Journal for Clinicians. 2014;64:225–249. doi: 10.3322/caac.21234. [DOI] [PubMed] [Google Scholar]
- Song L, Northouse LL, Braun TM, Zhang L, Cimprich B, Ronis DL, Mood DW. Assessing longitudinal quality of life in prostate cancer patients and their spouses: A multilevel modeling approach. Quality of Life Research. 2011;20:371–381. doi: 10.1007/s11136-010-9753-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song L, Northouse LL, Zhang L, Braun TM, Cimprich B, Ronis DL, Mood DW. Study of dyadic communication in couples managing prostate cancer: A longitudinal perspective. Psycho-Oncology. 2012;21:72–81. doi: 10.1002/pon.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strecher V. Internet methods for delivering behavioral and health-related interventions (eHealth) Annual Review of Clinical Psychology. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Quick guide to health literacy. 2006 Retrieved from http://www.health.gov/communication/literacy/quickguide/Quickguide.pdf.
- U.S. Department of Health and Human Services. Contextual interview. 2015 doi: 10.3109/15360288.2015.1037530. Retrieved from http://www.usability.gov/how-to-and-tools/methods/contextual-interview.html. [DOI] [PubMed]
- Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56:899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- Wilson C, Blostein J. Usability techniques: Pros and cons of co-participation in usability studies. Usability Interface. 1998;4 [Google Scholar]
- Zickuhr K, Madden M. Older adults and internet use. 2012 Retrieved from http://www.pewinternet.org/fles/old-media/Files/Reports/2012/PIP_Older_adults_and_internet_use.pdf.
- Zulman DM, Kirch M, Zheng K, An LC. Trust in the internet as a health resource among older adults: Analysis of data from a nationally representative survey. Journal of Medical Internet Research. 2011;13:E19. doi: 10.2196/jmir.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]